Abstract
Background and Aims:
While prescribed and illicit opioid use are primary drivers of the national surges in overdose deaths, opioid overdose deaths in which stimulants are also present are increasing in the U.S. We determined the social determinants and sociodemographic factors associated with opioid-only versus polysubstance opioid overdose deaths in Massachusetts. Particular attention was focused on the role of stimulants in opioid overdose deaths.
Methods:
We analyzed all opioid-related overdose deaths from 2014–2015 in an individually-linked population database in Massachusetts. We used linked postmortem toxicology data to identify drugs present at the time of death. We constructed a multinomial logistic regression model to identify factors associated with three mutually exclusive overdose death groups based on toxicological results: opioid-related deaths with (1) opioids only present, (2) opioids and other substances not including stimulants, and (3) opioids and stimulants with or without other substances.
Results:
Between 2014 and 2015, there were 2,244 opioid-related overdose deaths in Massachusetts that had accompanying toxicology results. Toxicology reports indicated that 17% had opioids only, 36% had opioids plus stimulants, and 46% had opioids plus another non-stimulant substance. Persons older than 24 years, non-rural residents, those with comorbid mental illness, non-Hispanic black residents, and persons with recent homelessness were more likely than their counterparts to die with opioids and stimulants than opioids alone.
Conclusions:
Polysubstance opioid overdose is increasingly common in the US. Addressing modifiable social determinants of health including barriers to mental health services and homelessness, is important to reduce polysubstance use and overdose deaths.
Keywords: opioid-related overdose, polysubstance use, stimulants, cocaine, amphetamines
1.0. INTRODUCTION
Drug overdose is the leading cause of accidental death in the U.S., with more than 70,000 deaths in 2016 (Scholl, Seth, Kariisa, Wilson, & Baldwin, 2018). While opioids are present and likely causative in the majority of overdose deaths (CDC, 2018; Scholl et al., 2018), it is crucial to gain a better understanding of which other drugs may also be involved and who is affected by polysubstance use. Studies have consistently demonstrated an increased risk of overdose death with concurrent opioid and benzodiazepine use (Hernandez, He, Brooks, & Zhang, 2018; Sun et al., 2017). Concomitant use of stimulants—cocaine and methamphetamine—is rising and may also confer an additional risk of mortality (Al-Tayyib, Koester, Langegger, & Raville, 2017; Degenhardt et al., 2011; McCall Jones, Baldwin, & Compton, 2017; Nechuta, Tyndall, Mukhopadhyay, & McPheeters, 2018; Seth, Scholl, Rudd, & Bacon, 2018; Shiau, Arpadi, Yin, & Martins, 2017; Turner et al., 2018). While other studies evaluated sociodemographic risk factors for drug overdose deaths broadly (Kandel, Hu, Griesler, & Wall, 2017; Nechuta et al., 2018), few have compared non-polysubstance opioids-related deaths with polysubstance opioid-related deaths, specifically with regard to stimulants. This knowledge gap may be fueling disparities in the public health response to the overdose crisis and might overlook key social determinants of health that could help address the addiction crisis. We aimed to determine the factors associated with opioid-related polysubstance overdose death compared with opioid death alone.
2.0. METHODS
We analyzed data from the Massachusetts Public Health Data Warehouse (PHD), previously described as the “Chapter 55” database, a state-permitted, individually-linked database from several Massachusetts government agencies (Massachusetts Budget Summary, 2017; Chapter 55 Acts of 2015, 2015). The PHD links claims-level data from the Massachusetts All-Payer Claims Database (APCD) to other state databases that include person-level demographics and data. Each record is de-identified and assigned a unique identification number that is consistent across all databases (Massachusetts Department of Public Health, 2017). We analyzed opioid overdose deaths among persons 11 years of age and older from January 1, 2014 through December 31, 2015. The creation of the PHD was mandated by law and work within it is conducted by a public health authority.
First, we identified poisoning deaths in the Registry of Vital Records and Statistics mortality files using the International Classification of Disease (ICD-10) codes for underlying cause-of-death poisoning codes: X40–49 (unintentional) or Y10–Y19 (undetermined intent). For this study, we excluded X60–69 (intentional self-harm, suicide) and X85-X90 (assault or homicide). For overdoses, the death certificate lists drugs involved as immediate or contributory causes of death. These are included as ICD-10 “T-codes.” Opioid involvement is indicated by the T-codes T40.0, T40.1, T40.2, T40.3, T40.4, T40.6. We included only those opioid-related overdoses with toxicology data for opioids, stimulants, and selected other substances obtained from the Office of the Chief Medical Examiner (Supplementary Appendix).
Based on toxicology results, we divided the population into 3 mutually exclusive groups: (1) opioid-related deaths with opioids only on toxicology, (2) opioid-related deaths with opioids and an “other substance” (benzodiazepines, alcohol, marijuana, gabapentin, or clonidine) not including stimulants (cocaine or amphetamines) on toxicology, and (3) opioid-related deaths with opioids and stimulants with or without another substance on toxicology. We constructed a multinomial logistic regression model to compare these groups by certain variables (see Supplementary Table 1 for complete variable definitions and data sources). Hepatitis C virus (HCV) infection was not included in the primary analysis since it is incompletely classified in the PHD. A reference group was chosen for each independent variable. The comparison group among the three dependent variable categories of opioid-related death was chosen as only opioids present on toxicology (opioids alone). The model produced two sets of odds ratios and 95% confidence intervals (CIs) for each non-reference exposure variable group: 1) opioids and stimulants vs. opioids alone and 2) opioids and other substances, but no stimulants, present on toxicology vs. opioids alone.
To further examine whether characteristics were different among those who used opioids and stimulants only or opioids, stimulants, and other substances, we performed a secondary analysis in which we categorized the opioid-related deaths into 4 mutually exclusive toxicology groups: (1) opioids only on toxicology (comparison group), (2) opioids and stimulants only on toxicology, (3) opioids and other substances, but no stimulants, on toxicology, and (4) opioids, stimulants, and other substances on toxicology. The methods for this analysis were the same as for the primary analysis.
3.0. RESULTS
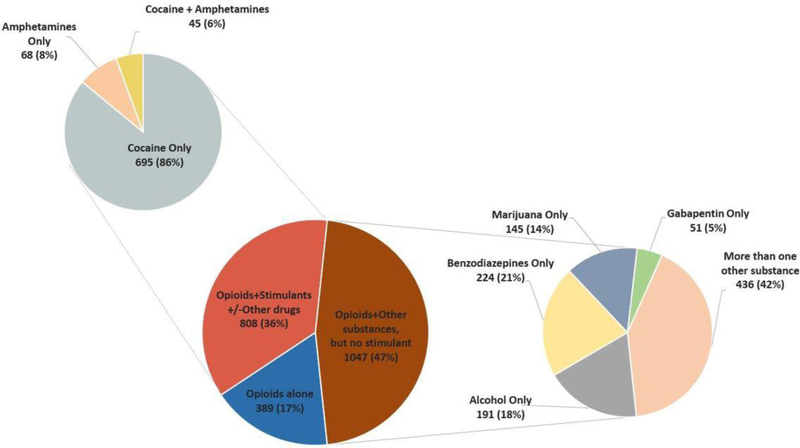
Between 2014 and 2015, we identified 2,928 opioid-related overdoses in Massachusetts, and 2,244 (77%) had accompanying toxicology results (Supplementary Table 2). Of these opioid-related deaths with toxicology results, 72% involved fentanyl or heroin without prescription opioids; 9% involved prescription opioids without fentanyl or heroin; and 19% involved both (Supplementary Table 3). Additionally, 83% of these opioid-related deaths involved another substance in addition to opioids. Specifically, 389 (17%) had opioids-only; 1,047 (47%) had opioids and another substance that was neither cocaine nor amphetamines; and 808 (36%) had opioids plus stimulants with or without another substance. The breakdown of other substances present on toxicology is outlined in Figure 1.
Figure 1. Opioid-related overdose deaths with accompanying toxicology, 2014 and 2015, combined (n=2,244).
This figure demonstrates the proportion of opioid-related overdose deaths by accompanying substances found on toxicology. Deaths were divided into three mutually exclusive groups: (1) opioid-related deaths with opioids only present on toxicology (dark blue), (2) opioid-related deaths with opioids and stimulants (with or without other substances) present on toxicology (red), and (3) opioid-related deaths with opioids and other substances not including stimulants present on toxicology (green). Opioids include any of the following: opiates, fentanyl and fentanyl analogs, tramadol, heroin, hydrocodone, morphine, oxycodone, codeine, hydromorphone, oxymorphone, or prescription opioids not otherwise classified). Stimulants include either cocaine or amphetamines. “Other substances” include any of the following: benzodiazepines, alcohol, marijuana, gabapentin, or clonidine. Smaller pie charts distinguish the specific stimulant or other substance present on toxicology.
The majority of opioid overdose deaths were among men (75%) and non-Hispanic white residents (86%), followed by non-Hispanic black residents (4.2%) (Table 1). Of the 808 deaths that involved stimulants, the proportion of residents who were non-Hispanic black was 6.2%. More than half (54%) of all overdoses occurred in people with comorbid mental health disease.
Table 1.
Characteristics of opioid-related deaths with accompanying toxicology results in Massachusetts, 2014 and 2015 combined
| Total No. (%) |
Opioids alonea No. (%) |
Opioids + Other substancesb, without stimulantsc No. (%) |
Opioids +/− Other substances with stimulants No. (%) |
|
|---|---|---|---|---|
| Total | 2244 | 389 (17) | 1047 (47) | 808 (36) |
| Age | ||||
| 11–24 | 224 (10) | 53 (14) | 110 (10) | 61 (8) |
| 25–44 | 1279 (57) | 220 (56) | 565 (54) | 494 (61) |
| 45+ | 741 (33) | 116 (30) | 372 (36) | 253 (31) |
| Sex | ||||
| Male | 1674 (75) | 303 (78) | 791 (76) | 580 (72) |
| Female | 570 (25) | 86 (22) | 256 (24) | 228 (28) |
| Race/Ethnicity | ||||
| White, non-Hispanic | 1934 (87) | 334 (87) | 943 (91) | 657 (82) |
| Black, non-Hispanic | 94 (4) | 13 (3) | 31 (3) | 50 (6) |
| Hispanic | 186 (8) | 34 (9) | 59 (6) | 93 (11) |
| Other | 21 (1) | § | § | § |
| Residence | ||||
| Non-Rural Rural |
2088 (93) | 351 (90) | 968 (92) | 769 (95) |
| 156 (7) | 38 (10) | 79 (8) | 39 (5) | |
| HIV status | ||||
| Yes | 24 (1) | § | § | § |
| Homelessd | ||||
| Yes | 338 (15) | 47 (14) | 143 (42) | 148 (44) |
| Mental health comorbiditye | ||||
| Yes | 1220 (54) | 165 (42) | 599 (57) | 456 (56) |
| Incarceration in past 12 monthsf | ||||
| Yes | 149 (7) | 28 (19) | 51 (34) | 70 (47) |
| MOUD in the past 12 monthsg | ||||
| Yes | 536 (24) | 88 (16) | 231 (44) | 217 (40) |
There was no missing data for this cohort of persons who had an opioid-related overdose with accompanying toxicology for any of the variables assessed
Opioids include opiates, fentanyl, tramadol, designer fentanyl, heroin, hydrocodone, morphine, oxycodone, codeine, hydromorphone, oxymorphone, or prescription opioids not otherwise classified) on toxicology
Other substances include marijuana, alcohol, gabapentin, benzodiazepines, or clonidine on toxicology
Stimulants include cocaine and amphetamines on toxicology
Homelessness during any period of time from 2011–2015
Includes depression, bipolar disorder, schizophrenia
Any release from prison or jail in Massachusetts in the 12 months that preceded the fatal overdose
Medication for opioid use disorder; includes naltrexone, methadone, or buprenorphine in the 12 months that preceded the fatal overdose
Cells with 1–10 observations were suppressed
Results of the multinomial regression are outlined in Supplementary Table 4. Persons in both of the older age groupings (25–44 and 45 and older) were more likely than the youngest age group (ages 11–24) to overdose with stimulants present than with opioids alone (ages 25–44: odds ratio (OR): 1.84, 95% confidence interval (CI): 1.23–2.76; ages 45 and older: OR: 1.7, 95% CI: 1.10–2.64). The majority of all overdose deaths occurred among those living in non-rural areas (93%). Residents of rural areas were less likely than residents of non-rural areas to overdose with opioids and stimulants on toxicology than with opioids alone (OR: 0.52, 95% CI: 0.33–0.84), whereas the opposite was true for persons with other mental illness compared to those without mental illness (OR: 1.56, 95% CI: 1.20–2.03). Finally, persons with recent incarceration were less likely than those without recent incarceration to die of opioids with non-stimulant substances than with opioids alone (OR: 0.53, 95% CI: 0.36–0.79).
There were also statistically significant and clinically notable findings in the secondary analysis in which the population with stimulants was subcategorized into those with and without other substances (Supplementary Table 5). In this analysis, non-Hispanic black residents were more likely than non-Hispanic white residents to die with stimulants and opioids than with opioids alone (OR: 2.18, 95% CI: 1.01–4.70). Persons with current or recent homelessness were more likely than persons without to die with stimulants and opioids than with opioids alone (OR: 1.85, 95% CI:1.15–2.98).
4.0. DISCUSSION
This study demonstrates that among Massachusetts residents who die from an opioid-related overdose, five out of six (83%) involve another substance in addition to an opioid, and 19% of all deaths involve both heroin or fentanyl and prescription opioids. Using multiple substances, in addition to opioids, is the rule rather than the exception for opioid-related deaths.
Our study supports the notion that there are sociodemographic risk factors that are associated with overdose deaths that involve other substances—particularly stimulants—along with opioids. This analysis demonstrated that non-Hispanic blacks are twice as likely to die with opioids and stimulants than with opioids alone, as compared with non-Hispanic whites. A recent national study demonstrated that cocaine-related overdose death rates in non-Hispanic blacks were nearly equal to opioid-related overdose death rates in non-Hispanic whites (Shiels, Freedman, Thomas, & Berrington de Gonzalez, 2018). It appears non-Hispanic blacks are at increased risk for death from opioid and stimulant use than their non-Hispanic white counterparts, which may be the result, in part, of a cocaine supply that is contaminated with illicitly produced fentanyl (Khatri, Viner, & Perrone, 2018; Tomassoni et al., 2017). It is crucial to recognize this risk in an already marginalized population, such that education efforts address the increasing risk of unintentional exposure to opioids in this population.
Our study is unique in that it highlights important modifiable risk factors associated with different types of overdoses. For example, persons with comorbid mental illness accounted for more than half of all overdoses and were more likely to die with other substances—with or without stimulants—than opioids alone. Current or recent homelessness was a risk factor for overdose with opioids and stimulants; whereas recent incarceration was a risk factor for overdose with opioids alone as opposed to polysubstance overdose. Taken together, these findings provide two key lessons. First, to adequately address the drug overdose epidemic, modifiable risk factors—social determinants of health—such as access to mental health services, homelessness, and incarceration must be addressed on a systemic level. Second, interventions aimed at decreasing overdose mortality need to account for the context of polysubstance use. For instance, overdose with opioids alone among persons recently released from incarceration may reflect the lack of opioid use disorder treatment availability in the penal system. Polysubstance opioid-related overdose may reflect inadvertent exposure to opioids, which might be the case among those recently on medications for opioid use disorder, or it may reflect the increased risk of relapse among those with co-occurring substance use disorders and mental health disorders (Brands et al., 2008; Maremmani et al., 2007; White et al., 2014). It may also reflect that the combined use of stimulants and opioids (e.g., “speedballs”) may lead a person to use increased amounts of opioids or at increased frequency, leading to greater risk of overdose (Glick et al., 2018). Also, people intending to use cocaine, but who were opioid naïve, may unwittingly be exposed to fentanyl mixed into cocaine, which may cause an opioid overdose (Khatri et al., 2018; Tomassoni et al., 2017). Our study draws attention to the heterogeneity of the problem at hand and that there is not a one-size-fits-all approach to addressing the overdose epidemic, which is increasingly driven by polysubstance use. The type of opioid, the presence of polysubstance use, and the social context all influence the type of education and prevention approaches that are needed.
Some limitations to this study merit attention. First, we report only opioid-related overdose deaths and did not examine overdose deaths that did not include opioids as the cause of death, based on ICD codes. The original intent of the legislation that mandated the establishment of the PHD was to study and respond to opioid-related overdoses (Chapter 55 Acts of 2015, 2015). As a result, the toxicology results for non-opioid related deaths were not initially included in the linked datasets. Also, the lack of comprehensive toxicology on all decedents may limit the generalizability of the study. Second, the two-year time period for this study was dictated by data availability (i.e., toxicology reports only available for 2014 and 2015), rather than a hypothesis-based justification. Future studies should assess overdose trends over longer time horizons to corroborate or refute these findings. Third, while the PHD individually links multiple datasets, in most cases these datasets are comprised of administrative data that may be incomplete, such as the APCD that forms the backbone of the database. Thus, certain characteristics (e.g., HCV status) are incompletely classified and were not included in the analysis. Fourth, the variable we used for rurality dichotomized rural and non-rural communities, so we were not able to investigate differences in urban and suburban locations. Finally, we did not include all possible drugs found on toxicology; rather, we chose the ones most likely to be involved in opioid overdoses. Future studies could consider additional drugs that act on the central nervous system, but were not included in this analysis.
5.0. CONCLUSIONS
In sum, we identified social determinants and sociodemographic factors that are associated with opioid overdose deaths involving multiple substances. There is an urgent need to develop and implement tailored programs that address polysubstance use among people who use opioids, especially for populations that are marginalized by and from the healthcare system. This is a crucially important step to addressing the crisis of drug-related harms and associated health disparities in the U.S.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to acknowledge the Massachusetts Department of Public Health for creating the unique, cross-sector database used for this project and for providing technical support for the analysis. The Massachusetts Department of Public Health was not engaged in human subjects research, and no IRB review was required. This project was determined by the Boston Medical University Campus Institutional Review Board to be non-human subjects research.
REFERENCES
- Al-Tayyib A, Koester S, Langegger S, & Raville L (2017). Heroin and methamphetamine injection: an emerging drug use pattern. Subst Use Misuse. 2017;52(8):1051–8. doi: 10.1080/10826084.2016.1271432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brands B, Blake J, Marsh DC, Sproule B, Jeyapalan R, & Li S (2008). The impact of benzodiazepine use on methadone maintenance treatment outcomes. J Addict Dis, 27(3), 37–48. doi: 10.1080/10550880802122620 [DOI] [PubMed] [Google Scholar]
- Commonweath of Massachusetts FY2018 Budget Summary. 2017. http://budget.digital.mass.gov/bb/gaa/fy2018/prnt_18/os_18/p48.htm. Accessed February 1, 2019.
- Degenhardt L, Singleton J, Calabria B, McLaren J, Kerr T, Mehta S, … Hall WD (2011). Mortality among cocaine users: a systematic review of cohort studies. Drug Alcohol Depend, 113(2–3), 88–95. doi: 10.1016/j.drugalcdep.2010.07.026 [DOI] [PubMed] [Google Scholar]
- Glick SN, Burt R, Kummer K, Tinsley J, Banta-Green CJ, & Golden MR (2018). Increasing methamphetamine injection among non-MSM who inject drugs in King County, Washington. Drug Alcohol Depend, 182, 86–92. doi: 10.1016/j.drugalcdep.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez I, He M, Brooks MM, & Zhang Y (2018). Exposure-response association between concurrent opioid and benzodiazepine use and risk of opioid-related overdose in Medicare part D beneficiaries. JAMA Netw Open, 1(2), e180919. doi: 10.1001/jamanetworkopen.2018.0919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel DB, Hu MC, Griesler P, & Wall M (2017). Increases from 2002 to 2015 in prescription opioid overdose deaths in combination with other substances. Drug Alcohol Depend, 178, 501–511. doi: 10.1016/j.drugalcdep.2017.05.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatri UG, Viner K, & Perrone J (2018). Lethal fentanyl and cocaine intoxication. N Engl J Med, 379(18), 1782. doi: 10.1056/NEJMc1809521 [DOI] [PubMed] [Google Scholar]
- Maremmani I, Pani PP, Mellini A, Pacini M, Marini G, Lovrecic M, … Shinderman M (2007). Alcohol and cocaine use and abuse among opioid addicts engaged in a methadone maintenance treatment program. J Addict Dis, 26(1), 61–70. doi: 10.1300/J069v26n01_08 [DOI] [PubMed] [Google Scholar]
- Massachusetts Department of Public Health. An Assessment of Fatal and Nonfatal Opioid Overdoses in Massachusetts (2011–2015). August 2017. Retrieved from https://www.mass.gov/files/documents/2017/08/31/legislative-report-chapter-55-aug-2017.pdf. Accessed 12/31/2018.
- McCall Jones C, Baldwin GT, & Compton WM (2017). Recent increases in cocaine-related overdose deaths and the role of opioids. Am J Public Health, 107(3), 430–432. doi: 10.2105/AJPH.2016.303627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nechuta SJ, Tyndall BD, Mukhopadhyay S, & McPheeters ML (2018). Sociodemographic factors, prescription history and opioid overdose deaths: a statewide analysis using linked PDMP and mortality data. Drug Alcohol Depend, 190, 62–71. doi: 10.1016/j.drugalcdep.2018.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholl L, Seth P, Kariisa M, Wilson N, & Baldwin G (2018). Drug and Opioid-Involved Overdose Deaths - United States, 2013–2017. MMWR Morb Mortal Wkly Rep, 67(5152), 1419–1427. doi: 10.15585/mmwr.mm675152e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seth P, Scholl L, Rudd RA, & Bacon S (2018). Overdose deaths involving opioids, cocaine, and psychostimulants - United States, 2015–2016. MMWR Morb Mortal Wkly Rep, 67(12), 349–358. doi: 10.15585/mmwr.mm6712a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiau S, Arpadi SM, Yin MT, & Martins SS (2017). Patterns of drug use and HIV infection among adults in a nationally representative sample. Addict Behav, 68, 39–44. doi: 10.1016/j.addbeh.2017.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiels MS, Freedman ND, Thomas D, & Berrington de Gonzalez A (2018). Trends in U.S. drug overdose deaths in non-Hispanic black, Hispanic, and non-Hispanic white persons, 2000–2015. Ann Intern Med, 168(6), 453–455. doi: 10.7326/M17-1812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun EC, Dixit A, Humphreys K, Darnall BD, Baker LC, & Mackey S (2017). Association between concurrent use of prescription opioids and benzodiazepines and overdose: retrospective analysis. BMJ, 356, j760. doi: 10.1136/bmj.j760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The 190th General Court of the Commonwealth of Massachusetts. Chapter 55 of the Acts of 2015: An Act Requiring Certain Reports for Opiate Overdoses. In: 2015. Available at: https://malegislature.gov/Laws/SessionLaws/Acts/2015/Chapter55. Accessed December 1, 2018.
- Tomassoni AJ, Hawk KF, Jubanyik K, Nogee DP, Durant T, Lynch KL, … D’Onofrio G (2017). Multiple fentanyl overdoses - New Haven, Connecticut, June 23, 2016 MMWR Morb Mortal Wkly Rep, 66(4), 107–111. doi: 10.15585/mm6604a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner C, Chandrakumar D, Rowe C, Santos GM, Riley ED, & Coffin PO (2018). Cross-sectional cause of death comparisons for stimulant and opioid mortality in San Francisco, 2005–2015. Drug Alcohol Depend, 185, 305–312. doi: 10.1016/j.drugalcdep.2017.12.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White WL, Campbell MD, Spencer RD, Hoffman HA, Crissman B, & DuPont RL (2014). Patterns of abstinence or continued drug use among methadone maintenance patients and their relation to treatment retention. J Psychoactive Drugs, 46(2), 114–122. doi: 10.1080/02791072.2014.901587 [DOI] [PubMed] [Google Scholar]
- US Centers for Disease Control and Prevention. Wide-ranging online data for epidemiologic research (WONDER). http://wonder.cdc.gov. Published 2016. Accessed February 5, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.