Abstract
The contribution of mast cells in the microenvironment of solid malignancies remains controversial. Here we functionally assess the impact of tumor-adjacent, submucosal mast cell accumulation in murine and human intestinal-type gastric cancer. We find that genetic ablation or therapeutic inactivation of mast cells suppresses accumulation of tumor-associated macrophages, reduces tumor cell proliferation and angiogenesis, and diminishes tumor burden. Mast cells are activated by interleukin (IL)-33, an alarmin produced by the tumor epithelium in response to the inflammatory cytokine IL-11, which is required for the growth of gastric cancers in mice. Accordingly, ablation of the cognate IL-33 receptor St2 limits tumor growth, and reduces mast cell-dependent production and release of the macrophage-attracting factors Csf2, Ccl3, and Il6. Conversely, genetic or therapeutic macrophage depletion reduces tumor burden without affecting mast cell abundance. Therefore, tumor-derived IL-33 sustains a mast cell and macrophage-dependent signaling cascade that is amenable for the treatment of gastric cancer.
Subject terms: Cancer microenvironment, Cancer models, Gastric cancer, Interleukins, Tumour immunology
Mast cells within the tumor microenvironment have controversial roles. Here, the authors show, using genetic mouse models, that in gastric cancer, mast cells at the periphery of the tumors are activated via cancer cell produced-IL33 and promote tumorigenesis by recruiting macrophages within the tumors.
Introduction
The interactions between cancer cells and their microenvironment can result in tumor progression as well as suppression and/or eradication of cancers1. Besides extracellular matrix and stromal cells, the tumor microenvironment is composed of immune cells of the adaptive and innate immune system, with the latter comprising neutrophils, macrophages, mast cells, myeloid-derived suppressor cells, dendritic cells, innate lymphocytes, and natural killer cells. Often T-lymphocytes and tumor-associated macrophages (TAMs) account for the most abundant immune cell populations infiltrating established tumors2,3.
Mast cells are long-lived secretory cells of hematopoietic origin that function as sentinels by responding to changes in their environment4. They respond to extrinsic signals through a multitude of cell surface receptors to secrete histamine and proteases from prestored sources in cytoplasmic granules5, alongside newly synthesized inflammatory mediators4. Accordingly, mast cells can be part of innate and adaptive immune responses and therefore contribute to various pathophysiological conditions6. In cancer, the presence of mast cells, both at the tumor periphery and in the tumor core can correlate with disease progression, increased metastasis and reduced survival of patients with melanoma7, prostate cancer8, pancreatic adenocarcinoma9, squamous cell carcinoma10, and gastric cancer11,12. However in other solid malignancies, mast cells have been associated with more favorable outcomes13–15. The conflicting nature of these correlative findings are reminiscent of contradictory functional observations in mouse models claiming that mast cells are required for pancreatic islets tumorigenesis16, while pancreatic adenocarcinoma occurs in a tumor microenvironment devoid of mast cells17.
Interleukin (IL)-33 is a danger-associated signal that can serve as a molecular alarmin when released upon necroptotic and necrotic cell death including death of cancer cells18–21. However, cell death-independent IL-33 release can also occur22,23. IL-33 signals through the heterodimeric ST2 receptor, encoded by Il1rl1 gene, which is constitutively expressed on the surface of some innate immune cells including mast cells24, innate lymphoid cells type 2 (ILC2)25, and regulatory T-cells (Treg)26,27. IL-33/ST2 signaling is involved in triggering innate immune responses upon parasite and viral infections, and has been identified as an important mast cell activating factor24,28 in the context of allergy29. Furthermore, elevated IL-33 expression was associated with poor outcomes in patients with gliomas30, ovarian31, as well as head and neck cancers32. However, predicting the outcome of IL-33/ST2 signaling in malignancies remains uncertain with both tumor promoting as well as tumor restricting activities being reported in knockout mouse models33–36.
Here, we employ preclinically validated mouse models of gastric cancer and corresponding patient biopsies to functionally elucidate the role of mast cells during gastric tumorigenesis. Our genetic analysis reveals a linear signaling axis initiated by tumor epithelial-derived IL-33 that activates mast cells to produce a chemotactic cytokine expression signature. These factors promote the accumulation of TAMs, which in turn sustain tumor angiogenesis and growth in mice. In gastric cancer patients, this mast cell activation signature, alongside markers for tumor-associated macrophages, correlates with decreased patient survival. Our findings delineate an IL-33/mast cell/macrophage axis, which affords a clinical opportunity for the treatment of gastric cancer.
Results
Increased mast cell density in human intestinal-type gastric cancer and in corresponding mouse models
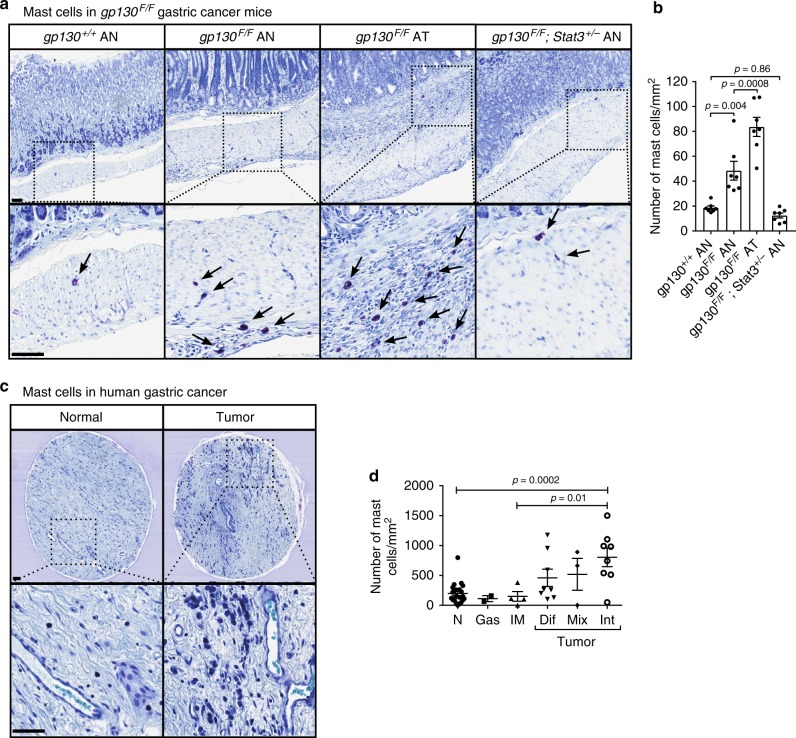
In order to characterize the role of mast cells in gastric cancer, we initially investigated the mast cell frequency in gp130FF mice, a preclinically validated model for spontaneously occurring intestinal-type gastric cancer37,38. Gastric tumors in gp130FF mice, which harbor a knock in germline mutation in the shared IL-6/IL-11 receptor subunit gp130, arise from excessive IL-6/IL-11 dependent STAT3 activity; these tumors remain associated with chronic inflammation and immune cell infiltration. We used toluidine blue stains to quantify mast cells, and observed profound accumulation of mast cells in the submucosa of the gastric antrum in gp130FF mice compared to wild-type mice. Importantly, mast cells in the submucosa adjacent to gastric tumors were more abundant than the mast cells in the normal antrum-associated submucosa of gp130FF mice (Fig. 1a, b). In addition, mast cell numbers in gp130FF; Stat3+/− compound mutant mice, which neither develop gastric tumors nor the other pan-inflammatory changes observed in their Stat3-proficient gp130FF; Stat3+/+ littermates39,40, remained comparable to those in wild-type mice.
Fig. 1.
Submucosal mast cell numbers are increased in gastric cancer in mice and humans. a Representative cross sections of stomachs of 100 day old gp130 mutant mice of the indicated genotype and stained with toluidine blue showing the affected antrum (AN) and antral tumor (AT), respectively. Mast cells appear purple (arrows). Scale bars = 50 µm. b Quantification of submucosal mast cell in sections depicted in (a). n = 7 mice per cohort obtained from two independent experiments, one-way ANOVA F (DFn = degree of freedom nominator, Dfd = degree of freedom denominator) = 34.96 (3, 24). c Representative sections of toluidine blue-stained biopsy cores of human gastric cancer (GC) and adjacent submucosa and of normal stomach submucosa. Scale bars = 50 µm. d Quantification of submucosal mast cell in sections depicted in c. Each symbol represents an individual patient biopsy from submucosa of normal (N; n = 22), gastritis (Gas; n = 2), intestinal metaplasia (IM; n = 4), diffuse (Dif; n = 8), mixed (Mix; n = 3), and intestinal-type (Int; n = 8) gastric cancer. One-way ANOVA F (DFn, Dfd) = 5.809 (5, 41). Data are represented as mean ± SEM, with p < 0.05 considered significant. Source data are provided as a Source Data file. See also related Supplementary Fig. 1
To ascertain that submucosal mast cell accumulation correlated with tumorigenesis independently of the nature of the oncogenic driver mutation, we also assessed mast cell distribution in Tg(Tff1-CreERT2); Pik3caH1047R/+; Ptenfl/fl mice. In this model, conditional activation of a pan-glandular gastric epithelium-specific Cre-recombinase induces aberrant activation of phosphatidylinositol 3-kinase (PI3K), a pathway frequently mutated in human gastric cancer. Akin to our observations in gp130FF mice, mast cells also accumulated in the submucosa of tumors in Tg(Tff1-CreERT2); Pik3caH1047R/+; Ptenfl/fl mice (Supplementary Fig. 1a, b). Strikingly, toluidine blue, alcian blue/safranin O, and May–Grunwald–Giemsa stains for granular content all consistently revealed that mast cells localized to the submucosal layers of the antrum and body of the stomach, rather than within the tumors (Supplementary Fig. 1c).
We next assessed the stromal abundance of mast cells in human biopsies collected from patients with either histopathologically classified diffuse or intestinal-type gastric cancer, or patients with preneoplastic intestinal metaplasia or chronic gastritis. Similar to our observation in mice, we observed a profound submucosal accumulation of toluidine-blue positive mast cells in intestinal-type gastric cancer. Strikingly, mast cells numbers were not elevated in the submucosa of patients with gastritis or intestinal metaplasia (Fig. 1c, d). Collectively, our results show increased mast cell abundance in the tumor-adjacent submucosa of intestinal-type gastric adenocarcinoma in human and mice, irrespective of the nature of the oncogenic driver mutation(s).
Mast cell deficiency diminishes gp130FF-driven tumor growth
Having established a reproducible correlation between submucosal mast cell density and gastric cancer in humans and mice, we next determined the functional role of mast cells during tumor initiation and progression. For this we exploited the gp130FF model because of its high disease concordance with the human GC subtype, reproducible penetrance, onset, and progression of gastric tumorigenesis.
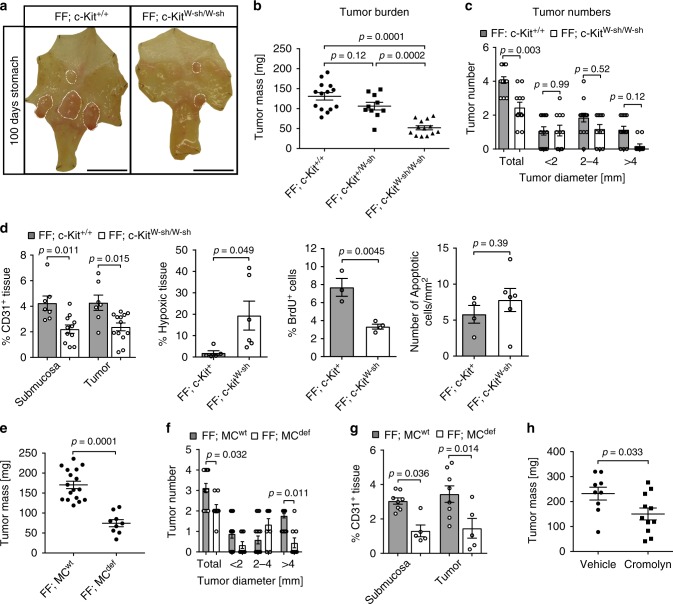
In order to establish whether submucosal mast cell accumulation preceded tumorigenesis, we analyzed stomach sections of 4-week-old gp130FF mice prior to onset of tumor formation. We detected increased mast cell density in the gastric submucosa of these tumor-free gp130FF mice when compared to the submucosa of age-matched WT littermates (Supplementary Fig. 2a). To functionally determine whether mast cells indeed promote gastric tumor growth, we crossed gp130FF mice with mast cell-deficient C57BL/6 c-KitW-sh/W-sh mice carrying an inversion of the 5′-regulatory region of the c-Kit gene that results in hypomorphic expression of the corresponding stem cell factor receptor protein. Accordingly, c-KitW-sh/W-sh mice exhibit a substantial reduction of mast cells in all tissues41–43, but do not suffer from anemia, sterility and lethality associated with complete c-Kit deficiency41. Likewise, we did not observe differences in the peripheral blood composition between gp130FF and gp130FF; c-KitW-sh/W-sh compound mutants and we confirmed that EpCAM positive tumor cells lack c-Kit expression (Supplementary Figs. 2b, c). However, gp130FF; c-KitW-sh/W-sh compound mice had significantly smaller and fewer tumors than their age and sex-matched gp130FF littermates (Fig. 2a–c). This reduction in tumor burden coincided with reduced tumor cell proliferation rather than increased apoptosis, and was associated with a reduction of CD31+ endothelial cells (Fig. 2d and Supplementary Fig. 2d).
Fig. 2.
Gastric tumor burden is reduced in mast cell–deficient gp130FF tumor mice. a Representative whole mounts of pinned out stomachs, from 100-day-old gp130FF; c-Kit+/+ and mast cell-deficient gp130FF; c-KitW-sh/W-sh mice. Scale bars = 1 mm. b Quantification of total tumor burden per mouse as in (a). Each symbol represents an individual mouse. One-way ANOVA F (DFn, Dfd) = 25.97 (2, 24). c Enumeration of total tumor number and tumor size distribution as in a from gp130FF; c-Kit+/+ (n = 14) and gp130FF; c-KitW-sh/W-sh mice (n = 11). One-way ANOVA F (DFn, Dfd) = 24.59 (7, 92). d Quantification of CD31, Hypoxyprobe (hypoxia), BrdU (proliferation), or ApopTag (apoptosis) on immunostained gastric tumors sections. Number of mice (n) for CD31: FF; c-Kit+/+ n = 7, FF; c-KitW-sh/W-sh n = 11 with ANOVA F (DFn, Dfd) = 7.075 (3, 34); Hypoxyprobe: FF; c-Kit+ n = 5, FF; c-KitW-sh n = 6 with t-test + Welch correction’s t (df) = 2.55 (5.256); BrdU: FF; c-Kit+ n = 3, FF; c-KitW-sh n = 4 with t-test’s t (df) = 4.905 (5); Apoptosis: FF; c-Kit+ n = 4, FF; c-KitW-sh n = 6 with t-test’s t (df) = 0.89 (8). e Quantification of total tumor burden per mouse of mast FF; MCwt (genotypes: FF; Cpa3-Creneg; Mcl1fl/fl and FF,Cpa-Cre;Macl1+/+) and mast cell-deficient FF; MCdef (genotype: FF; Cpa3-Cre; Mcl1fl/fl) mice. t-test’s t (df) = 6.72 (24). f Enumeration of the tumor number per mouse of FF; MCwt (n = 17 mice) and mast cell-deficient FF; MCdef (n = 9 FF; Cpa3-Cre; Mcl1fl/fl mice). One-way ANOVA F (DFn, Dfd) = 23.25 (7, 96). g CD31 angiogenic staining quantification of stomachs from (e, f). FF; MCwt (n = 8 mice) and FF; MCdef (n = 5) with one-way ANOVA F (DFn, Dfd) = 6.79 (3, 22). h Quantification of total tumor burden in gp130FF mice after 6 weeks administration of cromolyn (mast cell degranulation inhibitor) or vehicle. Each symbol represents an individual mouse and data was generated in three independent experiments. t-test’s p value is shown and t (df) = 2.313 (18). Data are represented as mean ± SEM, with p values p < 0.05, being considered significant. Source data are provided as a Source Data file. See also related Supplementary Fig 2
To exclude that the anticancer effect of the c-KitW-sh hypomorphic allele was not in part mediated by hematopoietic cells other than mast cells, we generated mast cell-deficient gp130FF; Cpa3-Cre; Mcl1fl/fl gastric cancer mice, where mast cell-specific carboxypeptidase A3 (Cpa3) promoter driven Cre recombinase activity leads to the deletion of Mcl1 prosurvival gene. As a consequence Cpa3-Cre; Mcl1fl/fl mice retain less than 10% mast cells and have reduced numbers of basophils, while all other hematopoietic cell populations remain unaffected44. We confirmed that gp130FF; Cpa3-Cre; Mcl1fl/fl mutant mice lack mast cells in their stomachs, while their gp130FF; Cpa3-Cre; Mcl1+/+ littermates display normal mast cell density (Supplementary Fig. 2e). Importantly, mast cell-deficient gp130FF;Cpa3-Cre; Mcl1fl/fl mice had significantly reduced tumor mass and tumor number compared to their mast cell-proficient controls (Fig. 2e, f), and this observation coincided with reduced angiogenic vessel density in the tumors of gp130FF; Cpa3-Cre; Mcl1fl/fl mice (Fig. 2g).
To assess whether therapeutic mast cell manipulation could reduce the burden of established tumors, we exploited sodium cromoglycate (cromolyn) as a blocking agent for mast cell degranulation in patients. We treated tumor-bearing gp130FF mice for 6 weeks with cromolyn, which significantly decreased tumor burden when compared to vehicle-treated mice (Supplementary Fig. 2f and Fig. 2h). Akin to our observations genetic observations in gp130FF; c-KitW-sh/W-sh and gp130FF; Cpa3-Cre; Mcl1fl/fl mice, cromolyn treatment of gp130FF mice also reduced macrophage accumulation, tumor angiogenesis and proliferation (Supplementary Fig. 2g). These findings demonstrate the importance of mast cells and their released products for gastric tumor growth and suggest that mast cells promote tumor proliferation through mechanisms involving angiogenesis.
In the gp130FF mutant mice all cells harbor the gp130F mutation. When expressed, the gp130F mutant protein increases Stat3 signaling in response to IL-6 family cytokines. Because mast cells express the gp130 coreceptor and can respond to IL-6 family cytokines45,46, we next excluded the possibility that the gp130F allele in mast cells may augment their tumor-promoting ability. For this, we reconstituted the hematopoietic compartment of 6-week-old lethally irradiated gp130FF hosts with the bone marrow from WT (gp130+/+) or gp130FF mice (Supplementary Fig. 2h). Indeed, WT → gp130FF and gp130FF→ gp130FF bone marrow chimeras showed not only similar mast cell frequencies in the gastric submucosa but also comparable tumor burden, and macrophage infiltration in the submucosa and tumor core (Supplementary Fig. 2i). These results indicate that the systemic presence of the gp130FF mutation did not skew hematopoietic cells towards a tumor-promoting role, nor did it increase the mast cell abundance within the gastric tumor microenvironment.
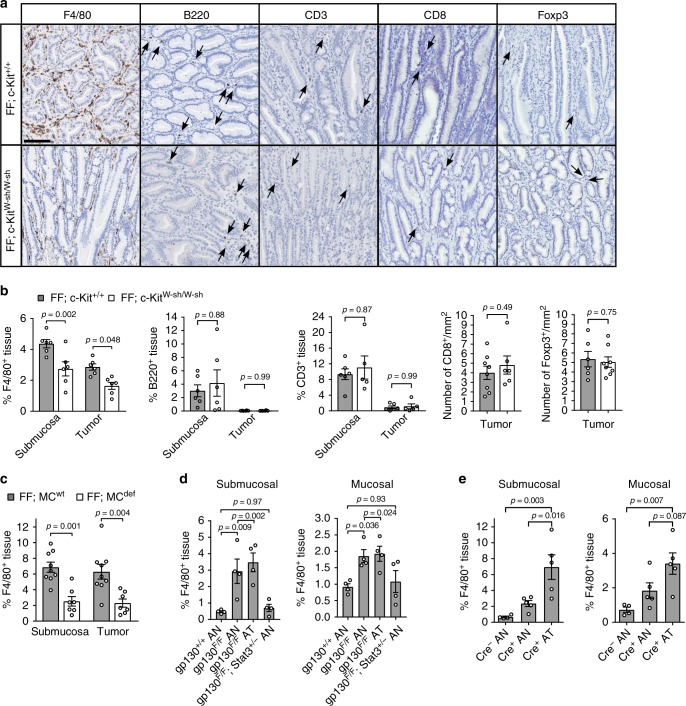
Macrophages are reduced in gastric tumors in a mast cell-dependent manner
Because we observed mast cells outside of the tumor cores, we surmised that tumor-promoting effect of mast cells might occur indirectly by affecting the composition and/or function of tumor infiltrating immune cells. We therefore enumerated tumor-free and tumor-containing stomach sections collected from gp130FF and mast cell-deficient gp130FF; c-KitW-sh/W-sh mice for the F4/80 macrophage, CD3 T lymphocyte and B220 B-lymphocyte markers. While we observed a 30% reduction in macrophage frequency in the submucosa and cores of tumors from gp130FF; c-KitW-sh/W-sh mice, the lymphocyte (CD3+), Treg (Foxp3+), and CD8+ T cell frequencies remained unchanged (Fig. 3a, b). Reduced macrophage abundance within the tumor core and submucosa was also observed in the mast cell-deficient gp130FF; Cpa3-Cre; Mcl1fl/fl mice (Fig. 3c) and cromolyn-treated gp130FF mice (Supplementary Fig. 2g). Because genetic or pharmacological interference with mast cells not only inhibited tumor growth but concomitantly also reduced the abundance of tumor-associated macrophages, we postulate that a hierarchical mast cell—macrophage relationship underpins the growth of gastric cancer.
Fig. 3.
Mast cell depletion reduces macrophage infiltration in gastric tumors of gp130FF mice. a Representative images of tissue sections immunostained for macrophages (F4/80), B cells (B220) or T cells (CD3, CD8, Foxp3) in gastric tumor sections of gp130FF; c-Kit+/+ and mast cell-deficient gp130FF; c-KitW-sh/W-sh mice. Arrows indicate specific positive cell staining; scale bars = 100 µm. b Quantification of F4/80, B220, or CD3 expressing cells in tumor and tumor-associated submucosal layers of sections from (a). F4/80: n = 6 each group, one-way ANOVA F (DFn, Dfd) = 13.43 (3, 20); B220: n = 6 each group, one-way ANOVA F (DFn, Dfd) = 3.782 (3, 20); CD3: FF; c-Kit+/+ n = 6, FF; c-KitW-sh/W-sh n = 5, one-way ANOVA F (DFn, Dfd) = 11.55 (3, 18); CD8: FF, c-Kit+/+ n = 8, FF; c-KitW-sh/W-sh n = 6, t-test t (df) = 0.71 (12); Foxp3: FF, c-Kit+/+ n = 6, FF; c-KitW-sh/W-sh n = 8, t-test t (df) = 0.33 (12). Data from two independent experiments were analyzed. c F4/80+ cells frequency in stomach submucosa and tumors of FF; MCwt mice (n = 9) and mast cell-deficient FF; MCdef mice (n = 7 FF;Cpa3-Cre; Mcl1fl/fl). One-way ANOVA F (DFn, Dfd) = 10.81 (3, 28). d Quantification of F4/80+ cells in unaffected antrum (AN) or antrum tumor (AT) in submucosa or mucosa of mice of the indicated genotype. All groups n = 4. Submucosal: one-way ANOVA F (DFn, Dfd) = 10.12 (3, 12); Mucosal: one-way ANOVA F (DFn, Dfd) = 5.086 (3, 12). e Quantification of F4/80+ cells in unaffected antrum (AN) or antrum tumors (AT) in submucosa or mucosa of mice from the Tg(Tff1-CreERT2); Pik3caH1047R/+; Ptenfl/fl strain that either harbor (Cre+) or lack (Cre−) the Tff1-CreERT2 driver. Cre− AN n = 4, Cre+ AN and Cre+ AT n = 5 for both. Analyses from two independent experiments. Submucosal: one-way ANOVA F (DFn, Dfd) = 10.52 (2, 11); Mucosal: one-way ANOVA F (DFn, Dfd) = 7.485 (2, 11). Data are represented as mean ± SEM, with p values p < 0.05 considered being significant. Source data are provided as a Source Data file. See also related Supplementary Fig. 3
Macrophage infiltration coincides with gastric tumorigenesis
To ascertain that the accumulation of tumor-associated macrophages was a common occurrence for intestinal-type gastric cancers, we assessed macrophages density in the submucosa and mucosa of tumor-bearing gp130FF and Tg(Tff1-CreERT2); Pik3caH1047R/+; Ptenfl/fl mice. We noted an increased abundance of macrophages in the submucosa and the mucosa of either model (Fig. 3d, e and Supplementary 3a, b), consistent with the increased abundance of submucosal mast cells in both models (Fig. 1a, b and Supplementary Fig. 1a, b). To establish whether the increased macrophage accumulation occurs prior to tumor formation, akin to our observations with mast cells, we analyzed naïve gp130FF mice at 4 weeks of age. In these mice macrophage numbers were increased in the submucosal layers, but remained similar between the precancerous mucosa of gp130FF and of WT mice (Supplementary Fig. 3c, d). Collectively, these findings positively correlate macrophage numbers with gastric tumor growth and suggest a potential macrophage contribution to tumor formation and progression.
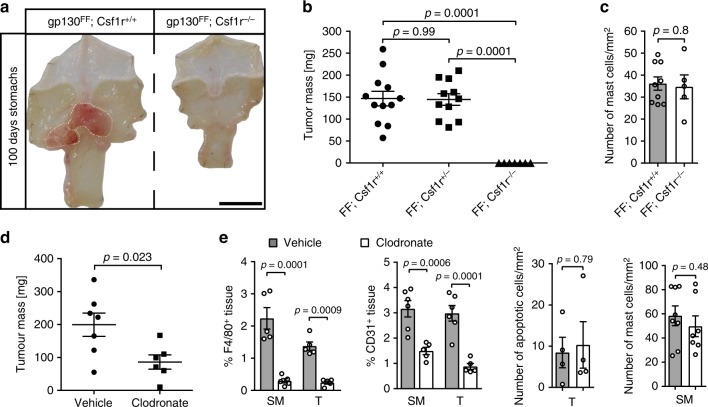
Macrophages are required for gastric tumorigenesis in gp130FF mice
Macrophages have been established as drivers of tumor growth and cancer therapy targets for several tumor entities47,48. To formally investigate a functional contribution of macrophages to gastric tumorigenesis, we generated macrophage-deficient gp130FF; Csf1r−/− mice, because expression of the Csf1r gene and its corresponding receptor protein for macrophage colony-stimulating factor is required for maturation of bone marrow-derived macrophages (BMDM) from their monocytic precursors. Strikingly, the few surviving gp130FF; Csf1r−/− mice remained completely free of gastric tumors (Fig. 4a, b). The submucosal mast cell density was not altered in the macrophage-deficient animals (Fig. 4c). We next confirmed that this phenotype reversion was not related to the runted phenotype of gp130FF; Csf1r−/− mice associated with their feeding requirement for mashed chow to overcome the Csf1R deficiency-dependent absence of teeth. We therefore depleted macrophages in adult tumor-bearing gp130FF mice by systemic administration of clodronate-loaded liposomes (clodrosomes) for 6 consecutive weeks and observed a significant reduction of tumor burden when compared to the vehicle control cohort (Fig. 4d). Although toluidine-staining confirmed that clodrosome treatment did not reduce the abundance of submucosal mast cells, gastric tumors and adjacent submucosa from the clodrosome cohort revealed reduced density of CD31-positive microvessels (Fig. 4e and Supplementary Fig. 4a).
Fig. 4.
Tumor burden in gp130FF mice diminishes upon macrophage depletion. a Representative whole mount of stomachs from 100-day-old mice of the indicated genotype. Scale bar = 1 mm. b Quantification of total tumor burden per mouse as in (a). Each symbol represents an individual mouse. Due to ill health some gp130F/F; Csf1r−/− mice had to be analyzed before the 100 day endpoint; average mouse age per groups were: gp130F/F; Csf1r+/+ 88.2 days, gp130F/F; Csf1r+/− 90.4 days, and gp130F/F; Csf1r−/− 81.6 days. One-way ANOVA F (DFn, Dfd) = 27.55 (2, 27). c Quantification of mast cell density in antral submucosa of indicated genotype was performed with gp130F/F; Csf1r+/+ n = 9 and gp130F/F; Csf1r−/− n = 5 biological samples from two independent experiments t-test t (df) = 0.262 (12). d Assessment of total tumor burden in gp130FF mice after 6 weeks administration of clodronate (50 μl of a clodrosome solution containing 5 mg/ml clodronate) or vehicle. Each symbol represents an individual mouse; data from two independent experiments (t-test t (df) = 2.622 (11)). e Quantification of F4/80, CD31, ApopTag, or toluidine blue (for detection of mast cells) stained sections of gastric tumors (T) and tumor-associated submucosa (SM) from gp130FF mice of the indicated treatment cohort. F4/80: all n = 5, one-way ANOVA F (DFn, Dfd) = 27.17 (3, 16); CD31: n = 6 (SM tissues), n = 5 (T tissues), one-way ANOVA F (DFn, Dfd) = 18.15 (3, 18); apoptotic cells: n = 4 (both groups), t-test t (df) = 0.27 (6); mast cells: n = 8 (vehicle) and n = 7 (Clodronate), t-test t (df) = 0.73 (13). Data are represented as mean ± SEM, with p values p < 0.05 considered being significant. Source data are provided as a Source Data file. See also related Supplementary Fig. 4
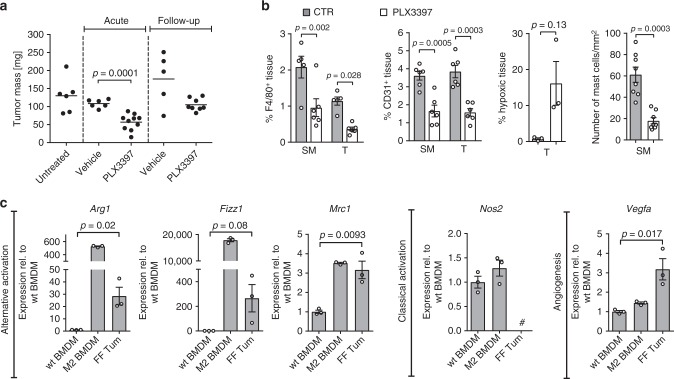
The reduced tumor-burden and microvessel density observed in the clodronate cohort were similar to our findings from the mast cell depletion experiments. We next aimed to exclude that they relate to off-target-effects associated with bisphosphonate (i.e., clodronate) administration. We therefore treated tumor-bearing gp130FF mice with the small molecule Csfr1/c-kit/Flt3 kinase inhibitor PLX3397 (Pexidartinib). We supplied PLX3397 in the food to tumor-bearing gp130FF mice for 4 weeks (acute therapeutic) and continued a cohort for a further 4 weeks without PLX3397 treatment (follow-up) (Supplementary Fig. 4b). Acute PLX3397 treatment revealed a significant reduction in tumor burden, although this antitumoral effect was reversible as the tumor burden increased once PLX3397 treatment ceased in the follow-up cohort (Fig. 5a). In the acute treatment cohort, we confirmed by immunohistochemical staining a significant reduction of F4/80-positive macrophages accompanied by reduced density of CD31-positive angiogenic vessels and increased staining for tumor-hypoxia (Fig. 5b and Supplementary Fig. 4c). However, owing to the specificity of PLX3397, we also observed a decrease of tumor-adjacent submucosal mast cells. All these parameters reverted back to their pretreatment state following a drug-free period in the follow-up cohort (Supplementary Fig. 4c).
Fig. 5.
Pharmacological macrophage targeting and macrophage polarization in gp130FF tumors. a Total tumor burden in gp130FF mice was quantified either acutely after a 4-week-treatment period with PLX3397 (Csf1r/c-Kit/Flt3 tyrosine kinase receptor inhibitor) or vehicle or after a 4 weeks treatment-free follow-up period. Each symbol represents an individual mouse. Data from three independent experiments are presented. t-test t (df) = 5.23 (14). b Quantification of F4/80, CD31, Hypoxyprobe or toluidine-blue-stained sections of submucosa (SM) or gastric tumors (T) of gp130FF mice of the indicated acute treatment cohort. F4/80: n = 5 (Vehicles) and n = 6 (PLX3397), one-way ANOVA F (DFn, Dfd) = 12.34 (3, 18); CD31: n = 6, one-way ANOVA F (DFn, Dfd) = 18.33 (3,20); hypoxic tissue: n = 3, t-test with Welch’s correction t (df) = 2.53 (2); mast cells: n = 8 (both groups), and t-test with Welch’s correction t (df) = 5.59 (9.27). c qPCR expression analysis of genes associated with alternative activation (Arg1, Fizz1, Mrc1), classical activated (Nos2) and angiogenesis (Vegfa) of purified F4/80+ tumor-associated macrophages (FF Tum) or following stimulation of bone marrow-derived macrophages (BMDM) from wild-type mice and stimulated either with vehicle (wt BMDM) or with IL-4/IL-13 (20 ng/ml) to induce an alternative activated endotype (M2 BMDM). n = 3 mice. Hash indicates that expression was below detection limit. Arg1: t-test t (df) = 3.8 (4); Fizz1: t-test t (df) = 2.39 (4); Mrc1: t-test t (df) = 4.69 (4); Vegfa: t-test t (df) = 3.96 (4). Data are represented as mean ± SEM, with p values p < 0.05 considered being significant. Source data are provided as a Source Data file. See also related Supplementary Fig. 4
Based on our proposed role for macrophages to mediate the tumor promoting effect of mast cells, we hypothesized that the tumor-associated macrophages in the gastric lesions of gp130FF mice should have a tumor-promoting alternatively activated endotype. We therefore compared expression of macrophage endotype markers between naïve BMDM and tumor-associated macrophages, and used standard in vitro polarization protocols for BMDM to generate a reference population for alternative activation. For the tumor-associated macrophage populations, this analysis revealed high expression of the alternative activation markers Arg1, Fizz1, and Mrc1, which coincided with reduced mRNA levels of the classically activated marker Nos2 (Fig. 5c). Consistent with the pronounced presence of microvasculature in tumors of these gp130FF mice, we also recorded elevated expression of angiogenic Vegfa in the tumor-associated macrophage population when compared to the naïve BMDM population from the same mice (Fig. 5c). Given the alternative activated endotype of tumor-associated macrophages, our data collectively suggests that their abundance is likely to be a rate-limiting factor for the establishment of tumor microvasculature and the growth of gastric tumors.
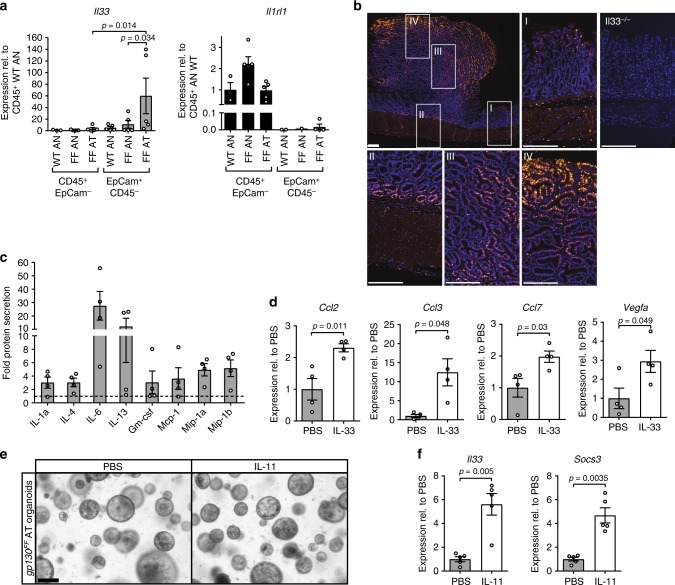
Tumor-derived IL-33 activates mast cell secretion and expression of macrophage-attracting chemokines
Although our observations thus far suggested a functional mast cell–macrophage relationship, it remained to determine the molecular network underpinning this hierarchy including how its activation could occur. We therefore focused on IL-33 as a potential tumor-derived activator of mast cells, because IL-33 was reported to serve as an alarmin that is generated and released by necrotic cells, and that triggers mast cell degranulation49. Indeed, we detected increased expression of Il33 in the EpCam+/CD45− epithelial components of the tumors in gp130FF mice with a reciprocal expression of the Il1rl1 gene in the hematopoietic CD45+/EpCam− compartment of the antrum, which encodes the cognate St2 receptor subunit for IL-33 (Fig. 6a). In line with the reported storage of IL-33 protein in vesicles, we detected increased levels of Il33 mRNA and IL-33 protein in whole tumor tissue (Supplementary Figs. 5a, b). Immunofluorescence staining revealed that IL-33 protein localized most prominently to the peripheral regions of the epithelial components of the tumors (Fig. 6b) coinciding with the location of the highest level of cellular turn-over37.
Fig. 6.
IL-33 expression in gastric tumors of gp130FF mice and mast cell activation analysis. a qPCR expression analysis of Il33 and full-length St2 (Il1rl1) genes associated with hematopoietic (CD45+; EpCam−) and epithelial (EpCam+; CD45−) cells purified from unaffected antrum (AN) or antrum tumors (AT) from wild-type and gp130FF (FF) mice. Data are normalized to Gapdh and plotted as relative expression to CD45+; EpCAM− WT AN expression. n = 5 mice. Il1rl1 expression in EpCam+; CD45− cells was for several samples below detection limit. Data was pooled from two independent experiments. For IL33 data, one-way ANOVA was performed with F (DFn, Dfd) = 2.871(5, 22); b Immunofluorescence staining for IL-33 in stomachs of tumor-bearing gp130FF mice with insets referring to unaffected antrum (I), submucosal-tumor junction (II), tumor core (III), and tumor edge (IV). Stomachs from Il33−/− mice were used for specificity controls. Scale bars = 200 µm. c Multiplex cytokine analysis of supernatant of FACS-purified tumor-associated mast cells stimulated with IL-33 (30 ng/ml) for 3 h. Data are shown only for factors with > 3 fold increase relative to unstimulated control cultures. n = 4 from four independent experiments. d qPCR gene expression analysis in FACS-purified tumor-associated mast cells stimulated with IL-33 (30 ng/ml) for 3 h or vehicle. n = 4 from four independent experiments. Ccl2: t-test t (df) = 3.61 (6); Ccl3: t-test t (df) = 3.2 (3.09); Ccl7: t-test t (df) = 2.84 (6); Vegfa: t-test t (df) = 2.45 (6). e Representative images of organoids derived from antral tumors (AT) of gp130FF mice stimulated either with PBS or IL-11 (100 ng/ml for 2 days). Scale bar = 200 µm. f Il33 gene expression analysis of gp130FF tumor-derived epithelial organoids either stimulated with IL-11 (100 ng/ml) or with PBS for 4 h. For comparison expression of Stat3-target gene, Socs3, was also analyzed. n = 5 from two independent experiments. Stat3: t-test t (df) = 4.96 (4.42); Socs3: t-test t (df) = 5.6 (4.48). Data are represented as mean ± SEM, with p values p < 0.05 considered being significant. Source data are provided as a Source Data file. See also related Supplementary Fig. 5
To assess whether tumor-associated mast cells could respond to IL-33, we FACS purified the c-Kit+/FcεR1+ mast cells from the submucosal antrum of WT and gp130FF mice using stomachs from gp130FF; c-KitW-sh/W-sh mice as a specificity control for our purification strategy (Supplementary Fig. 5c). We confirmed the homogeneity of the c-Kit+/FcεR1+ mast cell population by toluidine blue staining (Supplementary Fig. 5d) and showed prominent expression of the St2 receptor in the c-Kit+/FcεR1+ mast cells isolated from the stomach of gp130FF mice (Supplementary Fig. 5e). We then stimulated this cell population for 3 h with IL-33 and detected by the multiplex cytokine assay increased amounts of IL-6 and IL-13 and to lesser extent of IL-1α, IL-4, alongside elevated secretion of the macrophage growth and attracting factors Gm-csf, Mcp1, Mip-1α, and Mip-1β (Supplementary Fig. 5f and Fig. 6c). Likewise, qPCR analysis of the IL-33 stimulated mast cells also revealed increased expression of Ccl2 (encoding Mcp1 protein), Ccl3 (encoding Mip-1α protein), and Ccl7 (Fig. 6d), which collectively exert chemotactic activity towards macrophages and neutrophils50–52. Also, IL-33-stimulation induced elevated expression of angiogenic growth factor gene Vegfa (Fig. 6d). In order to confirm the chemotactic activity of the mast cell produced factors on gp130FF macrophages, we performed migration assays with BMDM. Indeed, Mcp1 and Mip-1α alone induced migration significantly (Supplementary Fig. 5g).
Because gp130FF-driven gastric tumorigenesis has an absolute requirement for IL-11 signaling38, we predicted that IL-11 could stimulate IL-33 expression in tumor-derived epithelium. To test this, we exposed epithelial organoids grown from gp130FF-tumors to recombinant IL-11 in vitro. While organoid growth and morphology were not altered (Fig. 6e and Supplementary Fig. 5h), we observed a marked increase in Il33 expression upon IL-11 stimulation, which was comparable to the extent of induction of the bona fide IL-11/Stat3-target gene Socs3 (Fig. 6f). Additionally, we conducted a chromatin immunoprecipitation (ChIP) experiment on DNA from gastric tumors of gp130FF mice 60 min after acute systemic administration of IL-11. The ChIP experiment revealed a Stat3-specific binding peak on chromosome 19, which maps to the 5′-region of the Il33 gene and which contains a Stat3-binding site motif (Supplementary Fig. 5i, j). Collectively, these data indicate that tumor-derived IL-11 induces Il33 gene expression in gastric tumor cells, which triggers the secretion as well as the de novo synthesis of cytokines and chemokines by mast cells to produce a tumorigenic immune environment.
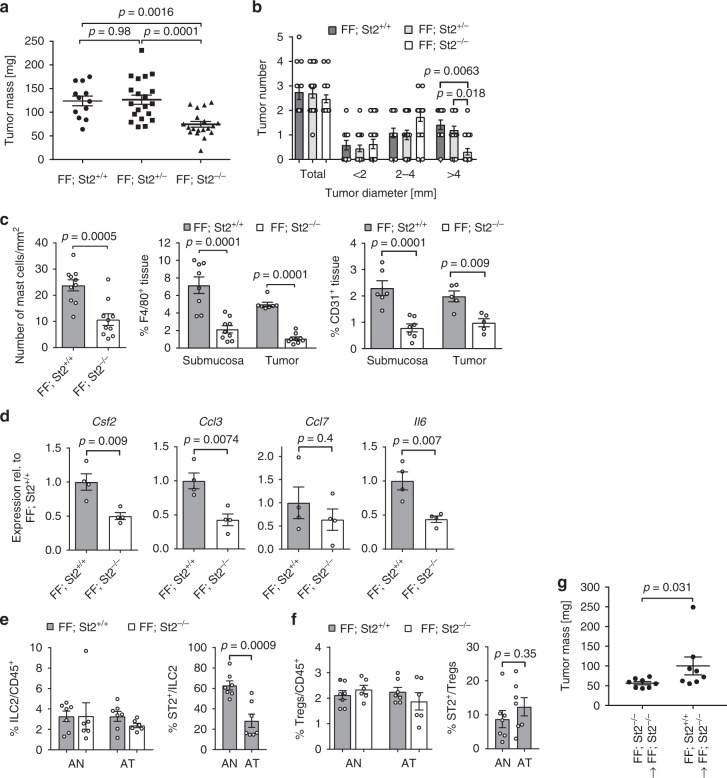
IL-33/St2 signaling deficiency decreases gp130FF-mediated gastric tumor growth
To validate a functional contribution of IL-33 signaling as a master regulator of mast cell activation in the gastric tumor microenvironment, we generated IL-33 signaling deficient gp130FF; St2−/− mice. Compared to their St2+/+ and St2+/−-proficient compound mutant littermates, gp130FF; St2−/− mice harbored a significantly lower overall tumor burden at 100 days of age (Fig. 7a), which arose from reduced tumor growth rather than reduced tumor incidence (Fig. 7b). These observations coincided with a decrease in mast cell numbers in the tumor-adjacent submucosal layers and reduced density of F4/80+ macrophages in the tumors of gp130FF; St2−/− mice as well as reduced abundance of CD31-positive microvessels (Fig. 7c).
Fig. 7.
Tumor burden is reduced in St2 receptor-deficient gp130FF mice. a Quantification of total tumor burden in 100-day-old mice of the indicated genotype. Each symbol represents an individual mouse. One-way ANOVA was performed with F (DFn, Dfd) = 11.83 (2, 48). b Enumeration of total tumor number from mice in a, and of tumors following classification according to their size. n = 12 (FF, St2+/+), n = 20 (FF, St2+/−), and n = 19 (FF, St2−/−) mice. One-way ANOVA was performed with F (DFn, Dfd) = 22.79 (11, 192). c Quantification of toluidine blue (for detection of mast cells; submucosal tissue), F4/80 and CD31 stained sections of gastric tumors of mice of the indicated genotype. Mast cells: n = 10 mice, t-test t (df) = 4.25 (18); F4/80: n = 8 (FF; St2+/+), n = 9 (FF; St2−/−), one-way ANOVA F (DFn, Dfd) = 27.52 (3,29); CD31: n = 6 (Submucosa) n = 5 (Tumor), and one-way ANOVA F (DFn, Dfd) = 13.6 (3,19). d qPCR expression analysis of chemokines expressed by FACS-purified tumor-associated mast cells from stomachs of either FF; St2+/+ or FF; St2−/− mice. All n = 4 from two independent experiments. Csf2: t-test t (df) = 3.81 (6); Ccl3: t-test t (df) = 3.97 (6); Ccl7: t-test t (df) = 0.88(6); Il6:: t-test t (df) = 4.02 (6); e, f Flow cytometric analysis of unaffected antrum (AN) and antrum tumors (AT) of indicated genotype for the frequency of ILC2 cells (lineage−, Cd11b−, Gata3+), Tregs (Foxp3+, CD4+), and proportion of St2+ cells within these cell types. FF; St2+/+ n = 7 and FF; St2−/− n = 6, from two independent experiments. ST2+/ILC2: t-test t (df) = 4.39 (12); ST2+/Treg: t-test t (df) = 0.98 (12). g Enumeration of total tumor burden at 14 weeks of age of FF; St2−/− host mice, which received tail vein injections of either FF; St2−/− or FF, St2+/+ bone marrow-derived mast cells (BMMC) (n = 8 mice per group). Mann–Whitney test was performed with Mann–Whitney U = 11.5. Data are represented as mean ± SEM, with p values p < 0.05 considered being significant. Source data are provided as a Source Data file. See also related Supplementary Fig. 6
We next confirmed that c-Kit+/FcεR1+ mast cells isolated from gp130FF; St2−/− mice showed significantly decreased expression of the macrophage recruiting and inflammatory mediators Csf2 (encoding Gm-csf), Ccl3, and Il6 (Fig. 7d). Because IL-33 signaling is involved in expansion and activation of ILC2 and Tregs, which could also afford a mechanism for IL-33 to promote gastric tumorigenesis in gp130FF mice, we assessed the relative abundance of ILC2 and Tregs among all cells harboring the pan-hematopoietic surface marker CD45. We observed comparable frequency of these cells between unaffected antrum and tumors of gp130FF and gp130FF; St2−/− mice. Moreover, less than 30% of all tumor-associated ILC2 cells, and less than 15% of all Tregs, expressed the St2 receptor (Fig. 7e, f).
To investigate the involvement of mast cells in the antitumoral effect of St2-deficiency, we established bone marrow-derived mast cells (BMMC) from gp130FF; ST2−/− and gp130FF; St2+/+ mice, confirmed their purity (Supplementary Figs. 6a–c) and performed adaptive transfer of BMMC into gp130FF; St2−/− hosts (Supplementary Fig. 6d). Reconstitution with St2+ wild-type BMMC (gp130FF; St2+/+) increased tumor burden compared to littermates injected with gp130FF; St2−/− BMMCs (Fig. 7g and Supplementary Fig. 6e). At the time point of tumor analysis 8% of the gastric submucosal mast cells stained positive for St2 expression and therefore represent the transplanted BMMC mast cells, which homed to the gastric tumor site and compete with the endogenous ST2−/− mast cell compartment (Supplementary Fig. 6f).
These observations further support a mechanism by which IL-33 promotes gastric tumorigenesis through mast cell activation rather than by promoting ILC2 or Treg accumulation.
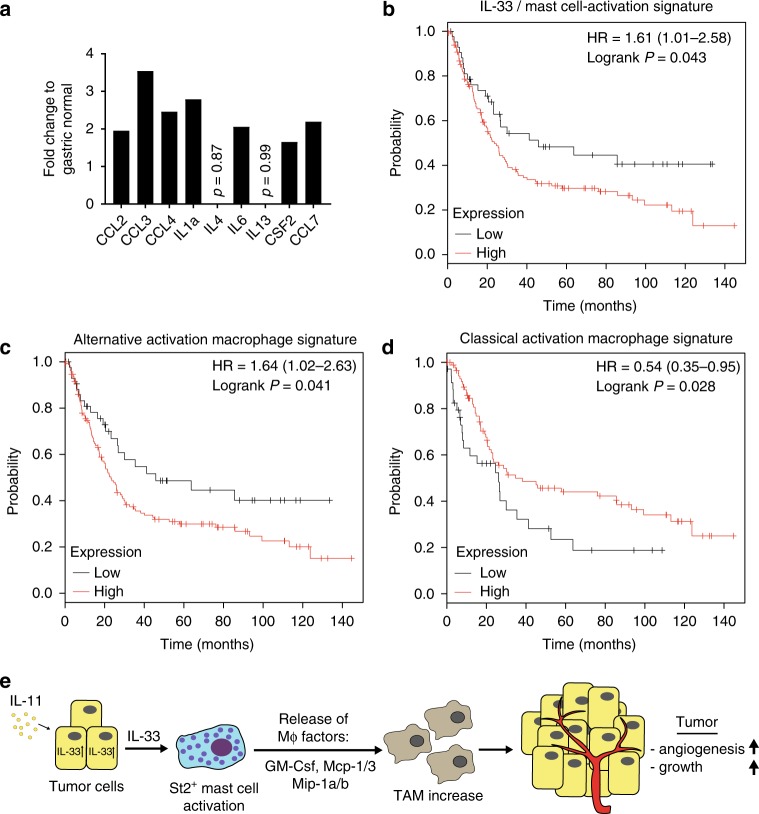
IL-33/mast cells-activity gene expression signature predicts poor survival for human intestinal-type gastric cancer
In order to translate our preclinical findings in mice to a relevant setting in humans, we hypothesized that the extent of mast cell activation might provide retrospective prediction of patient survival. Based on the mast cell activation gene expression signature derived from our in vitro mast cell stimulation with IL-33, we analyzed a publically available data set (DErrico Gastric data set; GEO: GSE13911) for differential expression of the mast cell signature comprising CCL2, CCL3, CCL4, IL1a, IL4, IL6, IL13, CSF2, and CCL7. With the exception of IL-4 and IL-13, we found that all other factors were at least 1.6-fold increase in the cancer samples (p ≤ 0.05) (Fig. 8a). We therefore assigned the differentially expressed factors (i.e., CCL2, CCL3, CCL4, IL1a, IL6, CSF2, and CCL7) to an IL-33/mast cell activation gene expression signature for a Kaplan–Meier survival analysis (KMplot.com)53. Remarkably, we found a lower overall survival for intestinal-type gastric cancer patients with high expression of the entire signature (HR = 1.61; logRank P = 0.043) (Fig. 8b). Similar to our IL-33/mast cell activation gene expression signature, a trend for better survival probability was found for high expression of a classical mast cell marker gene signature consisting of KIT, FCER1G, and HDC (encoding Histidine Decarboxylase) (HR = 1.42; logRank P = 0.067) (Supplementary Fig. 7a) as well as for ST2-receptor encoding gene IL1RL1 (HR = 1.57; logRank P = 0.049) (Supplementary Fig. 7b). In accordance with our mast cell–macrophage hierarchy model, Kaplan–Meier survival analysis for macrophages revealed a survival disadvantage for intestinal-type gastric cancer patients with high expression of an alternatively activated macrophage gene signature (Fig. 8c). On the other hand, high expression of a classically activated gene signature correlates with a higher survival probability (Fig. 8d). Our preclinical data argue strongly for a tumor promoting role of a signaling axis emanating from IL-11-induced, tumor cell-derived IL-33 and the subsequent hierarchical activation cascade of mast cells and tumor-associated macrophages. Collectively, these innate immune cells enable the establishment of the microvasculature required for gastric tumor growth and may provide therapeutically actionable targets (Fig. 8e).
Fig. 8.
Kaplan–Meier analysis for an IL-33 - mast cell activation gene expression signature. a Expression analysis of genes associated with IL-33 dependent mast cell activation derived from the DERRICO gastric data set (GEO: GSE13911, extracted from oncomine.org) and comparing normal gastric mucosa (n = 31) and gastric intestinal-type adenocarcinoma (n = 29). The p-value for the genes is p < 0.05 except where indicated. b–d Kaplan–Meyer survival analysis was performed for human intestinal-type gastric cancer (iGC) with IL-33/ mast cell activation signature consisting of CCL2, CCL3, CCL4, IL1a, IL6, CSF2, and CCL7 (b), with alternative activation macrophage expression signature (CD163, CD204, MARCO, ARG1) (c) and classical activation macrophage expression signature (NOS2A, HLA-DRA, CD80, CD86, CD169) (d). e Schematic illustration of the proposed gastric cancer growth promoting IL-11/IL-33/mast cell/TAM signaling axis. Source data are provided as a Source Data file. See also related Supplementary Fig. 7
Discussion
Although conflicting data indicate a dichotomous role of mast cells to either restrict or support tumorigenesis, compelling evidence implicates mast cells in promoting progression and metastasis in many solid malignancies. Retrospective studies on human gastric cancers have suggested an involvement of tumor-adjacent submucosal mast cells to late stage disease54 and metastasis formation12. However, the molecular mechanism by which submucosal mast cells contribute to gastric tumorigenesis, and indeed early stage tumorigenesis, is not understood. Here we demonstrate that submucosal accumulation of mast cells in two independent murine models of intestinal-type gastric cancer functionally contributes to tumorigenesis and the maintenance of established tumors and that this coincides with the presence of alternatively activated protumorigenic tumor-associated macrophages. We provide evidence that tumor cell-derived IL-33 stands on the apex of a cascade by which mast cells, through recruitment of tumor-associated macrophages and their support of a vascular network, ensures the growth and maintenance of gastric tumors. Indeed, ablating mast cells or macrophages in tumor-bearing mice either individually with cromolyn or clodrosomes, or together with PLX3397, were associated with a vascular collapse and tumor hypoxia. Importantly, we support the relevance of our functional findings in mice with a correlation in humans where a mast cell activation signature associates with poor patient outcome for intestinal-type gastric cancer.
Within the tumor microenvironment, myeloid cells are among the most important innate immune cells that promote tumor formation and restrict the effect of many forms of therapy, most notable immunotherapy55. In particular the plasticity of tumor-associated macrophages has attracted interest as therapeutic opportunities to limit the angiogenic and immune suppressive functions conferred by their alternatively activated endotype3. On the other hand, mast cells have been proposed to be an abundant source of VEGF, TGFβ, and other angiogenic factors, as well as matrix metalloproteinase 9 and related stromal remodeling enzymes56. Indeed, mast cells are one of the earliest cell types recruited into the tumor microenvironment11,57, and progression of gastric cancer correlates with both the accumulation of chymase-positive mast cells and increased microvascular density11,58. Functionally, these observations are mirrored by an angiogenic switch proposed to be orchestrated by mast cells during early stages of pancreatic cancer in mice required for the extensive vascular elaboration to prevent hypoxia during expansion of tumors16. Surprisingly, the authors in this early study had argued against a role for macrophages in mast cell-dependent induction of early tumor angiogenesis, based on their observations that macrophage recruitment to pancreatic islets remained unaffected by mast cell deficiency. Indeed, our observations that IL-33 result in the induction of Vegfa expression in isolated mast cells supports this view and this is corroborated by reduced microvessel density in tumors of gp130FF; St2−/− mice. However, our observations presented here following either genetic ablation of mast cells or macrophages, or their respective pharmacological inhibition by cromolyn and clodronate or PLX3397 strongly suggest that the endothelial cell support provided by mast cells also depends in part on the recruitment of macrophages.
Because we functionally link tumor growth to the presence of mast cells in two independent genetic models, it is highly unlikely that this arises from independent serendipitous effects of the two models other than mast cells. Thus, it is highly likely that the incompletely understood mechanisms by which cromolyn blocks mast cell degranulation mediated the anti-tumor effect observed here, rather than cromolyn also affecting monocytes, the production of the neutrophil product myeloperoxidase, and circulating growth59. Akin to tumor-associated macrophages being induced by tumor cells to adopt an alternatively activated endotype optimized for wound healing, neoplastic epithelia appears to also corrupt the wound healing function of mast cells to facilitate tumor growth55. Accordingly, tumor cell-specific overexpression of the master-regulator c-Myc not only results in epithelial hyper-proliferation (when coinciding with increased expression of BH3 survival proteins) but also in expression of chemo-attracting CCL2, CCL3, and CCL5 and concomitant accumulation of mast cells16. Here we identify a second mechanism that depends on the IL-1 cytokine family member IL-33, which acts as a chief regulator of innate immunity and inflammation, and maintains epithelial barrier functions of the intestine. Indeed, IL-33 serves a bona fide alarmin and is released by damaged epithelium as an endogenous danger signal to activate innate immune responses28. Accordingly, mast cells and ILC2s respond through the IL-33/ST2 axis to the damaged intestinal mucosa arising from acute injury or infection. Therefore mast cells are found at sites of epithelial recovery60, and ILC2 cells release IL-13 to stimulate the intestinal stem cell compartment, respectively61. Intriguingly, our experimental lines of evidence from tumors of gp130FF; St2−/− mice show that their reduced tumor burden correlates with decreased mast cell frequency rather than a change in ILC2 abundance. While not ruling out minor contributions by ILC2, regulatory T-cells or other IL-33 responsive cells, the increased tumor mass in gp130FF; St2−/− mice following adoptive transfer of St2-proficient mast cells, provides definitive functional evidence that mast cells act as the major cell population through which IL-33 promotes tumor growth. Accordingly tumor growth of gp130FF mice was susceptible to the highly mast cell-selective cellular deficiency in gp130FF; Cpa3-Cre; Mcl1fl/fl mice, or to cromolyn-dependent inhibition of mast cell degranulation. Meanwhile, and consistent with the capacity of IL-33 to promote tissue repair and wound healing, IL-33 can also mediate metaplasia of the gastric epithelium62.
Although epithelial cells of barrier tissues exposed to the environment are major sources of IL-33, and IL-33 expression is further increased during inflammation and in the tumor epithelium63, the exact nature of the factors that induce IL-33 expression and its release remain unclear. For instance TNF, IL-1β, TGFβ, prostaglandins, lipopolysaccharides, and other pathogen-associated molecular patterns have all been suggested as drivers for IL-33 expression during intestinal adenomatous polyposis64–66. Here, we provide evidence for IL-33 expression in gastric tumor epithelium to also be stimulated by an IL-11/Stat3 signaling cascade, which we and others have identified as an absolute requirement for effective growth of gastrointestinal tumors. However, at this stage we can only speculate that subepithelial myofibroblasts and possibly tumor-associated endothelial cells, which have been proposed as sources of IL-1167, may also contribute to epithelial expression of IL-33. Furthermore, because mast cells express gp130, we could not formally exclude the possibility that the presence of the hypermorphic gp130F allele in mast cells may promote their proliferation and survival46, as this receptor allele augments Stat3 signaling in response to IL-6 family cytokines. However, we noted similar submucosal mast cell accumulation adjacent to tumors in gp130FF and in Tg(Tff1-CreERT2); Pik3caH1047R/+; Ptenfl/fl mice, where the latter cohorts express WT gp130. Likewise, reconstitution of gp130FF mice with WT bone marrow did not affect mast cell numbers and tumor burden, as would be expected if the gp130F allele augmented mast cell activity.
Therapeutic inhibition of IL-33 signaling is gaining interest with anti-ST2 antibodies being trialed for asthma. Given the dichotomous activity of IL-33 in tumor biology, timing of anti-IL-33 signaling therapy will be crucial. In the context of gastric cancer, mast cells may not only promote metastasis but also modulate the immunosuppressive tumor environment through the release of IL-1768. Thus, IL-33 signaling provides a target to restrict the tumor promoting activities of the myeloid compartment and may ultimately enable rational combination therapies to alleviate the activity by which myeloid cells limit the antitumor immune response. The linear signaling cascade identified here comprising IL-11/IL-33/mast cells/macrophages/tumor cells should provide complementary molecular and cellular targets for the development of improved cancer therapies.
Methods
Study approval
All animal studies were conducted in accordance with all relevant ethical regulations for animal testing and research including the Australian code for the care and use of animals for scientific purposes. All animal studies were approved by the Animal Ethics Committee of the Ludwig Institute for Cancer Research, the Walter and Eliza Hall Institute of Medical Research, or Austin Health.
We have complied with all relevant ethical regulations for work with human participants. Collection and usage of human gastric cancer tissues was approved by the Peter MacCullum Cancer Center Ethics Committee and informed consent was obtained from all subjects.
Mice
Knockin mice (gp130Y757F/Y757F, alias gp130FF mice), the compound mutants strains gp130FF; Stat3+/−39,40 and Tg(Tff1-CreERT2); Pik3caH1047R/+; Ptenlox/+ as well as wild-type control mice were bred on a mixed C57B6 × 129/Sv background. gp130FF; c-KitW-sh/W-sh41, gp130FF; Csf1r−/−69, and gp130FF; St2−/− mice70, knockout of the Il-33 receptor (encoding gene name: Il1rl1), gp130FF; Cpa3-Cre; Mcl1lox/lox44 (mast cell-deficient gp130FF compound mutant mice) were maintained on a C57B6 background.
Tg(Tff1-CreERT2); Pik3caH1047R/+; Ptenlox/+ compound mutant mice were established, where mutant allele induction is induced by the Tff1-CreERT2 transgene and is specific for the gastric epithelium of the stomach71.
gp130FF mice used in the PLX-treatment experiment were propagated on a C57B6 background.
Cohoused, age- and gender-matched littermates were utilized for all experiments. All strains were housed under specific pathogen–free conditions.
Human gastric cancer tissue
Human gastric cancer tissue micro arrays (TMA) were used to identify toluidine blue-stained mast cells in gastric disease. TMA were established previously72. In short, formalin-fixed paraffin-embedded gastric tissue samples we selected, pathology was confirmed by independent pathology review and 0.6 mm punches were reembedded to generate the TMA. Usage of human gastric cancer tissues was approved by the Peter MacCullum Cancer Center Ethics Committee and informed consent was obtained from all subjects.
Inhibitors and treatment regimes
Cromolyn sodium salt (referred to as cromolyn; Sigma–Aldrich, Cat# C0399) is a clinically approved mast cell-degranulation inhibitor73. Cromolyn was dissolved in phosphate buffered saline (PBS) and administered at a concentration of 75 mg/kg body weight via the intraperitoneal route (100 µl) three times per week for 6 consecutive weeks. Control cohorts received PBS.
Clodronate, formulated as liposome-loaded clodrosomes (containing 5 mg clodronate per 1 ml of clodrosome suspension), was injected intraperitoneal as 50 µl clodrosomes suspension twice per week for 6 consecutive weeks. Liposomes containing suspension was injected as placebo in control mice.
The csf1r/c-kit/Flt3-specific inhibitor PLX3397 (Plexxicon), supplied at 800 mg PLX3397 per kg of chow, was given to mice for 4 consecutive weeks represents an estimated dose of 100 mg per kg body weight daily. Vehicle cohorts received unmanipulated chow. For the follow-up cohorts, mice were kept for 4 weeks on unmanipulated chow following their 4-week-treatment period.
Tissue preparation and processing
Tumors and adjacent antral tissues were resected and weighed and then snap-frozen for RNA or protein isolation. Entire stomachs were removed and fixed in 10% neutral buffer formalin for histological analysis39.
Histological and immunohistochemical analysis
Hematoxylin-Eosin, toluidine blue, Alcian blue, Safranin O, and May-Grünwald-Giemsa staining of formalin-fixed paraffin-embedded stomach slides were performed according to theory and practice of histological technique from JD Bancroft74.
For in vivo assessment of proliferation by anti-BrdU staining, tissues were collected 2 h after i.p. injection of 50 mg/kg BrdU (Amersham Biosciences, GE Healthcare). Stainings for apoptosis (Cell Death Detection Kit, Roche) and tissue hypoxia (60 mg/kg HP1 i.p. injection 30 min prior to tissue collection, detection with Hypoxyprobe-1 Kit, from Hypoxyprobe Inc., USA) were performed according to manufacturers’ instructions.
All other immunostaining procedures were conducted as follows. For antigen-retrieval, paraffin-embedded sections were either heated in citrate buffer in a microwave pressure cooker (pH 6 for 15 min) or were incubated in 0.1% trypsin, 3% acetic acid solution at 37° for 10 min. Sections were then blocked in 10% (v/v) normal goat serum for 1 h at room temperature. Primary antibodies were diluted in 10% (v/v) normal goat serum and incubated overnight at 4 oC in a humidified chamber. Biotin-labeled secondary antibodies from the Avidin Biotin Complex ABC-kit (Vector Laboratories) were used according to the manufacturer’s instructions. Visualization was achieved using 3,3-Diaminobenzine (DAB, DAKO). Images were generated with Aperio ImageScope v11.2.0.780 software. Primary antibodies used: rabbit anti-mouse CD31 (1:200 dilution, Abcam, Cat# 28364, RRID: AB_726362), rat anti-mouse F4/80 (1:200 dilution, Abcam, Cat# 6640, RRID: AB_1140040), rat anti-mouse B220 (1:200 dilution, BD Biosciences, Cat# 550286, RRID:AB_393581), rabbit anti-mouse CD3 (1:200 dilution, Abcam, Cat# ab5690, RRID:AB_305055), rat anti-mouse CD8 (1:150 dilution, eBioscience, Cat# 14–0808–82, RRID: AB_2572861), and rat anti-mouse Foxp3 (1:100 dilution, eBioscience, Cat# 12–5773–80, RRID: AB_465935).
Immunofluorescence staining
Paraffin-embedded stomach sections were dewaxed, rehydrated and antigen-retrieval was performed by heating in EDTA buffer (pH9) for 15 min in microwave pressure cooker. Section were incubated for 1 h at room temperature with goat anti-mouse IL-33 (1:150 dilution, R&D Systems, Cat# AF3626, RRID:AB_884269) and then for 1 h with AlexaFluor 568-conjugated donkey anti-goat secondary antibody (Molecular Probes Cat# A-11057, RRID:AB_142581). After counter staining with spectral DAPI (1:200 dilution, PerkinElmer, Cat# FP1490) for 5 min, sections were mounted with Vectashield mounting solution (VECTORlabs, Cat# H-1400). Imaging was preformed with a Vectra 3.0 Automated Quantitative Pathology Imaging System (PerkinElmer, Cat# CLS142338) and representative images were produced using PhenochartTM v1.0.4 software (PerkinElmer).
Quantification
For quantification of mast cell numbers at least three fields of view (10x ocular) of three toluidine blue section per mouse were counted, submucosal area was measured and data represented as mast cells number/area tissue. Similarly, for quantification of CD3, BrdU, and ApopTag staining, either entire tumors or three fields of view of three sections were counted and analyzed comparing to tissue area.
F4/80, CD31, B220, and Hypoxia immune-staining was quantified using Metamorph software (Molecular Devices) or Fiji scripts (ImageJ, htps://Fiji.sc/) determining percentage positive area per area tissue.
Isolation of gastric epithelial cells, immune cells, and flow cytometric analysis
Glandular stomachs or antral tumors were dissected, cut into very small pieces and incubated at 37 °C for 30 min in Ca2+- and Mg2+-free HBSS medium plus 2.5% FCS and 1 mM EDTA with gentle shaking. Then samples were vortexed for 30 s and the supernatants containing intraepithelial lymphocytes were separated from the tissue fragments and kept on ice. The remaining tissue samples were further digested in Collagenase/Dispase (Roche) and DNase I (Roche) in Ca2+- and Mg2+-free HBSS medium plus 2% FCS for 45 min at 37 °C under continuous rotation. Samples were vortexed for 30 s once during incubation and once after the incubation. Afterwards, cell suspensions from both incubations were pooled, filtered and washed in PBS plus 5% FCS for analysis by flow cytometry.
Single cell suspensions were stained for cell surface markers (listed below) and cell viability was controlled with propidium iodide (ThermoFisher Scientific, Cat# P3566) or SYTOXBlue (ThermoFisher Scientific, Cat# S34857) staining. Cell sorting was performed with an Aria II cell sorter (BD Bioscience). All cell-type specific flow cytometric gating strategies are presented as a supplementary figure (Supplementary Fig. 8a–e). Mast cells sorting: from CD45+EpCam− cell population the CD11b− cells were selected, then finally the c-Kit+FceRI+ population represents the mast cells. Macrophage sorting: from CD45+EpCam− cells, the F4/80HighCD11b+ population was selected and back-gated to confirm that the selected macrophage population was Ly6C−Ly6G−.
The following fluorochrome-conjugated antibodies were used for flow cytometric cell sorting and analysis: CD16/CD32 (1/100 dilution, clone 93, Cat# 14-0161-86), EpCAM-FITC (1/400 dilution, clone 9CA,Cat# 11-5791-82), Ly6c-eF450 (1/300 dilution, HK1.4, Cat# 48-5932-82), F4/80-PE-Cy7 (1/400 dilution, BM8, Cat# 25-4801-82), St2-PerCP-eFluor710 (1:200 dilution, clone RMST2-2, Cat# 46-9335-82), Foxp3-PE (1/200 dilution, clone FJK-165, Cat# 12-5773-82), Gata3-PE (1/200 dilution, clone TWAJ, Cat# 12-9966-42), FceR1-PE-Cy7 (1/300, clone 36951, Cat# 25-5898-82), and CD3-PE-Cy7 (1/1000, 145-2C11, Cat# 25-0031-82) all from Ebioscience; CD11b-PE (1/400 dilution, M1/70, Cat# 553311), Ly6g (1/300 dilution, 1A8, Cat# 560602) from BD Pharmingen and CD45.2-A700 (1/400 dilution, clone S450-15-2), CD4 (1/50 dilution, clone GK 1.5), CD11b-PB (1/400 dilution, M1/70), and c-Kit-APC (1/200, ACK-2) from WEHI monoclonal antibody facility.
Isolation and stimulation of BMDM
Bone marrow was collected from the femur and tibia of mice by flushing with sterile PBS. Cells were washed with PBS twice and were filtered through a 100 mm sieve. Resulting cell suspensions were cultured in DMEM supplemented with 10% (v/v) FCS and L929 conditioned medium for 7 days with fresh media changes every second day until fully differentiated into BMDM. After reseeding of cells, alternative macrophage polarization was conducted by stimulation with IL-4 (20 ng/ml, Preprotech) and IL-13 (20 ng/ml, Preprotech) for one day.
Cytokine bead array
A total of 50,000 isolated gastric gp130FF mast cells were cultured in 96-well plates for 3 h in 30 ng/mL IL-33. Supernatants were collected, diluted 1:2 in assay buffer and assayed for cytokine concentration using the Bio-Rad Bioplex cytokine bead assay (Bio-Rad Mouse 23-Plex Panel M60009RDPD) strictly according to manufacturer’s instructions.
BMMC adaptive transfer assay
Mast cells were generated from bone marrow from either gp130FF; ST2+/+ or gp130FF; ST2−/− mice. Bone marrow was extracted and cells were maintained in IL-3-containing culture medium for several weeks until >95% pure BMMC cultures were established. Purity of BMMCs (FceR1+, c-Kit+) was determined via flow cytometry. For the BMMC transplantation assay, syngeneic BMMC from the same colony as the host mice were used. Either gp130FF; ST2+/+ or gp130FF; ST2−/− BMMCs were injected into the tail vein of gp130FF; ST2−/− mice. Each mouse received 107 BMMC at 5, 8, and 11 weeks of age and final tumor analysis was performed at 14 weeks of age.
Gastric organoid assay
Antral tumors from gp130FF mice were used to establish tumor-epithelial organoids. Organoids were established and maintained in IntestiCultTM Organoid Growth Medium (StemCell Technologies) according to manufacturer's protocols. Established organoids were stimulated with 100 ng/ml IL-11 or PBS control for 4 h and then processed for gene expression analysis via qPCR. For assessment of organoid growth, PBS or IL-11 stimulated organoids were monitored over 4 days.
RNA isolation and quantitative RT-PCR
Total RNA was extracted from frozen tissue samples using Trizol®Reagent (life technologies, Cat# 15596026) and cDNA was prepared from 2 µg RNA using the High capacity cDNA Reverse Transcription kit (Applied Biosystems, Cat# 4368813) according to the manufacturer’s protocol.
From isolated gastric mast cells and from FACS sorted macrophages, RNA was extracted using the RNeasy Plus Micro Kit (QIAGEN, Cat# 74034) and cDNA synthesis was performed with the ThermoScriptTM RT-PCR System (Invitrogen, Cat# 11146-024) according to the manufacturer’s instructions.
Quantitative RT-PCR analyses were performed in technical triplicates with SensiMix SYBR kit (Bioline, Cat# QT605–20) using the ViiA™ 7 Real Time PCR System (life technologies). Further details and the sequences of the used oligonucleotides are described in the supplementary methods and Supplementary Table S1.
Kaplan–Meier survival analysis
All Kaplan–Meier survival analysis was performed with KMplot (KMplot.com)53. Data from 179 intestinal-type gastric cancer patient were analyzed and following settings were applied: probes = all probe sets, Laurens classification = intestinal-type, Data sets included: GSE14210, GSE15459, GSE22377, GSE29272, and GSE51105, but excluding GSE62254 (as recommended; due to markedly different survival and shifted expression compared to the other data sets). All other settings were kept as default.
Statistics
Unless otherwise stated, data are presented as mean values ± standard error of the mean (M ± SEM). Exact n values are depicted for every data set in the figure legends and they are always true biological replicates, not technical replicates. All data sets were tested for normality with Shapiro–Wilk normality test. Comparisons between two mean values were performed by two-tailed unpaired Student’s t-test using Prism6 software (GraphPad Software, California, USA). When data sets had significantly different standard deviations according to Prism’s F-test of variances, Welch correction was applied. T-test t values and corresponding degree of freedom (df) are given in figure legends. For comparisons of more than two groups one-way ANOVA test was performed with multiple comparison correction (either Tukey or Bonferroni). ANOVA F values are depicted in each figure legend as F (DFn, Dfd), where DFn is the df nominator and Dfd the df denominator. P values of less than 0.05 were considered statistically significant.
Sample size determination
G*power3.1 software was used to estimate the minimal required sample sizes. Based on previous mean values and SD from previous studies using the gp130FF mouse model, we calculated a minimal sample size for eight mice per group, when the mean difference is 40% and the SD 20% (unpaired two-tailed t-test; α = 0.05, Power = 0.95). Due to difference in availability and frequency of target genotypes born, the number of mice analyzed between cohorts differed. Sample size for subsequent analysis of tissue section staining was limited to number available, as tissues were required for several downstream processes including FACS analysis, RNA and protein expression in addition to histological and immunohistochemical analysis.
Randomization
No formal randomization procedure was performed. However, for genetic mouse experiments, littermates were used to compare different target genotype mice. For in vivo treatment experiments, different treatment groups were equally distributed between mouse litters and mouse cages as well as female and male ratio were kept at 1:1.
Data exclusion
No data was excluded after commencement of quantification. In a few cases, tissue slides were excluded from downstream analysis due to strong background staining or absence of tumor tissue. These slides were excluded from analysis before commencement of quantification and without knowledge of genotypes/treatment details (aka blinded).
Blinding
Assessors were blinded for determining tumor masses and numbers and for quantification of histo- and immunohistochemical staining. Blinding was achieved through labeling minimized to mouse IDs. Genotypes and treatment were only linked back to the mouse ID after completion of quantification.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Acknowledgements
We thank the animal facility staff of La Trobe University and the Ludwig Institute for Cancer Research as well as the Austin and WEHI histology department for technical assistance. We also acknowledge the excellent support for cell sorting by David Baloyan (ONJCRI) and image generation and analysis by Cameron Nowell (Monash University) and Lachlan Whitehead (WEHI). This work was supported through the Victorian State Government Operational Infrastructure Support, the Nation Health and Medical Research Council (NHMRC) of Australia grants 1092788, 1067244, 1069024 and Cancer Council Victoria’s Grant-in-Aid 1160708. M.E. is a NHMRC Principal Research Fellow and also received funding from Ludwig Cancer Research.
Author contributions
Experimental work: M.F.E., A.J., M.B., R.J.J.O’D., T.P., C.D., J.B., S.T., E.T., N.D.H., N.E., A.R.P., and F.M. Data interpretation: M.F.E, A.J., M.B., R.J.J.O’D., A.B., M.L.H., M.A.G., F.M., and M.E. Writing and editing of manuscript: M.F.E., M.L.H., F.M., and M.E. Study concept: M.F.E., A.J., F.M., and M.E. Funding: M.E.
Data availability
The Stat3 chromatin immunoprecipitation-sequencing (ChIP-Seq) data have been deposited in the NCBI gene expression omnibus (GEO) under the accession code GSE48285. The source data underlying Figs. 1b, d, 2b–h, 3b–e, 4b–e, 5a–c, 6a, c, d, f, 7a–g, and 8a and Supplementary Figs 1b, 2a, b, g, i, 3d, 5a, b, g, h, and 6e, f are provided as a source data file. All the other data supporting the findings of this study are available within the article and its supplementary information files and from the corresponding author upon reasonable request. A reporting summary for this article is available as a Supplementary Information file.
Competing interests
The authors declare no competing interests.
Footnotes
Peer review information: Nature Communications thanks Jean Marshall and other anonymous reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information accompanies this paper at 10.1038/s41467-019-10676-1.
References
- 1.Joyce JA. Therapeutic targeting of the tumor microenvironment. Cancer Cell. 2005;7:513–520. doi: 10.1016/j.ccr.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 2.Fridman WH, Pagès F, Sautès-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nat. Rev. Cancer. 2012;12:298–306. doi: 10.1038/nrc3245. [DOI] [PubMed] [Google Scholar]
- 3.Qian B-Z, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39–51. doi: 10.1016/j.cell.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galli SJ, Nakae S, Tsai M. Mast cells in the development of adaptive immune responses. Nat. Immunol. 2005;6:135–142. doi: 10.1038/ni1158. [DOI] [PubMed] [Google Scholar]
- 5.Blank U, Rivera J. The ins and outs of IgE-dependent mast-cell exocytosis. Trends Immunol. 2004;25:266–273. doi: 10.1016/j.it.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Galli SJ, Grimbaldeston M, Tsai M. Immunomodulatory mast cells: negative, as well as positive, regulators of innate and acquired immunity. Nat. Rev. Immunol. 2008;8:478–486. doi: 10.1038/nri2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ribatti D, et al. Tumor vascularity and tryptase-positive mast cells correlate with a poor prognosis in melanoma. Eur. J. Clin. Investig. 2003;33:420–425. doi: 10.1046/j.1365-2362.2003.01152.x. [DOI] [PubMed] [Google Scholar]
- 8.Nonomura N, et al. Decreased number of mast cells infiltrating into needle biopsy specimens leads to a better prognosis of prostate cancer. Br. J. Cancer. 2007;97:952–956. doi: 10.1038/sj.bjc.6603962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strouch MJ, et al. Crosstalk between mast cells and pancreatic cancer cells contributes to pancreatic tumor progression. Clin. Cancer Res. 2010;16:2257. doi: 10.1158/1078-0432.CCR-09-1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elpek G, et al. The prognostic relevance of angiogenesis and mast cells in squamous cell carcinoma of the oesophagus. J. Clin. Pathol. 2001;54:940–944. doi: 10.1136/jcp.54.12.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ribatti D, et al. Mast cells and angiogenesis in gastric carcinoma. Int. J. Exp. Pathol. 2010;91:350–356. doi: 10.1111/j.1365-2613.2010.00714.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yano H, et al. Mast cell infiltration around gastric cancer cells correlates with tumor angiogenesis and metastasis. Gastric Cancer. 1999;2:26–32. doi: 10.1007/s101200050017. [DOI] [PubMed] [Google Scholar]
- 13.Theoharides TC. Mast cells and pancreatic cancer. N. Engl. J. Med. 2008;358:1860–1861. doi: 10.1056/NEJMcibr0801519. [DOI] [PubMed] [Google Scholar]
- 14.Nielsen HJ, et al. Independent prognostic value of eosinophil and mast cell infiltration in colorectal cancer tissue. J. Pathol. 1999;189:487–495. doi: 10.1002/(SICI)1096-9896(199912)189:4<487::AID-PATH484>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 15.Rajput AB, et al. Stromal mast cells in invasive breast cancer are a marker of favourable prognosis: a study of 4,444 cases. Breast Cancer Res. Treat. 2008;107:249–257. doi: 10.1007/s10549-007-9546-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soucek L, et al. Mast cells are required for angiogenesis and macroscopic expansion of Myc-induced pancreatic islet tumors. Nat. Med. 2007;13:1211–1218. doi: 10.1038/nm1649. [DOI] [PubMed] [Google Scholar]
- 17.Schonhuber N, et al. A next-generation dual-recombinase system for time- and host-specific targeting of pancreatic cancer. Nat. Med. 2014;20:1340–1347. doi: 10.1038/nm.3646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lüthi AU, et al. Suppression of interleukin-33 bioactivity through proteolysis by apoptotic caspases. Immunity. 2009;31:84–98. doi: 10.1016/j.immuni.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 19.Rickard JA, et al. RIPK1 regulates RIPK3-MLKL-driven systemic inflammation and emergency hematopoiesis. Cell. 2014;157:1175–1188. doi: 10.1016/j.cell.2014.04.019. [DOI] [PubMed] [Google Scholar]
- 20.Martin NT, Martin MU. Interleukin 33 is a guardian of barriers and a local alarmin. Nat. Immunol. 2016;17:122–131. doi: 10.1038/ni.3370. [DOI] [PubMed] [Google Scholar]
- 21.Nile CJ, Barksby E, Jitprasertwong P, Preshaw PM, Taylor JJ. Expression and regulation of interleukin-33 in human monocytes. Immunology. 2010;130:172–180. doi: 10.1111/j.1365-2567.2009.03221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kouzaki H, Iijima K, Kobayashi T, O’Grady SM, Kita H. The danger signal, extracellular ATP, is a sensor for an airborne allergen and triggers IL-33 release and innate Th2-type responses. J. Immunol. 2011;186:4375–4387. doi: 10.4049/jimmunol.1003020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ohno T, et al. Caspase-1, caspase-8, and calpain are dispensable for IL-33 release by macrophages. J. Immunol. 2009;183:7890–7897. doi: 10.4049/jimmunol.0802449. [DOI] [PubMed] [Google Scholar]
- 24.Wang J-X, et al. IL-33/ST2 axis promotes mast cell survival via BCLXL. Proc. Natl Acad. Sci. USA. 2014;111:10281–10286. doi: 10.1073/pnas.1404182111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Licona-Limon P, Kim LK, Palm NW, Flavell RA. TH2, allergy and group 2 innate lymphoid cells. Nat. Immunol. 2013;14:536–542. doi: 10.1038/ni.2617. [DOI] [PubMed] [Google Scholar]
- 26.Schiering C, et al. The alarmin IL-33 promotes regulatory T-cell function in the intestine. Nature. 2014;513:564–568. doi: 10.1038/nature13577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vasanthakumar A, et al. The transcriptional regulators IRF4, BATF and IL-33 orchestrate development and maintenance of adipose tissue-resident regulatory T cells. Nat. Immunol. 2015;16:276–285. doi: 10.1038/ni.3085. [DOI] [PubMed] [Google Scholar]
- 28.Schmitz J, et al. IL-33, an Interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23:479–490. doi: 10.1016/j.immuni.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 29.Molofsky AB, Savage A, Locksley RM. Interleukin-33 in tissue homeostasis, injury and inflammation. Immunity. 2015;42:1005–1019. doi: 10.1016/j.immuni.2015.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gramatzki D, et al. Interleukin-33 in human gliomas: expression and prognostic significance. Oncol. Lett. 2016;12:445–452. doi: 10.3892/ol.2016.4626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tong X, et al. Interleukin-33 predicts poor prognosis and promotes ovarian cancer cell growth and metastasis through regulating ERK and JNK signaling pathways. Mol. Oncol. 2016;10:113–125. doi: 10.1016/j.molonc.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen S-F, et al. The paracrine effect of cancer-associated fibroblast-induced interleukin-33 regulates the invasiveness of head and neck squamous cell carcinoma. J. Pathol. 2013;231:180–189. doi: 10.1002/path.4226. [DOI] [PubMed] [Google Scholar]
- 33.Maywald Rebecca L., Doerner Stephanie K., Pastorelli Luca, De Salvo Carlo, Benton Susan M., Dawson Emily P., Lanza Denise G., Berger Nathan A., Markowitz Sanford D., Lenz Heinz-Josef, Nadeau Joseph H., Pizarro Theresa T., Heaney Jason D. IL-33 activates tumor stroma to promote intestinal polyposis. Proceedings of the National Academy of Sciences. 2015;112(19):E2487–E2496. doi: 10.1073/pnas.1422445112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O’Donnell C, et al. An antitumorigenic role for the IL-33 receptor, ST2L, in colon cancer. Br. J. Cancer. 2016;114:37–43. doi: 10.1038/bjc.2015.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Malik A, et al. IL-33 regulates the IgA-microbiota axis to restrain IL-1α–dependent colitis and tumorigenesis. J. Clin. Investig. 2016;126:4469–4481. doi: 10.1172/JCI88625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eissmann MF, et al. Interleukin 33 signaling restrains sporadic colon cancer in an interferon-gamma dependent manner. Cancer Immunol. Res. 2018;6:409–421. doi: 10.1158/2326-6066.CIR-17-0218. [DOI] [PubMed] [Google Scholar]
- 37.Thiem S, et al. mTORC1 inhibition restricts inflammation-associated gastrointestinal tumorigenesis in mice. J. Clin. Investig. 2013;123:767–781. doi: 10.1172/JCI65086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Putoczki TracyL, et al. Interleukin-11 Is the dominant IL-6 family cytokine during gastrointestinal tumorigenesis and can be targeted therapeutically. Cancer Cell. 2013;24:257–271. doi: 10.1016/j.ccr.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 39.Ernst M, et al. STAT3 and STAT1 mediate IL-11–dependent and inflammation-associated gastric tumorigenesis in gp130 receptor mutant mice. J. Clin. Investig. 2008;118:1727–1738. doi: 10.1172/JCI34944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jenkins BJ, et al. Hyperactivation of Stat3 in gp130 mutant mice promotes gastric hyperproliferation and desensitizes TGF-beta signaling. Nat. Med. 2005;11:845–852. doi: 10.1038/nm1282. [DOI] [PubMed] [Google Scholar]
- 41.Grimbaldeston MA, et al. Mast cell-deficient W-sash c-kit Mutant KitW-sh/W-sh mice as a model for investigating mast cell biology in vivo. Am. J. Pathol. 2005;167:835–848. doi: 10.1016/S0002-9440(10)62055-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wolters PJ, et al. Tissue-selective mast cell reconstitution and differential lung gene expression in mast cell-deficient KitW-sh/KitW-sh sash mice. Clin. Exp. Allergy. 2005;35:82–88. doi: 10.1111/j.1365-2222.2005.02136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duttlinger R, et al. W-sash affects positive and negative elements controlling c-kit expression: ectopic c-kit expression at sites of kit-ligand expression affects melanogenesis. Development. 1993;118:705. doi: 10.1242/dev.118.3.705. [DOI] [PubMed] [Google Scholar]
- 44.Lilla JN, et al. Reduced mast cell and basophil numbers and function in Cpa3-Cre; Mcl-1fl/fl mice. Blood. 2011;118:6930–6938. doi: 10.1182/blood-2011-03-343962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Traum D, et al. IL-10-induced gp130 expression in mouse mast cells permits IL-6 trans-signaling. J. Leukoc. Biol. 2012;91:427–435. doi: 10.1189/jlb.0411209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gyotoku E, et al. The Il-6 family cytokines, interleukin-6, interleukin-11, oncostatin M, and leukemia inhibitory factor, enhance mast cell growth through fibroblast-dependent pathway in mice. Arch. Dermatol. Res. 2001;203:508–514. doi: 10.1007/PL00007465. [DOI] [PubMed] [Google Scholar]
- 47.Li X, et al. Targeting of tumour-infiltrating macrophages via CCL2/CCR2 signalling as a therapeutic strategy against hepatocellular carcinoma. Gut. 2017;66:157–167. doi: 10.1136/gutjnl-2015-310514. [DOI] [PubMed] [Google Scholar]
- 48.Ries CH, et al. Targeting tumor-associated macrophages with anti-CSF-1R antibody reveals a strategy for cancer therapy. Cancer Cell. 2014;25:846–859. doi: 10.1016/j.ccr.2014.05.016. [DOI] [PubMed] [Google Scholar]
- 49.Komai-Koma M, et al. Interleukin-33 amplifies IgE synthesis and triggers mast cell degranulation via interleukin-4 in naïve mice. Allergy. 2012;67:1118–1126. doi: 10.1111/j.1398-9995.2012.02859.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Belo AV, et al. Murine chemokine CXCL2/KC is a surrogate marker for angiogenic activity in the inflammatory granulation tissue. Microcirculation. 2005;12:597–606. doi: 10.1080/10739680500253535. [DOI] [PubMed] [Google Scholar]
- 51.Michalec L, et al. CCL7 and CXCL10 orchestrate oxidative stress-induced neutrophilic lung inflammation. J. Immunol. 2002;168:846. doi: 10.4049/jimmunol.168.2.846. [DOI] [PubMed] [Google Scholar]
- 52.Amann B, Perabo F, Wirger A, Hugenschmidt H, Schultze-Seemann W. Urinary levels of monocyte chemo-attractant protein-1 correlate with tumour stage and grade in patients with bladder cancer. Br. J. Urol. 1998;82:118–121. doi: 10.1046/j.1464-410x.1998.00675.x. [DOI] [PubMed] [Google Scholar]
- 53.Szász AM, et al. Cross-validation of survival associated biomarkers in gastric cancer using transcriptomic data of 1,065 patients. Oncotarget. 2016;7:49322–49333. doi: 10.18632/oncotarget.10337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhao Y, et al. Increased numbers of gastric-infiltrating mast cells and regulatory T cells are associated with tumor stage in gastric adenocarcinoma patients. Oncol. Lett. 2012;4:755–758. doi: 10.3892/ol.2012.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Engblom C, Pfirschke C, Pittet MJ. The role of myeloid cells in cancer therapies. Nat. Rev. Cancer. 2016;16:447–462. doi: 10.1038/nrc.2016.54. [DOI] [PubMed] [Google Scholar]
- 56.Kanbe N, et al. Human mast cells produce matrix metalloproteinase 9. Eur. J. Immunol. 1999;29:2645–2649. doi: 10.1002/(SICI)1521-4141(199908)29:08<2645::AID-IMMU2645>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 57.Ranieri G, et al. Tryptase-positive mast cells correlate with angiogenesis in early breast cancer patients. Int. J. Oncol. 2009;35:115–120. doi: 10.3892/ijo_00000319. [DOI] [PubMed] [Google Scholar]
- 58.Kondo K, et al. Expression of chymase-positive cells in gastric cancer and its correlation with the angiogenesis. J. Surg. Oncol. 2006;93:36–42. doi: 10.1002/jso.20394. [DOI] [PubMed] [Google Scholar]
- 59.Bot I, et al. Perivascular mast cells promote atherogenesis and induce plaque destabilization in apolipoprotein E–deficient mice. Circulation. 2007;115:2516. doi: 10.1161/CIRCULATIONAHA.106.660472. [DOI] [PubMed] [Google Scholar]
- 60.Rigoni A, et al. Mast cells infiltrating inflamed or transformed gut alternatively sustain mucosal healing or tumor growth. Cancer Res. 2015;75:3760. doi: 10.1158/0008-5472.CAN-14-3767. [DOI] [PubMed] [Google Scholar]
- 61.von Moltke J, Ji M, Liang HE, Locksley RM. Tuft-cell-derived IL-25 regulates an intestinal ILC2-epithelial response circuit. Nature. 2016;529:221–225. doi: 10.1038/nature16161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Petersen Christine P, Meyer Anne R, De Salvo Carlo, Choi Eunyoung, Schlegel Cameron, Petersen Alec, Engevik Amy C, Prasad Nripesh, Levy Shawn E, Peebles R Stokes, Pizarro Theresa T, Goldenring James R. A signalling cascade of IL-33 to IL-13 regulates metaplasia in the mouse stomach. Gut. 2017;67(5):805–817. doi: 10.1136/gutjnl-2016-312779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liew FY, Girard J-P, Turnquist HR. Interleukin-33 in health and disease. Nat. Rev. Immunol. 2016;16:676–689. doi: 10.1038/nri.2016.95. [DOI] [PubMed] [Google Scholar]
- 64.Kobori A, et al. Interleukin-33 expression is specifically enhanced in inflamed mucosa of ulcerative colitis. J. Gastroenterol. 2010;45:999–1007. doi: 10.1007/s00535-010-0245-1. [DOI] [PubMed] [Google Scholar]
- 65.Nishida A, et al. Expression of interleukin 1-like cytokine interleukin 33 and its receptor complex (ST2L and IL1RAcP) in human pancreatic myofibroblasts. Gut. 2010;59:531. doi: 10.1136/gut.2009.193599. [DOI] [PubMed] [Google Scholar]
- 66.Yanagawa Y, Suzuki M, Matsumoto M, Togashi H. Prostaglandin E2 enhances IL-33 production by dendritic cells. Immunol. Lett. 2011;141:55–60. doi: 10.1016/j.imlet.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 67.Suen Y, Chang M, Lee SM, Buzby JS, Cairo MS. Regulation of interleukin-11 protein and mRNA expression in neonatal and adult fibroblasts and endothelial cells. Blood. 1994;84:4125–4134. [PubMed] [Google Scholar]
- 68.Liu X, et al. Intratumor IL-17-positive mast cells are the major source of the IL-17 that is predictive of survival in gastric cancer patients. PLoS One. 2014;9:e106834. doi: 10.1371/journal.pone.0106834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dai X-M, et al. Targeted disruption of the mouse colony-stimulating factor 1 receptor gene results in osteopetrosis, mononuclear phagocyte deficiency, increased primitive progenitor cell frequencies, and reproductive defects. Blood. 2002;99:111. doi: 10.1182/blood.V99.1.111. [DOI] [PubMed] [Google Scholar]
- 70.Hoshino K, et al. The absence of interleukin 1 receptor–related T1/St2 does not affect T helper cell Type 2 development and its effector function. J. Exp. Med. 1999;190:1541. doi: 10.1084/jem.190.10.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Thiem S, et al. Stomach-specific activation of oncogenic KRAS and STAT3-dependent inflammation cooperatively promote gastric tumorigenesis in a preclinical model. Cancer Res. 2016;76:2277–2287. doi: 10.1158/0008-5472.CAN-15-3089. [DOI] [PubMed] [Google Scholar]
- 72.Boussioutas A, et al. Distinctive patterns of gene expression in premalignant gastric mucosa and gastric cancer. Cancer Res. 2003;63:2569–2577. [PubMed] [Google Scholar]
- 73.Thompson PJ, Hanson JM, Morley J. Asthma, mast cells, and sodium cromoglycate. Lancet. 1983;322:848–849. doi: 10.1016/S0140-6736(83)90761-4. [DOI] [PubMed] [Google Scholar]
- 74.Bancroft, J. D. & Alan, S. Theory and practice of histological techniques. 3rd edn, (Churchill Liningstone Elsevier, New York, 1990).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The Stat3 chromatin immunoprecipitation-sequencing (ChIP-Seq) data have been deposited in the NCBI gene expression omnibus (GEO) under the accession code GSE48285. The source data underlying Figs. 1b, d, 2b–h, 3b–e, 4b–e, 5a–c, 6a, c, d, f, 7a–g, and 8a and Supplementary Figs 1b, 2a, b, g, i, 3d, 5a, b, g, h, and 6e, f are provided as a source data file. All the other data supporting the findings of this study are available within the article and its supplementary information files and from the corresponding author upon reasonable request. A reporting summary for this article is available as a Supplementary Information file.