Abstract
Vaccine trials and cohort studies in Plasmodium falciparum endemic areas indicate that naturally-acquired and vaccine-induced antibodies to merozoite surface protein 2 (MSP2) are associated with resistance to malaria. These data indicate that PfMSP2 has significant potential as a component of a multi-antigen malaria vaccine. To overcome challenges encountered with subunit malaria vaccines, we established that the use of highly immunogenic rPfMSP8 as a carrier protein for leading vaccine candidates rPfMSP119 and rPfs25 facilitated antigen production, minimized antigenic competition and enhanced induction of functional antibodies. We applied this strategy to optimize a rPfMSP2 (3D7)-based subunit vaccine by producing unfused rPfMSP2 or chimeric rPfMSP2/8 in Escherichia coli. rPfMSP2 formed fibrils, which induced splenocyte proliferation in an antigen receptor-independent, TLR2-dependent manner. However, fusion to rPfMSP8 prevented rPfMSP2 amyloid-like fibril formation. Immunization of rabbits elicited high-titer anti-PfMSP2 antibodies that recognized rPfMSP2 of the 3D7 and FC27 alleles, as well as native PfMSP2. Competition assays revealed a difference in the specificity of antibodies induced by the two rPfMSP2-based vaccines, with evidence of epitope masking by rPfMSP2-associated fibrils. Rabbit anti-PfMSP2/8 was superior to rPfMSP2-elicited antibody at opsonizing P. falciparum merozoites for phagocytosis. These data establish rPfMSP8 as an effective carrier for a PfMSP2-based subunit malaria vaccine.
Subject terms: Malaria, Parasite host response
Introduction
Throughout the past several years, great progress has been made towards the goal of malaria elimination and eventual eradication with the widespread implementation of a number of control strategies1. The distribution and use of insecticide treated bednets, indoor spraying of residual insecticides, rapid diagnosis and treatment of mild malaria and intermittent preventative treatment of vulnerable populations have all contributed to the global reduction in malaria. However, data from the most recent World Malaria Report indicate that the preceding decline in clinical cases of malaria and malaria-related deaths is beginning to level off in most regions and is even showing signs of reversal in others. These data are concerning and are likely a result of increases in drug-resistant parasites and insecticide-resistant mosquitoes, along with the challenge of sustaining multiple control programs in endemic areas1. Considering the immunogenicity and efficacy data from a recent phase 3 clinical trial of RTS,S, the most advanced subunit malaria vaccine candidate, it seems unlikely that deployment of this vaccine will dramatically shift these trends2–5.
Natural immunity to malaria is acquired over time following repeated exposure to the many antigens of multiple strains of Plasmodium falciparum blood-stage parasites6. Protection has been associated with antibody responses primarily targeting polymorphic, parasite-encoded erythrocyte membrane proteins and multiple antigens of invasive merozoites7–9. A few of these antigens have emerged as potential vaccine candidates10. In general, success with merozoite antigen-based vaccines has been limited due to the structural complexity of these antigens leading to difficulties in production, antigen polymorphism and the allele-specificity of protective responses, low immunogenicity and ultimately insufficient vaccine efficacy11,12. Approaches to overcome these challenges have focused on the identification of new targets, novel vaccine delivery platforms and adjuvants, as well as modification of dose and schedule of vaccine administration11,13,14. As most subunit vaccine candidates have been tested as single antigen formulations, concurrent immunization with multiple target antigens and/or multiple alleles of those antigens affords significant potential to increase overall protective efficacy and durability of vaccine-induced responses.
We have previously demonstrated the utility of P. falciparum MSP8 as a carrier protein for P. falciparum vaccine candidates for overcoming some of the challenges with recombinant antigen production and/or immunogenicity of multi-component formulations15–17. Through genetic fusion of the blood-stage vaccine candidate, PfMSP119, to the N-terminus of the conserved, highly immunogenic PfMSP8, we were able to produce high yields of chimeric rPfMSP1/8 antigen with properly folded EGF-like domains. This chimeric antigen approach prevented antigenic competition and the vaccine elicited high-titer antibodies specific for conformation-dependent, protective epitopes of PfMSP11916. Most significantly, antibodies elicited by immunization of mice, rabbits and non-human primates demonstrated potent activity in the standard in vitro growth inhibition assay16,18.
The strategy to use PfMSP8 as a universal carrier protein was further applied to a leading transmission-blocking candidate, Pfs25, a structurally complex protein notoriously difficult to produce and purify. As compared to rPfs25 alone, we showed that fusion of Pfs25 to the PfMSP8 carrier (rPfs25/8) significantly increased yield and quality of rPfs25, without requiring refolding procedures to achieve proper conformation of its four EGF-like domains. Immunization with chimeric rPfs25/8 induced high titers of antibodies against conformational epitopes of Pfs25 that exhibited potent transmission-reducing activity as measured in the standard membrane feeding assay17. The success with chimeric rPfMSP1/8 and rPfs25/8 vaccines with respect to production, folding, immunogenicity and induction of functional antibodies, prompted us to evaluate PfMSP8 as a fusion partner for another leading blood-stage vaccine candidate, P. falciparum MSP2.
PfMSP2 is a~25 kDa GPI-anchored protein abundantly expressed on the merozoite surface that has a presumed role in erythrocyte invasion and is essential for parasite growth19–23. It is characterized by conserved N- and C-termini flanking highly polymorphic central variable regions (CVR), which can be classified into two major allelic families (3D7 and FC27)24,25. Recombinant PfMSP2 has been characterized as highly disordered, but is known to form amyloid-like fibrils in vitro26–30. The propensity of PfMSP2 to form these fibrillar structures has been linked to the key residues within the conserved N-terminal domain, but the fibril structure and rate of fibril formation may be modulated by CVR elements26,29,31,32. The exact structure of PfMSP2 on the surface of the merozoite is unknown. However, recent evidence suggests that native PfMSP2 may be conformationally constrained on the parasite membrane due to oligomerization30 and/or interaction with lipids33–35.
PfMSP2-specific antibody responses elicited during natural infection have been correlated with acquired immunity in endemic populations, making PfMSP2 an attractive vaccine candidate7,36,37. Furthermore, clinical trials of a PfMSP2-containing multi-component vaccine demonstrated that induced anti-PfMSP2 antibodies contribute to protective efficacy in an allele-specific manner38,39. Naturally-acquired and vaccine-induced anti-PfMSP2 specific antibodies are primarily of the IgG1 and IgG3 isotypes and can function by complement-mediated mechanisms, or by cooperation with Fc receptor-bearing innate immune cells via antibody-dependent cellular inhibition (ADCI) and/or opsonic-phagocytosis40–44. As with other P. falciparum vaccine candidate antigens, success with PfMSP2 vaccines has been limited by challenges linked to antigenic polymorphism, recombinant protein structure and immunogenicity. In an effort to address these challenges, we generated rPfMSP2 and chimeric rPfMSP2/PfMSP8 (rPfMSP2/8) vaccine antigens. Through comparative studies, we evaluated the ability of the PfMSP8 carrier to affect yield, structure and/or immunogenicity of PfMSP2 and the functionality of PfMSP2-specific antibodies.
Results
Design, expression, and purification of unfused rPfMSP2 and chimeric rPfMSP2/8
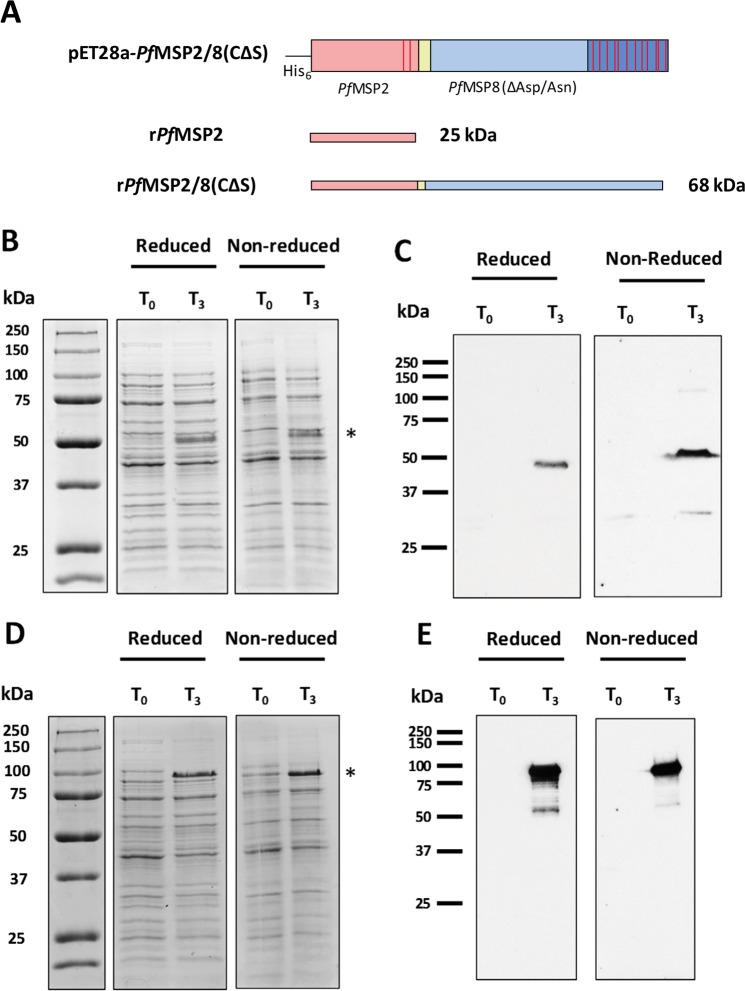
The mature coding sequence of the 3D7 allele of the pfmsp2 gene was codon harmonized for expression in E. coli using previously established algorithms45. The codon harmonized synthetic gene was directionally subcloned into the pET28-MCS-PfMSP8(CΔS) expression vector to facilitate production of two recombinant PfMSP2-based antigens: an unfused rPfMSP2 antigen (25 kDa) and a chimeric rPfMSP2/8 antigen (68 kDa, Fig. 1A). Two stop codons were incorporated 3′ of the PfMSP2 (3D7) coding sequence to generate the unfused construct. Following sequence verification, plasmids were transformed into SHuffle T7 Express lysY E. coli cells for expression. Pre- and post-induction samples of bacterial lysate were assessed for recombinant protein production via SDS-PAGE under reducing and non-reducing conditions. Coomassie Blue staining demonstrated robust protein expression of unfused rPfMSP2 and chimeric rPfMSP2/8 three hours post-induction (T3, Fig. 1B,D). Unfused rPfMSP2 migrated as an ~50 kDa band, well above its predicted molecular weight of 24,721 daltons. This is consistent with previous reports documenting the aberrant migration of PfMSP230, attributed to its lack of hydrophobic residues. Anomalous migration during SDS-PAGE has been observed with several plasmodial proteins with disordered regions, highly charged repeat domains and/or deficits in hydrophobic residues46,47. Likewise, the chimeric rPfMSP2/8 migrated as a corresponding ~100 kDa band, well above its predicted molecular weight of 67,659 daltons. Immunoblot analysis using polyclonal rabbit anti-PfMSP2 sera confirmed the identity of rPfMSP2 and rPfMSP2/8 (Fig. 1C,E).
Figure 1.
Expression of unfused rPfMSP2 and chimeric rPfMSP2/8. (A) Cartoon of expression constructs for rPfMSP2 and rPfMSP2/8 production. Cysteine residues are indicated by red bars, yellow region indicates Gly-Ser linker domain. (B,C) E. coli lysate at time of induction (T0) or 3 hours post-induction (T3) was separated on 10% polyacrylamide gels and rPfMSP2 expression was analyzed by (B) Coomassie Blue staining and (C) immunoblot using anti-PfMSP2 antibody (1:20,000 dilution). (D,E) rPfMSP2/8 expression was analyzed by (D) Coomassie Blue staining and (E) immunoblot as described for rPfMSP2. Asterisks indicate induced rPfMSP2 and rPfMSP2/8 protein products. The T0 samples served as negative controls for the immunoblot analysis of protein expression.
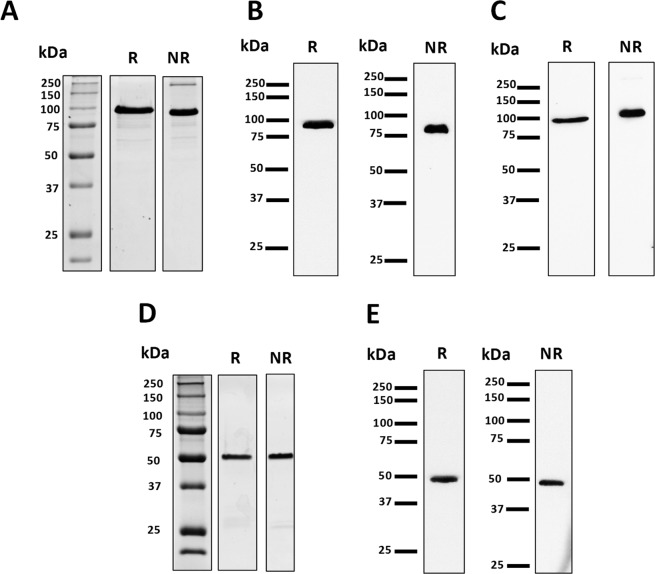
Chimeric rPfMSP2/8 was released from a bacterial inclusion body fraction by treatment with 0.2% sarkosyl and purified by nickel-chelate affinity chromatography under non-denaturing conditions with a final yield of 7.81 mg/g (wet weight) of bacterial cells. Purity was assessed via Coomassie Blue staining of 10% polyacrylamide gels run under reducing and non-reducing conditions, identifying the predominant product migrating at the expected ~100 kDa (Fig. 2A), with only a minor high molecular weight product observed under non-reducing conditions. Immunoblot analysis demonstrated strong reactivity of rPfMSP2/8 with both rabbit anti-PfMSP2 sera and rabbit anti-MSP8 IgG (Fig. 2B,C).
Figure 2.
Purification of recombinant PfMSP2-based antigens. (A–C) Analysis of purified rPfMSP2/8 under reducing (R) and non-reducing (NR) conditions via (A) Coomassie Blue staining (3 μg/lane) or immunoblot (50 ng/lane) using (B) anti-PfMSP2 antibody (1:5,000 dilution) or (C) anti-PfMSP8 IgG (1 μg/ml). (D,E) Purified rPfMSP2 was analyzed by (D) Coomassie Blue staining (3 μg/lane) or (E) immunoblot using anti-PfMSP2 (100 ng/lane) as described for PfMSP2/8.
A similar procedure for lysis and purification was used for unfused rPfMSP2. However, without the PfMSP8 domain, the protein was present in the soluble supernatant following initial lysis. The soluble bacterial lysate was fractionated by ammonium sulfate precipitation prior to purification by nickel-chelate affinity chromatography under non-denaturing conditions. The final yield of unfused rPfMSP2 was 4.22 mg/g (wet weight) of bacterial cells. Coomassie Blue staining of purified product under reducing and non-reducing conditions revealed a single, predominant protein migrating at the expected ~50 kDa (Fig. 2D). Strong reactivity with rabbit anti-PfMSP2 sera was confirmed via immunoblot (Fig. 2E).
rPfMSP2, but not rPfMSP2/8, forms amyloid-like fibrils in vitro which stimulate immune cells via TLR2
It has been established that recombinant PfMSP2 can form amyloid-like fibrils in vitro26,29,48. In an effort to minimize fibril formation, purified rPfMSP2 and chimeric rPfMSP2/8 were stored at −80 °C in buffer containing 0.2% sarkosyl. To evaluate fibrillar content immediately upon thawing, rPfMSP2 and rPfMSP2/8 were analyzed by size exclusion chromatography (SEC). Similar to previous studies30,49, recombinant rPfMSP2 eluted as a prominent monomeric species at 3–4 times its predicted molecular weight. A second heterogeneous mixture of larger oligomeric species of rPfMSP2 was also observed representing 5–10% of the total preparation (Fig. S1). In contrast, SEC analysis of rPfMSP2/8 revealed single prominent monomeric protein (Fig. S1). To further assess the propensity of rPfMSP2-based proteins to form fibrils, and to determine if genetic fusion of rPfMSP2 to rPfMSP8 affects fibril formation, a standard fluorescence-based assay was used. Thioflavin T (ThT), a stain that detects amyloid-like fibrils, was used to assess fibril formation of unfused rPfMSP2, chimeric rPfMSP2/8, or rPfMSP8 carrier alone. Recombinant proteins were diluted in PBS without sarkosyl, prior to ThT staining and incubation at 37 °C for up to 98 hours. As shown in Fig. 3A, staining revealed fibrillar structures present in unfused rPfMSP2 at baseline to a greater extent than in both rPfMSP2/8 or rPfMSP8. Fibril formation of the unfused rPfMSP2 steadily increased during the incubation period, while the structure of chimeric rPfMSP2/8 or rPfMSP8 did not change relative to baseline. To further confirm the formation of amyloid-like fibrils, the assay was conducted in the presence of epigallocatechin-3-gallate (EGCG), an established inhibitor of fibril formation27,28. EGCG disrupted the fibrils present in the initial unfused rPfMSP2 sample and inhibited additional fibril formation over time (Fig. 3A). Consistently, no difference in fibrillar content of rPfMSP2/8 or rPfMSP8 was observed. These data indicate that genetic fusion of rPfMSP2 to rPfMSP8 prevents the amyloid-like fibril formation characteristic of unfused rPfMSP2.
Figure 3.
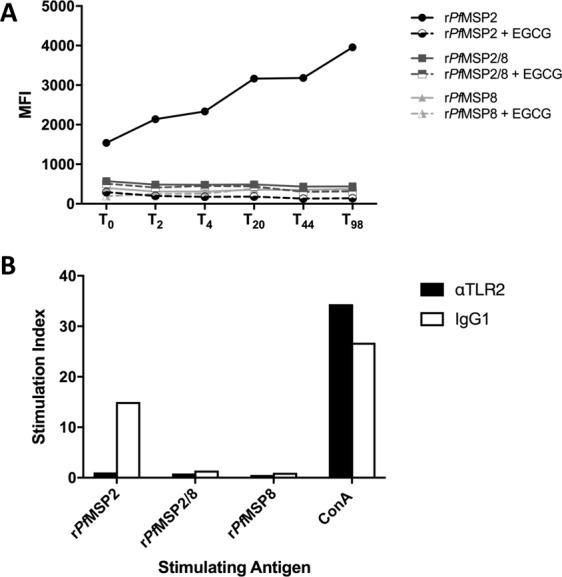
Assessment of fibril formation and stimulation of splenocytes with rPfMSP2 antigens. (A) Recombinant proteins (10 μM) were stained with ThT (30 μM) and incubated at 37 °C. Fluorescence was measured at baseline (T0) prior to incubation and at indicated time points throughout (T2-T98, solid lines). In parallel, EGCG (40 μM) was co-incubated with recombinant proteins to prevent fibril formation and measured as above (dashed lines). Data are presented as the average of duplicate samples. (B) Naïve mouse splenocytes were plated, and triplicate samples were stimulated with recombinant antigen (10 μg/ml) in the presence of 1 μg/ml neutralizing anti-TLR2 mAb (black bars) or an IgG1 isoptype control (white bars). Concanavalin A (ConA, 1 μg/ml) served as positive control. Proliferation was quantitated by [3H]thymidine incorporation, and stimulation index was calculated for each sample relative to unstimulated controls.
Several fibrillar proteins have been shown to stimulate immune cells through TLR2. Therefore, to independently validate the differences in antigen structure determined above, the ability of fibrillar rPfMSP2 versus non-fibrillar rPfMSP2/8 or rPfMSP8 to stimulate the proliferation of naïve mouse splenocytes was measured in vitro. A single cell suspension of splenocytes from a naïve CB6F1/J mouse was stimulated with 10 μg/ml of recombinant antigen in the presence of an anti-TLR2-blocking antibody or isotype control. Concanavalin A (ConA) was used as positive control for proliferation. As shown in Fig. 3B, rPfMSP2 stimulated robust proliferation of splenocytes which was inhibited in the presence of the TLR2-blocking monoclonal antibody. rPfMSP2/8 and rPfMSP8, lacking fibrils, did not stimulate splenocytes to proliferate. Immunophenotyping experiments of naïve mouse splenocytes confirmed that among adaptive immune cell populations with proliferative capacity, B cells were the primary TLR2+ cell population with small populations of TLR2+ cells present among CD4+ and CD8+ T cells. Innate immune cell populations with limited proliferative capacity including dendritic cells, monocytes/macrophages and neutrophils represented only a minor population of TLR2+ splenocytes (data not shown). Together, these data demonstrate that fibrillar rPfMSP2, but not rPfMSP2/8, can stimulate naïve mouse splenocytes in a TLR2-dependent, antigen receptor-independent manner.
Immunization with rPfMSP2-based vaccines elicits high-titer, polyclonal antibody capable of recognizing native P. falciparum antigen
To generate high-titer, polyclonal rabbit sera, New Zealand White rabbits were immunized with unfused rPfMSP2 (n = 4) or chimeric rPfMSP2/8 (n = 4) antigen formulated with Montanide ISA 720, or with adjuvant alone (n = 1). Rabbits received three immunizations with serum samples collected 3 weeks following the primary and secondary immunizations, and with terminal bleed four weeks post tertiary immunization. Antigen-specific antibody titers were measured against each component antigen (rPfMSP2, rPfMSP2/8, or rPfMSP8) by ELISA (Fig. 4). A single immunization with rPfMSP2 or rPfMSP2/8 elicited antibodies that bound to both rPfMSP2- and rPfMSP2/8- coated wells. Additionally, rabbits immunized with chimeric rPfMSP2/8 generated a response against the rPfMSP8 carrier domain, as expected. Following secondary immunization, antigen-specific antibody titers were boosted (anti-PfMSP2 titers, p = 0.04; anti-PfMSP8 titers, p < 0.02) to high levels but titers did not significantly increase further with a third immunization. Rabbits immunized with unfused rPfMSP2 demonstrate low, but detectable, reactivity against rPfMSP8 plate-bound antigen, which is potentially attributable to a shared epitope in a linker domain. Overall, high and comparable PfMSP2-specific antibody titers were generated by immunization with rPfMSP2 and rPfMSP2/8.
Figure 4.
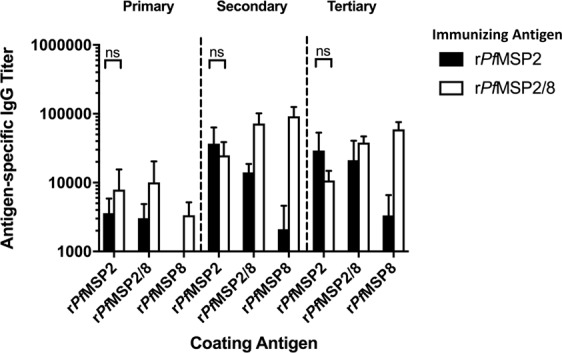
Immunization with rPfMSP2-based vaccines elicits high-titer PfMSP2-specific antibodies. New Zealand White (NZW) rabbits were immunized three times with rPfMSP2 (n = 4, black bars) or rPfMSP2/8 (n = 4, white bars) formulated with Montanide ISA 720. Antigen-specific IgG titers (mean ± SD) following each immunization were analyzed by ELISA. Signal detected by sera from the adjuvant control rabbit (n = 1) was subtracted from individual titers as background (Friedman test with Dunn’s multiple comparisons post hoc test; ns, not significant).
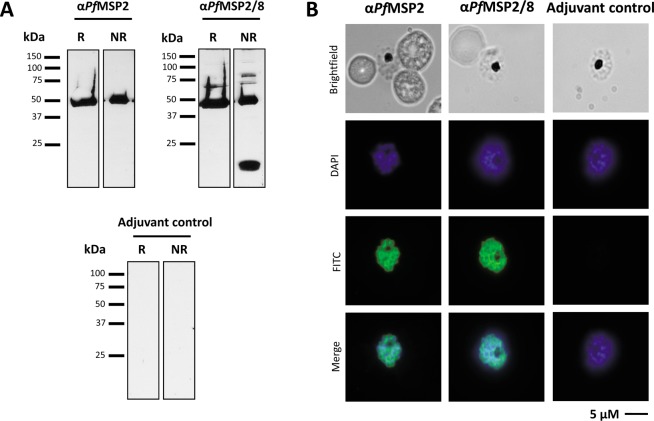
The ability of antisera generated by immunization with rPfMSP2-based vaccines to recognize native parasite protein was assessed via immunoblot and indirect immunofluorescence assay (IFA). A lysate of mixed P. falciparum blood-stage parasites was separated by SDS-PAGE, then blotted and probed with sera from rPfMSP2- or rPfMSP2/8- immunized rabbits, or adjuvant control sera. Strong recognition of parasite-derived PfMSP2 was demonstrated using pooled sera from rPfMSP2- and rPfMSP2/8-immunized animals at the expected ~50 kDa when assessed under reducing and non-reducing conditions. Sera from animals immunized with rPfMSP2/8 also recognized full-length native PfMSP8 (~80 kDa) and the prominent ~17 kDa C-terminal processed product under non-reducing conditions only. As previously reported, anti-rPfMSP8 antibodies are primarily conformation-dependent, directed against epitopes within the double EGF-like domain of its C-terminus15 (Fig. 5A). Immunoreactive proteins were not detected using adjuvant control sera. Pooled sera were also evaluated by indirect IFA of fixed P. falciparum late-stage schizonts. Sera from rabbits immunized with rPfMSP2 and rPfMSP2/8 demonstrated strong recognition of parasite-associated PfMSP2 as noted by clear perimeter staining of the merozoite (Fig. 5B). No signal was detected on slides probed with adjuvant control sera (Fig. 5B, right). These data indicate that immunization with fibrillar rPfMSP2 or non-fibrillar rPfMSP2/8 generates high-titer PfMSP2-specific antibodies that strongly recognize native PfMSP2.
Figure 5.
rPfMSP2 and rPfMSP2/8 vaccines induce antibody that recognizes native P. falciparum antigen. (A) Pools of anti-PfMSP2 and anti-PfMSP2/8 rabbit sera were used to determine recognition of native P. falciparum antigen via immunoblot of parasite lysate. (B) Detection of parasite-associated antigen using pooled sera was determined via indirect immunofluorescence assay of fixed, late-stage schizonts. Adjuvant control sera were also tested in both assays, serving as negative controls (R, reduced; NR, non-reduced).
PfMSP2-based vaccine-induced antibodies recognize 3D7 and FC27 allelic families
To quantitatively assess the levels of allele-specific and cross-reactive antibodies induced by rPfMSP2 (3D7)-based vaccines, recombinant PfMSP2 (FC27) was generated. The mature coding sequence of the FC27 allele of the pfmsp2 gene was codon harmonized for expression in E. coli, synthesized, subcloned and expressed as described above for rPfMSP2 (3D7). During purification, an additional denaturation and glutathione-catalyzed renaturation procedure was necessary to eliminate aggregates of rPfMSP2 (FC27) and promote proper disulfide bond formation. To assess potential differences in cross-reactive antibody populations generated by rPfMSP2 and rPfMSP2/8, antibodies capable of binding rPfMSP2 (3D7) or rPfMSP2 (FC27) were quantified by ELISA. Sera from animals immunized with rPfMSP2 (3D7) were equally reactive with plated-bound rPfMSP2 (3D7) and rPfMSP2 (FC27) with no significant difference in IgG titers (p = 0.20). While immunization with rPfMSP2/8 (3D7) induced antibodies that recognized the two major alleles of PfMSP2, titers against the homologous rPfMSP2 (3D7) were significantly higher than titers against the heterologous rPfMSP2 (FC27) (p < 0.03, Fig. 6). Antibody binding to the shared His6 -tag was minimal as assessed by binding to recombinant P. chabaudi AMA1, an unrelated, but His6 -tagged control antigen. These data suggest that there are differences in the fine-specificity of antibodies elicited by immunization with rPfMSP2 versus rPfMSP2/8.
Figure 6.
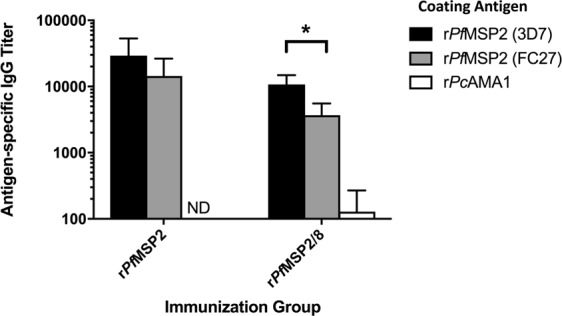
PfMSP2 and PfMSP2/8 vaccines induce rPfMSP2 (3D7)- and rPfMSP2 (FC27)- specific IgG. Antibody titers for rPfMSP2 (3D7) or (FC27) allelic families were determined by ELISA (mean ± SD) using tertiary sera from each rabbit. rPcAMA1-coated wells were used to measure His6-specific IgG. Adjuvant control responses were subtracted from individual titers as background. Asterisk indicates significance (Mann-Whitney U test, p < 0.03).
Differences in antibody populations induced by fibrillar vs non-fibrillar PfMSP2-based vaccine antigens
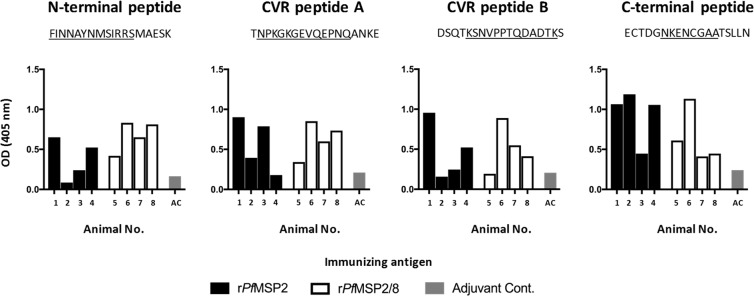
Fusion of rPfMSP2 to rPfMSP2/8 affected the structure of rPfMSP2 by eliminating the propensity for fibrillization (Fig. 3). To begin to assess the impact of such conformational changes on antibody epitope specificity, the reactivity of vaccine-induced antibodies to known B cell epitopes of PfMSP2 was profiled by ELISA. The four PfMSP2 peptides (18-mers) evaluated contained i) the conserved N-terminal region epitope recognized by mAb 6D8, ii) two PfMSP2 (3D7)-specific CVR epitopes recognized by mAb 11E1 and mAb 9D11, respectively, and iii) the conserved C-terminal region epitope recognized by mAb 4D11 and 9G848. As shown in Fig. 7, sera from animals immunized with fibrillar rPfMSP2 recognized the N-terminal epitope and the two CVR epitopes to varying degrees, with stronger recognition of the C-terminal epitope. Sera from animals immunized with non-fibrillar rPfMSP2/8 recognized all four epitopes, but the response was more uniformly distributed across epitopes in comparison to rPfMSP2-induced sera. These data are consistent with a more open conformation of the rPfMSP2 molecule when fused to the rPfMSP8 carrier. Of significance, sera from all four rPfMSP2/8-immunized rabbits recognized the conserved C-terminal epitope, confirming that fusion of PfMSP8 to the C-terminus of PfMSP2 did not alter epitope accessibility near this junction (Fig. 7, right panel).
Figure 7.
rPfMSP2-based vaccines induce antibodies that recognize established mAb epitopes. To determine the impact of antigen conformation on antibodies induced by immunization, PfMSP2 peptides containing established mAb epitopes were used for analysis via ELISA. Sera from individual immunized rabbits (black, white) and control rabbit (grey) were diluted and tested for reactivity with each peptide. Data are presented as the average of duplicate A405 values. Underlined portion of peptide sequence represents mAb epitopes 6D8, 11E1, 9D11 and 4D11/9G8 (left to right).
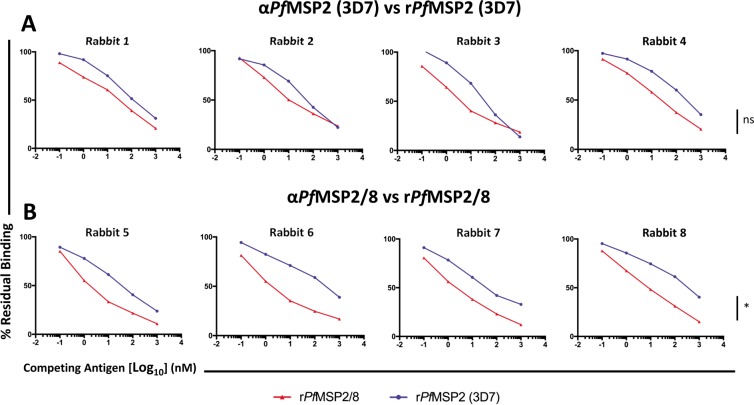
To further evaluate differences in the nature of the PfMSP2-specific epitopes recognized by antibodies induced by immunization with fibrillar rPfMSP2 or non-fibrillar rPfMSP2/8, seroreactivity was evaluated by competition ELISA. The ability of rPfMSP2 (3D7) (fibrillar) and rPfMSP2/8 (non-fibrillar) to inhibit binding of anti-PfMSP2 (3D7) or anti-PfMSP2/8 antibody to plate-bound immunizing antigen was quantified. To eliminate the detection of PfMSP8-specific antibody binding, 1 μM of rPfMSP8 was included in all antibody + inhibitor incubations. At this concentration of rPfMSP8, minimal residual binding was detected against plate-bound PfMSP8.
In the first set of assays, the ability of rPfMSP2 (3D7) or rPfMSP2/8 to inhibit the binding of anti-PfMSP2 (3D7) sera to plate-bound rPfMSP2 (3D7) was tested. rPfMSP2 (3D7) efficiently inhibited a high proportion of the anti-PfMSP2 (3D7) antibody binding with 65–86% inhibition at the highest concentrations of inhibitor (Fig. 8A, blue). Chimeric rPfMSP2/8 was equally as effective at inhibiting anti-PfMSP2 antibody binding to plate-bound PfMSP2 (3D7) with 76–81% inhibition at the highest concentrations (Fig. 8A, red; Table 1, p > 0.48). The second set of assays tested the ability of rPfMSP2 (3D7) or rPfMSP2/8 to inhibit the binding of anti-PfMSP2/8 sera to plate bound rPfMSP2/8. Chimeric rPfMSP2/8 was shown to be a potent inhibitor of anti-PfMSP2/8 antibody binding with 83–90% inhibition at high concentrations of inhibitor (Fig. 8B, red). Comparatively, rPfMSP2 (3D7) inhibited anti-PfMSP2/8 antibody binding to plate-bound rPfMSP2/8 (60–79% inhibition) to a significantly lesser degree than rPfMSP2/8, even at the highest concentrations tested (Fig. 8A, blue; Table 1, p < 0.03). Combined, these data indicate that antibodies generated by immunization with chimeric rPfMSP2/8 consistently recognize a broad range of PfMSP2 epitopes that are displayed on rPfMSP2/8, but are presumably masked on unfused rPfMSP2 due to its fibrillar nature (Table 1).
Figure 8.
rPfMSP2-associated fibrils mask relevant PfMSP2-specific epitopes. Competition ELISAs were conducted using a fixed concentration of rabbit antibody induced by (A) rPfMSP2 or (B) rPfMSP2/8 immunization. Sera were co-incubated in solution with increasing amounts of rPfMSP2 or rPfMSP2/8. Residual binding to plate-bound immunizing antigen for each antigen + antibody cocktail was measured in duplicate by ELISA and calculated as (A405 of IgG with inhibitor/A405 without inhibitor) × 100. Statistical significance was conducted at maximum levels of inhibition. Data from samples within an immunization group were averaged and compared. Asterisk indicates significance (Mann-Whitney U test, p < 0.03; ns, not significant).
Table 1.
Anti-PfMSP2/8 IgG recognizes PfMSP2-specific epitopes masked by rPfMSP2-associated fibrils.
| Rabbit Sera | Inhibitor | Maximum % Inhibition (Mean ± SD) | p value |
|---|---|---|---|
| αPfMSP2 (3D7) | rPfMSP2/8 | 79.1 ± 2.1 | 0.4857 |
| rPfMSP2 (3D7) | 74.4 ± 9.6 | ||
| αPfMSP2/8 | rPfMSP2/8 | 86.3 ± 2.7 | 0.0286 |
| rPfMSP2 (3D7) | 66.0 ± 7.5 |
Functional activity of antibodies induced by immunization with rPfMSP2 versus rPfMSP2/8
The growth inhibition assay (GIA) was used to determine the ability of antibodies induced by immunization with rPfMSP2-based vaccines to inhibit in vitro growth of blood-stage P. falciparum parasites. Purified IgG from each rabbit was tested at a concentration of 2.5 mg/ml and 5.0 mg/ml. At 2.5 mg/ml, there was no detectable growth inhibitory activity in any of the four anti-PfMSP2 IgG samples (Table 2). When the IgG concentration was elevated to 5.0 mg/ml, a low level of growth inhibition was observed in three out of four samples. Similarly, all four anti-PfMSP2/8 IgG samples demonstrated no growth inhibitory activity at 2.5 mg/ml. This remained consistent for three out of four samples when the IgG concentration was raised to 5.0 mg/ml (Table 2). The low and variable growth inhibitory activity for anti-PfMSP2 and anti-PfMSP2/8 samples at high concentration were comparable to adjuvant control background levels. As anticipated, anti-PfMSP1/8 IgG positive control samples demonstrated a high levels of growth inhibition in both assays with ~60% inhibition at 2.5 mg/ml and ~80% inhibition at 5.0 mg/ml. These data show that antibodies induced by immunization with rPfMSP2 or rPfMSP2/8 are not functional in this assay. These data are consistent with previously reported GIA data for naturally-acquired and vaccine-induced PfMSP2-specific antibodies50–52.
Table 2.
In vitro inhibition of P. falciparum (NF54) by rabbit MSP-specific IgG.
| Assay | Rabbit antiserum | % Growth Inhibition | |
|---|---|---|---|
| 2.5 mg/ml | 5 mg/ml | ||
| (animal no.) | IgG | IgG | |
| 1 | PfMSP2 (1) | ND | 15 |
| PfMSP2 (2) | ND | ND | |
| PfMSP2 (3) | ND | 3 | |
| PfMSP2 (4) | ND | 2 | |
| Adjuvant Control | ND | 10 | |
| PfMSP1/8 Control | 58 | 80 | |
| 2 | PfMSP2/8 (5) | ND | ND |
| PfMSP2/8 (6) | ND | ND | |
| PfMSP2/8 (7) | ND | ND | |
| PfMSP2/8 (8) | ND | 19 | |
| Adjuvant Control | 2 | 4 | |
| PfMSP1/8 Control | 61 | 79 | |
ND, not detected.
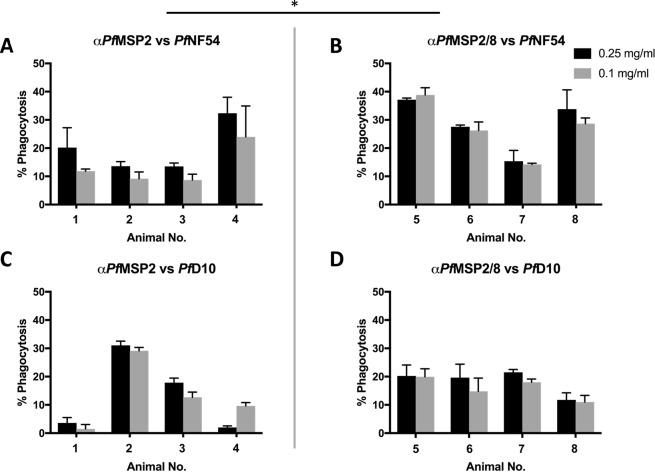
The functionality of PfMSP2-specific antibodies, in cooperation with monocytes/macrophages, has been previously demonstrated using an in vitro opsonophagocytosis assay (OPA)43. To test the opsonizing capacity of anti-PfMSP2 and anti-PfMSP2/8 antibodies, an adapted and optimized OPA was used. Purified IgG from each animal was tested for the ability to opsonize homologous (P. falciparum NF54) and heterologous (P. falciparum D10) merozoites for phagocytosis by THP-1 monocytic cells. Prior to use, the sequence of the msp2 gene of the NF54 and D10 strains of P. falciparum was confirmed to be the 3D7 and FC27 msp2 allelic variants, respectively. As shown in Fig. 9A, phagocytosis of P. falciparum NF54 merozoites opsonized with anti-PfMSP2 IgG at a concentration of 0.1 mg/ml ranged only from 9–24%. A modest increase to 14–32% phagocytosis was observed when the concentration was raised to 0.25 mg/ml. At a concentration of 0.1 mg/ml, opsonization with anti-PfMSP2/8 IgG promoted the efficient phagocytosis of homologous P. falciparum NF54 merozoites (14–39% phagocytosis), a significant increase relative to phagocytosis observed with anti-PfMSP2 IgG at the same concentration of 0.1 mg/ml (p = 0.05). Comparable levels of phagocytosis were observed when the anti-PfMSP2/8 IgG concentration was increased to 0.25 mg/ml (15–37% phagocytosis, Fig. 9B). Assessment of anti-PfMSP8 IgG confirmed that increased phagocytic activity of rPfMSP2/8 IgG was not due to reactivity of anti-PfMSP8 antibodies (Table S1).
Figure 9.
Anti-PfMSP2/8 IgG exhibits enhanced functionality in the opsonophagocytosis assay as compared to anti-PfMSP2. (A,B) The ability of purified (A) PfMSP2 IgG or (B) PfMSP2/8 IgG to enhance phagocytosis of homologous P. falciparum merozoites was measured by OPA at high (0.25 mg/ml, black) and low (0.1 mg/ml, grey) concentrations. (C,D) Parallel assays with (C) PfMSP2 IgG and (D) PfMSP2/8 IgG were performed on heterologous merozoites. Phagocytosis was tested in triplicate and quantified as the percent fluorescent THP-1 following co-incubation with opsonized merozoites (% phagocytosis, mean ± SD). Concentration-matched adjuvant control-opsonized samples were subtracted as background. For statistical analysis, data from individual animals within an immunization group were averaged and compared. Asterisk indicates significance (Mann-Whitney U test, p < 0.05).
To evaluate the cross-strain neutralizing capacity of vaccine-induced antibodies, parallel OPAs were performed with merozoites isolated from the heterologous P. falciparum D10 strain. As shown in Fig. 9C, opsonization of heterologous merozoites with anti-PfMSP2 IgG resulted in variable and generally low levels of phagocytosis (2–13% at 0.1 mg/ml and 4–18% phagocytosis at 0.25 mg/ml). The exception was one anti-PfMSP2 IgG sample that led to ~30% phagocytosis at both concentrations (Fig. 9C). In contrast, opsonization of heterologous merozoites with anti-PfMSP2/8 IgG promoted a modest level of phagocytosis of a concentration of 0.1 mg/ml (11–20%), with comparable levels at 0.25 mg/ml (12–20%, Fig. 9D). Opsonization of heterologous merozoites by anti-PfMSP2 IgG and anti-PfMSP2/8 IgG was not significantly different (p > 0.48). Together, these data showed that anti-PfMSP2/8 IgGs were consistently and potently functional in their capacity to opsonize homologous and heterologous merozoites for phagocytosis by THP-1 cells. In contrast, anti-PfMSP2 IgGs were less potent and more variable in their capacity to enhance phagocytosis of homologous merozoites.
Discussion
We firmly believe that the development of a highly efficacious, multi-stage vaccine will be necessary to achieve the goals of malaria elimination and eradication. We also believe that an essential component of that vaccine will need to target blood-stage malaria parasites. The complexity of the host immune response to merozoites, the low immunogenicity of vaccine candidates, and the limited availability of potent, human-compatible adjuvants, are significant challenges for the vaccine effort. For subunit malaria vaccines, various vaccine platforms, immunization strategies and potential candidate antigens have been evaluated, but progress has been slow. Our lab has focused on the use of a Plasmodium-specific carrier protein, PfMSP8, to enhance production and immunogenicity of leading vaccine antigens15. We have validated this approach with the genetic fusion of PfMSP119 and Pfs25 to the PfMSP8 carrier protein. With chimeric rPfMSP1/8 and rPfs25/8 antigens, overall production and immunogenicity was improved while the conformation of critical protective epitopes and domains was retained. Antibody responses against the PfMSP119 and Pfs25 targeted domains were strong, and the elicited IgGs were highly functional in growth inhibition and standard membrane-feeding assays, respectively16–18. These results provided a clear rationale to evaluate another leading vaccine candidate, PfMSP2, with PfMSP8 as its carrier.
PfMSP2 is an attractive blood-stage vaccine candidate. PfMSP2 elicits an immune response in P. falciparum infected individuals living in endemic areas that has been correlated with protection36,37. This protective antibody response has been characterized as allele-specific, suggesting that the central variable repeat regions are immunodominant in the context of infection48,53. In Phase IIb trials of the Combination B vaccine, anti-MSP2-specific responses contributed to vaccine efficacy38,39. Again, protection was PfMSP2-allele specific suggesting that a successful PfMSP2-containing vaccine may need to include both major alleles. If possible for a PfMSP2-containing vaccine, however, induction of a protective, cross-reactive immune response targeting conserved N- and C- terminal PfMSP2 epitopes with sufficient magnitude and durability would be highly desirable. Results from a recent study analyzing antibodies induced by a bi-allelic MSP2-based vaccine in Phase I trials exemplify this paradigm, demonstrating that co-immunization with both allelic families of PfMSP2 induced cross-reactive, functional antibodies54. As such, recent studies of PfMSP2-based vaccines have focused on partial and/or 3D7-FC27 fusion proteins that exclude portions of the PfMSP2 full-length protein in an effort to simplify production, eliminate fibrillar aggregates and/or enhance the antibody response to conserved B cell epitopes55,56. Some success has been achieved with long synthetic PfMSP2 peptides and with the PfMSP2 3D7-FC27 mosaics, which have demonstrated immunogenicity in mouse studies, as well as reactivity with sera from semi-immune adults living in malaria endemic areas49,57. However, there is inadequate information on the relationship between immunizing antigen and PfMSP2 structure on the surface of the merozoite to adequately justify elimination of selected PfMSP2 domains from vaccine constructs. It is important to keep in mind that although PfMSP2 is characterized as a highly disordered protein, recent evidence indicates that PfMSP2 on the merozoite surface may be conformationally constrained due to oligomerization or interaction with membrane lipids, in addition to the GPI anchor21,33. Additionally, the protective anti-PfMSP2 antibody responses detected in individuals living in endemic areas primarily target readily accessible, allele-specific epitopes36,37.
In this study, we were able to produce chimeric rPfMSP2/8 in high yield using straightforward purification protocols. We used size exclusion chromatography and a fluorescence-based assay to monitor the extent of fibril formation of rPfMSP2/8 versus rPfMSP2. Our results showed that unfused rPfMSP2 formed fibrils, however, upon fusion to the PfMSP8 carrier, rPfMSP2 fibril formation was prevented. Of note, reactivity of PfMSP2 (3D7)-associated fibrils with ThT has not previously been reported. Adda et al. have shown that rPfMSP2 (FC27) fibrils can be detected by ThT fluorescence, but that rPfMSP2 (3D7) fibrils do not bind the dye. The rPfMSP2 (3D7) produced by Adda et al. contained a C-terminal His6 tag while our rPfMSP2 (3D7) was tagged at its N-terminus. As such, the presence or absence of the His-tag at the N-terminus, where fibril formation has been proposed to initiate,26,29,31,32 may have influenced fibril formation and/or ThT binding to some degree. Further evidence of structural differences between rPfMSP2 and rPfMSP2/8 were obtained, as only rPfMSP2 stimulated splenocyte proliferation through TLR2. Binding and signaling through TLR2 has been reported as a characteristic of some fibrillar proteins58,59. It is unclear how TLR2-mediated recognition of fibrillar PfMSP2 impacts infection-induced immune responses elicited by native, parasite-associated PfMSP2 in vivo, but it is of interest and will require further study.
Because of the uncertainty regarding the structure of native PfMSP2 on the surface of the merozoite, we pursued an evaluation of the immune response to fibrillar versus non-fibrillar PfMSP2 in an effort to inform rPfMSP2-based vaccine design. We aimed to determine whether the fibrillar nature of rPfMSP2 skewed the immune response toward the generation of cross-reactive or allele-specific antibodies. Upon examining the ability of rPfMSP2 vaccine-induced antibody to recognize both allelic families of rPfMSP2, we observed no significant difference in antibody titers when assayed via ELISA. However, anti-PfMSP2/8 sera contained significantly higher titers of antibodies that recognized rPfMSP2 (3D7) compared to rPfMSP2 (FC27). It is possible that these results were influenced by the conformation of plate-bound, unfused rPfMSP2 and the accessibility of B cell epitopes.
We determined that fusion of rPfMSP2 to rPfMSP8 carrier affects the conformation of the rPfMSP2 component. This fusion could potentially alter accessibility of relevant B cell epitopes, particularly in the conserved C-terminal region of PfMSP2 near the junction with PfMSP8. However, antibody induced by immunization with rPfMSP2/8 bound to a peptide containing a conserved C-terminal region epitope recognized by mAbs 4D11 and 9G8. These data confirm that this epitope was not altered or blocked by fusion of rPfMSP2 to PfMSP8. With this approach, we also profiled the reactivity to a conserved N-terminal epitope defined by mAb 6D8, and two 3D7-associated CVR epitopes recognized by mAbs 11E1 and 9D11. The results suggest that in contrast to rPfMSP2, immunization with rPfMSP2/8 induced a more balanced antibody response distributed across epitopes throughout rPfMSP2.
Competitive-binding ELISAs provided a unique and effective opportunity to further parse out the potential differences in the fine specificity of rPfMSP2- or rPfMSP2/8- induced antibodies. In this series of competition assays, non-fibrillar antigen in an open and uniform conformation (rPfMSP2/8) or antigen with a mixture of monomeric and fibrillar conformations (rPfMSP2) were used in solution to compete out PfMSP2-specific antibody binding to plate-bound immunizing antigen. These data identified a population of PfMSP2-specific antibodies elicited by rPfMSP2/8 immunization that could not be effectively competed out by homologous fibrillar rPfMSP2. This was only observed in sera from rPfMSP2/8-immunized animals, as both fibrillar and non-fibrillar PfMSP2 efficiently inhibited binding of antibodies elicited by immunization with unfused rPfMSP2. These results suggest that the rPfMSP2/8 vaccine induced an additional population of antibodies that recognized PfMSP2-specific epitopes masked by fibrils formed by the rPfMSP2 antigen. Together, with the results from SEC, ThT fluorescence assays and TLR2-dependent splenocyte proliferation assays (Fig. 3, S1), we have established that rPfMSP2 fibrillar content impacts the display of PfMSP2 epitopes, and that the non-fibrillar conformation of rPfMSP2/8 increases the extent to which PfMSP2 epitopes are accessible.
Vaccine-induced PfMSP2-specific antibodies that are cross-reactive between the two major allelic variants are desirable. However, it is critical that these antibodies are functional in the neutralization and clearance of merozoites. The GIA is an established assay to assess the functionality of antibodies to merozoite antigens. However, analyses of naturally-acquired and vaccine-induced PfMSP2-specific antibodies have inconsistently demonstrated the ability to inhibit parasite growth in this assay. As such, we sought to determine if IgG induced by our PfMSP2-based vaccines demonstrated in vitro growth inhibitory activity. We did not observe any significant growth inhibition by PfMSP2-specific IgG derived from animals immunized with either chimeric rPfMSP2/8 or unfused rPfMSP2 vaccines. These results are consistent with previous studies of both vaccine-induced and naturally-acquired PfMSP2-specific antibodies50–52.
Recent development and use of the opsonophagocytosis assay (OPA) has contributed to the understanding of anti-PfMSP2 antibody functionality and has proven to be a better measure of PfMSP2-dependent immunity than the GIA43. The ability of rabbit IgG (produced as a single isotype) to bind to human Fc receptors on THP-1 cells has previously been exploited for analysis of immunization-induced IgG in the OPA60. Therefore, to measure the functionality of our rabbit anti-PfMSP2 antibodies, we utilized the OPA. Here, we simply report the percent of THP-1 cells containing fluorescent merozoites, allowing direct side-by side comparison of the opsonizing capacity of immunization-induced rabbit IgGs. This is in contrast to Beeson et al., who report relative phagocytic index (RPI) as a percentage of the test antibody activity relative to a positive control43,54,60. We demonstrated that anti-PfMSP2/8 IgG effectively opsonized homologous merozoites (P. falciparum NF54) at both concentrations tested (0.1 and 0.25 mg/ml). Conversely, the functionality of anti-PfMSP2 IgG was significantly lower than that of anti-PfMSP2/8 IgG overall, and more variable between rabbits. Opsonization of heterologous merozoites (P. falciparum D10) and phagocytosis by THP-1 cells was comparable between antibodies elicited by immunization with rPfMSP2 and rPfMSP2/8, as supported by our evaluation of cross-reactive antibody responses (Fig. 6). Combined, the data indicate that antibodies induced by immunization with non-fibrillar, chimeric PfMSP2/8 are able to recognize relevant PfMSP2-specific epitopes that contribute to antibody functionality. Of interest, these PfMSP2/8-induced antibodies were more potently functional against parasites expressing the homologous allele of PfMSP2. Altogether, we conclude that rPfMSP2 and rPfMSP2/8 vaccines induce an equally potent amount of cross-reactive antibody, but that an additional population of PfMSP2-specific antibodies induced by rPfMSP2/8 are allele-specific and functional in the OPA.
There is still more to learn about the structural differences between PfMSP2 on the surface of the merozoite and PfMSP2 in purified, recombinant form. In the meantime, it is essential to evaluate the ability of vaccine-induced PfMSP2-specific antibody not only to recognize parasite-associated antigen, but also to function in a way that facilitates merozoite neutralization. Through fusion to PfMSP8, we have affected the structure and immunogenicity of rPfMSP2 and increased accessibility of neutralizing epitopes on rPfMSP2. We believe this is of significant benefit from a vaccine perspective. While unfused rPfMSP2 is immunogenic, it exists as a mix of fibrillar and non-fibrillar structures that changes with time, temperature, pH, etc. This presents significant challenges for uniform production of a vaccine antigen that can elicit antibody responses of predictable specificity that can be easily measured in conventional immunoassays. These issues are markedly reduced with the chimeric rPfMSP2/8. Our data also suggest that a bi-allelic PfMSP2/8-based vaccine that can induce allele-specific, neutralizing antibodies to both PfMSP2 variants, in addition to cross-strain neutralizing antibodies, may improve overall efficacy. Finally, these PfMSP2 vaccine studies provide further support for the broad application of PfMSP8 as a carrier for subunit malaria vaccine antigens.
Methods
Design and Production of unfused PfMSP2 and chimeric PfMSP2/8
The coding sequences of pfmsp2 (3D7 allele, amino acids 21–248; FC27 allele, amino acids 21–240) were codon harmonized for expression in E. coli as previously described45. SpeI and AflII restriction sites were added to the 5′ and 3′ ends respectively, to facilitate directional cloning. The PfMSP2 (3D7) codon harmonized gene (GenBank Accession # MK450589) and PfMSP2 (FC27) codon harmonized gene (GenBank Accession # MK450590) were commercially synthesized (Blue Heron Biotechnology Inc., Bothell, WA). The synthetic PfMSP2 (3D7) gene was then subcloned into pET28a-MCS-PfMSP8(CΔS)17 for expression of chimeric PfMSP2/8 (3D7). For expression of unfused PfMSP2 (3D7) and PfMSP2 (FC27), two stop codons (TGA, TAA) were incorporated at the 3′ end of the PfMSP2 coding sequences. PfMSP2 sequences were verified (GENEWIZ, South Plainfield, NJ) prior to transformation into SHuffle T7 express lysY competent E. coli cells (New England Biolabs, Ipswich, MA).
Bacteria were grown in enriched media (5 L) using a BioFlo115 Benchtop Bioreactor (New Brunswick Scientific) and recombinant antigens expressed as previously described17. Cells were harvested by centrifugation, washed in phosphate-buffered saline (PBS, pH 7.4) and stored as pellets at −80 °C. Protein expression was assessed by SDS-PAGE on 10% polyacrylamide gels followed by Coomassie Blue staining or immunoblot analysis using polyclonal rabbit antibody specific for PfMSP2. This anti-PfMSP2 serum was obtained through the Malaria Research and Reference Reagent Resource Center as part of the BEI Resources Repository, NIAID, NIH: Plasmodium falciparum Anti-MSP2 Antibodies, MRA-318, deposited by RL Coppel (MR4, BEI Resources, ATCC, Manassas, VA). Bound antibody was detected by horseradish-peroxidase (HRP)-conjugated goat anti-rabbit IgG (0.1 μg/ml; Thermo Fisher Scientific) and SuperSignalTM West Pico chemiluminescent substrate (Thermo Fisher Scientific).
Purification of rPfMSP2/8 and rPfMSP2
To purify rPfMSP2/8, bacterial pellets were lysed using BugBuster HT protein extraction reagent in the presence of recombinant lysozyme and benzonase nuclease (Millipore Sigma, St. Louis, MO). Inclusion bodies were pelleted, washed and solubilized in Binding Buffer (20 mM Tris-HCl, pH 7.9, 0.5 M NaCl, 5 mM imidazole) containing 0.2% sarkosyl (N-lauroylsarcosine, Millipore Sigma) at 4 °C, overnight with rotation. Residual insoluble material was pelleted at 7600 × g, and rPfMSP2/8 was purified from the soluble fraction by nickel-chelate affinity chromatography (Ni-NTA agarose beads; Qiagen, Valencia, CA) under non-denaturing conditions in the presence of 0.2% sarkosyl. A portion of the rPfMSP2/8 that remained in the unbound fraction was reapplied to the Ni-NTA column to maximize yield. The final rPfMSP2/8 product was dialyzed into 25 mM Tris-HCl, pH 8.0, 150 mM NaCl (TBS) containing 0.2% sarkosyl. For purification of rPfMSP2 (3D7 and FC27), bacterial pellets were lysed as above. Following centrifugation, the soluble supernatant containing rPfMSP2 was fractionated by treatment with 20% ammonium sulfate. The resulting supernatant was dialyzed overnight at 4 °C into Binding Buffer +0.2% sarkosyl and rPfMSP2 was purified by two rounds of nickel-chelate affinity chromatography. For rPfMSP2 (FC27), an additional denaturation and glutathione-catalyzed refolding step17 was added to eliminate aggregation in the final product. We have successfully used this protocol to promote proper disulfide bond formation and restore conformational epitopes on several recombinant malarial proteins expressed in E. coli. Protein concentration was determined by bicinchoninic acid (BCA) protein assay (PierceTM, Thermo Fisher Scientific). Purity and conformation were assessed under reducing and non-reducing conditions by SDS-PAGE and immunoblot analysis using anti-PfMSP2 antibody (MRA-318, 1:5,000 dilution) or anti-PfMSP8 IgG (1 μg/ml) as described above. The specificity of the rabbit anti-PfMSP8 IgG has been established previously15.
Assessment of fibril formation
-
(I).
Size exclusion chromatography. PfMSP2 and PfMSP2/8 recombinant proteins were evaluated for presence of monomeric and oligomeric populations via size exclusion chromatography on a Superdex® 75 matrix (GE Health Care Life Sciences, Marlborough, MA). The column was equilibrated in TBS and calibrated using ribonuclease A, ovalbumin and conalbumin standards (GE Health Care Life Sciences). Immediately after thawing, 1 mg of purified recombinant protein was applied to the column at a flow rate of 0.5 ml/min and absorbance of the eluate at 214 nm monitored.
-
(II).
Thioflavin T fluorescence assay. To assess amyloid-like fibril formation, recombinant proteins (10 μM, in PBS) were co-incubated with 30 μM Thioflavin T (ThT; Thomas Scientific, Swedesboro, NJ) in the presence or absence of 40 μM epigallocatechin-3-O-gallate (EGCG; Millipore Sigma), an inhibitor of fibril formation26,29,48. Samples were transferred in duplicate to a 96-well black microwell plate (Thermo Fisher Scientific, 300 μl /well) and incubated at 37 °C for 98 hours. PBS alone and PBS with 30 μM ThT served as negative controls. Fluorescence was measured (443 nm excitation, 484 nm emission) at 0, 2, 4, 20, 44 and 98 hours of incubation on a Hitachi F-7000 Fluorescence Spectrophotometer. Duplicate samples were averaged and blanked against PBS with Thioflavin T.
Mouse splenocyte proliferation assay and TLR2 neutralization
Male CB6F1/J (BALB/cJ X C57BL/6 J) mice were purchased from The Jackson Laboratory and housed in the Animal Care Facility of Drexel University College of Medicine. Animal studies were reviewed, approved and conducted in compliance with Drexel University’s Institutional Animal Care and Use Committee (Protocol No. 20645) and in accordance with the US Public Health Service (PHS) Policy on Humane Care and Use of Laboratory Animals. Naïve splenocytes were prepared as described previously and stimulated in triplicate with 10 μg/ml of recombinant antigen, 1 μg/ml of concanavalin A (ConA, Millipore Sigma) or left unstimulated15,16,61. Proliferation was measured in the presence of anti-TLR2 blocking monoclonal antibody or an IgG1 isotype control (1 μg/ml; InvivoGen, San Diego, CA). After 78 hours of incubation at 37 °C in 5% CO2, 1 μCi of [3H]thymidine (PerkinElmer Life and Analytican Sciences; Shelton, CT) was added to each well, and cells were harvested after an additional 18 hours. Based on [3H]thymidine incorporation, a stimulation index for each condition was calculated as the mean counts per minute of stimulated samples divided by the mean counts per minute of unstimulated samples.
Generation of polyclonal rabbit antisera
Polyclonal rabbit antisera were generated by Lampire Biological Laboratories (Pipersville, PA). Adult New Zealand White rabbits (n = 4) were immunized subcutaneously with 100 μg of recombinant PfMSP2 or PfMSP2/8 emulsified in Montanide ISA 720 (0.5 ml; Seppic Inc., Paris, France) at a ratio of 70:30 (vol/vol). One control rabbit received adjuvant alone. Two booster immunizations were administered at 4-week intervals. Test bleeds were taken two weeks after primary and secondary immunizations and terminal sera were collected four weeks after the tertiary immunization. The specificity of newly generated rabbit anti-PfMSP2 and anti-PfMSP2/8 is established in Figs 4–7.
P. falciparum in vitro culture and assays of native PfMSP2
Plasmodium falciparum blood-stage parasites (NF54 and D10 strains) were maintained as previously described17.
-
(I).
Immunoblot of parasite lysate. A mixed blood-stage lysate from asynchronous P. falciparum infected RBCs15,17 (2.3 × 107 parasite equivalents per lane) was separated by SDS-PAGE on 12% gels under reduced and non-reduced conditions, blotted and probed with rabbit anti-rPfMSP2/8 and anti-PfMSP2 sera diluted 1:2500. Adjuvant control rabbit sera served as a negative control. Bound antibodies were detected as above.
-
(II).
Indirect immunofluorescence assay. Thin blood smears of P. falciparum NF54-infected RBCs were prepared and fixed in acetone-methanol (1:1)15,62. Slides were incubated with pooled rPfMSP2/8 or rPfMSP2 antisera or adjuvant control sera (1:400) for 30 minutes at 37 °C. Bound antibody was detected by fluorescein isothiocyanate (FITC)-conjugated goat anti-rabbit IgG (5 μg/ml; Invitrogen). Slides were mounted with SlowFade Gold antifade reagent with DAPI (4′,6-diamidino-2-phenylindole; Life Technologies, Thermo Fisher Scientific). Images were acquired using an Olympus BX60 fluorescence microscope (Olympus America, Inc.; Melville, NY) and SensiCam QE cooled digital 12-bit charge-coupled-device (CCD) camera system (PCO-Tech, Inc.; Romulus, MI), and analyzed using SlideBook 5.0 software (Intelligent Imaging Innovations, Inc.; Denver, CO).
Quantification of antigen-specific antibody by ELISA
-
(I).
Direct binding ELISA. Antigen-specific antibody titers generated by PfMSP2-based vaccines were quantified by direct-binding ELISA17. ELISA plates were coated with 0.25 μg/well of rPfMSP2 (3D7), rPfMSP2 (FC27), rPfMSP2/8 or rPfMSP8 and incubated with 2-fold serial dilutions of individual rabbit sera. High-titer pooled sera included on each plate were used for normalization. Bound antibody was detected by HRP-conjugated goat anti-rabbit IgG with ABTS [2,2′-azino-bis(ethylbenzothiazoline-6-sulfonic acid) diammonium salt] as substrate. A405 values between 1.0 and 0.1 were plotted, and titer was calculated as reciprocal of the dilution that yielded an A405 of 0.5. For peptide ELISAs, four representative peptides (18-mers) containing characterized B cell epitopes (underlined) were synthesized (RP-HPLC purity > 90%; GenScript, Piscataway, NJ). The four selected peptide sequences were as follows: N-terminal conserved region peptide (FINNAYNMSIRRSMAESK), central variable region (CVR) peptide A (TNPKGKGEVQEPNQANKE), CVR peptide B (DSQTKSNVPPTQDADTKS) and C-terminal conserved region peptide (ECTDGNKENCGAATSLLN). Plates were coated with 0.5 μg/well of each peptide and incubated with individual rabbit sera (1:200 dilution). Bound antibody was detected as above.
-
(II).
Competition ELISA15. Each rabbit serum was diluted to yield an A405 of ~1.0. Anti-rPfMSP2 (3D7) or anti-PfMSP2/8 sera were pre-incubated with 10-fold increasing concentrations (1 pM-1 μM) of rPfMSP2 (3D7) or rPfMSP2/8 in buffer containing 20 mM Tris-HCl (pH 8.0), 50 mM NaCl, 5 mM EDTA, 0.5% Triton-X-100, and 0.5% deoxycholate at 4 °C, overnight. All antibody-antigen mixtures also contained 1 μM of rPfMSP8 to completely adsorb anti-rPfMSP8-specific antibodies. The antibody-antigen samples were then added to ELISA wells coated with rPfMSP2/8 or rPfMSP2 (3D7) and binding of non-complexed, free antibodies was quantified as described above. Percent inhibition was calculated as [1 − (A405 of IgG in the presence of inhibitor/A405 of IgG in the absence of inhibitor)] × 100.
P. falciparum growth inhibition assay
A 1.5 ml sample of each rabbit serum was heat inactivated and adsorbed against human O + RBCs prior to purification of the IgG fraction by Protein G affinity chromatography63. The ability of purified rabbit anti-PfMSP2 and anti-PfMSP2/8 IgG (5.0 mg/ml and 2.5 mg/ml) to inhibit the in vitro growth of P. falciparum (NF54) was measured in a standard growth inhibitory assay (GIA)64. Rabbit anti-PfMSP1/8 and adjuvant control IgG were used as positive and negative controls, respectively. Parasite growth inhibition was based on measurement of parasite lactate dehydrogenase activity relative to P. falciparum incubated with RBCs in the absence of rabbit IgG.
Opsonophagocytosis Assay
-
(I).
THP-1 in vitro culture. THP-1 cells (ATCC® TIB-202) were purchased and maintained in RPMI 1640 (ATCC 30-2001) supplemented with 0.05 mM 2-mercaptoethanol and 10% fetal bovine serum. Cell density was regularly monitored and maintained between 1 × 105 and 1 × 106 cells/ml. Cells were passaged when cell density reached 8 × 105 cells/ml and were not used beyond passage ten.
-
(II).
Merozoite isolation and preparation. For isolation of merozoites, P. falciparum cultures were synchronized by treatment with 5% D-sorbitol. Late stage, pigmented trophozoites were isolated by magnetic column purification65 and subsequently cultured with complete culture medium supplemented with 10 μM trans-epoxysuccinyl-L-leucylamido-(4-guanidino) butane (E64, Millipore Sigma) for 6–8 hours. Merozoites were mechanically released from late stage, fully segmented schizonts15 and free hemozoin removed by a second passaged over a magnetic column. Purified merozoites were pelleted and stained with 5 μM Nuclear RedTM LCS1 (AAT Bioquest, Sunnyvale, CA) for 15 minutes at 4 °C. Stained merozoites were washed and fixed with 2% formaldehyde (Polysciences Inc., Warrington, PA). Fixed, stained merozoites were washed and counted using CountBrightTM Absolute Counting Beads (Thermo Fisher Scientific) on a BD AccuriTM C6 (BD Biosciences) flow cytometer. Merozoites were resuspended at 1 × 107 merozoites/ml in THP-1 culture media and used as described.
-
(III).
Opsonization and Phagocytosis. U-bottom, 96-well plates were pre-coated with FBS (1 hr at room temperature). For opsonization, 30 μl merozoites (1 × 107 merozoites/ml) were transferred to each well and incubated with 3 μl of test IgG at a concentration of 0.1 mg/ml or 0.25 mg/ml for 1 hr at room temperature. Unopsonized and control IgG opsonized merozoites served as negative controls. Opsonized merozoites were washed, resuspended in 150 μl THP-1 medium and plated in triplicate (50 μl/well). THP-1 cells were resuspended at 2 × 105 cells/ml, and 100 μl were co-incubated with opsonized merozoites for 10 minutes at 37 °C. Phagocytosis was stopped by the addition of 50 μl cold PBS containing 3% FBS. THP-1 cells were washed, fixed in 2% formaldehyde and analyzed on BD AccuriTM C6 flow cytometer using FlowJo® analysis software. The level of phagocytosis was determined as percentage of THP-1 cells positive for Nuclear Red fluorescence relative to unopsonized negative control. Percent phagocytosis of adjuvant control IgG was subtracted from concentration-matched test samples.
Statistical analysis
In the comparison of two, non-paired samples, Mann-Whitney test was used to determine statistical significance of differences between antigen-specific IgG titers. To determine statistical significance of boosting in antigen-specific IgG titers, the Friedman test followed by Dunn’s post hoc test was used. Considering sample sizes, nonparametric tests were used. Differences were considered significant with probability (p) values ≤ 0.05.
Equipment and Settings
-
(I).
Coomassie-stained polyacrylamide gels. Coomassie Blue-stained polyacrylamide gels were imaged using the ImageQuantTM LAS 4000, gel documentation camera (GE Healthcare Life Sciences Technology, Marlborough, MA). Images were imported into Microsoft PowerPoint for mock up. Brightness and contrast were adjusted to increase clarity of unstained portion of gel; adjustments were applied to entire gel equally. Full-length gels are shown in Figs 1B,D, 2A,D.
-
(II).
Immunoblots. Chemiluminescent immunoblot images were acquired by exposure to HyBlot CL® Autoradiography Film (Denville Scientific Inc., Metuchen, NJ). Developed films were scanned using an HP Scanjet G4050 scanner, and scanned images were imported into Microsoft PowerPoint for mock up. Minimal adjustments to brightness and contrast were made increase clarity of the gray film background. All adjustments were applied to the entire gel equally. Full-length gels shown in Figs 1C,E, 2B,C,E and 5A.
-
(III).
Microscopy. Images were acquired at a resolution of 1376 × 1040 pixels using an Olympus BX60 fluorescence microscope with a UPlanApo (100×/1.35) oil immersion objective lens (Olympus America, Inc.; Melville, NY) and SensiCam QE cooled digital 12-bit charge-coupled-device (CCD) camera system (PCO-Tech, Inc.; Romulus, MI), and analyzed using SlideBook 5.0 software (Intelligent Imaging Innovations, Inc.; Denver, CO). Representative images (Fig. 5B) were imported into Microsoft PowerPoint for mock up. Edges were cropped to the focal point of the image to eliminate blank space.
For all gel, immunoblot and microscopy images, Microsoft PowerPoint figures were saved in ‘Press Quality’ PDF format and imported into Adobe Photoshop v5.5 at a resolution of 600 dpi. In Photoshop, the image was sized, flattened and saved in a Tagged Image File Format (TIFF) with Image Compression set to LZW, Pixel Order set to Interleaved and Byte Order set to IBM PC. No additional adjustments were made to any of the images in Photoshop.
Data Availability
The data generated and analyzed that support the scientific findings and claims of this study are presented in this published article.
Supplementary information
Acknowledgements
This work was supported by NIH-NIAID Grant AI114292 (JMB). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author Contributions
J.S.E. and J.M.B. conceived and designed the experiments. J.S.E. completed experiments for Figures 1–6, 9, Table 1 and Table S1. J.M.B. completed experiments for Figures 7, 8 and S1. D.M.G. completed G.I.A. assays for Table 2. R.G.F. expressed and purified rPfMSP2 (FC27). J.S.E. and J.M.B. analyzed the data and prepared the manuscript. All authors reviewed and approved the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-45440-4.
References
- 1.World Health Organization. World Malaria Report, https://www.who.int/malaria/publications/world-malaria-report-2018/en/ (2018).
- 2.RTS,S Clinical Trials Partnership Efficacy and safety of RTS,S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet. 2015;386:31–45. doi: 10.1016/S0140-6736(15)60721-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White MT, et al. Immunogenicity of the RTS,S/AS01 malaria vaccine and implications for duration of vaccine efficacy: Secondary analysis of data from a phase 3 randomised controlled trial. Lancet Infect. Dis. 2015;15:1450–1458. doi: 10.1016/S1473-3099(15)00239-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ubillos I, et al. Baseline exposure, antibody subclass, and hepatitis B response differentially affect malaria protective immunity following RTS,S/AS01E vaccination in African children. BMC Med. 2018;16:197. doi: 10.1186/s12916-018-1186-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gosling R, von Seidlein L. The Future of the RTS,S/AS01 Malaria Vaccine: An Alternative Development Plan. PLoS Medicine. 2016;13:e1001994. doi: 10.1371/journal.pmed.1001994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crompton PD, et al. A prospective analysis of the Ab response to Plasmodium falciparum before and after a malaria season by protein microarray. Proc. Natl. Acad. Sci. 2010;107:6958–6963. doi: 10.1073/pnas.1001323107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osier FHA, et al. Breadth and magnitude of antibody responses to multiple Plasmodium falciparum merozoite antigens are associated with protection from clinical malaria. Infect. Immun. 2008;76:2240–2248. doi: 10.1128/IAI.01585-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richards JS, et al. Association between naturally acquired antibodies to erythrocyte‐binding antigens of Plasmodium falciparum and protection from malaria and high‐density parasitemia. Clin. Infect. Dis. 2010;51:e50–e60. doi: 10.1086/656413. [DOI] [PubMed] [Google Scholar]
- 9.Chan JA, et al. Patterns of protective associations differ for antibodies to P. falciparum -infected erythrocytes and merozoites in immunity against malaria in children. Eur. J. Immunol. 2017;47:2124–2136. doi: 10.1002/eji.201747032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Richards JS, et al. Identification and prioritization of merozoite antigens as targets of protective human immunity to Plasmodium falciparum malaria for vaccine and biomarker development. J. Immunol. 2013;191:795–809. doi: 10.4049/jimmunol.1300778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Draper SJ, et al. Malaria vaccines: recent advances and new horizons. Cell Host Microbe. 2018;24:43–56. doi: 10.1016/j.chom.2018.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barry AE, Arnott AS. Strategies for designing and monitoring malaria vaccines targeting diverse antigens. Front. Immunol. 2014;5:359. doi: 10.3389/fimmu.2014.00359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ouattara A, et al. Designing malaria vaccines to circumvent antigen variability. Vaccine. 2015;33:7506–7512. doi: 10.1016/j.vaccine.2015.09.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nahrendorf W, Scholzen A, Sauerwein RW, Langhorne J. Cross-stage immunity for malaria vaccine development. Vaccine. 2015;33:7513–7517. doi: 10.1016/j.vaccine.2015.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alaro JR, et al. Evaluation of the immunogenicity and vaccine potential of recombinant Plasmodium falciparum merozoite surface protein 8. Infect. Immun. 2012;80:2473–2484. doi: 10.1128/IAI.00211-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alaro JR, et al. A chimeric Plasmodium falciparum merozoite surface protein vaccine induces high titers of parasite growth inhibitory antibodies. Infect. Immun. 2013;81:3843–3854. doi: 10.1128/IAI.00522-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parzych EM, Miura K, Ramanathan A, Long CA, Burns JM. Evaluation of a Plasmodium-specific carrier protein to enhance production of recombinant Pfs25, a leading transmission-blocking vaccine candidate. Infect. Immun. 2017;86:e00486–17. doi: 10.1128/IAI.00486-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burns JM, Miura K, Sullivan J, Long CA, Barnwell JW. Immunogenicity of a chimeric Plasmodium falciparum merozoite surface protein vaccine in Aotus monkeys. Malar. J. 2016;15:159. doi: 10.1186/s12936-016-1226-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smythe JA, et al. Identification of two integral membrane proteins of Plasmodium falciparum. Proc. Natl. Acad. Sci. USA. 1988;85:5195–5199. doi: 10.1073/pnas.85.14.5195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smythe JA, et al. Structural diversity in the 45-kilodalton merozoite surface antigen of Plasmodium falciparum. Mol. Biochem. Parasitol. 1990;39:227–234. doi: 10.1016/0166-6851(90)90061-P. [DOI] [PubMed] [Google Scholar]
- 21.Gilson PR, et al. Identification and stoichiometry of glycosylphosphatidylinositol-anchored membrane proteins of the human malaria parasite Plasmodium falciparum. Mol. Cell. Proteomics. 2006;5:1286–1299. doi: 10.1074/mcp.M600035-MCP200. [DOI] [PubMed] [Google Scholar]
- 22.Sanders PR, et al. A set of glycosylphosphatidyl inositol-anchored membrane proteins of Plasmodium falciparum is refractory to genetic deletion. Infect. Immun. 2006;74:4330–4338. doi: 10.1128/IAI.00054-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boyle MJ, et al. Sequential processing of merozoite surface proteins during and after erythrocyte invasion by Plasmodium falciparum. Infect. Immun. 2014;82:924–936. doi: 10.1128/IAI.00866-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smythe JA, et al. Structural diversity in the Plasmodium falciparum merozoite surface antigen 2. Proc. Natl. Acad. Sci. USA. 1991;88:1751–1755. doi: 10.1073/pnas.88.5.1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fenton B, et al. Structural and antigenic polymorphism of the 35- to 48-kilodalton merozoite surface antigen (MSA-2) of the malaria parasite Plasmodium falciparum. Mol. Cell. Biol. 1991;11:963–971. doi: 10.1128/MCB.11.2.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang X, et al. Identification of key residues involved in fibril formation by the conserved N-terminal region of Plasmodium falciparum merozoite surface protein 2 (MSP2) Biochimie. 2010;92:1287–1295. doi: 10.1016/j.biochi.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chandrashekaran IR, Adda CG, MacRaild CA, Anders RF, Norton RS. EGCG disaggregates amyloid-like fibrils formed by Plasmodium falciparum merozoite surface protein 2. Arch. Biochem. Biophys. 2011;513:153–157. doi: 10.1016/j.abb.2011.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chandrashekaran IR, Adda CG, MacRaild CA, Anders RF, Norton RS. Inhibition by flavonoids of amyloid-like fibril formation by Plasmodium falciparum merozoite surface protein 2. Biochemistry. 2010;49:5899–5908. doi: 10.1021/bi902197x. [DOI] [PubMed] [Google Scholar]
- 29.Yang X, et al. A partially structured region of a largely unstructured protein, Plasmodium falciparum merozoite surface protein 2 (MSP2), forms amyloid-like fibrils. J. Pept. Sci. 2007;13:839–848. doi: 10.1002/psc.910. [DOI] [PubMed] [Google Scholar]
- 30.Adda CG, et al. Plasmodium falciparum merozoite surface protein 2 is unstructured and forms amyloid-like fibrils. Mol. Biochem. Parasitol. 2009;166:159–171. doi: 10.1016/j.molbiopara.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Low A, et al. Merozoite surface protein 2 of Plasmodium falciparum: expression, structure, dynamics, and fibril formation of the conserved N-terminal domain. Biopolymers. 2007;87:12–22. doi: 10.1002/bip.20764. [DOI] [PubMed] [Google Scholar]
- 32.Zhang X, et al. Role of the helical structure of the N-terminal region of Plasmodium falciparum merozoite surface protein 2 in fibril formation and membrane interaction. Biochemistry. 2012;51:1380–1387. doi: 10.1021/bi201880s. [DOI] [PubMed] [Google Scholar]
- 33.MacRaild CA, Pedersen MØ, Anders RF, Norton RS. Lipid interactions of the malaria antigen merozoite surface protein 2. Biochim. Biophys. Acta – Biomembr. 2012;1818:2572–2578. doi: 10.1016/j.bbamem.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 34.MacRaild CA, et al. Conformational dynamics and antigenicity in the disordered malaria antigen merozoite surface protein 2. PLoS One. 2015;10:e0119899. doi: 10.1371/journal.pone.0119899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lu C, et al. Interaction of merozoite surface protein 2 with lipid membranes. FEBS Lett. 2019;593:288–295. doi: 10.1002/1873-3468.13320. [DOI] [PubMed] [Google Scholar]
- 36.Osier FHA, et al. Allele-specific antibodies to Plasmodium falciparum merozoite surface protein-2 and protection against clinical malaria. Parasite Immunol. 2010;32:193–201. doi: 10.1111/j.1365-3024.2009.01178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reddy SB, et al. High affinity antibodies to Plasmodium falciparum merozoite antigens are associated with protection from malaria. PLoS One. 2012;7:e32242. doi: 10.1371/journal.pone.0032242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Genton B, et al. A recombinant blood‐stage malaria vaccine reduces Plasmodium falciparum density and exerts selective pressure on parasite populations in a phase 1–2b trial in Papua New Guinea. J. Infect. Dis. 2002;185:820–827. doi: 10.1086/339342. [DOI] [PubMed] [Google Scholar]
- 39.Genton B, et al. Safety and immunogenicity of a three-component blood-stage malaria vaccine (MSP1, MSP2, RESA) against Plasmodium falciparum in Papua New Guinean children. Vaccine. 2003;22:30–41. doi: 10.1016/S0264-410X(03)00536-X. [DOI] [PubMed] [Google Scholar]
- 40.Taylor RR, Allen SJ, Riley EM, Greenwood BM. IgG3 antibodies to Plasmodium falciparum merozoite surface protein 2 (MSP2): increasing prevalence with age and association with clinical immunity to malaria. Am. J. Trop. Med. Hyg. 1998;58:406–413. doi: 10.4269/ajtmh.1998.58.406. [DOI] [PubMed] [Google Scholar]
- 41.Stanisic DI, et al. Immunoglobulin G subclass-specific responses against Plasmodium falciparum merozoite antigens are associated with control of parasitemia and protection from symptomatic illness. Infection and Immunity. 2009;77:1165–1174. doi: 10.1128/IAI.01129-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stubbs J, et al. Strain-transcending Fc-dependent killing of Plasmodium falciparum by merozoite surface protein 2 allele-specific human antibodies. Infect. Immun. 2011;79:1143–1152. doi: 10.1128/IAI.01034-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Osier FH, et al. Opsonic phagocytosis of Plasmodium falciparum merozoites: mechanism in human immunity and a correlate of protection against malaria. BMC Med. 2014;12:108. doi: 10.1186/1741-7015-12-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boyle MJ, et al. Human antibodies fix complement to inhibit plasmodium falciparum invasion of erythrocytes and are associated with protection against malaria. Immunity. 2015;42:580–590. doi: 10.1016/j.immuni.2015.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Angov E, Hillier CJ, Kincaid RL, Lyon JA. Heterologous protein expression is enhanced by harmonizing the codon usage frequencies of the target gene with those of the expression host. PLoS One. 2008;3:e2189. doi: 10.1371/journal.pone.0002189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Plassmeyer ML, et al. Structure of the Plasmodium falciparum circumsporozoite protein, a leading malaria vaccine candidate. J. Biol. Chem. 2009;284:26951–26963. doi: 10.1074/jbc.M109.013706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Singh SK, et al. Lactococcus lactis provides an efficient platform for production of disulfide-rich recombinant proteins from Plasmodium falciparum. Microb. Cell Fact. 2018;17:55. doi: 10.1186/s12934-018-0902-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Adda CG, et al. Antigenic characterization of an intrinsically unstructured protein, Plasmodium falciparum merozoite surface protein 2. Infect. Immun. 2012;80:4177–4185. doi: 10.1128/IAI.00665-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Krishnarjuna B, et al. Strain-transcending immune response generated by chimeras of the malaria vaccine candidate merozoite surface protein 2. Sci. Rep. 2016;6:20613. doi: 10.1038/srep20613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Duncan CJA, Hill AVS, Ellis RD. Can growth inhibition assays (GIA) predict blood-stage malaria vaccine efficacy? Hum. Vaccin. Immunother. 2012;8:706–714. doi: 10.4161/hv.19712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dent AE, et al. Antibody-mediated growth inhibition of Plasmodium falciparum: relationship to age and protection from parasitemia in Kenyan children and adults. PLoS One. 2008;3:e3557. doi: 10.1371/journal.pone.0003557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McCallum FJ, et al. Acquisition of growth-inhibitory antibodies against blood-stage Plasmodium falciparum. PLoS One. 2008;3:e3571. doi: 10.1371/journal.pone.0003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Weisman S, et al. Antibody responses to infections with strains of Plasmodium falciparum expressing diverse forms of merozoite surface protein 2. Infect. Immun. 2001;69:959–967. doi: 10.1128/IAI.69.2.959-967.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Feng G, et al. Human immunization with a polymorphic malaria vaccine candidate induced antibodies to conserved epitopes that promote functional antibodies to multiple parasite strains. J. Infect. Dis. 2018;218:35–43. doi: 10.1093/infdis/jiy170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mata E, et al. Adjuvant activity of polymer microparticles and Montanide ISA 720 on immune responses to Plasmodium falciparum MSP2 long synthetic peptides in mice. Vaccine. 2007;25:877–885. doi: 10.1016/j.vaccine.2006.09.036. [DOI] [PubMed] [Google Scholar]
- 56.Flueck C, et al. Evaluation of two long synthetic merozoite surface protein 2 peptides as malaria vaccine candidates. Vaccine. 2009;27:2653–2661. doi: 10.1016/j.vaccine.2009.02.081. [DOI] [PubMed] [Google Scholar]
- 57.Balam S, et al. Immunogenicity of dimorphic and C-terminal fragments of Plasmodium falciparum MSP2 formulated with different adjuvants in mice. Vaccine. 2016;34:1566–1574. doi: 10.1016/j.vaccine.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 58.Jana M, Palencia CA, Pahan K. Fibrillar amyloid-beta peptides activate microglia via TLR2: implications for Alzheimer’s disease. J. Immunol. 2008;181:7254–7262. doi: 10.4049/jimmunol.181.10.7254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tükel Ç, et al. Responses to amyloids of microbial and host origin are mediated through toll-like receptor 2. Cell Host Microbe. 2009;6:45–53. doi: 10.1016/j.chom.2009.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hommel M, et al. Evaluating antibody functional activity and strain-specificity of vaccine candidates for malaria in pregnancy using in vitro phagocytosis assays. Parasit. Vectors. 2018;11:69. doi: 10.1186/s13071-018-2653-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alaro JR, Lynch MM, Burns JM. Protective immune responses elicited by immunization with a chimeric blood-stage malaria vaccine persist but are not boosted by Plasmodium yoelii challenge infection. Vaccine. 2010;28:6876–6884. doi: 10.1016/j.vaccine.2010.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shi Q, Cernetich-Ott A, Lynch MM, Burns JM. Expression, localization, and erythrocyte binding activity of Plasmodium yoelii merozoite surface protein-8. Mol. Biochem. Parasitol. 2006;149:231–241. doi: 10.1016/j.molbiopara.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 63.Malkin EM, et al. Phase 1 clinical trial of apical membrane antigen 1: an asexual blood-stage vaccine for Plasmodium falciparum malaria. Infect. Immun. 2005;73:3677–3685. doi: 10.1128/IAI.73.6.3677-3685.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Miura K, et al. Comparison of biological activity of human anti-apical membrane antigen-1 antibodies induced by natural infection and vaccination. J. Immunol. 2008;181:8776–8783. doi: 10.4049/jimmunol.181.12.8776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hill DL, Eriksson EM, Schofield L. High yield purification of Plasmodium falciparum merozoites for use in opsonizing antibody assays. J. Vis. Exp. 2014;89:e51590. doi: 10.3791/51590. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data generated and analyzed that support the scientific findings and claims of this study are presented in this published article.