Abstract
Background
Anterior total hip arthroplasty (THA) allows the use of intraoperative fluoroscopy to assess leg-length and offset discrepancies. Two techniques to accomplish this are the transverse rod method and the radiographic overlay method. The aim of this study was to determine if they are equally effective options for minimizing postoperative radiologic discrepancies.
Methods
We completed a retrospective cohort study comparing 106 anterior THAs from 1 surgeon using the transverse rod technique to 94 anterior THAs from another surgeon using the radiograph overlay technique. Radiographic leg-length discrepancy (LLD) and offset discrepancy (OD) were measured independently on postoperative radiographs. Parametric, nonparametric, and categorical statistical tests were used to compare LLD and OD between groups.
Results
Baseline characteristics were similar between groups. The mean LLD of 4.8 mm in the radiograph overlay group was not significantly different from the 4.4 mm mean discrepancy in the transverse rod group (P = .424), and the rates of LLD < 5 mm and LLD < 10 mm were not significantly different (P = .772, P = .179). The mean OD of 5.1 mm in the radiograph overlay group was not significantly different from the 4.8 mm mean discrepancy in the transverse rod group (P = .668), and there was no significant difference in the rates of OD < 5 mm and OD < 10 mm (P = .488, P = .878).
Conclusions
There was no difference between the measured LLD and OD by the 2 surgeons, suggesting that the techniques are equally effective options.
Keywords: Anterior total hip arthroplasty, Leg-length discrepancy, Offset discrepancy, Surgical technique
Introduction
Restoring or maintaining equivalent leg lengths is an important goal of total hip arthroplasty (THA). Leg length inequality after THA has long been recognized as a complication of the procedure. [1], [2] Postoperatively, 32%-41% of patients notice a difference in leg lengths [3], [4] and up to 45% require use of a shoe lift. [2], [3], [5], [6] However, the degree to which leg-length discrepancy (LLD) affects clinical outcomes remains controversial. [3], [7], [8], [9], [10] The vast majority of patients who undergo THA have less than a 10 mm discrepancy postoperatively, [8], [11], [12], [13] and evaluation of iatrogenic discrepancies suggests that between 5 mm and 10 mm [14], [15] is well tolerated. Recreating hip offset, the difference between the center of rotation of the femoral head and the axis of the femur, is another consideration in THA, as appropriately increased offset has been associated with greater abductor muscle strength, [16], [17] improved pelvic stability, [16] superior gait, [18] and higher patient-reported outcomes. [10], [19]
Direct anterior approach THA has become increasingly popular [20] and provides the opportunity to utilize intraoperative fluoroscopy to assess leg length and offset. [11], [13] Although intraoperative imaging is seemingly an advantage, studies have suggested that limb length [11], [21], [22] and offset [21] measurements are similar between the anterior and posterior approaches. In anterior THA, the surgeon can obtain fluoroscopic images of the pelvis and compare the operative and nonoperative hips for overall symmetry and evaluate leg length using a transverse metal rod to compare distances between the ischial tuberosities and lesser trochanters. [11] Alternatively, a single intraoperative fluoroscopic image of the operative hip with trial implants in place can be printed and overlaid on an identical image of the same hip taken preoperatively to evaluate for appropriate anatomic relationships. This technique represents a variation on the technique initially described by Matta et al. (2005) [13].
The 2 major methods for measuring leg length and offset intraoperatively in direct anterior THA have not been formally compared in the literature. The objective of this study was to retrospectively compare radiographic outcomes between the 2 measurement techniques to determine if they are equally effective. We hypothesized that there would be no significant differences in leg length or offset discrepancy between the methods.
Material and methods
We completed a retrospective cohort study comparing radiographic leg length and offset discrepancies between intraoperative measurement techniques in direct anterior THA at a tertiary referral center in the Northeastern United States. The study was reviewed by the institutional review board, and a waiver of consent was granted. At our institution, there is variation between intraoperative anterior THA measurement techniques, allowing us to effectively make comparisons between 2 surgeons who exclusively used either the transverse rod or radiograph overlay option. Our study included all patients between 2014 and 2016 undergoing THA with either of the 2 surgeons using these methods. One surgeon had recently entered practice after fellowship, and his first 100 patients undergoing anterior THA were excluded to avoid any impact of a learning curve on our results. [23] Patients were included if they underwent a direct anterior THA for osteoarthritis, posttraumatic arthritis, or avascular necrosis. Patients who underwent surgery for fracture or malignancy, received sequential bilateral THA on the same day, experienced intraoperative fractures, required acetabular augmentation, or who did not have adequate postoperative radiographs were excluded from the study.
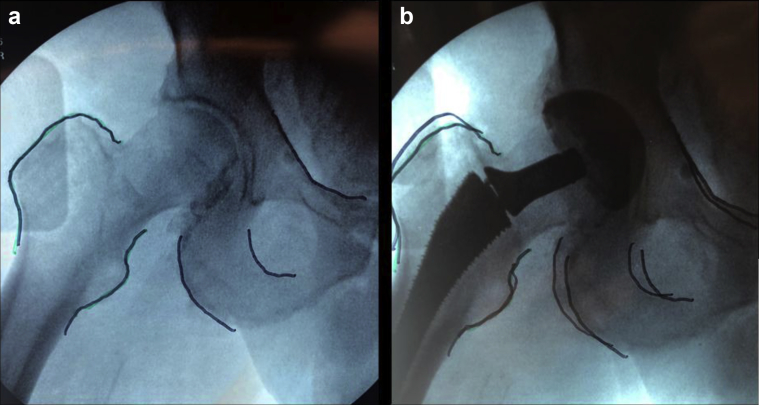
Patients undergoing anterior THA surgery were initially positioned on a Hana table (Mizuho OSI, Union City, CA, USA) before a direct anterior approach to the hip was completed. A portable fluoroscopy machine was used to complete intraoperative imaging in both groups (GE Healthcare, Model OEC 9900 Elite, Mobile C-Arm X-ray System, Waukesha, WI, USA). In the transverse rod group, the surgeon obtained an anteroposterior (AP) pelvic fluoroscopic image before the start of surgery to ensure proper positioning of the fluoroscopy machine and patient. After the implant trials were positioned, a sterile metal rod was held in a transverse orientation over the operative field, and an AP image was obtained (Fig. 1) as has been described previously. [11] A series of images were then obtained to properly position the rod directly in line with the bilateral ischial tuberosities. After this position was achieved, the relative position between the rod, tuberosities, and the less trochanters was judged visually by the attending surgeon to determine if any implant changes were necessary (Fig. 1). The offset was also evaluated visually for symmetry between sides.
Figure 1.
The transverse rod technique. An intraoperative radiograph is taken with the trial implants in place with a metal rod aligned across the ischial tuberosities. The apparent bend of the straight rod is an artifact due to parallax from using fluoroscopy. The relative position of the intersection between the metal rod and the lesser trochanters is judged on the operative and nonoperative sides to assess the relative leg lengths. The femoral offset is judged visually between the 2 sides.
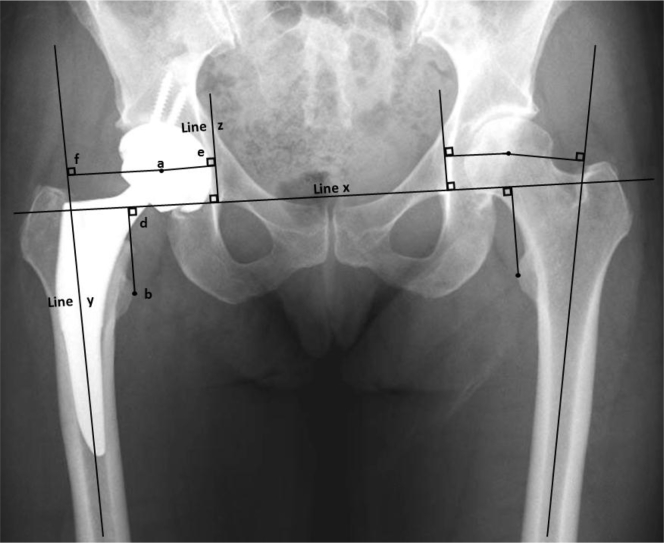
In the radiograph overlay group, an AP fluoroscopic image of the operative hip was obtained before prepping and draping the patient. This radiograph was printed on a translucent film and important landmarks, including the greater and lesser trochanters, were outlined with a surgical marker (Fig. 2). After the prosthetic trials were inserted, a second fluoroscopic image was obtained from the same point of view as the first. This image was then overlaid on top of the initial film to compare the congruency between the preprosthesis and postprosthesis images, as a measure of how well the native anatomy had been recreated in a variation on the overlay technique originally described by Matta et al. (2005) [13] (Fig. 1). Any necessary implant changes were made after evaluating the overlaid images. In cases where the preoperative examination or clinical imaging demonstrated a substantial LLD or offset discrepancy (OD), these differences could be accounted for by ensuring that the anatomic lines traced on the intraoperative film with the trials in place did not perfectly overlay the preoperative film but instead demonstrated an appropriate shift to account for the change in leg length or offset desired.
Figure 2.
The radiograph overlay technique. (a) The preoperative radiograph, taken after the patient was positioned on the operating table, with the reference landmarks appropriately marked in ink. (b) The second radiograph, taken after the trial implants were in place, overlaid on the preoperative image. The close proximity of the reference lines indicates successful recreation of both leg length and femoral offset.
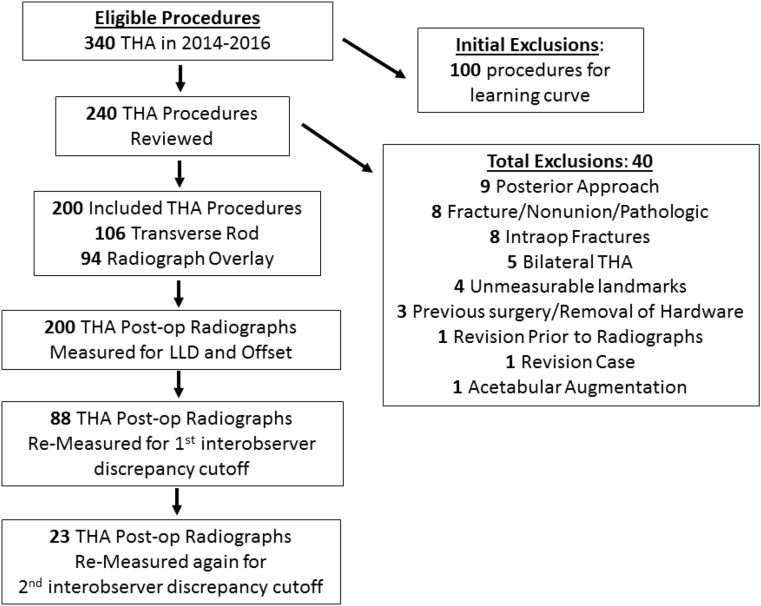
Preoperative data including age at surgery, sex, body mass index, Charlson comorbidity index, and the presence of a contralateral hip prosthesis were recorded for all patients. Postoperative AP radiographs of the pelvis were reviewed for all patients. Radiographs were considered adequate if they displayed the anatomic landmarks necessary for measurement, visualized bilateral hips, were completed before any revision surgery, and did not demonstrate any evidence of pathologic changes such as subsidence. Measurements of postoperative LLD and OD were determined for both the operative and nonoperative hips as described by Dastane et al. [24] (2011) and are demonstrated in Figure 3. The LLD or OD was determined by subtracting the nonoperative leg length or offset from that of the operative side. With this methodology, a positive discrepancy represented a relatively longer operative leg length or offset, while a negative value represented a relatively shorter or less offset limb. The absolute value of these differences was considered to be the LLD or OD measurements for the patient.
Figure 3.
Measurement technique used within the study. Line x was drawn to intersect the inferior portion of the teardrops and is used to anchor the limb-length measurements. Line z is a trans-teardrop line and is used to anchor the offset measurements as a medial reference. Line db is the radiographic limb length within the measurement algorithm. Line ae + af is the radiographic offset within the measurement algorithm.
Measurements of radiographs were completed independently by 2 surgeons (D.C.A. and B.E.D.) using the Philips IntelliSpace PACS Enterprise system, version 4.4 (Foster City, CA, USA). The LLD and OD measurements were determined as described in Figure 3. After initial measurements, the LLD and OD values for each patient were compared between the 2 observers to identify outliers requiring remeasurement. Based on the previous literature suggesting that a LLD of less than 5 mm is well tolerated [14], [15], if there was more than a 5 mm absolute difference between the reported LLD or OD between observers, the original values were discarded, and the measurements were repeated. Although this strategy rectified many of the obvious discrepancies between observers, as is shown in Figure 3, it was noted that discrepancies remained. To capture remaining large outliers, observations between observers were compared once again, and any measurements that were greater than 5 mm in magnitude, and opposite in sign, were discarded and remeasured. After completing these 3 rounds of measurements, all values were accepted, and final interobserver agreement statistics were calculated based on these values. The final LLD and OD values for each patient were calculated by averaging the LLD and OD values from each observer.
The primary outcomes of interest for this study were the LLD and OD in each group. Secondary outcomes included the proportion of patients with both LLDs and ODs less than 5 mm and 10 mm within each cohort. A LLD less than 5 mm was considered an appropriate cutoff as this discrepancy is generally well tolerated [14], [15] and has been used in previous studies. [25], [26] The LLD and OD data was primarily compared using a 2-sided student t-test. A secondary comparison of LLD and OD using the Wilcoxon rank-sum test was also completed to ensure that the slightly skewed nature of the LLD and OD data did not affect statistical conclusions. The Wilcoxon rank-sum test was also used to compare the highly skewed Charlson index data between groups. Dichotomous data including gender as well as LLD and OD rates were compared using chi-squared test. Statistical analysis was completed using Stata, version 15.0 (College Station, Texas, USA). A post hoc power analysis was completed using the online power analysis calculator Sealed Envelope [27], [28]. Interobserver reliability was evaluated after all measurements were completed using Spearman's correlation to assess LLD and OD as a continuous variable and Cohen's kappa to assess interobserver agreement on the rates of LLD and OD < 5 mm. A P-value of less than 0.05 was considered statistically significant.
Results
The initial query produced 340 eligible THA procedures from the 2 surgeons of interest. The first 100 patients from the transverse rod cohort were excluded as planned a priori to eliminate the influence of a learning curve on results, as that surgeon had recently completed fellowship training. An additional 40 patients were excluded after meeting exclusion criteria as shown in Figure 4. After exclusions, 200 total THA procedures were included, with 106 in the transverse rod cohort and 94 in the radiograph overlay cohort. Radiographs from all 200 patients were measured in the first round of observations; 88 (44%) of these patients required remeasurements after applying the first cutoff for interobserver discrepancy, and 23 (11.5%) were remeasured after applying the second cutoff for interobserver discrepancy (Fig. 4).
Figure 4.
Flowchart of the included and excluded procedures.
The age, proportion of females, body mass index, and Charlson scores were not significantly different between the 2 cohorts (Table 1). There were significantly more contralateral arthroplasties present within the transverse rod cohort (40.6% vs 13.8%; P < .001). Postoperatively, the mean difference in leg lengths between the operative and nonoperative side was −0.33 mm (standard deviation [SD] = 6.0) in the radiograph overlay group and 0.78 mm (SD = 5.35) in the transverse rod group; the values were not significantly different (P = .170). The mean difference in offset between the operative and nonoperative side was −2.1 mm (SD = 6.4) in the radiography overlay group and −1.2 mm (SD = 6.2) in the transverse rod cohort; values were not significantly different (P = .321).
Table 1.
A comparison of baseline characteristics between groups.
| Variable | Radiograph overlay, N = 94 | Transverse rod, N = 106 | P-value |
|---|---|---|---|
| Age (years)a | 62.9 (11.8) | 65.1 (9.8) | .147 |
| Female genderc | 45.7% (43) | 47.2% (50) | .840 |
| BMI (kg/m2)a | 29.8 (5.9) | 29.2 (5.9) | .461 |
| Charlson scoreb | 1 (0-2) | 0 (0-1) | .133 |
| Contralateral arthroplastyc | 13.8% (13) | 40.6% (43) | <.001 |
BMI, body mass index.
Student t-test, mean (standard deviation).
Wilcoxon rank-sum test, median (interquartile range).
Chi-squared analysis, % (n).
The postoperative mean LLD of 4.8 mm in the radiograph overlay group was not significantly different from the 4.4 mm mean discrepancy in the transverse rod group (P = .424; Table 2). Nonparametric testing also demonstrated that LLD was similar between groups (P = .628). The mean difference in leg length between the operative and nonoperative side was −0.33 mm (SD = 6.0) in the radiograph overlay group and 0.78 mm (SD = 5.35) in the transverse rod group; the values were not significantly different (P = .170). The 59.6% rate of LLD <5 mm in the radiograph overlay group was not significantly different from the 57.5% rate in the transverse rod cohort (P = .772; Table 2). Similarly, the 90.4% rate of LLD <10 mm in the radiograph overlay group was not significantly different from the 95.3% rate in the transverse rod cohort (P = .179).
Table 2.
Radiographic outcomes.
| Variable | Radiograph overlay, N = 94 | Transverse rod, N = 106 | P-value |
|---|---|---|---|
| Leg-length discrepancy (mm)a (parametric testing) | 4.8 (3.7) | 4.4 (3.1) | .424 |
| Leg-length discrepancy (mm)b (nonparametric testing) | 3.9 (1.8-7.2) | 3.8 (1.9-6.5) | .628 |
| Leg-length discrepancy <5 mmc | 59.6% (56) | 57.5% (61) | .772 |
| Leg-length discrepancy <10 mmc | 90.4% (85) | 95.3% (101) | .179 |
| Offset discrepancy (mm)a (parametric testing) | 5.1 (4.4) | 4.8 (4.0) | .668 |
| Offset discrepancy (mm)b (nonparametric testing) | 4.1 (1.9-7.2) | 3.9 (1.8-6.7) | .732 |
| Offset discrepancy <5 mmc | 57.4% (54) | 62.3% (66) | .488 |
| Offset discrepancy <10 mmc | 89.3% (84) | 88.7% (94) | .878 |
Student t-test, mean (standard deviation).
Wilcoxon rank-sum test, median (interquartile range).
Chi-square test, % (n).
The mean OD discrepancy of 5.1 mm in the radiograph overlay group was not significantly different from the 4.8 mm mean discrepancy in the transverse rod group (P = .668; Table 2). Nonparametric testing also suggested that OD (P = .732) was not significantly different between cohorts. The mean difference in offset between the operative and nonoperative side was −2.1 mm (SD = 6.4) in the radiograph overlay group and −1.2 mm (SD = 6.2) in the transverse rod cohort; the values were not significantly different (P = .321). The 57.4% rate of OD < 5 mm in the radiograph overlay group also was not significantly different from the 62.3% rate in the transverse rod group (P = .488; Table 2). Finally, the 89.3% rate of OD < 10 mm in the radiograph overlay group was not significantly different from the 88.7% rate in the transverse rod cohort (P = .878).
To control for the significantly different rate of contralateral arthroplasties present between the groups, subgroup analyses were completed. In the group of patients with a native hip on the contralateral side (n = 144), analyses demonstrated that the average LLD (nonparametric P = .83, parametric P = .56) and OD (nonparametric P = .54, parametric P = .96) were not significantly different between the radiograph overlay and transverse rod groups. In the subgroup of patients with a contralateral arthroplasty (n = 56), the average LLD (nonparametric and parametric P = .85) and average OD (nonparametric P = .11, parametric P = .62) were also not significantly different between cohorts.
Interobserver reliability testing utilizing Spearman's correlation coefficient demonstrated strong positive correlations of r = 0.87 for LLD and r = 0.79 for OD. The Cohen's kappa values of 0.60 for LLD <5 mm and 0.45 for OD < 5 mm were moderate. [29] A post hoc power analysis demonstrated that our sample size was adequate to determine equivalency within 1.5 mm for LLD and 1.8 mm for OD with an alpha of 0.05 and beta of 0.20.
Discussion
Restoring or maintaining equivalent leg lengths and offset after THA is an important goal for maximizing the postoperative function of a patient [3], [7], [8], [9], [10], [16], [17], [18], [19]. While the anterior approach to the hip affords the opportunity to routinely utilize intraoperative fluoroscopy, it is unclear if there is a superior method for assessing intraoperative leg length and offset. Our study demonstrated that a surgeon using the transverse rod method [11] was equally effective at minimizing LLD and OD as a surgeon utilizing the overlaid radiographs technique [13].
All outcomes including LLD, OD, the proportion of LLD and OD less than 5 mm, and the proportion of LLD and OD less than 10 mm were similar between groups, demonstrating the equivalence of the techniques. In addition, in both the groups, approximately 60% of patients demonstrated LLD and OD < 5 mm, and approximately 90% were within 10 mm, demonstrating the overall success of both methods. Previous research on induced LLDs reported that 5-10 mm of difference is generally well tolerated [14], [15] and suggests that the majority of our patients should be satisfied with their leg lengths postoperatively. Although both methods produced equivalent outcomes, it is notable that the radiograph overlay technique normally utilizes only 2 fluoroscopic images while the transverse rod requires multiple shots or even live fluoroscopy to obtain appropriate alignment and may result in lower radiation exposure to the patient and surgeon. However, the significance of this difference may not be relevant as a recent study demonstrated the radiation dose during anterior THA is less than a single pelvic radiograph for the patient and is nondetectable for the surgeon. [30] A downside to the radiograph overlay technique is the need to print transparent images on disposable film, an added cost that may be prohibitive in some settings.
Previous studies have reported postoperative radiographic LLD between 1.8 mm and 3.5 mm. [31], [32], [33]. The mean postoperative LLDs of 4.8 mm and 4.4 mm in our study are slightly higher than previous observations but are all within 3 mm of previous studies and likely do not reflect clinically meaningful differences. The 59.6% and 57.5% success rates of <5 mm LLD in our respective cohorts is similar to previous studies by Lin et al. [26] (2014) which reported success rates of 63% and 60% in their cohorts of anterior and posterior THA and Nam et al. [11] (2013) who observed success rates of 68.9% in anterior THA. However, Weber et al. [33] (2014) observed success rate of 98% for an LLD <5 mm with navigation and 77% with fluoroscopy in anterolateral THA; numbers that were notably higher than ours. The observed differences between our study and previous reports are likely attributable to differing measurement software and techniques, surgical approaches, radiographic techniques, and patient populations. The mean OD after THA has been previously reported to range from 2.0 mm to 3.6 mm [33] with success rates of OD < 5 mm to be between 68% [26] and 95% [33]. These values differ from the mean ODs of 5.1 mm and 4.8 mm, and 57%-62% success rate of OD < 5 mm that was observed in our study. Differences in radiographic measurement techniques may account for these differences as both of these studies were measured from the center of rotation to calculate OD. [26], [33] In contrast, we used a trans-teardrop line as the reference and accounted for differences in overall femoral angle to determine the overall offset of the femur from the pelvis [24], a distance we thought to be more relevant when considering abductor tension.
The limitations of our study included the use radiographic measurement tools and protocols that could be affected by human error. To address this issue, we carried out 2 quality-control checkpoints, where data were compared between observers to ensure that any outliers were discarded and remeasured. This protocol proved adequate as our results demonstrated that we had a strong correlation and moderate kappa score when the measurements were completed and compared. In addition, our radiographic measurement algorithm was limited in that it accounted for differences in leg abduction when measuring offset but did not do so when assessing leg length. However, the methodology we used has been used previously in the literature and does effectively account for pelvic tilt when considering leg length. A further limitation was the need to define our cohorts exclusively based on the practices of 2 surgeons, instead of having each surgeon utilize both techniques, or comparing the 2 techniques within a group of surgeons. Owing to this bias, we cannot definitively conclude that the techniques themselves are equally effective, rather that the radiographic outcomes of the 2 surgeons are similar. Although there may be differences in surgical techniques, in addition to the intraoperative measurement protocols, it is reassuring that we still observed similar LLD and OD between groups. Finally, we did not compare these techniques with a control group, in which no measurement protocol was used and instead surgeons made judgments based simply on the visual appearance of the implants. Accordingly, we cannot make conclusions that either of the options tested are better than a surgeon simply evaluating intraoperative radiography visually, and future studies are necessary to make this comparison.
Conclusions
Anterior THA affords the surgeon the opportunity to routinely use intraoperative fluoroscopy to evaluate LLD and OD in real time. Measurement techniques include either using either a transverse metal rod to judge the distance between the ischial tuberosities and lesser trochanters or by overlaying an intraoperative radiograph on top of a preoperative image to see the relative positions of anatomic landmarks. The results from this study demonstrated that the postoperative radiographic LLD and OD between patients from 1 surgeon utilizing the transverse rod method, and from another utilizing the radiograph overlay method, were similar. Although these results highlight the potential for using either of these intraoperative measurement techniques in direct anterior approach THA, future studies comparing these options to using visual assessment alone are necessary to see if they truly represent an advantage.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to doi:10.1016/j.artd.2018.09.005.
Appendix A. Supplementary data
References
- 1.Turula K.B., Friberg O., Lindholm T.S., Tallroth K., Vankka E. Leg length inequality after total hip arthroplasty. Clin Orthopaedics Relat Res. 1986;202:163. [PubMed] [Google Scholar]
- 2.Williamson J.A., Reckling F.W. Limb length discrepancy and related problems following total hip joint replacement. Clin Orthopaedics Relat Res. 1978;(134):135. [PubMed] [Google Scholar]
- 3.Kersic M., Dolinar D., Antolic V., Mavcic B. The impact of leg length discrepancy on clinical outcome of total hip arthroplasty: comparison of four measurement methods. J Arthroplasty. 2014;29(1):137. doi: 10.1016/j.arth.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Edeen J., Sharkey P.F., Alexander A.H. Clinical significance of leg-length inequality after total hip arthroplasty. Am J Orthopedics (Belle Mead, NJ) 1995;24(4):347. [PubMed] [Google Scholar]
- 5.Ranawat C.S., Rao R.R., Rodriguez J.A., Bhende H.S. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty. 2001;16(6):715. doi: 10.1054/arth.2001.24442. [DOI] [PubMed] [Google Scholar]
- 6.Bose W.J. Accurate limb-length equalization during total hip arthroplasty. Orthopedics. 2000;23(5):433. [PubMed] [Google Scholar]
- 7.Whitehouse M.R., Stefanovich-Lawbuary N.S., Brunton L.R., Blom A.W. The impact of leg length discrepancy on patient satisfaction and functional outcome following total hip arthroplasty. J Arthroplasty. 2013;28(8):1408. doi: 10.1016/j.arth.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 8.White T.O., Dougall T.W. Arthroplasty of the hip. Leg length is not important. J Bone Joint Surg Br. 2002;84(3):335. doi: 10.1302/0301-620x.84b3.12460. [DOI] [PubMed] [Google Scholar]
- 9.Konyves A., Bannister G.C. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br. 2005;87(2):155. doi: 10.1302/0301-620x.87b2.14878. [DOI] [PubMed] [Google Scholar]
- 10.Innmann M.M., Maier M.W., Streit M.R. Additive influence of hip offset and leg length reconstruction on postoperative improvement in clinical outcome after total hip arthroplasty. J Arthroplasty. 2018;33(1):156. doi: 10.1016/j.arth.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 11.Nam D., Sculco P.K., Abdel M.P., Alexiades M.M., Figgie M.P., Mayman D.J. Leg-length inequalities following THA based on surgical technique. Orthopedics. 2013;36(4):e395. doi: 10.3928/01477447-20130327-11. [DOI] [PubMed] [Google Scholar]
- 12.Unnanuntana A., Wagner D., Goodman S.B. The accuracy of preoperative templating in cementless total hip arthroplasty. J Arthroplasty. 2009;24(2):180. doi: 10.1016/j.arth.2007.10.032. [DOI] [PubMed] [Google Scholar]
- 13.Matta J.M., Shahrdar C., Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthopaedics Relat Res. 2005;441:115. doi: 10.1097/01.blo.0000194309.70518.cb. [DOI] [PubMed] [Google Scholar]
- 14.Sykes A., Hill J., Orr J. Patients' perception of leg length discrepancy post total hip arthroplasty. J Clin Exp Res Hip Pathol Ther. 2015;25(5):452. doi: 10.5301/hipint.5000276. [DOI] [PubMed] [Google Scholar]
- 15.O'Brien S., Kernohan G., Fitzpatrick C., Hill J., Beverland D. Perception of imposed leg length inequality in normal subjects. J Clin Exp Res hip Pathol Ther. 2010;20(4):505. doi: 10.1177/112070001002000414. [DOI] [PubMed] [Google Scholar]
- 16.Asayama I., Chamnongkich S., Simpson K.J., Kinsey T.L., Mahoney O.M. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005;20(4):414. doi: 10.1016/j.arth.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 17.McGrory B.J., Morrey B.F., Cahalan T.D., An K.N., Cabanela M.E. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br. 1995;77(6):865. [PubMed] [Google Scholar]
- 18.Renkawitz T., Weber T., Dullien S. Leg length and offset differences above 5mm after total hip arthroplasty are associated with altered gait kinematics. Gait Posture. 2016;49:196. doi: 10.1016/j.gaitpost.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 19.Clement N.D., S Patrick-Patel R., MacDonald D., Breusch S.J. Total hip replacement: increasing femoral offset improves functional outcome. Arch Orthopaedic Trauma Surg. 2016;136(9):1317. doi: 10.1007/s00402-016-2527-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brown T.S., Banerjee S., Russell R.D., Mont M.A., Huo M.H. What’s new in total hip arthroplasty. J Bone Joint Surg. 2014;96(18):1576. [Google Scholar]
- 21.Rodriguez J.A., Deshmukh A.J., Rathod P.A. Does the direct anterior approach in THA offer faster rehabilitation and comparable safety to the posterior approach? Clin Orthopaedics Relat Res. 2014;472(2):455. doi: 10.1007/s11999-013-3231-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.El Bitar Y.F., Stone J.C., Jackson T.J., Lindner D., Stake C.E., Domb B.G. Leg-length discrepancy after total hip arthroplasty: comparison of robot-assisted posterior, fluoroscopy-guided anterior, and conventional posterior approaches. Am J Orthopedics (Belle Mead, NJ) 2015;44(6):265. [PubMed] [Google Scholar]
- 23.Hartford J.M., Bellino M.J. The learning curve for the direct anterior approach for total hip arthroplasty: a single surgeon's first 500 cases. J Clin Exp Res Hip Pathol Ther. 2017;27(5):483. doi: 10.5301/hipint.5000488. [DOI] [PubMed] [Google Scholar]
- 24.Dastane M., Dorr L.D., Tarwala R., Wan Z. Hip offset in total hip arthroplasty: quantitative measurement with navigation. Clin Orthopaedics Relat Res. 2011;469(2):429. doi: 10.1007/s11999-010-1554-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jasty M., Webster W., Harris W. Management of limb length inequality during total hip replacement. Clin Orthopaedics Relat Res. 1996;(333):165. [PubMed] [Google Scholar]
- 26.Lin T.J., Bendich I., Ha A.S., Keeney B.J., Moschetti W.E., Tomek I.M. A comparison of radiographic outcomes after total hip arthroplasty between the posterior approach and direct anterior approach with intraoperative fluoroscopy. J Arthroplasty. 2017;32(2):616. doi: 10.1016/j.arth.2016.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sealed Envelope Ltd . 2012. Power calculator for continuous outcome equivalence trial [Online] https://www.sealedenvelope.com/power/continuous-equivalence/ [accessed 08.01.18] [Google Scholar]
- 28.Julious S.A. Sample sizes for clinical trials with normal data. Stat Med. 2004;23:1921. doi: 10.1002/sim.1783. [DOI] [PubMed] [Google Scholar]
- 29.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159. [PubMed] [Google Scholar]
- 30.McNabb D.C., Jennings J.M., Levy D.L., Miner T.M., Yang C.C., Kim R.H. Direct anterior hip replacement does not pose undue radiation exposure risk to the patient or surgeon. J Bone Joint Surg Am. 2017;99(23):2020. doi: 10.2106/JBJS.17.00351. [DOI] [PubMed] [Google Scholar]
- 31.Sayed-Noor A.S., Hugo A., Sjoden G.O., Wretenberg P. Leg length discrepancy in total hip arthroplasty: comparison of two methods of measurement. Int Orthopaedics. 2009;33(5):1189. doi: 10.1007/s00264-008-0633-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ogawa K., Kabata T., Maeda T., Kajino Y., Tsuchiya H. Accurate leg length measurement in total hip arthroplasty: a comparison of computer navigation and a simple manual measurement device. Clin Orthop Surg. 2014;6(2):153. doi: 10.4055/cios.2014.6.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weber M., Woerner M., Springorum R. Fluoroscopy and imageless navigation enable an equivalent reconstruction of leg length and global and femoral offset in THA. Clin Orthopaedics Relat Res. 2014;472(10):3150. doi: 10.1007/s11999-014-3740-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.