Abstract
Targeted drug delivery by nanoparticles (NPs) is an essential technique to achieve the ideal therapeutic effect for cancer. However, it requires large amounts of work to imitate the biomarkers on the surface of the cell membrane and cannot fully retain the bio-function and interactions among cells. Cell membranes have been studied to form biomimetic NPs to achieve functions like immune escape, targeted drug delivery, and immune modulation, which inherit the ability to interact with the in vivo environments. Currently, erythrocyte, leukocyte, mesenchymal stem cell, cancer cell and platelet have been applied in coating photothermal agents and anti-cancer drugs to achieve increased photothermal conversion efficiency and decreased side effects in cancer ablation. In this review, we discuss the recent development of cell membrane-coated NPs in the application of photothermal therapy and cancer targeting. The underlying biomarkers of cell membrane-coated nanoparticles (CMNPs) are discussed, and future research directions are suggested.
Keywords: cell membrane, nanoparticles, photothermal therapy, cancer targeting
Introduction
Cancer is one of the leading causes of death worldwide. According to the World Health Organization (WHO), the number of cancer-related mortalities per year is predicted to increase by 45% from 2007 to 2030. However, the non-targeted distribution of theranostic agents throughout the body and the poor targeting ability and bioavailability tend to demonstrate rapid excretion and severe toxicity, and thus, they require large dosages to achieve the ideal concentration in the targeted site.
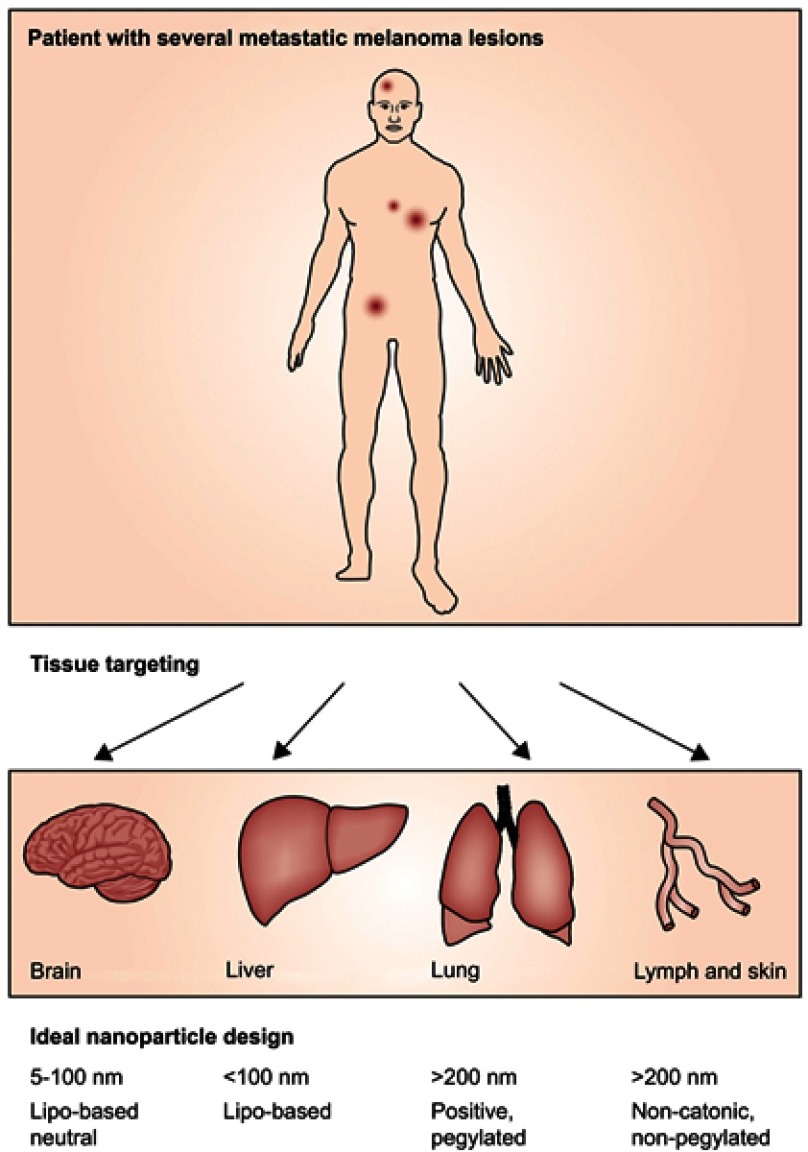
Since its first observation in the 1980s, the enhanced permeation and retention (EPR), which refers to the ability of solid tumors in animal models to selectively accumulate and retain polymeric drugs and nanomedicines,1,2 has been widely used in the design of anti-cancer drugs. Due to the EPR effect, nanoparticles (NPs), with the modification of shape, size and surface properties, have preferential accumulation in the tumor area (Figure 1). Nanotechnology has been rapidly developed and applied in various areas of biomedical research, including targeted drug delivery, vaccination,3,4 gene delivery,5 antimicrobial,6 tissue engineering,7 monitoring cancer cells’ phenotypic evolution during therapy to provide advice for treatment adjustment,8 and photothermal therapy (PTT).9–12
Figure 1.
Schematic strategy of effective designed nanoparticles for advanced stage melanoma. Reprinted from The Lancet Oncology, 15/1, Bombelli FB, Webster CA, Moncrieff M, Sherwood V. The scope of nanoparticle therapies for future metastatic melanoma treatment, e22-e32, Copyright (2014), with permission from Elsevier..110
PTT is a laser-based technique that requires optical absorbing agents to effectively convert energy from laser irradiation into heat to kill cancer cells, it is highly selective and can minimize the damage to the non-targeted regions.13 The current optical absorbing agents include various inorganic and organic nanoparticles with strong near infrared (NIR) absorbance. However, those synthetic NPs are exogenetic to the human body, and underlying concerns like easy recognition and capture by the reticuloendothelial system, and antibodies generated against those NPs causing early elimination from the blood have been raised. Moreover, safety concerns about non-biodegradable inorganic materials such as oxidative stress and lung inflammation, impaired efficiency of anti-tumor ability are asked by researchers. Answer to these questions, many approaches have been developed.14–16 Polyethylene glycol (PEG) modification of NPs has been made to enhance the longevity in blood circulation. However, anti-PEG immune response, renal damage and complex synthesis procedures still concern researchers.14 Some biomimetic NPs have been designed to imitate the extremely abundant protein and antigens associated with the biological function of the cell membrane. However, the process is rather complex and the results are barely satisfactory.
Since the 20th century, cells were employed to traffic drugs in treatment.17–20 However, concerns have been raised since drugs can be degraded or exocytosed by living cells, which will largely decrease the therapeutic effect of drugs. Furthermore, cells used in this kind of method are limited to normal cells, since the safety concerns will be raised genetically about the potential pathogenic ability if cells like tumor cells are considered.21 Beside cells, lipid-based nanoparticles have been developed as a cancer-targeted theranostic agent to achieve the purpose of diagnosis and treatment of cancer, as well as the monitoring of drug distribution.22,23 However, concerns about long-term safety for in vivo applications still exist.22 Furthermore, exosomes, extracellular vesicles which can bypass biological barriers including the blood brain barrier, have been considered as promising drug delivery carriers. Despite advantages like high stability in blood and immune tolerance, the application of exosomes is limited by the low quantity released by cells and the complicated purification procedure.24,25
In recent researches, cell membrane-coated nanoparticles (CMNPs) have demonstrated their unique ability of targeting, precisely delivering and controlling release of drugs in cancer sites, and immune activation. The functionality and complexity of cell membrane combined with the variability of the NPs lead to the high adaptability of CMNPs to the specific microenvironment of tumors and the intention of treatment. With the decoration of cell membrane, CMNPs can acquire various functions of different sources of cells, including the extravasation, chemotaxis, and cancer cell adhesion function of cancer cells if their membranes are collected. Moreover, the lipid bilayer provides an ideal foundation for the surface modification with a peptide or an antibody to achieve the goal of active targeting without damaging the existing membrane protein.26 Currently, membranes of erythrocytes, immune cells, platelets, stem cells, endothelial cells, activated fibroblast cells and even cancer cells have been studied for their abilities as a carrier.27–33
Cell membrane camouflaged delivery system has been widely used in various fields, including drug delivery for the treatment of cancer19,34–36 or other diseases like inflammatory arthritis,37 deadly bacterial infections,38–40 imaging (MRI, fluorescence/photoacoustic imaging),28,33,41–43 anticancer vaccination,44 detoxification,45 and virus detecting.46 In this article, we aim to provide an up-to-date review of various membrane-derived CMNPs for the PTT of cancer and the reported methods to collect and purify membranes.
Membrane sources for CMNPs
Erythrocytes
Erythrocytes are one of the most abundant cell types in blood. Since the first blood transfusion performed in 1667, it has become an important emergency and inpatient treatment in clinical application. Moreover, it lacks organelles like a cell nucleus and mitochondria, which is convenient for membrane extraction and purification. Erythrocytes have demonstrated their promising potential in the treatment of various diseases as long as the blood types match with the donor free of infectious diseases.
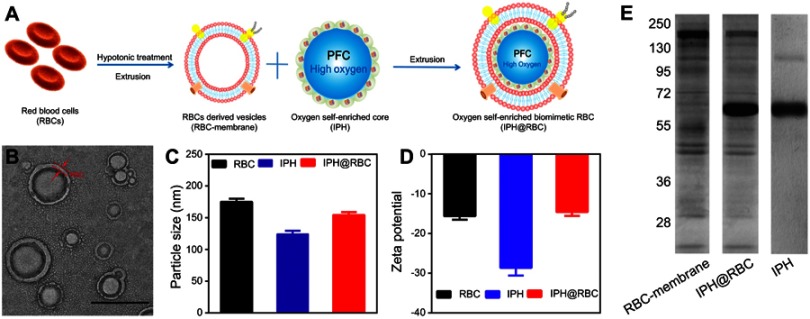
Red blood cells (RBCs) membrane was the first to be used to form cell membrane-coated nanoparticles, which were first derived by hypotonic treatment in 2011 by Che-Ming J. Hu and colleagues.29 Many researches regarding RBC-coated NPs were conducted after the first introduction. Ren et al47 designed oxygen self-enriched RBCs with a long circulation time and high oxygen capacity (Figure 2A). Transmission electron microscopy (TEM) revealed a core-shell structure as expected in a lipid bilayer-coated polymeric particle with approximately 70 nm-diameter polymeric core and an outer lipid shell 7–8 nm in thickness (Figure 2B). The hydrodynamic diameters (Figure 2C). and zeta potentials (Figure 2D) measured 180 nm and −16 mV, respectively. It is reported that RBC membrane can completely shield and stabilize NPs by lipid membranes and surface glycans, and can successfully coat nanoparticle substrates between 65 and 340 nm in diameter with the cell surface proteins retained in a right-side-out manner.48
Figure 2.
(A) Schematic preparation of CMNPs (B) TEM images of RBC-NPs. The mean particle size (C) and zeta potential (D) of NPs and RBC membranes. (E) SDS-PAGE protein visualization of RBC-membrane, IPH and purified RBC-membrane-camouflaged IPH nanoparticles. Reprinted from Biomaterials, 59, Hao R, Liu J, Li Y, et al.Oxygen self-enriched nanoparticles functionalized with erythrocyte membranes for long circulation and enhanced phototherapy. 59:269, Copyright (2017), with permission from Elsevier.47
Abbreviations: CMNPs, cell membrane-coated nanoparticles; TEM, transmission electron microscopy; RBC-NPs, red blood cell nanoparticles; IPH, human serum albumin nanoparticles.
RBC can achieve immune-evasive by the interaction of CD47, a marker on RBC membrane, with SIRPα, expressed by phagocytic cells, to inhibit phagocytosis of RBCs by immune cells.49 Besides RBCs, CD47 and its analogs have been proved to contribute to the in vivo survival of cancer cells50 and viruses.51 Careful studies about the surface properties of RBC-NPs showed the formed NPs possess similar density of CD47 to the source RBCs.52 More importantly, with the electrostatic repulsion between the negatively charged NPs core and the negatively charged extracellular side of the membranes, the surface proteins were proved to be oriented almost exclusively in the right-side-out fashion, with the extracellular part displayed on the RBC-NPs surface.48 Moreover, the composition of membrane proteins was mostly retained on the RBC-NPs (Figure 2E), with most of the functions of RBC inherited by the coated-NPs and demonstrating longer elimination half-life than bare NPs.29
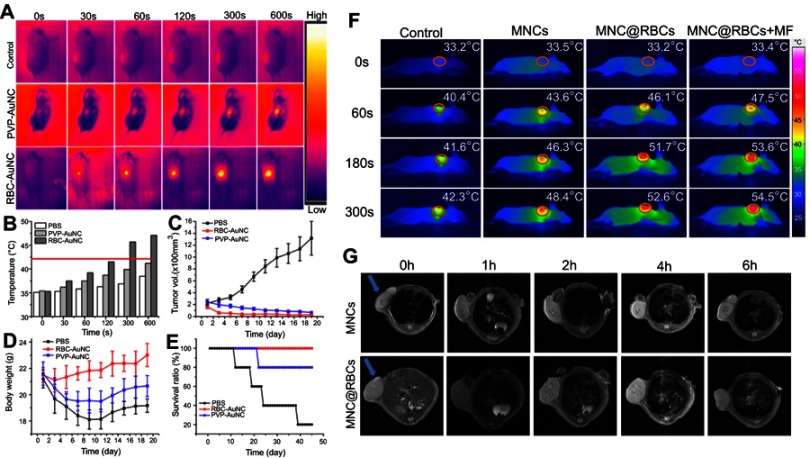
In PTT cancer treatment, RBC-NPs showed improved efficacy with the faster decrease of tumor volumes and higher survival rate than bare NPs53 (Figure 3A–E). By coating RBC membrane onto iron oxide magnetic clusters, the NPs demonstrated increased MRI imaging and heat converting ability,41 the properties which iron oxide already own54 (Figure 3F–G). It can be speculated that, the RBC-NPs inherited the photothermal conversion effects from the inner cores and the long blood retention from the RBC membrane coating. Besides coating the synthetic NPs with a membrane, chemotherapy agents can also be camouflaged. It has been demonstrated that the hypoxic environment of tumor tissue may promote the growth and metastasis.55 Qian et al30 designed a NP-RBC membrane camouflaged Prussian blue/manganese dioxide (PBMn) to efficiently catalyze the relatively abundant H2O2 in the tumor microenvironment, along with doxorubicin (DOX), to achieve the purpose of relieving hypoxia and improving photothermal conversion efficacy. Under irradiation for 5 minutes, the tumors treated by PBMn-DOX@RBC reached 59.6°C, while tumors treated by PBMn reached only 49.3°C. Researchers also studied the combination of non-toxic and biodegradable natural melanin nanoparticles extracted from living cuttlefish and RBC membrane.34 This NP inherited photoacoustic (PA) imaging capability, optimal accumulation in tumors, and significantly higher PTT efficacy. A study combining the photosensitizer (PS) of photodynamic therapy (PDT) and agents meditating PTT showed enhanced tumor ablation ability.47
Figure 3.
(A) Thermographs of mice injected with the RBC-AuNPs and the pristine PVP-AuNPs after 48 hours. The mice were irradiated with an 850 nm laser (1 W/cm2). (B) Tumor site temperature based on thermographs of mice in (A). Red line indicates the lowest cancerous cells ablation temperature –42°C. (C) Graphs of the average tumor volume. (D) Graphs of the average mouse body weight. (E) Graphs of the mouse survival ratio. (F) Thermographs of tumor-bearing mice under an 808 nm NIR laser exposure (5 W/cm2) for 0–300 seconds. (G) After intravenous injection with MNCs and MNC@RBCs, T2-weighted MR images of tumor-bearing mice were taken at different time points. Blue arrows indicate the tumor locations. 41,53 Reprinted from Biomaterials, 92, Ren X, Zheng R, Fang X, et al. Red blood cell membrane camouflaged magnetic nanoclusters for imaging-guided photothermal therapy. 13–24, Copyright (2016), with permission from Elsevier.41 Reprinted with permission from Piao J-G, Wang L, Gao F, You Y-Z, Xiong Y, Yang L. Erythrocyte membrane is an alternative coating to polyethylene glycol for prolonging the circulation lifetime of gold nanocages for photothermal therapy. ACS Nano. 2014;8(10):10414–10425. doi:10.1021/nn503779d. Copyright 2014 American Chemical Society.53
Notes: Fig 3 parts F, G is taken from reference 41, parts A-E is taken from reference 53.
Abbreviations: MNCs, iron oxide magnetic nanoclusters; MNC@RBCs, RBC membrane camouflaged iron oxide magnetic clusters; MF, magnetic field.
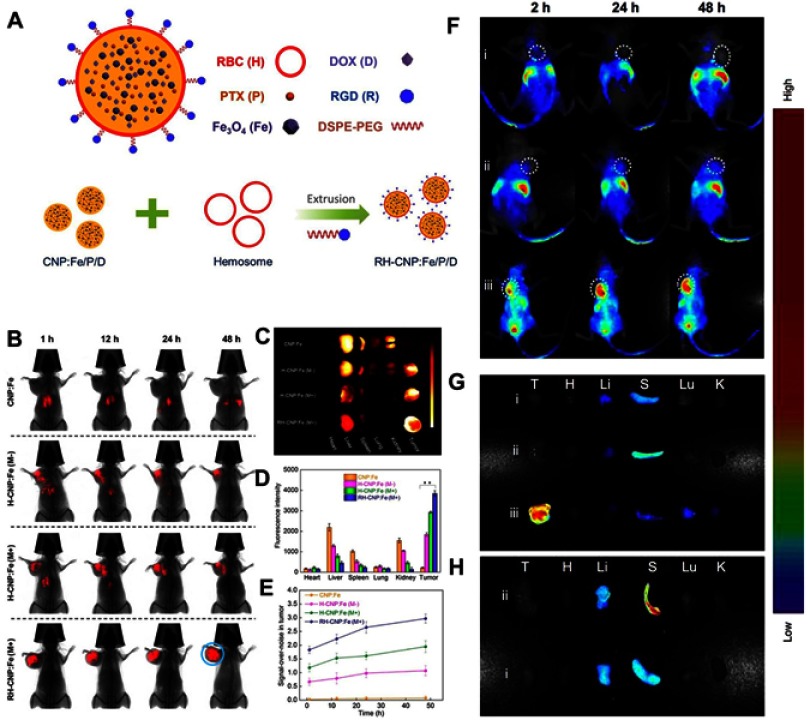
However, despite the immune escape and long blood retention time for RBC-NPs, the ability to actively target cancer cells and accumulate in cancer tissues is not satisfying. Chemical synthesis is a common way to introduce targeting ligands to the surface of cell membrane, however, it may damage the property and protein components of the membrane, which the functions of cell membrane are based on. Based on this consideration, a lipid-insertion approach has been developed.26,35,56,57 Fu et al35 designed a DSPE-PEG (1,2-distearoyl-sn-glycero-3-phosphoethanolamine-PEG) decorated cyclic Arg-Gly-Asp (RGD), which could be simultaneously inserted into the phospholipid layer of erythrocyte membranes. This process achieved prolonged circulation time, increased tumor uptake and accumulation, and lead to remarkably reduced tumor cell viability to 20%, improved survival rate, and decreased side effects (Figure 4A–E). It has been approved that the lipid-insertion approach can enhance the tumor-targeting ability of NPs56 (Figure 4F–H). Fang et al26 demonstrated that the lipid-insertion method can be applied to ligands of different molecular weights, including relatively large targeting ligands. Moreover, ligand density on the membranes can be adjusted by controlling the lipid-tethered ligand input. Liu et al58 designed epithelial cell adhesion molecule (EpCam)-RPAuNs, which is Au nanocages (AuNs) encapsulated antitumor drug paclitaxel coated by anti-EpCam antibodies modified RBC membranes. EpCam-RPAuNs showed increased cancer targeting ability by anti-EpCam antibodies, and the paclitaxel can be released when membrane was destroyed by heat generated by AuNs under laser irradiation to exert anti-cancer effects.
Figure 4.
(A) Schematic fabrication process depicting RBC membrane camouflaged programmed co-delivery system. (B) In vivo images of tumor targeting abilities of CNP:Fe, H-CNP:Fe, and RH-CNP:Fe with or without an external magnetic field. (C) Ex vivo optical images of tumors and major organs of tumor-bearing mice sacrificed at 48 hours. (D) Tissue distribution of different NPs in tumor-bearing mice 48 hours post-treatment. (E) The graph of the comparison of signal-over-noise ratios of fluorescence in tumor at different time point. (F) In vivo fluorescence imaging of tumor-bearing nude mice at 2, 24, and 48 hours post-intravenous injection of RBC-PTX (i), anti-EGFR-iRGD and RBC-PTX co-administration (ii) and PRP (iii). The white colored dotted circles indicated the tumor sites. (G) Ex vivo fluorescence imaging of the excised tumors and major organs at 48 hours post-injection. (H) Ex vivo fluorescence imaging of the excised tumors and major organs at 48 hours post-injection of group i and ii. Republished with permission of Royal Society of Chemistry, from Programmed co-delivery of paclitaxel and doxorubicin boosted by camouflaging with erythrocyte membrane, Fu Q, Lv P, Chen Z, et al, 7, 2015; permission conveyed through Copyright Clearance Center, Inc.35 Copyright ©2018. Dove Medical Press. Reproduced from Chen H, Sha H, Zhang L, et al.Lipid insertion enables targeted functionalization of paclitaxel-loaded erythrocyte membrane nanosystem by tumor-penetrating bispecific recombinant protein. Int J Nanomedicine. 2018;13:5347–5359. doi:10.2147/IJN.S165109.56
Notes: Fig 4 parts A-E is taken from reference 35, parts F-H is taken from reference 56.
Abbreviations: PTX, paclitaxel; RGD, Arg-Gly-Asp; DSPE-PEG, 1,2distearoyl-sn-glycero-3-phosphoethanolamine-polyethylene glycol; CNPs, O-carboxymethyl-chitosan (CMC) nanoparticles; PRP, anti-EGFR-iRGD-RBCm-PTX.
Leukocytes
Leukocytes are a cell population which includes granulocytes, monocytes and lymphocytes. They are widespread in blood vessels and lymphatic vessels as well as other tissues due to the amoeboid movement, which enables leukocytes to migrate between extravascular tissues and vessels. Chronic inflammation has been featured as one of the major characteristics of cancers in various stages, which may be partly due to the altered tissue homeostasis and integrity.59 Thus, various kinds of inflammatory cells are attracted by various cytokines, chemokines and prostaglandins produced by cancer cells and involved in progression of the tumor.60 The study by Zhang et al61 showed CXCR2, and LFA-1 play a key role in leukocyte homing to inflamed sites. However, some immune cells finally turn into an accomplice to cancer, like tumor-associated macrophages (M2 subtype) or fibroblasts, which associate with active promotion of tumorigenesis and inhibition of a protective immune response. Moreover, myeloid-derived suppressor cells recruited by CCL2, CXCL5, CXCL12 and stem cell factor secreted by tumor cells can suppress T cell function.62,63 Currently, various treatments have been developed targeting immune cells, including but not limited to anti-cytotoxic-T lymphocyte protein-4 and anti-programmed cell death 1 ligand 1 antibodies, macrophage colony-stimulating factor receptor inhibitors, and CD40 agonist CP-870,893 (Pfizer Inc., New York, NY, USA), they have achieved increased efficacy but not enough targeting ability.32 However, the inflammation and tumor targeting ability of leukocyte makes it a potential candidate for the design of biomimetic NPs in PTT.
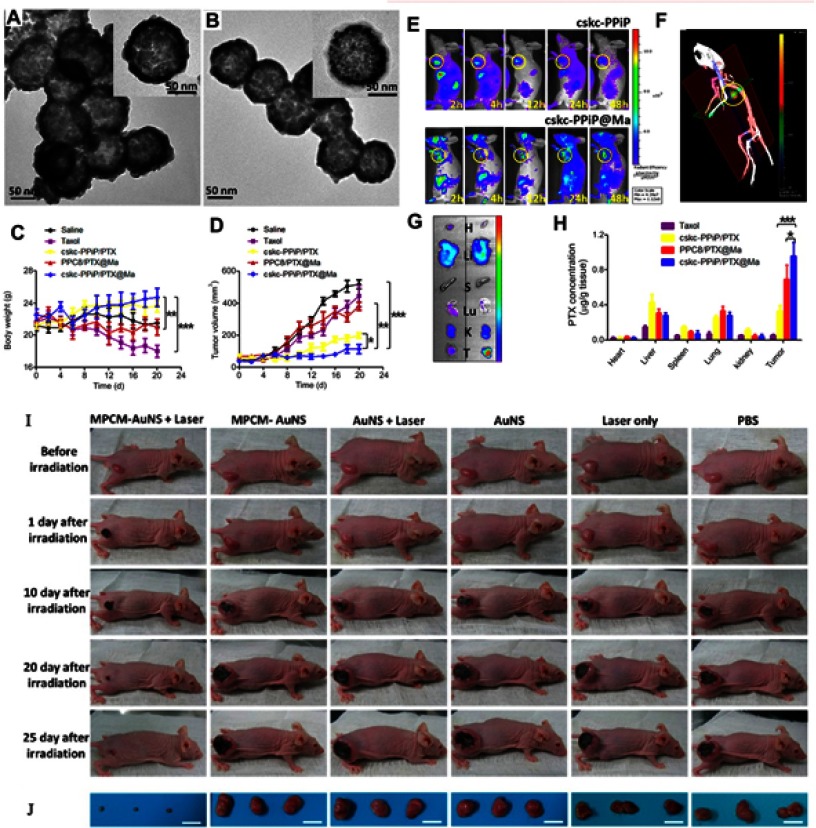
A large number of leukocytes associated with cancer immunology are macrophages. It can recognize and engulf cancer cells and any substances that do not have the specific biomarkers on their surface. The innate inflammation-directed chemotactic ability of macrophages could bring the carried agents to accumulate in chronic inflammatory tumor tissue.64 In 2013, Tasciottet al65 used leukocytes to derive cellular membranes, and coated nanoporous silicon particles to form leukolike vectors (LLVs). This design showed enhanced circulation time and improved accumulation in a tumor. For particles coated with J774 macrophage-like and THP-1 cell membrane, there was a 75% and 50% decrease in uptake by their source cells, respectively. Biomarkers and adhesion molecules used for vascular extravasation, like CD45, CD3z and CD11a were retained in the surface of LLVs, which may contribute to the reduced particle opsonization, delayed phagocytic uptake, increased trans-endothelium and targeted ability. Followed this study, many researches have been carried out using macrophage membrane. Meng et al66 collected macrophage membrane-derived vesicles and then coated them onto Fe3O4 NPs, a kind of nanomaterial that has been licensed by the Food and Drug Administration (FDA). The derived NPs demonstrated favorable biocompatibility, immune evasion ability through CD47, a biomarker that embedded in cell membranes, ideal cancer targeting ability and photothermal efficiency. Another study combined macrophage cell membrane and gold NPs (AuNPs) to achieve enhanced blood circulation time and local accumulation at the tumor, which is 83.18% of the coated NPs were internalized by 4T1 cancer cells incubated for 24 hours, whereas only 42.15% of the AuNPs were taken up. And thus, the increased taking up leads to increased PTT efficacy of AuNPs67 (Figure 5A–B, I–J).
Figure 5.
(A, B) TEM images of AuNPs, and macrophage cell membrane-camouflaged AuNPs, respectively. (C) Body weight and (D) tumor volume data were recorded in the course of 3-week treatment. (E) IVIS images of mice injected with cskc-PPiP and cskc-PPiP@ Ma loaded with near-infrared probe. (F) 48 hours post-treatment, 3D reconstruction of fluorescence signal were conducted in cskc-PPiP@Ma-treated mouse. (G) Major organs like heart (H), liver (Li), spleen (S), lung (Lu), kidney (K), and tumor (T) excised from the cskc-PPiP and cskc-PPiP@ Ma injected mouse. (H) Quantification of PTX concentration in organs and tumor tissue excised from mice treated with Taxol, cskc-PPiP/PTX, PPC8/PTX@Ma, and cskc-PPiP/PTX@Ma (n=4). (I) Photographs of the tumor region were taken after 5 minutes of 1 W/cm2 NIR irradiation. (J) Photographs of relevant tumors in accordance with each group in (I). All scale bars are 2 cm. Reprinted with permission from Xuan M, Shao J, Dai L, Li J, He Q. Macrophage cell membrane camouflged Au nanoshells for in vivo prolonged circulation life and enhanced cancer photothermal therapy. ACS Appl Mater Interfaces. 2016;8(15):9610–9618. doi:10.1021/acsami.6b00853. doi:10.1021/nn503779d. Copyright 2016 American Chemical Society.67 Reproduced with permission from Refs.67 Reprinted with permission from Zhang Y, Cai K, Li C, et al. Macrophage-membrane-coated nanoparticles for tumor-targeted chemotherapy. Nano Lett. 2018;18(3):1908–1915. doi:10.1021/acs.nanolett.7b05263. Copyright 2018 American Chemical Society.68
Notes: Fig 5 parts A, B, I, J is taken from reference 67, parts C-H is taken from reference 68.
Abbreviations: MPCM, macrophage cell membrane; AuNSs, gold nanoshells; PPiP, cationic 2aminoethyldiisopropyl group; PPC8, pH-insensitive polymer with neutral octyl group side chains.
It has been proved that macrophage membrane-coated NPs can achieve tumor-targeted chemotherapy delivery with a controlled release profile in response to tumor microenvironment stimuli.68 Zhang et al68 designed a step-by-step release strategy using the reduced pH in tumor microenvironment. After the eruption of coated membrane caused by interstitial pH of tumor tissue, the inner core will be taken up by tumor cells and intracellular pH of the tumor cells will lead to the release of chemo-drugs in NPs. Their resulting formulation (cskc-PPiP/PTX@Ma) exhibited favorable tumor-homing ability in systemic circulation and high biocompatibility (Figure 5C–H). A Janus particle designed by He et al69 is half cloaked by Au shell and half cloaked by THP-1 cellular membrane, and achieves improved cancer cell targeting ability, strong near infrared (NIR) absorption and ideal photothermal efficacy: the laser density of 23.6 mW/μm2 correlates to a temperature of 70−90°C on the fully gold-coated side and 40−45°C of the half-coated side due to a thinner gold layer and incomplete coating. Those two kinds of designs providedus with a new perspective of combining the cell membrane and photothermal agents according to the unique properties of the cancer microenvironment.
Besides macrophage, cytotoxic T-lymphocyte (CTL) membrane is another studied leukocyte membrane in the delivery of NPs. CTL can specifically recognize the antigen on the surface of tumor cells, which is presented by the antigen presenting cell, and activate anti-tumor immune response. Thus, the ability to be recruited and localized at tumor sites makes CTL an ideal candidate to create biomimetic delivery system. Studies about the combination of CTL membrane-coated NPs and local low-dose irradiation (LDI) demonstrated that camouflaging with CTL membranes would prolong the circulation time and improve tumor targeting ability. Moreover, LDI may increase the expression level of ICAM-1, a ligand for LFA-1.70 During the process of leukocyte adhesion, the interaction between LFA-1 and ICAM-1 is important, and it may also attribute to the localization of leukocytes in tumors. This reminds us that when we make use of the existing properties of cells, an additional treatment can be applied to enhance it. It may be applicable to combine the LDI and PTT to achieve greater efficacy.
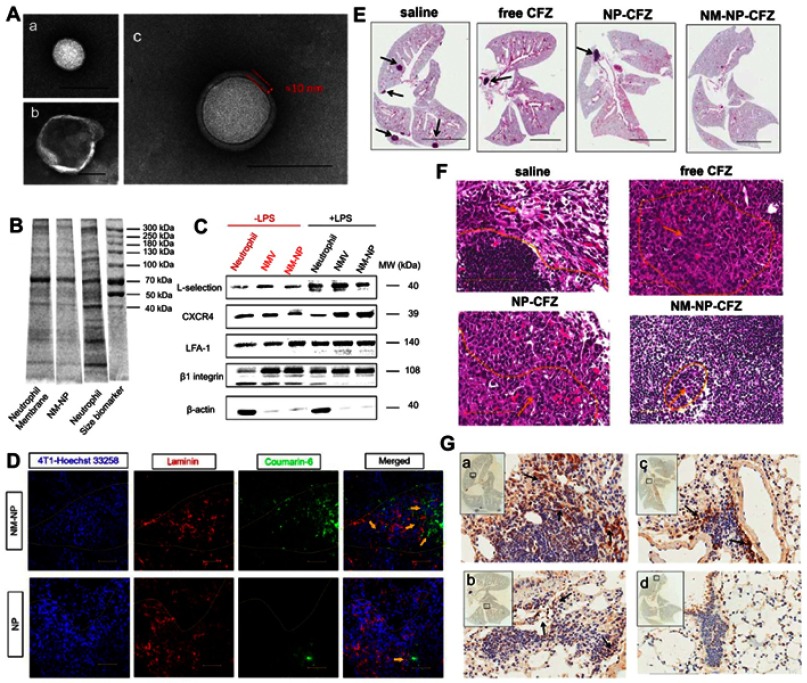
In the progression of malignant tumors, distant metastasis mostly results from dissemination, seeding, and colonization of circulating tumor cells (CTCs). Among all the immune response cells, inflammatory neutrophils possess a CTC-targeting property which depends largely on the distinct adhesion molecules on the membrane of neutrophils, and can regulate the adhesion process of metastasis.71 A study combined poly(lactic-co-glycolic acid) (PLGA) NPs and neutrophil membranes showed the formed neutrophil-mimicking nanoparticles (NM-NPs) can retain most of the membrane protein (Figure 6A,B), and functional adhesion proteins like L-selectin, LFA-1, β1 integrin, CXCR4 are fully preserved (Figure 6C). Compared with PLGA NPs, NM-NPs could capture CTCs and target metastasis lesions more efficiently, and show lower toxicity (Figure 6D–G). More importantly, it displayed the ability of prevention of the formation of early metastasis and the progression of already formed metastatic lesions.36 Compared with other cell types, monocyte is a relatively less studied membrane source in delivering NPs. Chan et al31 combined a drug-loaded PLGA core with monocyte cell membrane-derived shell to derive core-shell type “nanoghosts” with the ability of enhanced target specificity and efficacy.
Figure 6.
(A) TEM images of (a) bare PLGA NPs, (b) NMVs, and (c) NM-NPs. Scale bar is 100 nm. (B) SDS-PAGE protein tracking of the neutrophils membrane, NM-NPs, and neutrophils, respectively. (C) Western-blot identification of membrane-associated adhesive proteins with and without LPS stimulation. (D) Confocal microscopy analysis of NPs targeting pre-metastatic region in a mouse model (n=3). The injected NPs and NM-NPs were labeled with coumarin-6 (coumarin-6 dosage of 1 mg/kg). Scale bar, 50 μm. (E) H&E staining pictures of lung tissues after mice were treated with saline, free CFZ, NP-CFZ, and NM-NP-CFZ, respectively. Arrows points out metastatic nodules. Scale bar, 5 mm. (F) Histological analysis of cancer cells infiltration in lymph node after the same treatment in (E), n=3. Scale bar, 100 μm. (G) The evaluation of the ability of NM-NP-CFZ, NP-CFZ, and free CFZ to inhibit neutrophils recruitment in mice lungs by immunological staining with S100A9 (brown), n=3. The lung tissues are in accordance with (E). Arrows were pointed to S100A9-positive cells. S100A9 is a cytoplasm protein secreted by neutrophils at the site of inflammation. Scale bar, 100 μm. Reprinted with permission from Kang T, Zhu Q, Wei D, et al.Nanoparticles coated with neutrophil membranes can effectively treat cancer metastasis. ACS Nano. 2017;11:1397–1411. doi:10.1021/acsnano.6b06477. Copyright 2017 American Chemical Society.36
Abbreviations: NMV, Neutrophil-derived membrane vesicles; NM-NP, neutrophil-mimicking nanoparticle; CFZ, carfilzomib.
Cancer cells
Unlike other kinds of cells, cancer cells possess their unique characteristics like enabling replicative immortality, inducing angiogenesis, homologous targeting abilities and activating invasion and metastasis.72 Studies have indicated that interactions of surface adhesion molecules like T antigen-galectin-3,73 and EpCAM74 mediate homotypic intercellular adhesion of metastatic malignant tumor cells. The homotypic binding phenomenon allows tumor cells to bind with each other and leads to the rapid growing of metastatic masses.
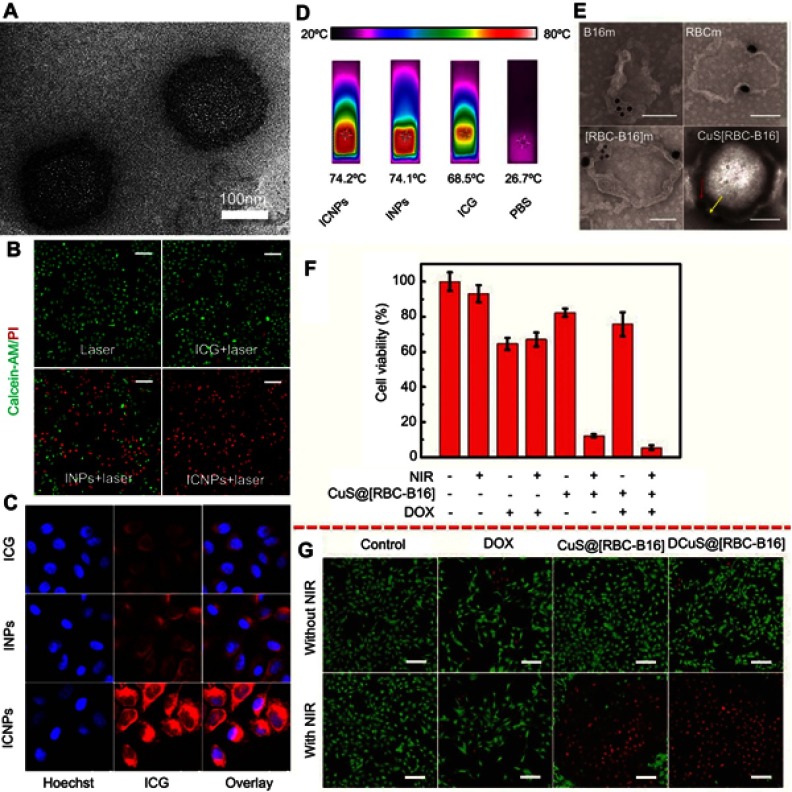
Since normal cells like RBC and WBC cannot efficiently target malignancies, the intercellular homologous binding capability of cancer cells have attracted the attention of researchers. Thus, surface modification of NPs by cancer cell membrane is being studied in current researches. A study conducted by Cai et al28 combined the fluorescence (FL)/PA imaging and photothermal ability of indocyanine green (ICG) and homologous targeting ability of cancer cell membrane to form the ICNP, a membrane-coated NP, which realize the purpose of high tumor accumulation, real-time dual-modal imaging with high spatial resolution, and significantly enhanced PTT efficiency. Under continuous laser irradiation for 8 minutes, the maximum temperature of free ICG, PBS and ICNPs reached 68.4°C, 27.6°C and 74.2°C, respectively. Magnetic nanobead with the ability of MR/NIR fluorescence imaging and cancer cell membrane with homing ability are also being studied43(Figure 7A–D).
Figure 7.
(A) TEM images of ICNPs. (B) Fluorescence images of MCF-7 cells stained with calcein-AM/PI, which were treated with laser, ICG + laser, INPs + laser, or ICNPs + laser. Scale bar, 100 µm. (C) Confocal microscopy images of MCF-7 cells treated with free ICG, INPs, or ICNPs. (D) The infrared thermographic images of ICNPs, INPs, free ICG and PBS after 8 mins continuous laser irradiation at power density 1 W/cm2. (E) Immunogold TEM images of B16-F10, RBC, RBC-B16 membrane, and CuS@[RBC-B16] NPs samples probed for CD47 (red arrows, large gold) and gp100 (yellow arrows, small gold), followed by negative staining with uranyl acetate (scale bars =100 nm). (F) The cell viabilities of B16-F10 cells with different combination of CuS@[RBC-B16] NPs, DOX, NIR. (G) Confocal fluorescent microscopy images of live/dead staining of B16-F10 cells treated with different materials with or without 1,064 nm NIR laser irradiation at power dense 1.0 W/cm2. Scale bar is 100 µm. Reprinted with permission from Chen Z, Zhao P, Luo Z, et al.Cancer cell membrane-biomimetic nanoparticles for homologous-targeting dual-modal imaging and photothermal therapy. ACS Nano. 2016;10(11):10049. doi:10.1021/acsnano.6b04695. Copyright 2016 American Chemical Society.28 Reprinted with permission from Wang D, Dong H, Li M, et al. Erythrocyte-cancer hybrid membrane camouflaged hollow copper sulfide nanoparticles for prolonged circulation life and homotypic-targeting photothermal/chemotherapy of melanoma. ACS Nano. 2018.12(6);5241–5252. Copyright 2018 American Chemical Society.75
Notes: Fig 7 parts A-D, is taken from reference 28, 7 parts E-G is taken from reference 75.
Abbreviations: INPs, PEGylated phospholipid and soybean lecithin shell coated ICG-PLGA core.
Current studies have combined the membrane materials derived from cancer cells and other cell types, like erythrocytes. A study created a hybrid biomimetic coating by fusing membrane of RBCs and melanoma cell line (B16-F10 cells) together, and camouflaged DOX-loaded hollow copper sulfide nanoparticles, to achieve prolonged blood retention time, enhanced homogenous targeting abilities, and excellent synergistic photothermal/chemotherapy inherited from the components of NPs. These synthetic NPs achieved about 100% melanoma tumor growth inhibition rate75 (Figure 7E–G).
Platelets
Platelets (PLT), also called thrombocytes, are fragments of the cytoplasm of megakaryocytes originating from the bone marrow, and then entering the circulation. The circulation lifetime of platelets is approximately 7–10 days. The main function of platelets is to contribute to hemostasis. It has also been found that activated platelets are able to participate in adaptive immunity by releasing antimicrobial peptides, defensins, and proteases against bacteria. It is demonstrated that platelets can recognize CTCs and protect tumor cells from immune elimination and promote their adhesion to the endothelium through the surface molecules and released factors.76 The interaction between PLT and cancer cells is mainly through P-selectin and CD44, which are expressed in PLT and many cancer cells, respectively.77 This adhesion is named as tumor cell-induced platelet aggregation (TCIPA).78
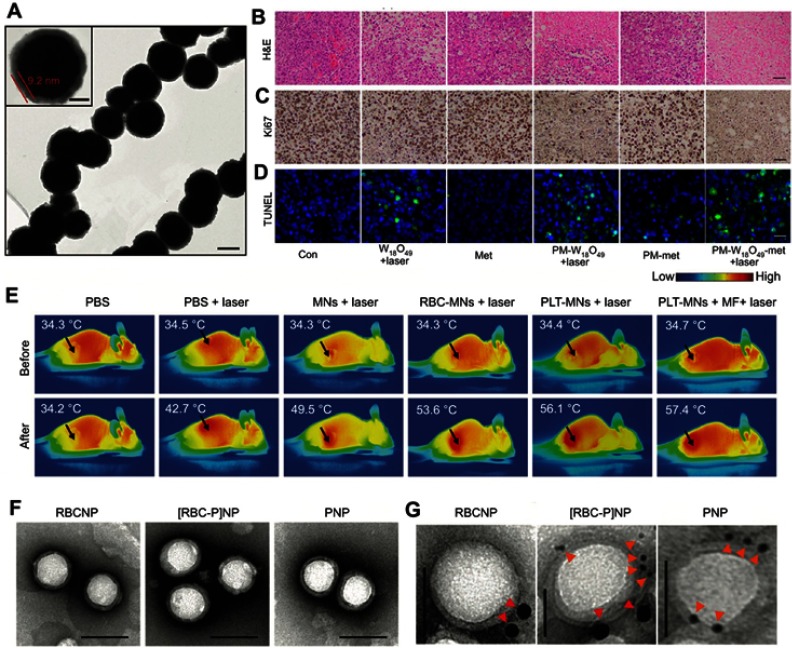
Membranes derived from platelets have been coated onto NPs like Fe3O4 to enable long circulation, cancer targeting capabilities from PLT, and imaging, optical absorption properties and PTT ability from NPs79 (Figure 8A, E). Besides the general benefits obtained from membrane coating, Rao et al79 found PTT treatment could facilitate PLT-NPs gathering in the PTT sites. This phenomenon mainly results from the function of PLTs in sealing injured vessels as the PTT damages blood vessels. The coating can also protect the quickly oxidized NPs from the exposition of oxygen and normal tissue besides targeted tumor. Zou et al80 derived PLT membrane to coat metformin, a conventional antidiabetic drug with the property of anti-oxidant, and W18O49 NPs, which can generate reactive oxygen species (ROS)81 and heat with high photothermal conversion efficacy under irradiation, to form PM-W18O49-Met NPs. This design combined the efficacy of PDT and PTT, and showed enhanced tumor ablation ability. After 10 minutes excitation under an 808 nm laser, the total apoptosis rate in the PM-W18O49-Met group reached about 88.30% (Figure 8B–D). A recent study reported the combination of RBC-membrane and PLT-membrane, the hybrid inherited the properties of these two kinds of cells, which are the long blood retention time of RBC and inflammation and damaged vessel targeting ability of PLT82 (Figure 8F, G).
Figure 8.
(A) Representative TEM image of negatively uranyl acetate-stained PLT-MNs.79 (B) Representative H&E staining of tumor tissues in tumor-bearing mice with different treatments. Scale bar =50 μm. (C) Images of Ki67 immunohistochemical staining in tumor tissues harvested from the mice in accordance with (B). Scale bar =50 μm. (D) TUNEL staining images of tumor sections from tumor-bearing mice after different treatments. The color blue is nuclei stained by DAPI. Scale bar =20 μm. (E) Representative in vivo IR thermal images of tumor-bearing mice before and after different combinations of treatments. (F) Representative TEM images of RBCNPs, [RBC-P]NPs, and PNPs, negatively stained with vanadium (scale bar =100 nm). (G) Immunogold TEM images of RBCNP, [RBC-P]NP, and PNP samples probed for CD235a (red arrows, large gold) and CD61 (orange arrows, small gold), followed by negative staining with vanadium (scale bars =50 nm). Copyright ©2017. John Wiley and Sons. Reproduced from Rao L, Bu -L-L, Meng Q-F, et al.Antitumor platelet-mimicking magnetic nanoparticles. Adv Funct Mater. 2017;27:9.79.79 Reprinted from Acta Biomaterialia, 80, Zuo H, Tao J, Shi H, He J, Zhou Z, Zhang C. Platelet-mimicking nanoparticles co-loaded with W18O49 and metformin alleviate tumor hypoxia for enhanced photodynamic therapy and photothermal therapy. 296–307, Copyright (2018), with permission from Elsevier.80 Copyright ©2017. John Wiley and Sons. Reproduced from Dehaini D, Wei X, Fang RH, et al.Erythrocyte-platelet hybrid membrane coating for enhanced nanoparticle functionalization. Adv Mater. 2017;29(16):1606209. doi:10.1002/adma.201700681.82
Notes: Fig 8 parts A, E is taken from reference 79, parts B-D is taken from reference 80, parts F,G is taken from reference 82.
Abbreviations: PLT-MNs, PLT membrane-coated particles; [RBC-P]NPs, RBC–platelet hybrid membrane-coated nanoparticles; PNPs, platelet membrane-coated nanoparticles.
Mesenchymal stem cells
Mesenchymal stem cells (MSCs) are multipotent progenitor cells that possess the ability of self-renewal and multi-potential differentiation. They have the potential of multiple clinical applications including increasing the success rate of transplants, reducing the side effects after chemotherapy, and in the treatment of auto-immune diseases. The role of MSCs in tumor development and metastasis have been studied in recent years. MSCs may exert direct paracrine influences on the tumor cells, promote the formation of tumor vasculature, and respond to the chemotactic signals transmitted by tumor cells. It may also be able to differentiate into other types of cells in tumor stromal, like tumor-associated fibroblasts.83–85 The homing of MSCs to malignancies is meditated by many mechanisms, like by CCL25 or sodium iodide symporter under the control of RANTES/CCL-5 promoter.86–88 It was reported that the targeting mechanism of MSCs is tumor-specific but not species-specific, which allows the application of MSCs derived from other species and expands the sources of cells.89
Mesenchymal stem cell membrane-coated gelatin nanogels (SCMGs) designed by He et al90 coated stem cell membrane to gelatin nanogels and DOX displayed long-term stability, pH-responsive drug release behavior and high drug-loading capacity. More importantly, it demonstrated excellent cancer targeting ability and enhanced accumulation in the tumor site. A similar drug delivery system coated with PLGA and DOX showed tumor-homing and anti-tumor features.91 In addition to drug delivering, stem cell membranes were used to camouflage upconversion NPs to improve the efficacy of deep-tissue PDT cancer treatment.92 Since MSC membrane has displayed promising tumor targeting and drug delivering ability in former studies, it is plausible to assume that it will enhance PTT by coating agents with high heat conversion rate and achieve ideal tumor ablation results.
Isolation methods to attain membranes
Despite the fact that CMNPs have been widely studied, the approaches of cell membrane extraction are limited with low output. The isolation of RBC membrane is now an extensively used approach with different moderations in different research groups. The basic steps include purifying the RBCs from whole blood, subject the RBCs to hypotonic medium treatment for hemolysis, centrifuging the mixture to remove hemoglobin and attain RBC ghosts.29
The eukaryocyte membrane aside from RBCs can be attained via a combination of hypotonic treatments, mechanical membrane disruption, and high-speed differential centrifugation. During the disruption and membrane purification process, DNase and RNase were plied to remove nuclear components, thereby alleviating concerns with the administration of genetic material to induce tumors. Ultracentrifugation through a discontinuous sucrose density gradient after hypotonic treatment can collect the cell membranes. The process of sucrose gradient65 or differential centrifugation93 can separate the cell membrane from nuclear and mitochondrial components.
Another method for the preparation of membrane is by dispersing the cells in membrane protein extraction buffer solution and treat them with sonication for 1 min, and then extrude the mixture through polycarbonate porous membranes.33 The freezing and thawing method is also used to attain cell membranes. After placing in an ice bath for several minutes, the cells were subjected to freezing and thawing cycles, and were centrifuged at different conditions to get purified cell membranes.94,95
Formation of CMNPs
During the process of coating the cell membrane onto the NPs, many aspects including membrane/NP ratio, surface charge and NP diameter can affect the results of coating. Since the electrostatic repulsion between the NP cores and asymmetrically charged membrane is a key factor in fabricating core-shell structure with the membrane to be right side out, it is crucial to design the surface charge of NPs to be opposite to that of the inner side of membrane.21 There have been various methods to achieve the goal of membrane-coated particles. The sonication method uses a bath sonicator to deal with the mixed solution of particles and cell membrane vesicles, the desired nanoparticles can be attained after several minutes.96 During the process, the frequency, power and duration should be optimized to avoid protein denaturation and maximized the fusion rate. Another method to achieve the purpose is to extrude the mixture through a polycarbonate porous membrane, the diameters of the membrane vary depending on the size of the particles.48 The combination of the above two methods can also be applied to attain the coated NPs.28,29
In addition, a cell membrane-templated gelation technique has also been used to form such particles. Instead of wrapping cell membrane onto pre-formed nanoparticle substrates, this approach uses vesicles to “guide” the core formation by extruding the reaction mixture through 100 nm porous membranes to generate RBC membrane-derived vesicles containing the reactants within the vesicles. It is reported to be flexible and can overcome the restrictions imposed by the surface and size of nanoparticle cores.97 The cell membrane-to-nanoparticles ratio should be carefully controlled in all the methods to achieve maximum coating rate.
Recently, microfluidic electroporation-facilitated synthesis cell membrane-coated nanoparticles have been reported by Rao et al.42 A microfluidic chip consisting of five primary parts (two inlets, a Y-shaped merging channel, an S-shaped mixing channel, an electroporation zone and one outlet) was used for electroporation in this process. The Fe3O4 magnetic nanoparticles (MNs) and RBC-vesicles were infused into the microfluidic chip and adequately mixed. After that, the mixture of MNs and RBC-vesicles was passed through the electroporation zone where the electric pulses can effectively promote the entry of MNs into RBC-vesicles. The resulting RBC-MNs demonstrated excellent enhanced tumor magnetic resonance imaging (MRI) and PTT, and better treatment effect.
The underlying biomarkers in CMNPs-based therapy
As has been discussed in the previous part of the article, the interactions among cells and cells with the extracellular matrix are meditated by cell adhesion molecules and various biomarkers on the surface of cells. They are crucial biomarkers for researchers to identify the successful membrane-coating process and the maintenance of cell membrane biological functions. CD47 is a biomarker on many cell types, like RBCs and cancer cells. It can assist cells to achieve immune evasion and prolong their blood retention time by interaction with a marker expressed on phagocytic cells, SIRPα.49,50 It can protect cancer cells from phagocytosis by myeloid cells, and help cancer stem cells (CSCs) to survive from conventional anti-tumor therapies and cause cancer recurrence.98,99 In the function of leukocytes, CXCR2, and LFA-1 play a key role in leukocyte homing to inflamed sites,61 and biomarkers and adhesion molecule like CD45, CD3z and CD11a were used for vascular extravasation.65 Besides, the homing of MSCs to malignancies is meditated by mechanisms like CCL25 or sodium iodide symporter under the control of RANTES/CCL-5 promoter.86–88 The metastatic cascade of late-stage cancer can be concluded as two coordinated subsequent steps, heterotypic adhesion to the microvascular endothelium and homotypic aggregation.74 Studies have suggested that homotypic aggregation of cancer cells was meditated by interactions of surface adhesion molecules like T antigen-galectin-3, EpCAM and tumor-associated Thomsen-Friedenreich glycoantigen.74 The interaction between PLT and cancer cells is mainly through ligands on the surface of cell membranes, P-selectin, platelet α6β1 and C-type lectin-like receptor 2 (CLEC2) are some biomarkers expressed in cancer-related PLTs, and CD44 and metalloproteinase 9 are expressed on many cancer cells (Table 1).77,100,101
Table 1.
Biomarkers for various cells
| Cell type | Representative biomarker | Function |
|---|---|---|
| Erythrocyte | CD47 | A marker of self, interacts with SIRPα on macrophages to prevent the clearance.49,111 |
| CD235a | A major RBC sialoglycoprotein, also known as glycophorin A.112 | |
| Macrophage | CD45, CD3z, CD11a, CD47 | Biomarker and adhesion molecule used for vascular extravasation, immune evasion.65 |
| Neutrophils | L-selectin, LFA-1, β1 integrin, CXCR4 | Adhesion molecules.36 |
| Monocyte | VLA4 | Interaction with VCAM-1 expressed on the surface of tumor.113 |
| Cancer cells | T antigen-galectin-3,73 EpCAM, Thomsen-Friedenreich glycoantigen74 | Homotypic intercellular adhesion. |
| CD4750,114 | Interaction with SIRPα expressed on myeloid cells to prevent phagocytosis;50,98 expression on cancer stem cells (CSCs) to cause cancer recurrence and protect CSCs from conventional anti-tumor therapies.99 | |
| MSCs | CCL25, sodium iodide symporter86–88 | Homing to malignancies. |
| Platelet | P-selectin, αIIbβ3,115 Toll-like receptor 4,116 P-selectin and CLEC2,100 α6β1, αIIbβ3101 | Interacting with tumor cells |
Abbreviations: RBC, red blood cell; MSC, mesenchymal stem cell.
Toxicity, target ability and immunogenicity of CMNPs
Since functions like the tumor targeting ability of leukocytes and homologous binding capability of tumor cells inherited accordingly by CMNPs reducing drug release and accumulation in non-target areas, the anti-cancer drugs carried by CMNPs have demonstrated reduced toxicity and side effects, and prolonged survival rate in the research of in vivo studies, even with much larger dosages than regular use.102
Besides drug delivery and PTT, CMNPs can also be applied in tumor vaccines for cancer prevention and treatment. By surface modification of cancer cell membrane and the loaded anti-cancer or immune modulation drugs, biomimetic nanovaccines could effectively migrate to draining lymph nodes (LNs) and trigger anti-tumor immune responses. And thus, realize delayed tumor development as well as outstanding therapeutic efficacy to established tumors.103,104 Since blood cells like RBCs and WBCs lack the protein that recognizes ligands on tumor cell surfaces, the merger of targeted tumor cells and other cell membranes can provide the combined ability of homing on malignancies and immune escape ability from normal cells.
It has been pointed out that protein corona formation around the NPs during the interaction of inorganic NPs and many biological fluids may exert great influence on their surface properties and functions.105 Although some studies indicated protein corona may hamper the targeting to desired tissues, and prevent cell damage and decrease cell uptake,106,107 others have reported it may induce the higher uptake.108 For NPs functionalized by proteins, antibodies or other biomolecules, protein corona may cover the targeting ligands on the surface and reduce their targeting capabilities. Research concerning protein corona formation after cell membrane camouflaging has suggested that RBC membranes can effectively prevent protein adsorption on the surface of NPs, and thus, maintain the biological properties of CMNPs. The natural properties of cell membranes may be the reason for the prevention of protein corona.109
Conclusion
CMNPs formed using different kinds of cells inherited from the complex protein components of the membrane surface, and thus, retained the biological functions cells exert in the circulation and with other cells. This procedure avoids the complicated identification and synthesis process to restore membrane protein and imitate their functions, and integrate the strength of synthetic and biological systems. CMNPs have demonstrated ideal targeting and immune escaping ability, prolonged blood retention time, controlled drug loading and releasing, reduced toxicity and side effects, as well as the prevention of protein corona formation in the currently ongoing in vitro and in vivo studies.
Despite the above advantages of CMNPs, this method still requires future improvement. Since the amount of NPs that are needed to acquire ideal therapeutic effect require relatively large numbers of cells, cell loss during the process of membrane extraction and camouflage should be reduced with modification. Moreover, the complex synthetic approach of forming and identifying such NPs needs to be simplified to realize further application. For cancer cell membrane, the nucleus and the genetic material should be strictly removed to eliminate the underlying oncogenic possibility. Since RBCs and WBCs are important sources of membrane and leukocytes are highly heterogeneous, blood-type compatibility tests and infectious diseases screening of the donor should be carried out if allogenic blood is used as the membrane source.
In conclusion, the newly developed cell membrane cloaked system showed its potential in the treatment of a wide range of diseases. With the modification of isolation and purification approach, these biomimetic NPs may have a high safety and promising therapeutic efficiency platform for clinical cancer treatment.
Acknowledgments
This research was funded by the Natural Science Foundation of China (No. 81772285), Shanghai Science and Technology Commission Project (No. 17411968700, 18441900300), Shanghai Science & Technology Research Program (13JC1401403), Shanghai Health System Excellent Personnel Training Program (No. 2017YQ051), Postdoctoral Science Foundation (2017M621534, BX201700173), and the Key Developing Disciplines of Shanghai Municipal Commission of Health and Family Planning (2015ZB0602).
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Matsumura Y, Maeda H. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agents Smancs. Cancer Res. 1986;46:1986. [PubMed] [Google Scholar]
- 2.Dai Y, Xu C, Sun X, Chen X. Nanoparticle design strategies for enhanced anticancer therapy by exploiting the tumour microenvironment. Chem Soc Rev. 2017;46(12):3830–3852. doi: 10.1039/c6cs00592f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kranz LM, Diken M, Haas H, et al. Systemic RNA delivery to dendritic cells exploits antiviral defence for cancer immunotherapy. Nature. 2016;534(7607):396–401. doi: 10.1038/nature18300 [DOI] [PubMed] [Google Scholar]
- 4.Siefert AL, Caplan MJ, Fahmy TM. Artificial bacterial biomimetic nanoparticles synergize pathogen-associated molecular patterns for vaccine efficacy. Biomaterials. 2016;97:85–96. doi: 10.1016/j.biomaterials.2016.03.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giljohann DA, Seferos DS, Prigodich AE, Patel PC, Mirkin CA. Gene regulation with polyvalent siRNA-nanoparticle conjugates. J Am Chem Soc. 2009;131(6):2072–2073. doi: 10.1021/ja808719p [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ouay BL, Stellacci F. Antibacterial activity of silver nanoparticles: a surface science insight. Nano Today. 2015;10(3):339–354. doi: 10.1016/j.nantod.2015.04.002 [DOI] [Google Scholar]
- 7.Amani H, Mostafavi E, Arzaghi H, et al. Three-dimensional graphene foams: synthesis, properties, biocompatibility, biodegradability, and applications in tissue engineering. ACS Biomater Sci Eng. 2019; 5(1): 193–214. [DOI] [PubMed] [Google Scholar]
- 8.Tsao SC-H, Wang J, Wang Y, Behren A, Cebon J, Trau M. Characterising the phenotypic evolution of circulating tumour cells during treatment. Nat Commun. 2018;9:1. doi: 10.1038/s41467-018-03725-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim HS, Lee DY. Near-infrared-responsive cancer photothermal and photodynamic therapy using gold nanoparticles. Polymers. 2018;10:9. doi: 10.3390/polym10090961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jabeen F, Najam-ul-Haq M, Javeed R, Huck CW, Bonn GK. Au-nanomaterials as a superior choice for near-infrared photothermal therapy. Molecules. 2014;19(12):20580–20593. doi: 10.3390/molecules191220580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao X, Qi T, Kong C, et al. Photothermal exposure of polydopamine-coated branched Au-Ag nanoparticles induces cell cycle arrest, apoptosis, and autophagy in human bladder cancer cells. Int J Nanomedicine. 2018;13:6413–6428. doi: 10.2147/IJN.S174349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qi W, Yan J, Sun H, Wang H. Nanocomposite plasters for the treatment of superficial tumors by chemo-photothermal combination therapy. Int J Nanomedicine. 2018;13:6235–6247. doi: 10.2147/IJN.S170209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shen S, Tang H, Zhang X, et al. Targeting mesoporous silica-encapsulated gold nanorods for chemo-photothermal therapy with near-infrared radiation. Biomaterials. 2013;34(12):3150–3158. doi: 10.1016/j.biomaterials.2013.01.051 [DOI] [PubMed] [Google Scholar]
- 14.Sung S-J, Min SH, Cho KY, et al. Effect of polyethylene glycol on gene delivery of polyethylenimine. Biol Pharm Bull. 2003;26(4):492–500. [DOI] [PubMed] [Google Scholar]
- 15.Inostroza-Riquelme M, Vivanco A, Lara P, et al. Encapsulation of gold nanostructures and oil-in-water nanocarriers in microgels with biomedical potential. Molecules. 2018;23:5. doi: 10.3390/molecules23051208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tang B, Qian Y, Gou Y, Cheng G, Fang G. VE-albumin core-shell nanoparticles for paclitaxel delivery to treat MDR breast cancer. Molecules. 2018;23:11. doi: 10.3390/molecules23112760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deloach J, Barton C, Culler K. Preparation of resealed carrier erythrocytes and in vivo survival in dogs. Am J Vet Res. 1981;42(4):667–669. [PubMed] [Google Scholar]
- 18.Hu CMJ, Fang RH, Fang L. Erythrocyte‐inspired delivery systems. Adv Healthc Mater. 2012;1(5):537–547. doi: 10.1002/adhm.201200138 [DOI] [PubMed] [Google Scholar]
- 19.Cao B, Yang M, Zhu Y, Qu X, Mao C. Stem cells loaded with nanoparticles as a drug carrier for in vivo breast cancer therapy. Adv Mater Weinheim. 2014;26(27):4627–4631. doi: 10.1002/adma.201401550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Phua KKL, Boczkowski D, Dannull J, Pruitt S, Leong KW, Nair SK. Whole blood cells loaded with messenger RNA as an anti-tumor vaccine. Adv Healthc Mater. 2014;3(6):837–842. doi: 10.1002/adhm.201300512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tan S, Wu T, Zhang D, Zhang Z. Cell or cell membrane-based drug delivery systems. Theranostics. 2015;5(8):863–881. doi: 10.7150/thno.11852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Namiki Y, Fuchigami T, Tada N, et al. Nanomedicine for cancer: lipid-based nanostructures for drug delivery and monitoring. Acc Chem Res. 2011;44(10):1080–1093. doi: 10.1021/ar200011r [DOI] [PubMed] [Google Scholar]
- 23.Reimhult E. Nanoparticle-triggered release from lipid membrane vesicles. New Biotechnol. 2015;32(6):665–672. doi: 10.1016/j.nbt.2014.12.002 [DOI] [PubMed] [Google Scholar]
- 24.Sun D, Zhuang X, Zhang S, et al. Exosomes are endogenous nanoparticles that can deliver biological information between cells. Adv Drug Deliv Rev. 2013;65(3):342–347. doi: 10.1016/j.addr.2012.07.002 [DOI] [PubMed] [Google Scholar]
- 25.Li B, Wang F, Gui L, He Q, Yao Y, Chen H. The potential of biomimetic nanoparticles for tumor-targeted drug delivery. Nanomedicine (Lond). 2018;13:16. doi: 10.2217/nnm-2018-0017 [DOI] [PubMed] [Google Scholar]
- 26.Fang RH, Hu C-MJ, Chen KNH, et al. Lipid-insertion enables targeting functionalization of erythrocyte membrane-cloaked nanoparticles. Nanoscale. 2013;5(19):8884–8888. doi: 10.1039/c3nr03064d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sheng G, Chen Y, Han L, et al. Encapsulation of indocyanine green into cell membrane capsules for photothermal cancer therapy. Acta Biomater. 2016;43:251–261. doi: 10.1016/j.actbio.2016.07.012 [DOI] [PubMed] [Google Scholar]
- 28.Chen Z, Zhao P, Luo Z, et al. Cancer cell membrane-biomimetic nanoparticles for homologous-targeting dual-modal imaging and photothermal therapy. ACS Nano. 2016;10(11):10049. doi: 10.1021/acsnano.6b04695 [DOI] [PubMed] [Google Scholar]
- 29.Hu C-MJ, Zhang L, Aryal S, Cheung C, Fang RH, Zhang L. Erythrocyte membrane-camouflaged polymeric nanoparticles as a biomimetic delivery platform. Proc Natl Acad Sci USA. 2011;108(27):10980–10985. doi: 10.1073/pnas.1106634108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peng J, Yang Q, Li W, et al. Erythrocyte-membrane-coated prussian blue/manganese dioxide nanoparticles as H2O2-responsive oxygen generators to enhance cancer chemotherapy/photothermal therapy. ACS Appl Mater Interfaces. 2017;9(51):44410–44422. doi: 10.1021/acsami.7b17022 [DOI] [PubMed] [Google Scholar]
- 31.Krishnamurthy S, Gnanasammandhan MK, Xie C, Huang K, Cui MY, Chan JM. Monocyte cell membrane-derived nanoghosts for targeted cancer therapy. Nanoscale. 2016;8(13):6981–6985. doi: 10.1039/c5nr07588b [DOI] [PubMed] [Google Scholar]
- 32.Crusz SM, Balkwill FR. Inflammation and cancer: advances and new agents. Nat Rev Clin Oncol. 2015;12(10):584–596. doi: 10.1038/nrclinonc.2015.105 [DOI] [PubMed] [Google Scholar]
- 33.Li J, Zhen X, Lyu Y, Jiang Y, Huang J, Pu K. cell membrane coated semiconducting polymer nanoparticles for enhanced multimodal cancer phototheranostics. ACS Nano. 2018;12(8):8520–8530. doi: 10.1021/acsnano.8b04066 [DOI] [PubMed] [Google Scholar]
- 34.Jiang Q, Luo Z, Men Y, et al. Red blood cell membrane-camouflaged melanin nanoparticles for enhanced photothermal therapy. Biomaterials. 2017;143:29. doi: 10.1016/j.biomaterials.2017.07.027 [DOI] [PubMed] [Google Scholar]
- 35.Fu Q, Lv P, Chen Z, et al. Programmed co-delivery of paclitaxel and doxorubicin boosted by camouflaging with erythrocyte membrane. Nanoscale. 2015;7(9):4020–4030. doi: 10.1039/c4nr07027e [DOI] [PubMed] [Google Scholar]
- 36.Kang T, Zhu Q, Wei D, et al. Nanoparticles coated with neutrophil membranes can effectively treat cancer metastasis. ACS Nano. 2017;11:1397−1411. doi: 10.1021/acsnano.6b06477 [DOI] [PubMed] [Google Scholar]
- 37.Zhang Q, Dehaini D, Zhang Y, et al. Neutrophil membrane-coated nanoparticles inhibit synovial inflammation and alleviate joint damage in inflammatory arthritis. Nat Nanotechnol. 2018. 13;1182–1190. [DOI] [PubMed] [Google Scholar]
- 38.Hu CMJ, Fang RH, Copp J, Luk BT, Zhang L. A biomimetic nanosponge that absorbs pore-forming toxins. Nat Nanotechnol. 2013;8(5):336–340. doi: 10.1038/nnano.2013.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu CM, Fang RH, Luk BT, Zhang L. Nanoparticle-detained toxins for safe and effective vaccination. Nat Nanotechnol. 2013;8(12):933–938. doi: 10.1038/nnano.2013.254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fitzgerald J, Foster T, Cox D. The interaction of bacterial pathogens with platelets. Nat Rev Microbiol. 2006;4(6):445. doi: 10.1038/nrmicro1425 [DOI] [PubMed] [Google Scholar]
- 41.Ren X, Zheng R, Fang X, et al. Red blood cell membrane camouflaged magnetic nanoclusters for imaging-guided photothermal therapy. Biomaterials. 2016;92:13–24. doi: 10.1016/j.biomaterials.2016.03.026 [DOI] [PubMed] [Google Scholar]
- 42.Rao L, Cai B, Bu -L-L, et al. Microfluidic electroporation-facilitated synthesis of erythrocyte membrane-coated magnetic nanoparticles for enhanced imaging-guided cancer therapy. ACS Nano. 2017;11(4):3496–3505. doi: 10.1021/acsnano.7b00133 [DOI] [PubMed] [Google Scholar]
- 43.Li J, Wang X, Zheng D, et al. Cancer cell membrane-coated magnetic nanoparticles for MR/NIR fluorescence dual-modal imaging and photodynamic therapy. Biomater Sci. 2018;6:7. doi: 10.1039/c8bm00675j [DOI] [PubMed] [Google Scholar]
- 44.Fang RH, Hu C-MJ, Luk BT, et al. Cancer cell membrane-coated nanoparticles for anticancer vaccination and drug delivery. Nano Lett. 2014;14(4):2181–2188. doi: 10.1021/nl500618u [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hu CM, Fang RH, Copp J, Luk BT, Zhang L. A biomimetic nanosponge that absorbs pore-forming toxins. Nat Nanotechnol. 2013;8(5):336–340. doi: 10.1038/nnano.2013.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen HW, Fang ZS, Chen YT, et al. Targeting and enrichment of viral pathogen by cell membrane cloaked magnetic nanoparticles for enhanced detection. Acs Appl Mater Inter. 2017;9:46. doi: 10.1021/acsami.7b09931 [DOI] [PubMed] [Google Scholar]
- 47.Hao R, Liu J, Li Y, et al. Oxygen self-enriched nanoparticles functionalized with erythrocyte membranes for long circulation and enhanced phototherapy. Acta Biomater. 2017;59:269. doi: 10.1016/j.actbio.2017.06.035 [DOI] [PubMed] [Google Scholar]
- 48.Luk BT, Hu C-MJ, Fang RH, et al. Interfacial interactions between natural RBC membranes and synthetic polymeric nanoparticles. Nanoscale. 2014;6(5):2730–2737. doi: 10.1039/c3nr06371b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barclay A, Berg T. The interaction between signal regulatory protein alpha (SIRPα) and CD47: structure, function, and therapeutic target. Annu Rev Immunol. 2014;32:25–50. doi: 10.1146/annurev-immunol-032713-120142 [DOI] [PubMed] [Google Scholar]
- 50.Jaiswal S, Jamieson CHM, Pang WW, et al. CD47 is upregulated on circulating hematopoietic stem cells and leukemia cells to avoid phagocytosis. Cell. 2009;138(2):271. doi: 10.1016/j.cell.2009.07.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cameron C, Barrett J, Mann M, Lucas A, Mcfadden G. Myxoma virus M128L is expressed as a cell surface CD47-like virulence factor that contributes to the downregulation of macrophage activation in vivo. Virology. 2005;337(1):55–67. doi: 10.1016/j.virol.2005.03.037 [DOI] [PubMed] [Google Scholar]
- 52.Hu C-MJ, Fang RH, Luk BT, et al. ‘Marker-of-self’ functionalization of nanoscale particles through a top-down cellular membrane coating approach. Nanoscale. 2013;5(7):2664–2668. doi: 10.1039/c3nr00015j [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Piao J-G, Wang L, Gao F, You Y-Z, Xiong Y, Yang L. Erythrocyte membrane is an alternative coating to polyethylene glycol for prolonging the circulation lifetime of gold nanocages for photothermal therapy. ACS Nano. 2014;8(10):10414–10425. doi: 10.1021/nn503779d [DOI] [PubMed] [Google Scholar]
- 54.Estelrich J, Busquets MA. Iron oxide nanoparticles in photothermal therapy. Molecules. 2018;23:7. doi: 10.3390/molecules23071567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thienpont B, Steinbacher J, Zhao H, et al. Tumour hypoxia causes DNA hypermethylation by reducing TET activity. Nature. 2016;537(7618):63–68. doi: 10.1038/nature19081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen H, Sha H, Zhang L, et al. Lipid insertion enables targeted functionalization of paclitaxel-loaded erythrocyte membrane nanosystem by tumor-penetrating bispecific recombinant protein. Int J Nanomedicine. 2018;13:5347–5359. doi: 10.2147/IJN.S165109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang Z, Qian H, Huang J, et al. Anti-EGFR-iRGD recombinant protein modified biomimetic nanoparticles loaded with gambogic acid to enhance targeting and antitumor ability in colorectal cancer treatment. Int J Nanomedicine. 2018;13:4961–4975. doi: 10.2147/IJN.S170148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhu D-M, Xie W, Xiao Y-S, et al. Erythrocyte membrane-coated gold nanocages for targeted cancer photothermal and chemical therapy. Nanotechnology. 2017;29:8. [DOI] [PubMed] [Google Scholar]
- 59.Trinchieri G. Cancer and inflammation: an old intuition with rapidly evolving new concepts. Annu Rev Immunol. 2012;30:677–706. doi: 10.1146/annurev-immunol-020711-075008 [DOI] [PubMed] [Google Scholar]
- 60.Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–444. doi: 10.1038/nature07205 [DOI] [PubMed] [Google Scholar]
- 61.Wang Q, Ren Y, Mu J, et al. grapefruit-derived nanovectors use an activated leukocyte trafficking pathway to deliver therapeutic agents to inflammatory tumor sites. Cancer Res. 2015;75(12):2520–2529. doi: 10.1158/0008-5472.CAN-14-3095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9(3):162–174. doi: 10.1038/nri2506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Murdoch C, Muthana M, Coffelt B, Lewis C. The role of myeloid cells in the promotion of tumour angiogenesis. Nat Rev Cancer. 2008;8(8):618–631. doi: 10.1038/nrc2444 [DOI] [PubMed] [Google Scholar]
- 64.Baek S-K, Makkouk AR, Krasieva T, Sun C-H, Madsen SJ, Hirschberg H. Photothermal treatment of glioma; an in vitro study of macrophage-mediated delivery of gold nanoshells. J Neuro-Oncol. 2011;104(2):439–448. doi: 10.1007/s11060-010-0511-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Parodi A, Quattrocchi N, ALvd V, et al. Synthetic nanoparticles functionalized with biomimetic leukocyte membranes possess cell-like functions. Nat Nanotechnol. 2013;8(1):61–68. doi: 10.1038/nnano.2012.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Meng Q-F, Rao L, Zan M, et al. Macrophage membrane-coated iron oxide nanoparticles for enhanced photothermal tumor therapy. Nanotechnology. 2018;29(13):134004. doi: 10.1088/1361-6528/aaa7c7 [DOI] [PubMed] [Google Scholar]
- 67.Xuan M, Shao J, Dai L, Li J, He Q. Macrophage cell membrane camouflged Au nanoshells for in vivo prolonged circulation life and enhanced cancer photothermal therapy. ACS Appl Mater Interfaces. 2016;8(15):9610–9618. doi: 10.1021/acsami.6b00853 [DOI] [PubMed] [Google Scholar]
- 68.Zhang Y, Cai K, Li C, et al. Macrophage-membrane-coated nanoparticles for tumor-targeted chemotherapy. Nano Lett. 2018;18(3):1908–1915. doi: 10.1021/acs.nanolett.7b05263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.He W, Frueh J, Wu Z, He Q. Leucocyte membrane-coated janus microcapsules for enhanced photothermal cancer treatment. Langmuir. 2016;32(15):3637–3644. doi: 10.1021/acs.langmuir.5b04762 [DOI] [PubMed] [Google Scholar]
- 70.Zhang L, Li R, Chen H, et al. Human cytotoxic T-lymphocyte membrane-camouflaged nanoparticles combined with low-dose irradiation: a new approach to enhance drug targeting in gastric cancer. Int J Nanomedicine. 2017;12:2129–2142. doi: 10.2147/IJN.S126016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Coffelt SB, Kersten K, Doornebal CW, et al. IL17-producing γδ T cells and neutrophils conspire to promote breast cancer metastasis. Nature. 2015;522(7556):345–348. doi: 10.1038/nature14282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hanahan D, Weinberg R. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 73.Khaldoyanidi SK, Glinsky VV, Sikora L, et al. MDA-MB-435 human breast carcinoma cell homo- and heterotypic adhesion under flow conditions is mediated in part by Thomsen-Friedenreich antigen-galectin-3 interactions. J Biol Chem. 2003;278(6):4127–4134. doi: 10.1074/jbc.M209590200 [DOI] [PubMed] [Google Scholar]
- 74.Glinsky VV, Glinsky GV, Glinskii OV, et al. Intravascular metastatic cancer cell homotypic aggregation at the sites of primary attachment to the endothelium. Cancer Res. 2003;63:3805–3811. [PubMed] [Google Scholar]
- 75.Wang D, Dong H, Li M, et al. Erythrocyte-cancer hybrid membrane camouflaged hollow copper sulfide nanoparticles for prolonged circulation life and homotypic-targeting photothermal/chemotherapy of melanoma. ACS Nano. 2018.12(6);5241–5252. [DOI] [PubMed] [Google Scholar]
- 76.Gay LJ, Felding-Habermann B. Contribution of platelets to tumour metastasis. Nat Rev Cancer. 2011;11(2):123. doi: 10.1038/nrc3004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Amo L, Tamayo-Orbegozo E, Maruri N, et al. Involvement of platelet-tumor cell interaction in immune evasion. Potential role of podocalyxin-like protein. Front Oncol. 2014;4:245. doi: 10.3389/fonc.2014.00245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Goubran HA, Stakiw J, Radosevic M, Burnouf T. Platelet-cancer interactions. Semin Thromb Hemost. 2014;40(3):296–305. doi: 10.1055/s-0034-1370767 [DOI] [PubMed] [Google Scholar]
- 79.Rao L, Bu -L-L, Meng Q-F, et al. Antitumor platelet-mimicking magnetic nanoparticles. Adv Funct Mater. 2017;27:9. [Google Scholar]
- 80.Zuo H, Tao J, Shi H, He J, Zhou Z, Zhang C. Platelet-mimicking nanoparticles co-loaded with W18O49 and metformin alleviate tumor hypoxia for enhanced photodynamic therapy and photothermal therapy. Acta Biomater. 2018;80(undefined):296–307. doi: 10.1016/j.actbio.2018.09.017 [DOI] [PubMed] [Google Scholar]
- 81.Kalluru P, Vankayala R, Chiang CS, Hwang KC. Photosensitization of singlet oxygen and in vivo photodynamic therapeutic effects mediated by PEGylated W 18 O 49 nanowires. Angew Chem. 2013;52(47):12332–12336. doi: 10.1002/anie.201307358 [DOI] [PubMed] [Google Scholar]
- 82.Dehaini D, Wei X, Fang RH, et al. Erythrocyte-platelet hybrid membrane coating for enhanced nanoparticle functionalization. Adv Mater. 2017;29(16):1606209. doi: 10.1002/adma.201700681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Karnoub A, Dash A, Vo A, et al. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature. 2007;449(7162):557–563. doi: 10.1038/nature06188 [DOI] [PubMed] [Google Scholar]
- 84.Au P, Tam J, Fukumura D, Jain RK. Bone marrow–derived mesenchymal stem cells facilitate engineering of long-lasting functional vasculature. Blood. 2008;111(9):4551–4558. doi: 10.1182/blood-2007-10-118273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Quante M, Tu SP, Tomita H, et al. Bone marrow-derived myofibroblasts contribute to the mesenchymal stem cell niche and promote tumor growth. Cancer Cell. 2011;19(2):257–272. doi: 10.1016/j.ccr.2011.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Knoop K, Schwenk N, Schmohl K, et al. Mesenchymal stem cell (MSC)-mediated, tumor stroma-targeted radioiodine therapy of metastatic colon cancer using the sodium iodide symporter as theranostic gene. J Nucl Med. 2015;56(4):600–606. doi: 10.2967/jnumed.114.146662 [DOI] [PubMed] [Google Scholar]
- 87.Xu S, Menu E, De BA, Van CB, Vanderkerken K, Van RI. Bone marrow-derived mesenchymal stromal cells are attracted by multiple myeloma cell-produced chemokine CCL25 and favor myeloma cell growth in vitro and in vivo. Stem Cells. 2012;30(2):266–279. doi: 10.1002/stem.787 [DOI] [PubMed] [Google Scholar]
- 88.Leibacher J, Henschler R. Biodistribution, migration and homing of systemically applied mesenchymal stem/stromal cells. Stem Cell Res Ther. 2016;7(1):1–12. doi: 10.1186/s13287-015-0253-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Seo KW, Lee HW, Oh YI, et al. Anti-tumor effects of canine adipose tissue-derived mesenchymal stromal cell-based interferon-β gene therapy and cisplatin in a mouse melanoma model. Cytotherapy. 2011;13(8):944–955. doi: 10.3109/14653249.2011.584864 [DOI] [PubMed] [Google Scholar]
- 90.Gao C, Lin Z, Jurado-Sánchez B, Lin X, Wu Z, He Q. Stem cell membrane-coated nanogels for highly efficient in vivo tumor targeted drug delivery. Small. 2016;12(30):4056–4062. doi: 10.1002/smll.201600624 [DOI] [PubMed] [Google Scholar]
- 91.Yang N, Ding Y, Zhang Y, et al. Surface functionalization of polymeric nanoparticles with umbilical cord-derived mesenchymal stem cell membrane for tumor-targeted therapy. ACS Appl Mater Interfaces. 2018;10(27):22963–22973. doi: 10.1021/acsami.8b05363 [DOI] [PubMed] [Google Scholar]
- 92.Gao C, Lin Z, Wu Z, Lin X, He Q. Stem-cell-membrane camouflaging on near-infrared photoactivated upconversion nanoarchitectures for in vivo remote-controlled photodynamic therapy. ACS Appl Mater Interfaces. 2016;8(50):34252. doi: 10.1021/acsami.6b12865 [DOI] [PubMed] [Google Scholar]
- 93.Suski JM, Lebiedzinska M, Wojtala A, et al. Isolation of plasma membrane-associated membranes from rat liver. Nat Protoc. 2014;9(2):312–322. doi: 10.1038/nprot.2014.016 [DOI] [PubMed] [Google Scholar]
- 94.Li S-Y, Cheng H, Qiu W-X, et al. Cancer cell membrane-coated biomimetic platform for tumor targeted photodynamic therapy and hypoxia-amplified bioreductive therapy. Biomaterials. 2017;142:149–161. doi: 10.1016/j.biomaterials.2017.07.026 [DOI] [PubMed] [Google Scholar]
- 95.Hu C-MJ, Fang RH, Wang K-C, et al. Nanoparticle biointerfacing via platelet membrane cloaking. Nature. 2015;526(7571):118–121. doi: 10.1038/nature15373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Pang Z, Hu C-MJ, Fang RH, et al. Detoxification of organophosphate poisoning using nanoparticle bioscavengers. ACS Nano. 2015;9(6):6450–6458. doi: 10.1021/acsnano.5b02132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang J, Gao W, Fang RH, Dong A, Zhang L. Synthesis of nanogels via cell membrane-templated polymerization. Small. 2015;11(34):4309–4313. doi: 10.1002/smll.201500987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Majeti R, Chao MP, Alizadeh AA, et al. CD47 is an adverse prognostic factor and therapeutic antibody target on human acute myeloid leukemia stem cells. Cell. 2009;138(2):286–299. doi: 10.1016/j.cell.2009.05.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sara S, Matin MM. Cancer stem cells and cancer therapy. Tumor Biol. 2011;32(3):425–440. doi: 10.1007/s13277-011-0155-8 [DOI] [PubMed] [Google Scholar]
- 100.Naoya F, Satoshi T. The impact of Aggrus/podoplanin on platelet aggregation and tumour metastasis. J Biochem. 2012;152(5):407–413. doi: 10.1093/jb/mvs108 [DOI] [PubMed] [Google Scholar]
- 101.Wang S, Li Z, Xu R. Human cancer and platelet interaction, a potential therapeutic target. Int J Mol Sci. 2018;19:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yurkin ST, Wang Z. Cell membrane-derived nanoparticles: emerging clinical opportunities for targeted drug delivery. Nanomedicine. 2017;12:16. doi: 10.2217/nnm-2017-0100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yang R, Xu J, Xu L, et al. Cancer cell membrane-coated adjuvant nanoparticles with mannose modification for effective anticancer vaccination. Acs Nano. 2018.12(6):5121–5129. [DOI] [PubMed] [Google Scholar]
- 104.Guo Y, Wang D, Song Q, et al. erythrocyte membrane-enveloped polymeric nanoparticles as nanovaccine for induction of antitumor immunity against melanoma. ACS Nano. 2015;9(7):6918. doi: 10.1021/nn507282f [DOI] [PubMed] [Google Scholar]
- 105.Amani H, Habibey R, Hajmiresmail S, Latifi S, Pazoki-Toroudi H, Akhavan O. Antioxidant nanomaterials in advanced diagnoses and treatments of ischemia reperfusion injuries. J Mater Chem B. 2017;5:9452–9476. doi: 10.1039/C7TB01689A [DOI] [PubMed] [Google Scholar]
- 106.Anna S, Pitek AS, Monopoli MP, et al. Transferrin-functionalized nanoparticles lose their targeting capabilities when a biomolecule corona adsorbs on the surface. Nat Nanotechnol. 2013;8(2):137–143. doi: 10.1038/nnano.2012.237 [DOI] [PubMed] [Google Scholar]
- 107.Lesniak A, Fenaroli F, Monopoli MP, Åberg C, KA Dawson, Salvati A. Effects of the presence or absence of a protein corona on silica nanoparticle uptake and impact on cells. ACS Nano. 2012;6(7):5845–5857. doi: 10.1021/nn300223w [DOI] [PubMed] [Google Scholar]
- 108.Yallapu MM, Chauhan N, Othman SF, et al. Implications of protein corona on physico-chemical and biological properties of magnetic nanoparticles. Biomaterials. 2015;46(11):1–12. doi: 10.1016/j.biomaterials.2014.12.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rao L, Meng QF, Bu LL, et al. Erythrocyte membrane-coated upconversion nanoparticles with minimal protein adsorption for enhanced tumor imaging. ACS Appl Mater Interfaces. 2017;9(3):2159–2168. doi: 10.1021/acsami.6b14450 [DOI] [PubMed] [Google Scholar]
- 110.Bombelli FB, Webster CA, Moncrieff M, Sherwood V. The scope of nanoparticle therapies for future metastatic melanoma treatment. Lancet Oncol. 2014;15(1):e22–e32. doi: 10.1016/S1470-2045(13)70333-4 [DOI] [PubMed] [Google Scholar]
- 111.Okazawa H, Motegi S, Ohyama N, et al. Negative regulation of phagocytosis in macrophages by the CD47-SHPS-1 system. J Immunol. 2005;174(4):2004–2011. [DOI] [PubMed] [Google Scholar]
- 112.Gagneux P, Varki A. Evolutionary considerations in relating oligosaccharide diversity to biological function. Glycobiology. 1999;9(8):747. doi: 10.1093/glycob/9.8.747 [DOI] [PubMed] [Google Scholar]
- 113.Liu YS, Lin HY, Lai SW, et al. MiR-181b modulates EGFR-dependent VCAM-1 expression and monocyte adhesion in glioblastoma. Oncogene. 2017;36:35. doi: 10.1038/onc.2017.129 [DOI] [PubMed] [Google Scholar]
- 114.Liu X, Kwon H, Li Z, Fu Y-X. Is CD47 an innate immune checkpoint for tumor evasion? J Hematol Oncol. 2017;10(1):12. doi: 10.1186/s13045-016-0381-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Coupland L, Hindmarsh E, Gardiner E, Parish C. The influence of platelet membranes on tumour cell behaviour. Cancer Metastasis Rev. 2017;36(2):215–224. doi: 10.1007/s10555-017-9671-3 [DOI] [PubMed] [Google Scholar]
- 116.Yu L-X, Yan L, Yang W, et al. Platelets promote tumour metastasis via interaction between TLR4 and tumour cell-released high-mobility group box1 protein. Nat Commun. 2014;5(undefined):5256. doi: 10.1038/ncomms5972 [DOI] [PubMed] [Google Scholar]