Abstract
OBJECTIVE:
This study assesses emergency contraception (EC) dispensed before and after a 3-minute video counseling intervention on EC.
METHODS:
We used a quasi-experimental design and two data sources to assess the impact of offering the video counseling intervention. We used electronic health records from six Planned Parenthood Association of Utah health centers with onsite oral EC dispensing to determine pre- and post-intervention EC distribution. Beginning July 2015, three participating locations offered the video counseling intervention to English-speaking EC clients. These clients completed a brief survey assessing EC knowledge and uptake, providing a patient-level data source. We used a difference-in-difference analysis of the clinic-level data to assess the effect of the video counseling intervention. This analysis compares the variation in oral EC distribution between clinics offering the video intervention and clinics not offering the video counseling before and after the video counseling was introduced. Multivariable logistic regression assessed client characteristics associated with receiving ulipristal.
RESULTS:
The six health centers served 8,269 English-language EC clients during 2015. At participating sites, provision of ulipristal increased from 12% (269/2315) pre-intervention to 28% (627/2266) post-intervention (p<0.001). Non-participating sites did not see a change. Clients seeking EC at sites offering video counseling were more likely to receive ulipristal, even after controlling for age, insurance, and ethnicity (adj.OR 3.4, 95% CI 3.0–3.9). Using the difference-in-difference analysis, the video counseling intervention accounted for an 18% (95%CI 14%−21%) increase in ulipristal provision at the participating health centers. Among the 2,266 women seeking EC who were offered video counseling, 19% (425/2,266) watched the video, and 60% (254/425) reported the video affected their EC preferences. Knowledge of the IUD for EC increased but reported uptake of this method remained low (6.8%).
CONCLUSIONS:
Exposure to video counseling increased use of more effective oral EC and increased knowledge about all EC options.
IMPLICATIONS:
Use of a brief informational video about EC options at family planning clinics may increase the proportion of EC clients receiving more effective EC methods.
INTRODUCTION
Women seeking emergency contraception (EC) desire to prevent a pregnancy after unprotected intercourse (UPI). Currently, the EC options for women in the United States include: oral levonorgestrel (LNG), oral ulipristal acetate (UPA), and the T380 copper IUD. The two oral options can be dispensed at the pharmacy, and the IUD requires an in-office procedure with a trained provider. The fourth EC option is the Yuzpe method of combined oral contraceptive pills. This less effective approach can still be used if the above options are not available or affordable, but its use will not be further addressed here. EC clients need to consider time since unprotected intercourse, risk of pregnancy, BMI, and desire for a reliable ongoing contraceptive option when choosing which option is best for them:.
EC users can access oral LNG, the most commonly used EC method, in pharmacies without a prescription. In 2010, the US Food and Drug Administration (FDA) approved oral UPA, a selective progesterone receptor modulator, for prescription EC use. However, women using EC who weigh more than 160lbs experience significantly lower efficacy with oral LNG relative to oral UPA [1]. Additionally, UPA efficacy and FDA approval for use extends up to 120 hours following unprotected sexual intercourse [2]. FDA approval and the package insert limit use of oral LNG to 72 hours after intercourse, but efficacy may go beyond that timeframe [3, 4]. The final and most effective form of EC is the copper IUD, which has a pregnancy risk of 1/1000, 1/10th the risk of UPA [5]. It also is the only option that continues to provide highly effective contraception for as long as the user desires up to twelve years after insertion. Though the FDA has labeled the copper IUD for up to 10 years of use, strong evidence indicates that it is effective for up to 12 years [6]. Disadvantages of the IUD for EC include its greater expense, the additional time for placement by a medical provider, patient discomfort at the time of placement, and potential unwanted side effects.
Several studies demonstrate gaps in patient knowledge of EC [7–9]. Patient-oriented video decision support tools provide an ideal opportunity to support EC clients to make an informed choice when multiple EC options are offered [10]. To meet this need, we developed a 3-minute video counseling for emergency contraception that seeks to counsel clients on their EC options. (Appendix 1. Video counseling script or for the full video https://www.youtube.com/watch?v=_Q2E8tsyCQE). We evaluated the impact of the video counseling on oral EC dispensing at the clinic level. Among clients who watched the video, we assessed EC knowledge, changes in EC plans, and satisfaction with the video as a decision support tool.
METHODS
STUDY DESIGN
We used a quasi-experimental design (i.e without random assignment to treatment and control groups) and two data sources to assess the video counseling intervention. At the clinic level, we used electronic health records from January 2015-December 2015 from six Planned Parenthood Association of Utah health centers with onsite oral EC dispensing. In the second half of the assessment period, from July 2015-December 2015, three locations adopted the video counseling intervention. Participants who watched the video completed a brief survey which provided a second data source. These clinics provide three EC options: oral LNG, UPA, and the copper IUD. In addition, while pharmacies provide oral LNG for EC without a prescription, Planned Parenthood remains the preferred EC provider among patients in these communities because the clinics provide EC services on a sliding scale based on ability to pay, making it more affordable than pharmacies. Out-of-pocket cost of EC at Utah’s Planned Parenthood clinics varies from $5 for oral LNG, $30 for UPA, and around $500 for the copper IUD; however, the payment scale slides to zero, if needed, for all EC visits. Women preferring oral LNG may approach the clinic front desk and receive the medication in less than 5 minutes without an appointment. Oral UPA requires a prescription and involves a minimal encounter with an advanced practice clinician. Finally, a copper IUD demands a full clinic appointment including counseling on the device and the insertion procedure. However, during the time of the intervention not all clinics had a clinician available for IUD insertion every day. On these days clinics provided clients with the oral EC of their choice and scheduled them for an IUD insertion at a later date.
During the intervention period, front desk staff offered English-speaking clients presenting for EC the opportunity to watch the video. The animated English-language video included information on oral LNG, oral UPA, and the copper IUD. Eligible women spoke English and requested EC at a participating health center during the 6-month intervention period. The study protocol did not include any additional eligibility criteria. Prior to starting the video and survey, an electronic cover letter approved by the University of Utah IRB explained the details of the study and continuation to the video implied consent. The counseling video content compared method characteristics of oral LNG, oral UPA, and the copper IUD and provided information on method efficacy, impact of BMI, and availability. This included the over the counter availability of oral LNG, the need for a prescription with UPA, and the need for professional placement with the copper T380 IUD. We developed the script based on information included on commonly used client sheets for EC users shared at Planned Parenthood clinics and on the Bedsider.org website. After watching the video, the client completed an anonymous survey reporting basic demographics, prior knowledge of EC, the impact of the video on their EC choice, and if they would recommend this video to other women seeking EC (Appendix 2. Video counseling survey). The client then continued with their clinic visit per standard of care. We used REDCap, a secure web application, to build, administer, and manage the online survey and database [17].
First, to examine the impact of the video counseling intervention we used pharmacy dispensing records from participating and non-participating health centers for the 6-months prior to the video counseling intervention, and during the 6-month video counseling intervention. We describe characteristics of clients’ age, race/ethnicity, and insurance status by sale of oral LNG and oral UPA, and use logistic regression to assess client characteristic associations with selection of UPA. During the study period, clinics did not have standardized reporting of which clients receiving IUDs used them specifically for EC, thus these data were not available from the clinical data. We compared oral EC dispensing data using a difference-in-difference analysis to assess the impact of the intervention on UPA, the more effective oral EC option. Difference-in-difference estimates the specific intervention effect of the intervention by comparing the observed outcome trend to an unobserved counterfactual. Second, using the survey data, we describe characteristics of the video counseling participants, baseline EC knowledge, EC type participants planned to request before watching the video, and what participants planned to request after video counseling. We used multivariable logistic regression to determine associations between patient characteristics and changing their mind on the type of EC they planned to request at their visit after watching the video. We adjusted for available sociodemographic data with potential associations with EC method selection including age, race/ethnicity, insurance status, gravidity, income, and highest level of education. We used Stata14 or higher to analyze all data (College Station, TX). The University of Utah Institutional Review Board approved this study.
RESULTS
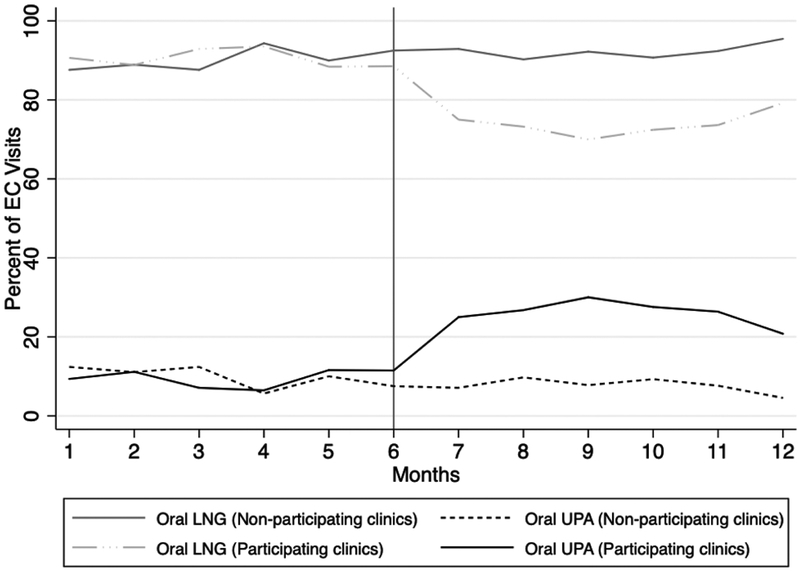
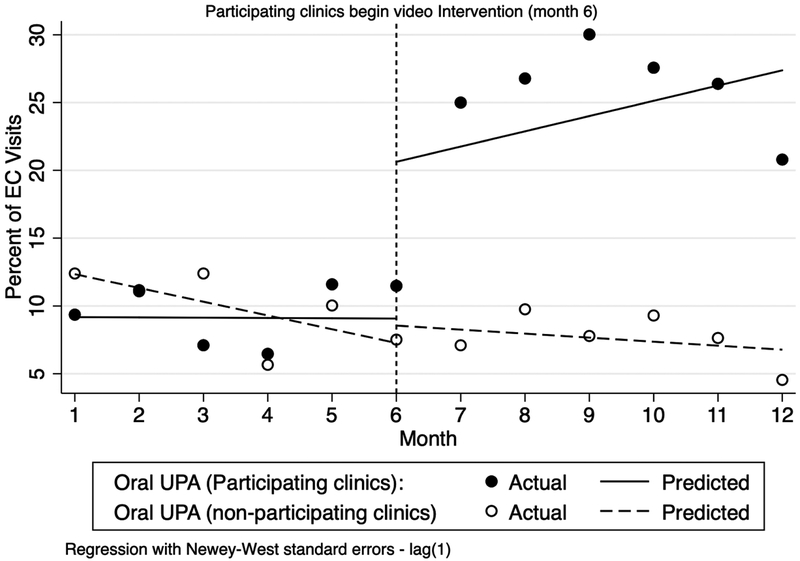
The six health centers with onsite EC dispensing reported 8,269 EC visits during 2015. Of these, 51% (n=4,216) occurred from January-June and 49% (n=4,053) from July-December. Approximately half of visits occurred at the three participating clinics (55%; n=4,581). EC clients at participating and non-participating clinics had similar ages and insurance status; however non-participating clinics had larger proportions of Hispanic, non-white clients (38% versus 22%; p-value<0.001) (Table 1). UPA dispensing increased from 12% (269/2315) pre-intervention to 28% (627/2266) post-intervention (p<0.001) at participating health centers, the other non-participating health centers did not see a change in UPA (10% vs 9%; p-value=0.11). Using the difference-in-differences analysis, the video counseling intervention accounted for an 18% (95%CI 14%−21%) increase in use of UPA at the participating health centers. Figure 1 provides observed monthly proportions of oral LNG and oral UPA among EC clients at participating clinics and non-participating clinics pre- and post- intervention. Figure 2 provides both the observed monthly averages and the regression predicted values of EC method uptake during the pre- and post-intervention periods. In this figure, we visualize the 18% intervention effect as the difference between the observed outcome trends and the unobserved counterfactual. Using multivariable logistic regression, we identified two variables associated with selecting UPA: insurance status and potential for video counseling exposure. Individuals using insurance (Medicaid or private insurance) reported UPA use 3.3 times more often (95%CI 2.7–4.2) than self-pay individuals. Clients seeking EC at sites offering video counseling were more likely to receive ulipristal, even after controlling for age, insurance, and ethnicity (adj.OR 3.4, 95% CI 3.0–3.9).(Table 2).
Table 1.
Demographic characters of Pre- and Post-Intervention by participating (n=3) and non-participating (n=3) clinics January 2015-December 2015, from medical records
| Participating Clinics (n=3) | Non-Participating Clinics (n=3) | |||
|---|---|---|---|---|
| Pre- (n=2315) n (%) |
Post- (n=2266) n (%) |
Pre- (n=1901) n (%) |
Post- (n=1787) n (%) |
|
| Age group | ||||
| ≤21 | 723 (31) | 758 (33) | 639 (34) | 626 (35) |
| 22–25 | 731 (31) | 701 (31) | 603 (32) | 499 (28) |
| 26–29 | 430(19) | 393 (17) | 347 (18) | 301 (17) |
| 30+ | 431 (19) | 414 (18) | 312 (16) | 361 (18) |
| Insurance Status | ||||
| Private | 102 (4) | 111 (52) | 73 (4) | 73 (4) |
| Public | 7 (0.3) | 12 (0.5) | 4 (0.2) | 6 (0.3) |
| None/Self-pay | 2206 (95) | 2143 (95) | 1824 (96) | 1708 (96) |
| Race/Ethnicity | ||||
| White, Non-Hispanic | 1511 (65) | 1539 (68) | 960 (51) | 928 (52) |
| Hispanic, Non-White | 533 (23) | 476 (21) | 733 (39) | 650 (37) |
| Non-Hispanic, Other | 271 (12) | 251 (11) | 208 (11) | 209 (11) |
| Clinic Location | ||||
| Clinic 1A/2A | 398 (17) | 366 (16) | 1388 (73) | 1371 (77) |
| Clinic 1B/2B | 1279 (55) | 1222 (54) | 261 (14) | 244 (14) |
| Clinic 1C/2C | 638 (28) | 678 (30) | 252 1 (13) | 172 (9) |
| EC Type | ||||
| Oral LNG | 2046 (88) | 1639 (72) | 1710 (90) | 1635 (91) |
| Oral UPA | 269 (12) | 627 (28) | 191 (10) | 152 (9) |
p-values all non-significant (p>.10) between pre- and post-intervention with the exception of EC-Type p<0.001. There only statistical difference between participating and non-participating clinics were race/ethnicity (p<0.001) and EC type(p<0.001)
Figure 1.
Medical record data on EC dispensing before and after video counseling was offered at participating health centers, compared to health centers offering no video counseling (Intervention starts month 6)
Figure 2.
Predicted mean monthly proportion of EC users receiving oral UPA at clinics that do and do not offer video counseling, data from medical records (Intervention starts month 6).
Table 2.
Associations between video counseling on emergency contraception and selected EC approach.
| Variables | Unadjusted OR | 95%CI | Adjusted OR* | 95%CI |
|---|---|---|---|---|
| Age (years) | 1.00 | [1.00, 1.00] | 1.01 | [1.00, 1.02] |
| Race/Ethnicity | ||||
| White, Non-Hispanic | REF | REF | REF | REF |
| Hispanic, Non-White | 0.87 | [0.75, 1.00] | 1.02 | [0.88, 1.46] |
| Non-Hispanic, Other | 1.12 | [0.93, 1.35] | 1.20 | [0.99, 1.46] |
| Insurance Used | ||||
| Self-Pay | REF | REF | REF | REF |
| Public or Private | 3.28 | [2.63, 4.08] | 3.31 | [2.64, 4.16] |
| Clinic Location | 1.13 | [1.09, 1.17] | 0.98 | [0.94, 1.02] |
| Intervention | ||||
| Not exposed to video counseling | REF | REF | REF | REF |
| Exposed to video counseling | 3.37 | [2.98, 3.82] | 3.54 | [3.06, 4.10] |
Adjusted for age, ethnicity, insurance status, and clinic location
A total of 2,266 eligible EC visits occurred during the intervention period at participating clinics, 19% (425/2266) of clients opted to watch the video counseling for EC and completed the survey. Individuals completing the survey ranged in age from 16 years to 43 years with a mean of 23 years old. The majority of participants in the video counseling intervention reported being single, non-cohabitating (76%), no prior pregnancies (86%), and annual household incomes of less than $24,000 per year (71%). Table 3 shows the demographics of the intervention participants.
Table 3.
Demographic characteristics of participants who completed surveys after video counseling on emergency contraception (N=425)
| Patient Characteristics | N | % |
|---|---|---|
| Age Group | ||
| 16–18 | 58 | 17.0 |
| 19–21 | 101 | 29.6 |
| 22–25 | 95 | 27.9 |
| 26–29 | 48 | 14.1 |
| 30+ | 39 | 11.4 |
| Relationship Status | ||
| Single/Divorced/Separated | 315 | 75.5 |
| Married/Living with Partner | 102 | 24.5 |
| Race/Ethnicity | ||
| White, Non-Hispanic | 260 | 64.4 |
| Hispanic, Non-White | 95 | 23.5 |
| Other, Non-Hispanic | 49 | 12.1 |
| Gravidity | ||
| Nulligravida | 354 | 85.9 |
| Gravid | 58 | 14.1 |
| Annual Income | ||
| ≤24,000 | 304 | 71.5 |
| 24,001–60,000 | 81 | 19.1 |
| >60,000 | 40 | 9.4 |
| Insurance Status | ||
| None | 154 | 47.1 |
| Public | 28 | 8.6 |
| Private | 145 | 44.3 |
| Education Level | ||
| High school or less | 146 | 35.2 |
| Some college or currently enrolled | 189 | 45.5 |
| College graduation or beyond | 80 | 19.3 |
| Employment Status | ||
| Unemployed/Homemaker | 65 | 16.0 |
| Student | 63 | 15.5 |
| Employed, part-time | 124 | 30.5 |
| Employed, full-time | 155 | 38.1 |
if columns don’t add up to 425 it is due to missing data
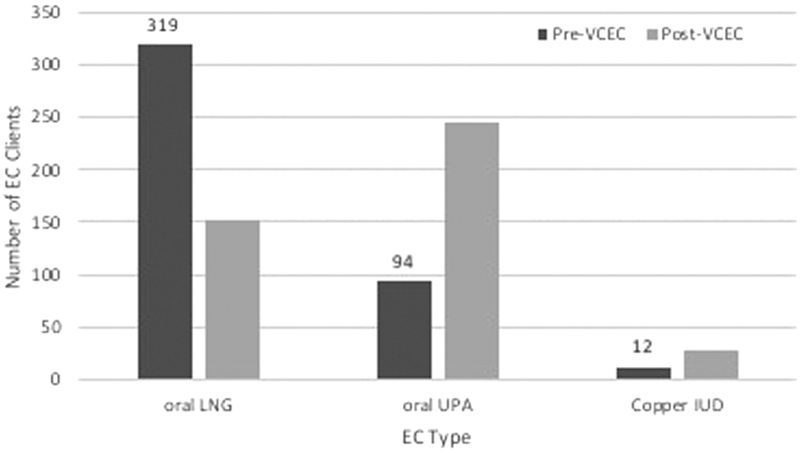
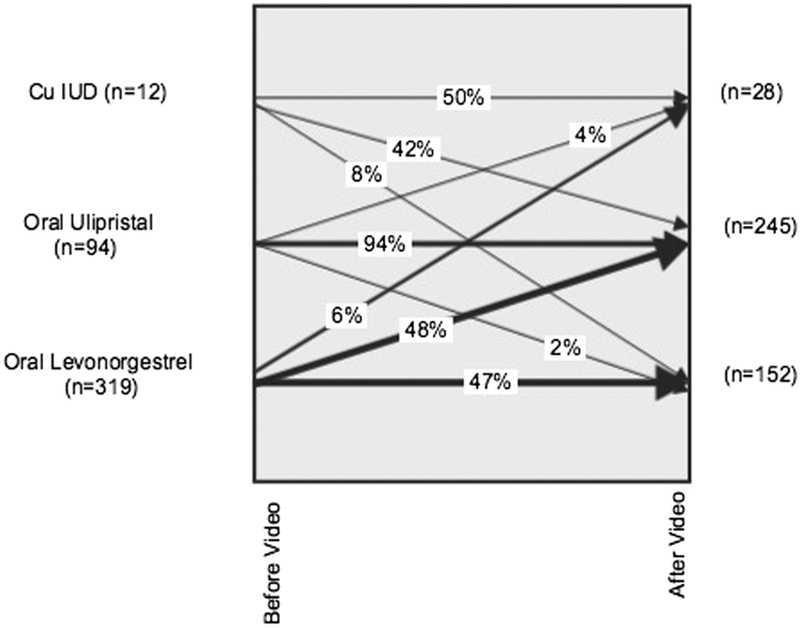
Among those completing the survey, over half (56%) of participants lacked awareness of EC options beyond oral LNG prior to watching the video, two-thirds (67%) did not know of more effective EC options, and three-quarters (77%) did not know that EC efficacy decreased for heavier women (>160lbs). The majority of women (60%) who engaged with the video counseling indicated that the video changed their EC choice they planned to request that day (Figure 3). Among the clients who said they changed their mind, 4% opted for a less effective option, while 96% indicated they changed to selecting a more effective method of EC than originally planned. Overall, 48% of the 319 women who walked into the clinic expecting to obtain oral LNG for EC ended up requesting UPA instead after watching the video. Using multivariable logistic regression, we assessed patient characteristics associated with changing desired EC method after watching the video compared to their desired method before watching the video. Figure 4 demonstrates this changed desire of EC method. Clients who had incomes over $24,000 more commonly reported they had changed their mind after watching the video. Age, ethnicity, insurance, previous pregnancy, and education did not have a significant association with reporting a change in EC method requested after watching the video (Table 4). Overall, patients reported high satisfaction with the video as almost all participants (96%) said they would recommend the the video to other women at the clinic to get EC.
Figure 3.
Preferred methods of EC, before and after video counseling among those receiving video counseling and completing surveys (n=425)
Figure 4.
Change in preferred method of EC after receiving video counseling among those completing surveys (n=425).
Note: The width of arrows corresponds to the proportion of participants reporting that particular combination of EC choices.
Table 4.
Variables associated with participants reporting selection of a method of emergency contraception after receiving video counseling that differed from their initially intended method of emergency contraception(n=425).
| Variables | Unadjusted Odds Ratio | 95% CI | Adjusted Odds Ratio* | 95% CI |
|---|---|---|---|---|
| Age | 1.04 | [1.00, 1.09] | 1.04 | [0.97, 1.11] |
| Race/Ethnicity | ||||
| White, Non-Hispanic | REF | REF | REF | REF |
| Hispanic, Non-White | 1.36 | [0.83, 2.22] | 1.30 | [0.64, 2.63] |
| Non-Hispanic, Other | 1.00 | [0.54, 1.86] | 0.68 | [0.30, 1.54] |
| Insurance Status | ||||
| None | REF | REF | REF | REF |
| Public | 0.97 | [0.43, 2.20] | 0.91 | [0.33, 2.51] |
| Private | 1.20 | [0.75, 1.90] | 0.73 | [0.39, 1.36] |
| Gravidity | ||||
| Nulligravida | REF | REF | REF | REF |
| Gravid | 1.30 | [0.73,2.33] | 0.97 | [0.41, 2.29] |
| Income Category | ||||
| <$24,000 | REF | REF | REF | REF |
| 24,001–60,000 | 1.99* | [1.17, 3.39] | 3.31** | [1.50, 7.32] |
| >60,000 | 1.46 | [0.74, 2.91] | 4.82* | [1.29, 18.00] |
| Highest Level of Education | ||||
| High school or less | 0.92 | [0.59, 1.43] | 0.59 | [0.31, 1.11] |
| Some college or currently enrolled | REF | REF | REF | REF |
| College grad or beyond | 1.02 | [0.60, 1.74] | 0.52 | [0.24, 1.11] |
Adjusted model includes age, race/ethnicity, insurance status, gravidity, annual income, and education.
DISCUSSION
Our findings showed that a brief video intervention can increase the uptake of more effective EC options and is highly acceptable to clients. After the patients viewed the video counseling, 4 out of 10 women decided to change their planned method of EC to a more effective form of EC. Although we lacked the ability to assess the effect of the video counseling on the uptake of IUDs for EC in the clinic data, we did see an increase in self-reports of selecting an IUD among participants in the survey. Additionally, nearly all patients who engaged with the intervention said they would recommend this video to other women seeking EC counseling. Limited prior studies address patient knowledge of EC options. Hickey and colleagues [7, 8] identified patient knowledge gaps pertaining to oral LNG, but did not address knowledge or misconceptions related to oral UPA or the copper IUD for EC. Batur and colleagues [18] addressed knowledge gaps among clinicians, finding that 95% of reproductive health clinicians had heard of oral LNG, with 81% actively prescribing it to patients, and only 52% had heard of UPA with 14% of them prescribing it for EC. Most reproductive health clinicians (83%) had heard of the copper IUD as a method for EC, but only 35% actively prescribed it for this purpose. These knowledge and practice gaps can be attributed to the convenience of oral LNG being offered over the counter. UPA and the copper IUD require more clinician attention. Our study identifies knowledge gaps among EC users, and provides a counseling tool widely accepted by this population of women. This work expands scientific literature to include information on the use of video counseling for EC to discuss alternatives to levonorgestrel pills [19].
A final critical aspect of placing this work in current context involves the complexities of transitioning to other hormonal contraception following UPA. When this video was developed we were unaware that women who initiate oral contraceptives soon after taking ulipristal are more likely to ovulate [20][21]. Current best practice requires sharing this information with women seeking EC, in addition to the information provided in the counseling video we studied.
Study limitations include the small proportion of EC clients that viewed the video counseling (19% of eligible clients). With a limited number of iPads available, clinic staff offered many patients video counseling but they did not want to wait for an iPad to become available. In addition, clinics lacked the ability to provide participant-level data from the clinic records for those exposed to video counseling. Therefore, specific patients who received video counseling could not be followed to confirm their use of their reported EC choice. Additionally, we lack specific data on the population unexposed to video counseling. Selection bias may have played a role in that those with video counseling exposure may have known less about EC, and their exposure could have been driven by the desire for more information about EC. Thus, the surveyed population may not be representative of the entire EC population. We also did not ask about the reasons why participants may or may not have changed their EC strategy. For instance, among the 4% of participants that opted for the less effective options we did not gauge why they changed their mind and if the video influenced the change. Understanding rationale for changes in behavior is an important area of future research. It is possible that clients may have been more comfortable watching the video in a private room rather than a waiting room; however, our team opted to use headphones in the waiting room to reduce disruption to clinic flow and to allow individuals who wished to continue with their purchase of LNG EC to do so without waiting for an exam room.
In conclusion, clinics that encourage women seeking EC to watch a 3-minute video about their EC options, appear to increase the number of women receiving more effective forms of EC.
Acknowledgements:
Local Salt Lake City artist Kate Wolsey designed and animated the video counseling on emergency contraception video (KateWolseyArt). Erica Torres was the voice in the video. The authors would also like to thank Planned Parenthood Association of Utah health center staff at participating locations for all of their hard work, especially Marci Fjelstad, who led the effort.
Funding: The University of Utah Department of Obstetrics and Gynecology Division of Family Planning independently funded the study. We collected and managed study data using REDCap (Research Electronic Data Capture) software hosted at the University of Utah; this service is supported by Center for Clinical and Translational Sciences grant 8UL1TR000105 (formerly UL1RR025764, NCATS/NIH). The University of Utah IRB approved the study (IRB 00071231). Team members receive support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development and the Office of Research on Women’s Health of the National Institute of Health, JNS via Award Number K12HD085852 and DKT via K24HD087436. The content is solely the responsibility of the authors and does not necessarily represent the official view of any of the funding agencies or participating institutions, including the National Institutes of Health, the University of Utah or Planned Parenthood Federation of America, Inc.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest : The Department of Obstetrics and Gynecology, University of Utah, receives contraceptive clinical trials research funding from Bayer, Cooper Surgical (formerly Teva), Medicines360, Merck and Sebela Pharaceuticals. We presented preliminary findings as a poster at the Society of Family Planning’s annual North American Forum on Family Planning in Denver in November 2016. The authors have no conflicts of interest to disclose.
REFERENCES:
- [1].Glasier A, Cameron ST, Blithe D, Scherrer B, Mathe H, Levy D, et al. Can we identify women at risk of pregnancy despite using emergency contraception? Data from randomized trials of ulipristal acetate and levonorgestrel. Contraception 2011;84:363–367. [DOI] [PubMed] [Google Scholar]
- [2].Glasier AF, Cameron ST, Fine PM, Logan SJ, Casale W, Van Horn J, et al. Ulipristal acetate versus levonorgestrel for emergency contraception: a randomised non-inferiority trial and meta-analysis. Lancet 2010;375:555–562. [DOI] [PubMed] [Google Scholar]
- [3].Piaggio G, Kapp N, von Hertzen H. Effect on pregnancy rates of the delay in the administration of levonorgestrel for emergency contraception: a combined analysis of four WHO trials. Contraception 2011;84:35–39. [DOI] [PubMed] [Google Scholar]
- [4].Duramed Pharmaceuticals I. Plan B One-Step (levonorgestrel) tablet, 1.5 mg, for oral use In: FDA, editor.2009. [Google Scholar]
- [5].Cleland K, Zhu H, Goldstuck N, Cheng L, Trussell J. The efficacy of intrauterine devices for emergency contraception: a systematic review of 35 years of experience. Hum Reprod 2012;27:1994–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Dean G, Schwarz EB. Intrauterine Contraceptives In: Hatcher RA, Trussell J, Nelson A, et al. , editors. Contraceptive Technology. 20 ed. New York: Ardent Media; 2011. [Google Scholar]
- [7].Hickey MT, White J. Female college students’ experiences with and perceptions of over-the-counter emergency contraception in the United States. Sex Reprod Healthc 2015;6:28–32. [DOI] [PubMed] [Google Scholar]
- [8].Hickey MT. Female college students’ knowledge, perceptions, and use of emergency contraception. J Obstet Gynecol Neonatal Nurs 2009;38:399–405. [DOI] [PubMed] [Google Scholar]
- [9].Mollen CJ, Miller MK, Hayes KL, Barg FK. Knowledge, attitudes, and beliefs about emergency contraception: a survey of female adolescents seeking care in the emergency department. Pediatr Emerg Care 2013;29:469–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].O’Connor AM, Wennberg JE, Legare F, Llewellyn-Thomas HA, Moulton BW, Sepucha KR, et al. Toward the ‘tipping point’: decision aids and informed patient choice. Health Aff (Millwood) 2007;26:716–725. [DOI] [PubMed] [Google Scholar]
- [11].Sanders JN, Turok DK, Royer PA, Thompson IS, Gawron LM, Storck KE. One-year continuation of copper or levonorgestrel intrauterine devices initiated at the time of emergency contraception. Contraception 2017;96:99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Turok DK, Gurtcheff SE, Handley E, Simonsen SE, Sok C, Murphy P. A pilot study of the Copper T380A IUD and oral levonorgestrel for emergency contraception. Contraception 2010;82:520–525. [DOI] [PubMed] [Google Scholar]
- [13].Turok DK, Gurtcheff SE, Handley E, Simonsen SE, Sok C, North R, et al. A survey of women obtaining emergency contraception: are they interested in using the copper IUD? Contraception 2011;83:441–446. [DOI] [PubMed] [Google Scholar]
- [14].Turok DK, Jacobson J, Simonsen SE, Gurtcheff SE, Trauscht-Van Horn J, Murphy PA. The copper T380A IUD vs. oral levonorgestrel for emergency contraception: a prospective observational study. Contraception 2011;84:321–322. [Google Scholar]
- [15].Turok DK, Sanders JN, Thompson IS, Royer PA, Eggebroten J, Gawron LM. Preference for and efficacy of oral levonorgestrel for emergency contraception with concomitant placement of a levonorgestrel IUD: a prospective cohort study. Contraception 2016;93:526–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Turok DK, Simonsen SE, Marshall N. Trends in levonorgestrel emergency contraception use, births, and abortions: the Utah experience. Medscape J Med 2009;11:30. [PMC free article] [PubMed] [Google Scholar]
- [17].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Batur P, Cleland K, McNamara M, Wu J, Pickle S, Group ECS. Emergency contraception: A multispecialty survey of clinician knowledge and practices. Contraception 2016;93:145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Schwarz EB, Gerbert B, Gonzales R. Computer-assisted provision of emergency contraception a randomized controlled trial. Journal of General Internal Medicine 2008;23:794–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Brache V, Cochon L, Duijkers IJ, Levy DP, Kapp N, Monteil C, et al. A prospective, randomized, pharmacodynamic study of quick-starting a desogestrel progestin-only pill following ulipristal acetate for emergency contraception. Hum Reprod 2015;30:2785–2793. [DOI] [PubMed] [Google Scholar]
- [21].Edelman AB, Jensen JT, McCrimmon S, Messerle-Forbes M, O’Donnell A, Hennebold JD. Combined oral contraceptive interference with the ability of ulipristal acetate to delay ovulation: A prospective cohort study. Contraception 2018;98:463–466. [DOI] [PMC free article] [PubMed] [Google Scholar]