Abstract
Background
In the EFFORT (Effects of Exercise and Diet in Nonobese Asthma Patients – A Randomized Controlled Trial) study, maximum exercise capacity (V′O2max) increased significantly within a 2-month high-intensity spinning period. Furthermore, the study concluded that only the combined exercise and diet intervention improved asthma control, significantly. This study examined whether original improvements in V′O2max and asthma control were present 1 year after intervention completion.
Method
In the original trial, 149 patients were randomised into four study groups. Participants were assessed with an incremental cycle ergometer test and the Asthma Control Questionnaire (ACQ). Of the 149 patients, 66 accepted the follow-up invitation. Participants were distributed in their original groups: exercise group (n=18), diet group (n=117), combined diet and exercise group (n=115) and the control group (n=110). Patients were assessed with original procedures. Though, upon measuring V′O2max, the original four study groups were merged into one spinning group (n=127) and one nonspinning group (n=133).
Results
Comparing the spinning and nonspinning group, there was no significant between-group difference in V′O2max, at 1-year follow-up (p=0.3). In addition, there was no significant between-group difference in ACQ score (p=0.6). Hence, in the combined group, the initial improvement in the ACQ score had regressed to pre-intervention values within 1 year from study completion.
Conclusion
There were no measurable long-lasting effects on V′O2max 1 year after the intervention was completed. Furthermore, there was no long-lasting effect of the combined intervention on asthma control.
Short abstract
This study provides evidence that improvements in maximal oxygen uptake prompted by a 2-month spinning programme regress to pre-intervention values. However, results suggest the presence of long-lasting improvements in self-reported asthma control. http://bit.ly/2wpMQDf
Introduction
Previous studies have shown an association between exercise and dietary interventions and improvements in asthma control, measured on bronchial hyperresponsiveness, airway inflammation and the number of exacerbations [1–3]. In addition, diets with low glycaemic index are associated with decreases in low-grade systemic inflammation [4], a condition associated with asthma. However, the above-mentioned studies revolve around low to moderate exercise interventions, and none of the studies have examined the effect of a combined exercise and diet intervention, in an asthma population. In contrast, the EFFORT (Effects of Exercise and Diet in Nonobese Asthma Patients – A Randomized Controlled Trial) study involved a 2-month supervised high-intensity exercise intervention and/or diet intervention. The study population included 149 nonobese (<30 body mass index (BMI)) patients with asthma randomised into three intervention groups and one nonintervention group (control group). Patients were distributed into an exercise group, diet group, diet and exercise group (combined group), and one control group. Each participant was assessed thoroughly at baseline and following the 2-month intervention period, using various procedures and questionnaires, including the Asthma Control Questionnaire (ACQ). The EFFORT asthma study concluded that patients that underwent an exercise intervention increased V′O2max significantly compared with the control group. Diet alone, had no significant impact on V′O2max. However, only the combined group showed a significant improvement in asthma control, compared with the control group [5]. While the outcomes support findings in similar trials, the long-term effects of high-intensity exercise and dietary interventions in asthma populations remains to be investigated. This 1-year follow-up study intends to examine these potential effects, using V′O2max and asthma control as an indirect measure of behavioural changes. Since the diet intervention alone had no significant effect on this study's primary and secondary outcome, the focus was on the long-term effects of the exercise and combined intervention.
Methods
Patients reconsented upon study entry and prior to any follow-up examinations. The study was approved by the Ethics Committee of Copenhagen, Denmark (H-4-2013-116) and registered at ClinicalTrials.gov (ID: NCT023559464).
Study design
The study was conducted as a follow-up study on the EFFORT asthma trial, 1 year after the trial was completed. In the 1-year follow-up study, participants were kept in their original randomisation groups: 1) exercise group, 2) diet group, 3) combined group and 4) control group.
All patients from the EFFORT asthma trial were invited to participate in the 1-year follow-up study. Participants were initially contacted by e-mail. Upon no response, participants were then contacted by phone. 1 year after completing the 2-month intervention programme, the original V′O2max and ACQ score measurements were repeated. In total, 66 patients were recruited, and 60 were included in the analyses. Following the EFFORT asthma trial, patients from the diet and control group were offered an exercise programme equivalent to the original exercise intervention. Patients that completed the subsequent exercise programme were excluded from the analyses (n=6).
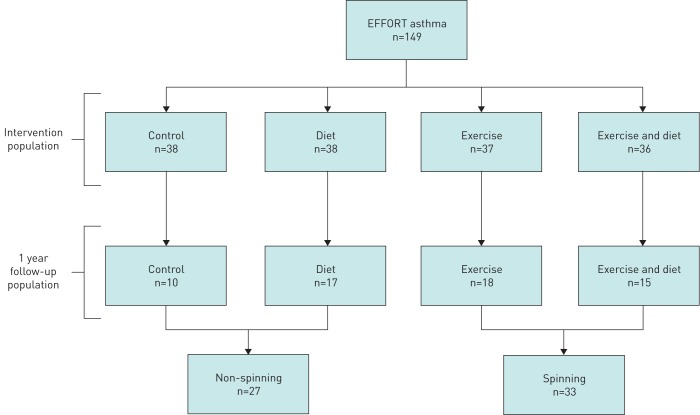
In the final analysis of V′O2max, the four groups were merged into one spinning group (n=27), including patients from the exercise group and the combined group, and one nonspinning group (n=33), including patients from the diet group and the control group (figure 1).
FIGURE 1.
Flowchart. EFFORT: Effects of Exercise and Diet in Nonobese Asthma Patients – A Randomized Controlled Trial.
Outcome assessment
At baseline, forced expiratory volume in the first second (FEV1) and forced vital capacity were measured in each patient. Lung capacity was assessed using spirometry according to European Respiratory Society (ERS) standards [6]. In addition, a skin-prick test was performed at baseline, according to the European standard [7]. Patients were defined as “atopic” if the skin-prick test was positive.
The level of V′O2max, was measured with an incremental cardiopulmonary, cycle ergometer test following the American Thoracic Society guidelines [8].
To determine any changes in fat mass, patients were assessed with a DEXA scan, according to the Osteoporosis Screening Guidelines [9].
Furthermore, asthma control in each participant was evaluated with the validated five-item ACQ (according to the procedure in the original EFFORT asthma trial). The questionnaire addresses asthma symptoms within the past week and general limitations in daily activities [10]. Patients were also asked about their daily use of corticosteroids (ICSs), dosage and number of inhalations, during the last 2 months. Lastly, patients were asked to report on the amount of light, moderate and heavy exercise activity, in minutes a week, during the past 3 months.
Statistical analyses
All statistical analyses were conducted with SPSS version 24.0. Cross-sectional analysis of V′O2max was performed using unpaired t-tests (normally distributed variable). Between-group analyses of patient distributions, ACQ scores and ICS usage were conducted with an ANOVA linear regression model. Categorical variables (e.g. sex, smoking and atopy) were compared using Chi-squared tests.
Results
Patient characteristics
Between-group analyses of baseline characteristics were conducted with participants distributed in their original randomisation groups (exercise group, diet group, combined group, and the control group). There was no significant between-group difference compared on sex, age, smoking habits, BMI, FEV1, and asthma-related atopy (table 1).
TABLE 1.
Pre-intervention characteristics by randomisation group
| Exercise group | Diet group | Combined group | Control group | |
| Patients | 18 | 17 | 15 | 10 |
| Females | 7 (38.9%) | 11 (64.7%) | 11 (73.3%) | 3 (30%) |
| Age years | 41.1±12.7 | 44.1±14.8 | 47.9±10.5 | 41.0±12.8 |
| BMI kg·m−2 | 24.6±2.1 | 24.1±2.6 | 25.7±2.6 | 25.0±1.9 |
| FEV1 % predicted | 88.6±11.8 | 88.1±16.8 | 84.1±13.4 | 89.4±16.0 |
| Smoking | ||||
| Former | 5 (27.7%) | 4 (23.5%) | 6 (40%) | 3 (30%) |
| Never | 12 (66.6%) | 13 (76.4%) | 9 (60%) | 7 (70%) |
| Atopy | 14 (77.7%) | 10 (66.6%) | 10 (76.9%) | 7 (77.7%) |
Data are presented as mean±sd unless otherwise stated. BMI: body mass index; FEV1: forced expiratory volume in 1 s.
Maximal oxygen uptake
There was no significant difference in V′O2max, between the spinning and the nonspinning group, at 1-year follow-up (p=0.3) (table 2). Hence, the original increase in V′O2max, was not detectable 1 year after study completion.
TABLE 2.
Maximal oxygen uptake (V′O2max) by spinning/nonspinning group at 1-year follow-up
| Spinning group | Nonspinning group | p-value | |
| Patients | 29 | 24 | |
| V′O2max mL·min−1 mean±sd | 2848.6±779.0 | 2482.8±692.1 | 0.3 |
p-value denotes the overall significance of differences between the two study groups.
Asthma control questionnaire
Analysis of the ACQ score was also conducted with participants distributed in their original randomisation groups (exercise group, diet group, combined group, and the control group).
Between-group analysis on ACQ scores was nonsignificant (p=0.6). The initial improvement in ACQ score, detected in the combined group, could not be reproduced at the 1-year follow- up (figure 2).
FIGURE 2.
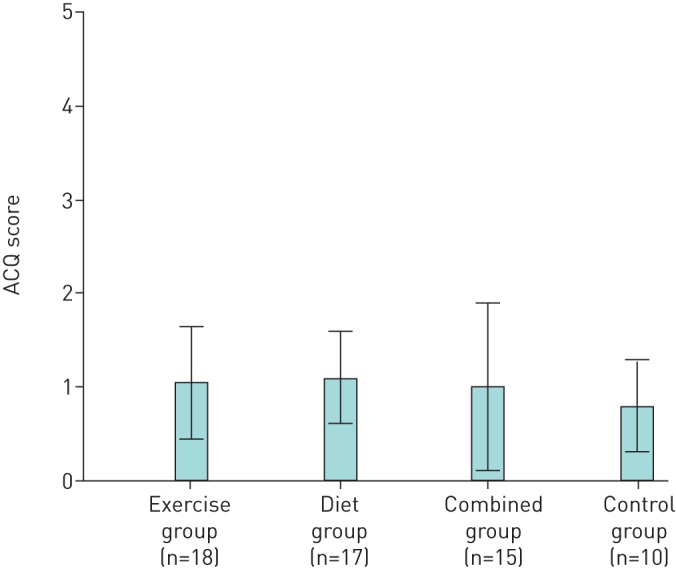
Asthma Control Questionnaire (ACQ) scores by randomisation group, at the 1-year follow up. Results are presented as mean±sd.
Inhaled corticosteroids
The analysis on the daily amount of ICS consumption (ICS prescription adjusted for compliance), was equally conducted with participants distributed in their original randomisation groups: exercise group (452.1 µg·day−1), diet group (436.9 µg·day−1), combined group (578.0 µg·day−1) and the control group (494.0 µg·day−1). Between-group analysis on ICS usage, showed no significant difference in ICS consumption between the four study groups, at the 1-year follow up (p=0.75).
Discussion
In this 1-year follow-up study on supervised dietary and exercise interventions in asthma patients, results showed that V′O2max regressed to pre-intervention levels, 1 year after the intervention was completed. In addition, there were no significant between-group differences in ACQ score. Hence, the 2-month high-intensity exercise programme and dietary intervention did not induce long-lasting behavioural changes.
There are few follow-up studies on diet and exercise interventions and, to our knowledge, no previous follow-up studies in asthma patients. In fact, most recent reviews on lifestyle interventions and behavioural changes call for additional follow-up studies [11–14]. However, our findings support previous outcomes on counselling and behavioural changes in cardiovascular and diabetic patient populations [15–17]. These studies, also, concluded that changes in exercise capacity and dietary habits regressed to pre-intervention levels after counselling was discontinued. The studies, however, primarily revolved around counselling and educational interventions, and the duration of the follow-up periods were longer. Other follow-up studies on patients with chronic obstructive pulmonary disease undergoing pulmonary rehabilitation showed long-term improvements, measured according to the BODE (BMI, airflow obstruction, dyspnoea, exercise capacity) index, 9 to 12 months after the intervention was completed [18, 19].
In contrast, other follow-up studies on supervised exercise interventions in gastric bypass and cancer patients have concluded that the exercise interventions induced long-lasting effects on physical activity and dietary intake habits. These studies involved patients with more immediate life-threatening conditions [20, 21] and therefore possibly less comparable to patients with mild-to-moderate asthma. Although a recent study involving 3×8 weeks of highly supervised exercise interventions during 1 year, in patients with heart transplants, found no significant difference in exercise capacity 5 years after the intervention was completed [22].
Considering this study's outcome, the potential impact of ICS adjustments on ACQ score was taken into consideration. However, between-group analysis on ICS usage, at the 1-year follow-up, was nonsignificant.
There are some limitations to this study; in similar randomised trials, the duration of the intervention period has ranged from 3–6 months. Although the 2-month intervention period in the EFFORT asthma trial was slightly shorter, thorough searches on follow-up studies showed no distinct correlation between the duration of the intervention period and study outcome [23–25]. Furthermore, the study was challenged by a small study population and limited statistical power. Considering the nonsignificant results, the presence of type II errors cannot be excluded. Additionally, the study was susceptible to loss to follow up despite the comprehensive process to re-recruit patients. In contrast with the original EFFORT trial, patients did not directly benefit from participating and only 44% of the patients were re-recruited. Upon recruitment, seasonal aggravation in asthma symptoms was taking into account by examining patients 1 year after entering the original EFFORT trial, with a maximal variation of 2 months.
In conclusion, this real-life follow-up study on patients with mild-to-moderate asthma symptoms provides the first evidence that improvements induced by exercise and dietary interventions, subsides within 1 year from intervention completion.
If physical and dietary interventions were implemented, as a nonpharmacological add-on, in regular asthma treatments, findings suggest that frequent booster interventions, and perhaps longer intervention periods, may be needed to maintain and prolong initial improvements.
Footnotes
This study is registered at www.clinicaltrials.gov with identifier number NCT023559464.
Conflict of interest: A.K. Bentzon has nothing to disclose.
Conflict of interest: L.W. Loehde has nothing to disclose.
Conflict of interest: V. Backer has nothing to disclose.
Conflict of interest: L. Toennesen has nothing to disclose.
References
- 1.Mendes FAR, Goncalves RC, Nunes MPT, et al. Effects of aerobic training on psychosocial morbidity and symptoms in patients with asthma: a randomized clinical trial. Chest 2010; 138: 331–337. [DOI] [PubMed] [Google Scholar]
- 2.Franca-Pinto A, Mendes FAR, de Carvalho-Pinto RM, et al. Aerobic training decreases bronchial hyperresponsiveness and systemic inflammation in patients with moderate or severe asthma: a randomised controlled trial. Thorax 2015; 70: 732–739. [DOI] [PubMed] [Google Scholar]
- 3.Mendes FAR, Almeida FM, Cukier A, et al. Effects of aerobic training on airway inflammation in asthmatic patients. Med Sci Sports Exerc 2011; 43: 197–203. [DOI] [PubMed] [Google Scholar]
- 4.Wood LG, Shivappa N, Berthon BS, et al. Dietary inflammatory index is related to asthma risk, lung function and systemic inflammation in asthma. Clin Exp Allergy 2014; 45: 177–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Toennesen LL, Meteran H, Hostrup M, et al. Effects of exercise and diet in nonobese asthma patients-a randomized controlled trial. J Allergy Clin Immunol Pract 2018; 6: 803–811. [DOI] [PubMed] [Google Scholar]
- 6.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005; 26: 319–338. [DOI] [PubMed] [Google Scholar]
- 7.Dreborg S, Belin L, Eriksson NE, et al. Results of biological standardization with standardized allergen preparations. Allergy 1987; 42: 109–116. [DOI] [PubMed] [Google Scholar]
- 8.American Thoracic Society, American College of Chest Physicians. ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 2003; 167: 211–277. [DOI] [PubMed] [Google Scholar]
- 9.International Society for Clinical Densitometry. Osteoporosis screening guidelines. www.iscd.org/publications/osteoflash/osteoporosis-screening-guidelines/ Date last accessed: December 15, 2018. Date last updated: December 17, 2012.
- 10.Juniper EF, Bousquet J, Abetz L, et al. Identifying “well-controlled” and “not well-controlled” asthma using the Asthma Control Questionnaire. Respir Med 2006; 100: 616–621. [DOI] [PubMed] [Google Scholar]
- 11.Madden SG, Loeb SJ, Smith CA. An integrative literature review of lifestyle interventions for the prevention of type II diabetes mellitus. J Clin Nurs 2008; 17: 2243–2256. [DOI] [PubMed] [Google Scholar]
- 12.Marcus BH, Williams DM, Dubbert PM, et al. Physical activity intervention studies what we know and what we need to know: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular. Circulation 2006; 114: 2739–2752. [DOI] [PubMed] [Google Scholar]
- 13.Fjeldsoe B, Neuhaus M, Winkler E, et al. Systematic review of maintenance of behavior change following physical activity and dietary interventions. Heal Psychol 2011; 30: 99–109. [DOI] [PubMed] [Google Scholar]
- 14.Spark LC, Reeves MM, Fjeldsoe BS, et al. Physical activity and/or dietary interventions in breast cancer survivors: a systematic review of the maintenance of outcomes. J Cancer Surviv 2013; 7: 74–82. [DOI] [PubMed] [Google Scholar]
- 15.Ellingsen I, Hjerkinn EM, Arnesen H, et al. Follow-up of diet and cardiovascular risk factors 20 years after cessation of intervention in the Oslo Diet and Antismoking Study. Eur J Clin Nutr 2006; 60: 378–385. [DOI] [PubMed] [Google Scholar]
- 16.Toobert D, Strycker L, Barrera M, et al. Seven-year follow up of a multiple-health-behaviour-diabetes intervention-HMC. Am J Heal Behav 2010; 34: 680–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baumann S, Toft U, Aadahl M, et al. The long-term effect of screening and lifestyle counseling on changes in physical activity and diet: the Inter99 Study – a randomized controlled trial. Int J Behav Nutr Phys Act 2015; 12: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guell M-R, Cejudo P, Ortega F, et al. Benefits of long-term pulmonary rehabilitation maintenance program in patients with severe chronic obstructive pulmonary disease. Three-year follow-up. Am J Respir Crit Care Med 2017; 195: 622–629. [DOI] [PubMed] [Google Scholar]
- 19.Jacome C, Marques A. Short and long-term effects of pulmonary rehabilitation in patients with mild COPD: A comparison with patients with moderate to severe COPD. J Cardiopulm Rehabil Prev 2016; 36: 445–453. [DOI] [PubMed] [Google Scholar]
- 20.Stacey FG, Lubans DR, Chapman K, et al. Maintenance of lifestyle changes at 12-month follow-up in a nutrition and physical activity trial for cancer survivors. Am J Health Behav 2017; 41: 784–795. [DOI] [PubMed] [Google Scholar]
- 21.Herring LY, Stevinson C, Carter P, et al. The effects of supervised exercise training 12–24 months after bariatric surgery on physical function and body composition: a randomised controlled trial. Int J Obes (Lond) 2017; 41: 909–916. [DOI] [PubMed] [Google Scholar]
- 22.Yardley M, Gullestad L, Bendz B, et al. Long-term effects of high-intensity interval training in heart transplant recipients: A 5-year follow-up study of a randomized controlled trial. Clin Transplant 2017; 31. [DOI] [PubMed] [Google Scholar]
- 23.Schmidt ME, Wiskemann J, Ulrich CM, et al. Self-reported physical activity behavior of breast cancer survivors during and after adjuvant therapy: 12 months follow-up of two randomized exercise intervention trials. Acta Oncol 2017; 56: 618–627. [DOI] [PubMed] [Google Scholar]
- 24.Gauffin H, Sonesson S, Meunier A, et al. Knee arthroscopic surgery in middle-aged patients with meniscal symptoms: a 3-year follow-up of a prospective, randomized study. Am J Sports Med 2017; 45: 2077–2084. [DOI] [PubMed] [Google Scholar]
- 25.Nogueira RC, Weeks BK, Beck B. One-year follow-up of the CAPO kid's trial: are physical benefits maintained? Pediatr Exerc Sci 2017; 29: 486–495. [DOI] [PubMed] [Google Scholar]