Abstract
Introduction: Reflection is formed through deep reflection on the event or a certain clinical position. The aim of this study was to determine the effect of reflection on nurse-patient communication skills of nurses working in emergency departments.
Methods: This interventional study was conducted on intervention and control groups and with a pretest-posttest design. 142 nurses working in the emergency departments of hospitals affiliated to Golestan University of Medical Sciences were enrolled in the study in 2015, and randomly divided into two groups. During eight weeks of the study, the intervention group was asked to write their clinical experiences with regard to communication issues with their patients. Before the intervention, the communication skills of both groups were compared using a questionnaire. Data analysis was performed, using independent t-test, paired t-test, Mann-Whitney and Wilcoxon tests.
Results: Of the 142 nurses, 122 nurses had full participation. In the intervention group the mean scores of verbal communication skills, non-verbal communication skills, general communication skills and communication skills based on patient safety were statistically significant, but there was no significant difference in the control group.
Conclusion: The results showed that eight weeks of reflection by nurses is an effective intervention in dimensions of communication skills. We therefore suggest that a reflective writing be encouraged as a vital tool for improving communication competency among emergency department nurses.
Keywords: Narration, Communication, Emergency nursing
Introduction
Communication skills are taught to nurses in the educational environment and are an important part of educational programs, but there are many concerns about communication weaknesses and lack of communication skills.1 Some nursing experts believe that appropriate communication skills are the cornerstone of all nursing care activities,2 resulting in improved patient care and professional development and personality growth of the nurses.3
Effective communication has positive effects on the patients, including improved vital signs, decreased pain and anxiety, increased satisfaction, improved treatment outcomes, and enhanced participation in treatment programs.4 The emergency room is the busiest and most serious part of any hospital.5 And smooth and organized management of this department can save the lives of many patients. Therefore, in this environment, nurses should be equipped with different capabilities and skills to withstand the pressure and tension, among which communication skills are one of the most important.6 Many qualitative and quantitative studies have evaluated the nurse-patient relationship.7 In a study about nursing care in emergency units, communication has been introduced as one of the elements of care in the emergency room. Therefore, special attention should be paid to effective communication between nurses, patients, their companions, and other care providers in the emergency units.6 Studies conducted in Iran show that the nurse-patient relationship is not quite effective and is even reported to be weak at times.8,9
The art of reflection encourages the person to search for and evaluate solutions in equivocal and complicated situations.10 The experience of utilizing the reflection process in a clinical setting causes a sense of ownership towards the created knowledge in nurses, because they achieve this knowledge through focusing on their own experience, using creative methods.11 The process of reflection starts when the person refers to his/her own experience and recollects what has occurred, reconsiders the experience, and reevaluates it.12 This effective strategy also improves critical thinking and problem-solving skills in nurses.13 Reflection is regarded as a proof of professionalism and is used as a skill related to clinical performance and professional behavior.14 Reflective thinking in recent years has been considered as a learning strategy for nursing students while not being used by novice nurses in practice.15 Studies have suggested that reflective thinking as a skill should be learned and used continuously.16,17 In general, nurses should know how to have reflection on their clinical performance and practice it regularly.Evidence suggests that nurses may not be able to recognize the effects of reflection thinking on their professional development.18 It seems there are some organizational barriers to hinder the use of reflective thinking.19,20 The study by Asselin and Fain on the effectiveness of a continuing education program using individual narratives and group discussion showed that many of the participants couldn’t complete the process of reflection process.21 Kim and colleagues in their study about the effects of a work-based critical reflection program for novice nurses recommended doing similar research with larger and more diverse samples.
Considering the effect of reflection on enhancing clinical activities and the importance of communication skills in advancing the therapeutic objectives and patient satisfaction and because patients are in a state of suspension and abeyance in emergency units, the best of the staff should be employed in these wards. Since university students have been the main target group of the studies conducted in Iran, and there has been no empirical evidence on the outcomes of reflective thinking among nurses in the emergency department, in this research we aimed to evaluate the effect of reflection on nurse-patient communication skills in emergency units.
Materials and methods
This single-blind, randomized, controlled clinical trial was conducted in nurses working in Sayyad Shirazi and Panj-Azar educational hospitals and west healthcare centers (Aqqala Al Jalil Hospital, Bandar Torkaman Imam Khomeini Hospital, Kordkuy Amir-Al-Momenin Hospital, and Bandar-e Gaz Shohada Hospital) with two parallel arms in 2015. The protocol of the study was approved by the ethics Committee of Golestan University of Medical Sciences (code: R.GOUMS. REC. 1394.73) and registered in the Iranian Registry of Clinical Trials (IRCT201501277821N1). The inclusion criteria were a minimum of 6 months’ experience in the emergency units, holding B.Sc or M.Sc. Degrees in nursing, and a negative history of acute stressful events in the past six months (death of fist-degree relatives, use of drugs related to psychotic disorders).
Leaving the emergency units or working in other units for any reason during the study, acute physical or mental crisis during the study (death of relatives, divorce, hospitalization), and incomplete recording of the reflection notebook (less than 4 reflections) were regarded as the exclusion criteria of the study. The participants were given information on the protocol and aims of the study, data anonymity, and confidentiality of the results. Informed consent was obtained from all the participating nurses. The sample size of the study was calculated, using the following formula, considering a study conducted by Hemmati Maslakpak et al.,22 With regards to the above study and an estimate of 80-80% for desirable verbal and non-verbal communication in ICU nurses of Urmia (Iran), an increase of at least 20% in desirable verbal communication was expected to occur after the study. Therefore, considering P1=0.75 and P2=0.95, confidence interval of 95%, and power of 90%, 62 nurses were required in each group (a total of 124 nurses); however, all nurses were included in the study to increase the precision of the study. The participants were allocated to the intervention or control group, using random blocks with block sizes of 4 and 6 and an allocation ratio of 1:1. For allocation concealment, the type of intervention was written on a piece of paper, placed in dark envelopes and numbered sequentially.
The allocation sequencing was done by a person who was not involved in the recruitment, data collection, and analysis. If a participant met the inclusion criteria, his/her name was written on the envelope. The envelopes were opened by the researcher to allocate the participants to either the intervention or control group.
The census method was used to invite all eligible nurses (142 out of 158) who met the inclusion criteria to participate in the study. A random number table generated by the SPSS software was again used to allocate the nurses to intervention and control groups. After obtaining informed consents and before the intervention, the nurse-patient communication skills questionnaire developed by Hemmati Maslakpak et al.,22 was completed by the nurses in both groups. In their study the average content validity index (0.887) and reliability coefficient of the questionnaire (alpha-coronbach = 0.96) were confirmed. In the present study the total Cronbach's alpha coefficient of questionnaire was 0.919 and for different dimensions were as verbal: 0.884, non-verbal: 0.848, and patient-based safety skill: 96.03, which indicates an acceptable homogeneity.
The participants in both groups were requested to complete the questionnaire once more after eight weeks. Special notebooks were designed based on the Gibb’s reflective cycle, and were given to the intervention group for reflective writing. Code 0 was assigned to the control group (n=71) and code 1 was given to the intervention group (n=71). Blinding: This study was a single-blind trial; in other words, the research assistant who collected the questionnaires was not aware of the allocation. After coordination with the nursing office of the afore-mentioned health centers, the schedule of the rotating shifts of the nursing staff of emergency units was obtained and then a briefing session was held about the process of work. The participants completed the nurse-patient communication skills questionnaire. Nurses in the intervention group practiced reflection at least once a week for 8 weeks. Since the purpose of this study was not to analyze the participants' notes in detail, the handwritten notes were only checked for relevance in relation to the communication skills with patients. There was no specific guideline to determine the length of reflective writing and national and international studies have reported different periods, so their average was used in this study. In reflection, based on the Gibb’s model, although there is no need to require the participants to adopt a certain framework, the following guide may help a person organize their thoughts and feelings:
What happened?
What were your reactions and feelings?
What was good or bad about the experience?
What did you learn from this situation?
What else could you do?
What will you do if it occurs again?23
According to the Gibb’s reflective cycle, the participants were asked to reflect on their clinical experiences and write their best and worst experience of communication with the patient and their companions, the most difficult moment, and the best moment. No intervention was applied in the control group. The participants completed the nurse-patient communication skills questionnaire before the study and also at the end of eight weeks, and then they were asked to complete the questionnaire. The collected data included demographic (age, sex, ethnicity, marital status) and occupational characteristics (work experience, type of employment, position, ward).
The questionnaire had three sections including verbal and non-verbal communication skills (21 questions) and patient safety-related communication skills (27 questions). The questions were scored, using a 5-point Likert scale as always (5 points), often (4 points), sometimes (3 points), rarely (2 points), and never (1 point).According to the total score, the verbal and non-verbal communication skills were categorized as weak (score: 21-48), moderate (score: 49-76), and good (score: 77-105), and patient safety-related communication skills were categorized as weak (score: 18-41), moderate (score: 42-65), and good (score: 66-90). A higher score indicated a better communication performance. The Cronbach’s alpha was 0.96 for the whole questionnaire, 0.87 for verbal communication section, 0.92 for non-verbal communication section, and 0.95 for patient safety-related communication section.22 The SPSS software, version 13 (IBM, Armonk, NY, USA) was used for analysis. The Kolmogorov-Smirnov and Shapiro-Wilk tests were applied to evaluate data normality. To determine the difference between quantitative variables in each group, independent t-test and paired t-test were used if the data were distributed normally and Mann-Whitney and Wilcoxon tests were used if the data distribution was not normal. P- values less than 0.05 were considered significant
Results
The present study was conducted from September 2015 until January 2016. Of 158 eligible nurses, 142 met the inclusion criteria of whom 71 were allocated to the intervention group and 71 were allocated to the control group. Finally, the data of 122 participants were analyzed (Fig. 1). The mean age of the participants was 29.97 (6.14) years, with 64.5% of the nurses in the control group and 60% of the nurses in the intervention group being female. There was no significant difference in demographic characteristics between the two groups (Table 1).
Figure 1.
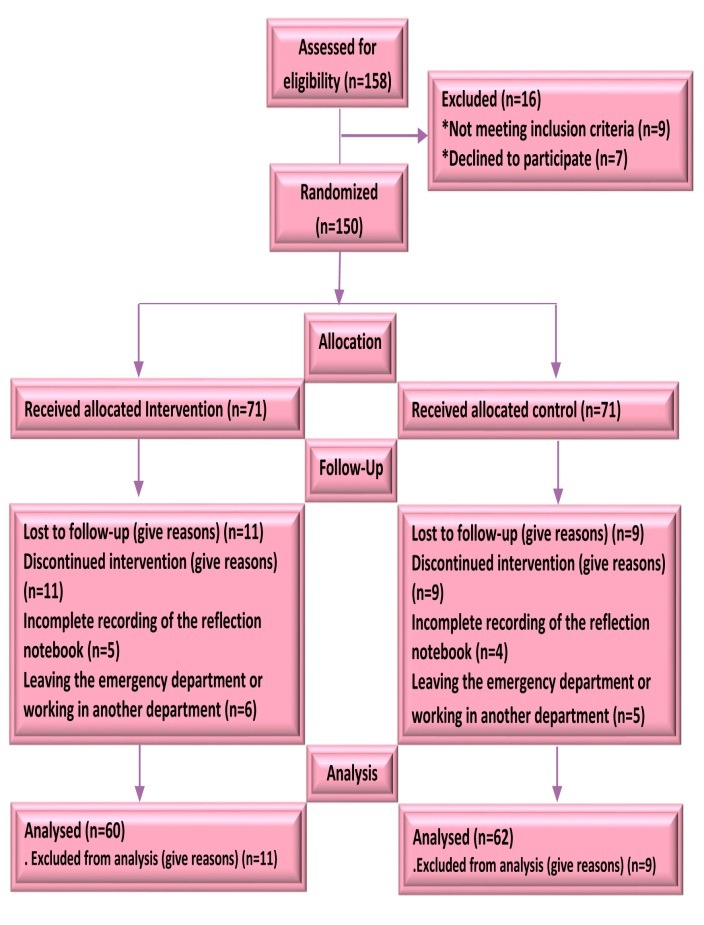
Flow chart of the participants through each
Table 1. Comparison of demographic and job variables among the participants in intervention and control group .
| Group Variable |
Intervention
group (N=60) |
Control
group (N=62) |
P |
| Age | 29.93 (5.4) | 30.01 (6.83) | 0.64b |
| Work experience (yrs)a | 6.24 (4.64) | 6.8 (5.74) | 0.96b |
| Work experience in emergency department (yrs)a | 3.21 (2.89) | 4.03 (4.01) | 0.05b |
| Genderd | 0.6c | ||
| Female | 36 (60) | 40 (64.5) | |
| Male | 22 (35.5) | 24 (40) | |
| Educationd | 0.99f | ||
| BSN | 59 (98.3) | 60 (96.8) | |
| MSN | 1 (1.17) | 2 (3.2) |
aMean (SD), bMann–Whitney U, cChi square, dn (%), eChi-square for trend, fFisher's exact test
The Shapiro-Wilk test was used to evaluate the normal distribution of quantitative continuous variables. Age, total work experience in hospitals, work experience in the emergency units, and nurse-patient communication skills had a non-normal distribution (P>0.05). A significant difference was observed in the score of verbal communication skills before and after the intervention in the intervention group (P<0.001) while the difference was not significant in the control group (P<0.418).
The difference in the score of non-verbal communication skills before and after the intervention was significant in the intervention group (P<0.001) while no significant difference was observed in the control group (P<0.413).
Moreover, there was a significant difference in patient safety related communication skills before and after the intervention in the intervention group (P<0.001); however, the difference was not significant in the control group (P<0104).
In general, a significant difference was seen in the total score of communication skills before and after the intervention in the intervention group (P<0.001) while no significant difference was observed in the control group (P<0.872) (Table 2).
Table 2. Comparison of the effect reflective journaling on communication skills in intervention and control groups .
| Group |
Intervention group
(N=60) |
Control
group (N=62) |
P |
| Variable and Time | Mean (SD) | Mean(SD) | |
| Verbal communication skill | |||
| Before intervention | 70.57 (12.97) | 80.30 (12.38) | 0.001a |
| After intervention | 91.25 (6.41) | 79.18 (10.63) | 0.001a |
| P | 0.001b | 0.41b | |
| Differences before and after the test | 20.67 (11.73) | -1.11 (10.78) | 0.001a |
| Non-verbal communication skills | |||
| Before intervention | 67.18 (14.92) | 77.62 (14.93) | 0.001a |
| After intervention | 89.21 (8.63) | 80.04 (11.12) | 0.001a |
| P | 0.001 b | 0.24b | |
| Differences before and after the test | 22.03 (16.25) | 2.41 (16.51) | 0.001a |
| Communication skills based on patient safety | |||
| Before intervention | 65.34 (14.74) | 78.28 (12.01) | 0.001a |
| After intervention | 89.93 (6.61) | 75.89 (7.62) | 0.001a |
| P | 0.001b | 0.10b | |
| Differences before and after the test | 24.59 (16.14) | -2.8 (11.4) | 0.001a |
| Total communication skill | |||
| Before intervention | 69.28 (12.5) | 79.28 (12.18) | 0.001a |
| After intervention | 90.47 (6.22) | 79.51 (9.11) | 0.001a |
| P | 0.001 b | 0.87b | |
| Differences before and after the test | 21.19 (12.04) | 0.23 (11.23) | 0.001a |
aMann–Whitney U, bWilcoxon
Discussion
The main findings of this study show that the reflective writing had a positive effect on the nurses’ clinical communication abilities. A significant difference was observed in verbal, non-verbal, and patient safety-related communication skills before and after the intervention while the difference was insignificant in the control group.
This study assessed the effect of reflection on communication skills of clinical nurses for the first time in Iran. Most national studies on reflection, such as those conducted by Sedaghti et al.,24 Abedini et al.,25 and Dehghany et al.,26 have mainly been of observational types. Moreover, most of the studies investigating the nurses’ communication skills were descriptive or related to reflection in the students. The results of the present study are in line with previous research findings according to which work-based critical reflection program or reflective journaling by hospital nurses (through fellowship program) improved critical thinking skills, communication abilities, and job performance.27,28
Fukui et al., showed that communication skills training improved the patients’ quality of life and increased the nurses’ job satisfaction.29 With regards to weak communication skills in clinical environments and their potential effects on the nurses, interventions are required to enhance these skills. It seems that the traditional teaching methods are not effective enough. A study by Heaven et al., revealed that despite the effectiveness of educational workshop, it was comparatively less effective in clinical environment, indicating the need for more clinical supervision and intervention in practice.29
Reflection enables the learners to search for their roles and responsibilities in an interdisciplinary context and enhance their verbal and teamwork skills. In the present study, among the three types of skills, verbal skills had the highest mean score after the intervention. Verbal communication skills are behaviors such as greetings, introducing to patients, and using open questions. It seems that the nurses had the highest score in their verbal skills because such behaviors are common in the practice.
The reflective writing helped nurses pay more attention to such apparently simple behaviors. Consequently, reflective thinking promoted positive social behaviors in communicating with their patients.
These findings are consistent with the results of a study by Lestander et al., in which the participants stated that their verbal communication skills with patients improved after three reflection sessions (two individual sessions and one group session), leading to their increased efficacy in the nursing profession.30 A study by Pai et al., showed that simulated learning opportunities with feedback, debriefing, and guided reflection enhanced critical thinking, clinical judgment, verbal communication skills and caring skills. Therefore, self-reflection may play an effective role in improving the nurses’ verbal communication skills.31 In that study, the participants also stated that reflective thinking helped them to use proper phrases to encourage patients to express their feelings or to try to provide training in plain and intelligible language. In a study by Abedini et al., on the effectiveness of reflection in clinical education, most of the students believed that reflection increased their communication and social skills.25 Therefore, verbal skills are an important part of nurse-patient communication skills and accurate identification of factors affecting verbal skills is required to improve them. The results of the present study also showed the high score of non-verbal communication skills (such as proper eye contact with the patient, body gesture and head movements or listening to the patient) of the nurses working in the emergency rooms. In a study by Thomas et al., the majority of patients needed non-verbal communication.32
Heinerichs et al., assessed the effect of non-verbal communication skills through videotaping and debriefing of clinical skills. The results showed non-verbal communication skills improved in 96% of the students and 98% of the students mentioned non-verbal communication skills as a proper means of communication.33 Although, in the present study, before and after the intervention, the non-verbal communication skills of the nurses increased in the intervention and control groups, this difference was only significant in the intervention group, which could be due to the rethinking and contemplation of nurses in their daily experiences of communicate with patients. The results of the present study also showed that nurses had good patient safety-related communication skills. Similarly, the results of a study by Hemmati et al., showed that from the perspective of the nurses, patient safety was in a good level for most patients hospitalized in the intensive care units of educational hospitals.22 However, some studies have reported contradictory results regarding patient safety.33,34 The domain of patient safety-related communication skills has a direct association with clinical competency of the nurses and their professionalism,27 which was significantly enhanced through reflection in our study. Pearson et al., noted that reflection by surgical residents improved their medical performance, communication, and professionalism.35 Moghadami et al., evaluated the effect of reflection on nurse-patient communication skills in nursing students, but found no significant difference in the students’ therapeutic communication skills between the two groups. Although clinical reflection was associated with an increase in the mean score of therapeutic communication skills, the difference was not significant.36 It is important for all nurses to possess communication abilities; therefore, those nurses working in the emergency unit are not exempt from this requirement. So, it is critical to help them improve their communication verbal and non-verbal abilities and patient safety through reflective writing, which is an easy and non-expensive approach.
The present study had certain limitations. Since the previous studies had not suggested a specific period for performing the narrative writing, a period of “eight weeks” was considered for the intervention based on the available evidence,. So it has to be admitted that a decrease or increase in this period could have been accompanied by other consequences not found in the present study. Due to mandatory rotating work shifts, the communication between the intervention and control groups was inevitable and there was a possibility of transmission of intervention into the control group. However, the fact that the participants had been selected from different hospitals (teaching hospitals, governmental hospitals), and from different cities of the same province can be considered as a strength of this research. Suggestions for further studies: It is suggested that in the future studies, the effect of group oral reflection on communication skills of nurses working in emergency units be investigated. Also, the effect of reflective narration on the patients’ safety and clinical errors and the other core clinical competencies can be studied. Exploring the effect of self-reflective narration through e-mail sounds interesting too. Implication for nursing: Every health care system should equip its nurses with good communication skills. Since reflective thinking leads to the development of critical thinking, it is expected that better decisions can be made by nurses in relation to patients, and better communications with patients can thus be established. It is, thus, recommended nurses’ administrators incorporate reflective writing into in-service training and use that as a tool for making sense in emergency units, learning and art in care practices.
Conclusion
The reflective writing not only had a positive effect on verbal, non-verbal and general communication skills, but also helped nurses to have better communication skills based on patient safety. In other words, reflection enables the nurses to support the patients more effectively in each stage and have a more prominent role in the health despite limitations in resources and the high work load. For these reasons, such a program could be considered an important tool for improving communication competency among nurses in emergency units. This educational approach emphasizes health, hopefulness, and positive thinking; therefore, it is consistent with the philosophy of nursing care and may be used in different situations like routine clinical care.
Acknowledgments
The authors wish to thank the education development center and deputy of Research, Golestan University of Medical Science, as well as the officials and emergency wards’ staff of the hospitals for their participations. This article was derived from a master thesis of at Golestan University of Medical Sciences, Gorgan, Iran.
Ethical issues
None to be declared.
Conflict of interest
The authors declare no conflict of interest in this study.
Citation: Pangh B, Jouybari L, Vakili MA, Sanagoo A, Torik A. The effect of reflection on nurse-patient communication skills in emergency medical centers. J Caring Sci 2019; 8 (2): 75-81. doi:10.15171/jcs.2019.011.
References
- 1.Merckaert I, Delevallez F, Gibon AS, Lienard A, Libert Y, Delvaux N. et al. Transfer of communication skills to the workplace: impact of a 38-hour communication skills training program designed for radiotherapy teams. Journal of Clinical Oncology. 2015;33(8):901–9. doi: 10.1200/jco.2014.57.3287. [DOI] [PubMed] [Google Scholar]
- 2.Bramhall E. Effective communication skills in nursing practice. Nursing Standard. 2014;29(14):53–9. doi: 10.7748/ns.29.14.53.e9355. [DOI] [PubMed] [Google Scholar]
- 3.Powell AE, Davies HTO. The struggle to improve patient care in the face of professional boundaries. Social Science and Medicine. 2012;75(5):807–14. doi: 10.1016/j.socscimed.2012.03.049. [DOI] [PubMed] [Google Scholar]
- 4.Hemsley B, Balandin S, Worrall L. Nursing the patient with complex communication needs: time as a barrier and a facilitator to successful communication in hospital. J Adv Nurs. 2012;68(1):116–26. doi: 10.1111/j.1365-2648.2011.05722.x. [DOI] [PubMed] [Google Scholar]
- 5.Abbasi S, Farsi D, Bahrani M, Davari S, Pishbin E, Kianmehr N. et al. Emergency medicine specialty may improve patient satisfaction. Medical Journal Of The Islamic Republic of Iran (MJIRI) 2014;28:61. (Persian) [PMC free article] [PubMed] [Google Scholar]
- 6.Jones T, Shaban RZ, Creedy DK. Practice standards for emergency nursing: An international review. Australas Emerg Nurs J. 2015;18(4):190–203. doi: 10.1016/j.aenj.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 7. Arnold E.C, Boggs K.U. Interpersonal Relationships-E-Book: Professional Communication Skills for Nurses. 8th ed. Elsevier Health Sciences, Printed in China; 2019. (ebook).
- 8.Aein F, Alhani F, Mohammadi E, Kazemnejad AN. Marginating the interpersonal relationship: Nurses and parent's experiences of communication in pediatric wards. Iranian Journal of Nursing Research. 2008;3(9):71–83. (Persian) [Google Scholar]
- 9.Rostami H, Mirzaei A, Golchin M. Evaluation of communication skills of nurses from hospitalized patients' perspective. Journal of Urmia Nursing and Midwifery Faculty. 2012;10(1):27–34. (Persian) [Google Scholar]
- 10.Weingarten K. The Art of Reflection: Turning the strange into the familiar. Family Process. 2016;55(2):195–210. doi: 10.1111/famp.12158. [DOI] [PubMed] [Google Scholar]
- 11. Kakar AK, Teaching theories underlying agile methods in a systems development course. System Sciences (HICSS). 47th Hawaii International Conference on System Sciences. 2014.
- 12.Clynes MP. A novice teacher’s reflections on lecturing as a teaching strategy: Covering the content or uncovering the meaning. Nurse Education in Practice. 2009;9(1):22–7. doi: 10.1016/j.nepr.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 13.Naber J, Wyatt TH. The effect of reflective writing interventions on the critical thinking skills and dispositions of baccalaureate nursing students. Nurse Education in Practice. 2014;34(1):67–72. doi: 10.1016/j.nedt.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Cooke M, Walker R, Creedy D, Henderson A. clinical progression portfolio: A resource for enhancing learning partnerships. Nurse Education in Practice. 2009;9(6):398–402. doi: 10.1016/j.nepr.2009.01.020. [DOI] [PubMed] [Google Scholar]
- 15.Asselin ME, Schwartz-Barcott D. Exploring problems encountered among experienced nurses using critical reflective inquiry: implications for nursing professional development. J Nurses Prof Dev. 2015;31(3):138–44. doi: 10.1097/NND.0000000000000145. [DOI] [PubMed] [Google Scholar]
- 16.Asselin ME. Reflective narrative: A tool for learning through practice. J Nurs Prof Dev. 2011;27(1):2–6. doi: 10.1097/NND.0b013e3181b1ba1a. [DOI] [PubMed] [Google Scholar]
- 17.Taylor B. Reflective practice for healthcare professionals: a practical guide. UK: McGraw-Hill Education; 2010. [Google Scholar]
- 18.Welp A, Johnson A, Nguyen H, Perry L. The importance of reflecting on practice: How personal professional development activities affect perceived teamwork and performance. Journal of Clinical Nursing. 2018;27(21-22):3988–99. doi: 10.1111/jocn.14519. [DOI] [PubMed] [Google Scholar]
- 19.Johnson JA. Reflective learning, reflective practice, and metacognition: the importance in nursing education. J Nurses Prof Dev. 2013;29(1):46–8. doi: 10.1097/NND.0b013e31827e2f27. [DOI] [PubMed] [Google Scholar]
- 20.Gustafsson C, Fagerberg I. Reflection, the way to professional development? Journal of Clinical Nursing. 2004;13(3):271–80. doi: 10.1046/j.1365-2702.2003.00880.x. [DOI] [PubMed] [Google Scholar]
- 21.Asselin ME, Fain JA. Effect of reflective practice education on self-reflection, insight, and reflective thinking among experienced nurses: A pilot study. J Nurses Prof Dev. 2013;29(3):111–9. doi: 10.1097/NND.0b013e318291c0cc. [DOI] [PubMed] [Google Scholar]
- 22.Hemmati Maslakpak M, Sheikhi N, Baghaie R, Sheikhbaklu M. Study the performance of nurses communication with patients in special education and non-teaching hospital, Urmia. Journal of Urmia Nursing and Midwifery Faculty. 2012;10(2):286–94. (Persian) [Google Scholar]
- 23.Palsson Y, Engstrom M, Leo Swenne C, Martensson G. A peer learning intervention targeting newly graduated nurses: A feasibility study with a descriptive design based on the medical research council framework. Journal of Advanced Nursing. 2018;74(5):1127–38. doi: 10.1111/jan.13513. [DOI] [PubMed] [Google Scholar]
- 24.Sedaghati M, Ezadi A. The effectiveness of reflection in clinical education based on nursing students perspective in Islamic Azad University-tonekabon in 2013. Journal of Urmia Nursing and Midwifery Faculty. 2014;12(3):221–9. (Persian) [Google Scholar]
- 25.Abedini Z, Raeisi M. Effectiveness of reflection in clinical education: nursing students’ perspective. Iran Journal of Nursing. 2011;24(71):74–82. (Persian) [Google Scholar]
- 26.Dehghany Z, Abbasizadeh A, Moattari M, Bahreini M. Effective reflection on clinical competency of nursing students. Payesh. 2012;12(1):63–70. (Persian) [Google Scholar]
- 27.Kim YH, Min J, Kim SH, Shin S. Effects of a work-based critical reflection program for novice nurses. BMC Med Educ. 2018;18(1):30. doi: 10.1186/s12909-018-1135-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zori S, Kohn N, Gallo K, Friedman MI. Critical thinking of registered nurses in a fellowship program. Journal of Continuing Education in Nursing. 2013;44(8):374–80. doi: 10.3928/00220124-20130603-03. [DOI] [PubMed] [Google Scholar]
- 29.Fukui S, Ogawa K, Yamagishi A. Effectiveness of communication skills training of nurses on the quality of life and satisfaction with healthcare professionals among newly diagnosed cancer patients: a preliminary study. Psycho-Oncology. 2011;20(12):1285–91. doi: 10.1002/pon.1840. [DOI] [PubMed] [Google Scholar]
- 30.Lestander O, Lehto N, Engstrom A. Nursing students' perceptions of learning after high fidelity simulation: Effects of a three-step post-simulation reflection model. Nurse Education Today. 2016;40:219–24. doi: 10.1016/j.nedt.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 31.Pai HC. An integrated model for the effects of self-reflection and clinical experiential learning on clinical nursing performance in nursing students: A longitudinal study. Nurse Education Today. 2016;45:156–62. doi: 10.1016/j.nedt.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 32.Thomas LA, Rodriguez CS. Prevalence of sudden speechlessness in critical care units. Clinical Nursing Research. 2011;20(4):439–47. doi: 10.1177/1054773811415259. [DOI] [PubMed] [Google Scholar]
- 33.Heinerichs S, Cattano NM, Morrison KE. Assessing nonverbal communication skills through video recording and debriefing of clinical skill simulation exams. Athletic Training Education Journal. 2013;8(1):17–22. doi: 10.4085/08010217. [DOI] [Google Scholar]
- 34.Nagpal K, Vats A, Lamb B, Ashrafian H, Sevdalis N, Vincent C. et al. Information transfer and communication in surgery: a systematic review. Annals of Surgery. 2010;252(2):225–39. doi: 10.1097/SLA.0b013e3181e495c2. [DOI] [PubMed] [Google Scholar]
- 35.Manser T. Teamwork and patient safety in dynamic domains of healthcare: a review of the literature. Acta Anaesthesiologica Scandinavica. 2009;53(2):143–51. doi: 10.1111/j.1399-6576.2008.01717.x. [DOI] [PubMed] [Google Scholar]
- 36.Moghadami A, Jouybari L, Baradaran HR, Sanagoo A. The effect of narrative writing on communication skills of nursing students. Journal of Urmia Nursing and Midwifery Faculty. 2016;16:149–56. (Persian) [Google Scholar]


