Abstract
Chronic migraine is a frequent and debilitating condition affecting 14% of the general population. This prospective observational pilot study investigated whether men with chronic migraine have lower than expected total serum testosterone levels. We identified 14 men ages 26-51 at our Institution who fulfilled the ICHD-3b criteria for chronic migraine and obtained serum total testosterone levels. The mean total testosterone level in our 14 patients was 322 ng/dL (range: 120-542 ng/dL) which is in the lower 5% of the reference range for our laboratory (300-1080 ng/dL). Men with chronic migraine had lower total testosterone levels compared to published agematched normative median values by a median difference of 62 ng/dL (P=0.0494). This finding suggests that hypothalamic regulation is altered in patients with chronic migraine. Further studies are warranted to determine whether testosterone supplementation in men with chronic migraine reduces the number of headaches or the associated symptoms of hypogonadism.
Key words: Neurology, Migraine, Testosterone, Hypothalamus, Hypogonadism
Introduction
Migraine is a common, multifactorial, disabling primary headache disorder.1,2 According to the International Classification of Headache Disorders, 3rd edition (beta version), chronic migraine refers to a headache occurring on 15 or more days per month for more than 3 months which has the features of migraine on at least 8 days per month.2 According to the National Health Interview Survey in 2012, the overall prevalence of migraine or severe headache is 14.2% in the United States, with 19.1% of females and 9.0% of males affected with substantial variations depending on age.3 Migraine ranked as the third most common cause of disability worldwide in individuals under 50 as reported by the Global Burden of Disease Survey 2015.4 Migraines are considered to involve the hypothalamus, brainstem, and cortex which regulates autonomic, affective, cognitive, and sensory functions.1 Chronic migraine may affect hypothalamic hormonal secretion. Many men with chronic migraine exhibit symptoms that are frequently seen with hypogonadism (depressed mood, reduced energy, difficulty concentrating).
Positron emission tomography (PET) has shown hypothalamic activation in spontaneous migraine attacks which persists after headache relief by sumatriptan.5,6 Attention has focused on the function of the hypothalamus in circadian rhythms, pain control coordinating the activity of the sympathetic and parasympathetic nervous systems, and in maintaining homeostasis.1,5,7 In addition, the hypothalamus is integrally involved with the body’s responses to stress.7 The hypothalamus secretes gonadotropin-releasing hormone (GnRH) which stimulates the anterior pituitary gland to release luteinizing hormone (LH) from the gonadotrophs.8 The receptors for LH are located on Leydig cells in the testis which synthesize testosterone following LH stimulation. 8 Figure 1 depicts the hypothalamic regulation of testosterone.
Figure 1.
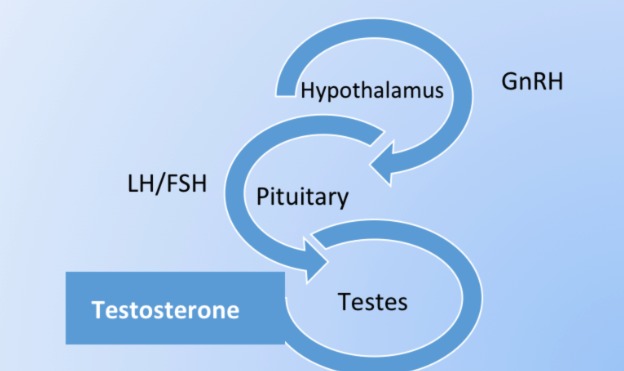
Hypothalamic regulation of testosterone.
There are no reports known to the authors on the effect that chronic migraine may have on testosterone levels in men. We investigated whether men with chronic migraine have lower than expected total serum testosterone levels. In this prospective pilot study, we present our findings pertaining to the interaction between chronic migraine and testosterone levels. We also discuss the impact of chronic migraine on the regulation of the hypothalamo-pituitarygonadal axis.
Materials and Methods
Patient population
Under an institutional review board (IRB) approved protocol, we prospectively identified 14 men who fulfilled the ICHD- 3b criteria for chronic migraine without opioid or barbiturate overuse at our Institution. These patients were evaluated by a neurologist at our Institution’s outpatient clinic in a metropolitan community. All men obtained serum total testosterone levels. These values were compared to the local laboratory normal values and to published agematched controls.9
Statistical analysis
Data are presented in listings and summarized as either mean (SD) or median (interquartile range: 25th %-tile & 75th %- tile). To test whether the testosterone distribution amongst those men with migraines differed from a control population distribution, the median testosterone from a published age-specific control population was matched to the age-specific testosterone level for the 14 migraine subjects.9 To assess whether these age-matched groups differed, Wilcoxon Signed Rank test was used to test for the testosterone distribution difference. An a-priori two-sided significance level of 5% was used to interrogate any observed difference.
Results
A total of 14 men fulfilled the criteria for inclusion. The mean age was 36.1 years (range: 26-51 years). The local laboratory normal range for total testosterone was 300-1080 ng/dL. Table 1 illustrates the total testosterone levels of migraine patients compared to published age-matched controls. The mean total testosterone level in the 14 patients with chronic migraine was 322 ng/dL (range: 120-542 ng/dL).
Table 1.
Total testosterone levels of migraine patients compared to published age-matched controls.
| Age | Total testosterone of migraine patients (ng/dL) | Normal for reference lab (1=yes;0=no) | Total testosterone of published age-matched controls (ng/dL)* |
|---|---|---|---|
| 26 | 406 | 1 | 406 |
| 27 | 428 | 1 | 403 |
| 30 | 120 | 0 | 392 |
| 32 | 434 | 1 | 386 |
| 33 | 270 | 0 | 383 |
| 33 | 324 | 1 | 383 |
| 34 | 378 | 1 | 383 |
| 35 | 268 | 0 | 380 |
| 37 | 542 | 1 | 378 |
| 38 | 360 | 1 | 378 |
| 40 | 230 | 0 | 375 |
| 42 | 310 | 1 | 375 |
| 48 | 196 | 0 | 375 |
| 51 | 245 | 0 | 375 |
Normal Testosterone Range (Local Reference Lab): 300-1080 ng/dL. *See Kelsey et al. 2014.9
For published age-matched controls, the mean total testosterone level was 384 ng/dL (SD=10.3). Six males (43%) had testosterone levels below the minimum of the normal local laboratory range. Men with chronic migraine had lower total testosterone levels compared to published agematched controls by a median difference of 62.0 ng/dL (interquartile range of 0.34 to 130). The Wilcoxon Signed rank statistic revealed a statistically significant difference between the two distributions (P=0.0494).
Discussion
In our pilot study, men with chronic migraine had statistically significant lower total testosterone levels compared to an age-matched normative population, suggesting that hypothalamic regulation is altered in patients with chronic migraine. We propose that the suppression of the hypothalamic pituitary axis as a result of chronic migraine inhibits the release of GnRH resulting in secondary hypogonadism. A host of studies have investigated the pathophysiology of the hypothalamus in both cluster headache10 and chronic migraine,1,5-7,11 however, a paucity of studies have explored the interaction between testosterone levels and chronic migraine, tension type headache (TTH), and cluster headache.12,13 It has been suggested that both male and female sex hormones could influence the course of primary headaches, specifically, tension-type headache, migraine, and cluster headache.14 Romiti and colleagues studied plasma testosterone levels in cluster headache and non-cluster headache controls.13 Plasma testosterone levels were significantly lower during the cluster attack and were within the reference limits in the remission period of episodic cluster headache.13 These authors suggest that a decrease of plasma testosterone levels in episodic cluster headache should be considered in relation to disordered rapid eye movement (REM) sleep in cluster headache.
The present study and that of Romiti et al. highlighted testosterone levels in migraine and cluster headache, respectively.13 Both studies reported that testosterone levels were significantly lower in the headache disorder group compared to controls. We demonstrated that men with chronic migraine had lower total testosterone levels compared to their agematched control by a median difference of 62 ng/dL (interquartile range of 0.34 to 130). In addition, there was a statistically significant difference between the two distributions (P=0.0494). Six males (43%) had testosterone levels below the minimum of the normal local laboratory range. Of note, the mean total testosterone level in our 14 patients with chronic migraine was 322 ng/dL which is in the lower 5% of the reference range for our laboratory (300-1080 ng/dL). This finding supports that testosterone levels are very low in migraine patients. Abnormality of the hypothalamuspituitary- gonadal axis is believed to be involved in the pathogenesis of migraine.15 In Li and colleagues’ study of the levels of HPG axis hormones serum FSH, LH, estradiol, progesterone, testosterone, prolactin, and GnRH, they reported that these hormones were abnormal in migraineurs and were associated with migraine-related clinical characteristics.15
Hypogonadism refers to “a clinical syndrome that results from failure of the testis to produce physiological levels of testosterone (androgen deficiency) and a normal number of spermatozoa due to disruption of one or more levels of the hypothalamicpituitary- testicular axis”.16 Hypogonadal symptoms include diminished libido, fatigue, poor concentration, erectile dysfunction, and depressed mood in the setting of low serum testosterone levels.17 Many men with chronic migraine exhibit symptoms that are frequently seen with hypogonadism, specifically, depressed mood, reduced energy, and difficulty concentrating. Testosterone supplementation has been shown to be beneficial in improving both hypogonadal symptoms and serum total testosterone levels.16,17 Testosterone therapy in hypogonadal men has been shown to be highly effective and safe for improving lower urinary tract symtpoms, cardiometabolic risk, and major adverse cardiovascular events18 as well as urinary and sexual function and quality of life.19 Testosterone serves as a neuroprotective agent,20 suggesting a valuable role in the treatment of chronic migraine. Continuous testosterone has also been reported as beneficial in reducing the severity of migraines in both pre- and post-menopausal women.21 These studies demonstrate that testosterone effectively treats migraine headaches in both men and women and that low testosterone is likely causal and not the result of migraines.
The strength of the present study is the prospective evaluation of the possible role of testosterone in migraine headaches as it is far less studied than estrogen/progesterone. Our study is limited by its small sample size. Prospective, randomized studies with a larger sample size are warranted to permit generalizability of our results.
Conclusions
In this pilot study, men with chronic migraine had statistically significant lower total testosterone levels compared to an age-matched normative population. Further investigation is necessary to determine whether testosterone supplementation in men with chronic migraine reduces either the number of headache days per month or the accompanying symptoms of hypogonadism.
Acknowledgements
The authors acknowledge Norton Healthcare for their continued support. They also acknowledge Douglas John Lorenz, Ph.D., Andrew J. Shearer, B.S., and Lauren A. Shelton, for their contributions to this work (data management and data checks for quality).
Funding Statement
Funding: none.
References
- 1.Burstein R, Noseda R, Borsook D. Migraine: multiple processes, complex pathophysiology. J Neurosci 2015; 35:6619-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Headache Classification Committee of the International Headache Society (IHS). The International Classification of headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33:629-808. [DOI] [PubMed] [Google Scholar]
- 3.Burch RC, Loder S, Loder E, et al. The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies. Headache 2015;55:21-34. [DOI] [PubMed] [Google Scholar]
- 4.Steiner TJ, Stovner LJ, Vos T. GBD 2015: migraine is the third cause of disability in under 50s. J Headache Pain 2016;17:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alstadhaug KB. Migraine and the hypothalamus. Cephalalgia 2009;29:809-17. [DOI] [PubMed] [Google Scholar]
- 6.Denuelle M, Fabre N, Payoux P, et al. Hypothalamic activation in spontaneous migraine attacks. Headache 2007;47:1418-26. [DOI] [PubMed] [Google Scholar]
- 7.Cortelli P, Pierangeli G. Hypothalamus and headaches. Neurol Sci 2007;28: S198-202. [DOI] [PubMed] [Google Scholar]
- 8.Handa RJ, Weiser MJ. Gonadal steroid hormones and the hypothalamo-pituitary- adrenal axis. Front Neuroendocrinol 2014;35:197-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelsey TW, Li LQ, Mitchell RT, et al. A validated age-related normative model for male total testosterone shows increasing variance but no decline after age 40 years. PLoS One 2014;9: e109346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leone M, Bussone G. A review of hormonal findings in cluster headache. Evidence for hypothalamic involvement. Cephalalgia 1993;13:309-17. [DOI] [PubMed] [Google Scholar]
- 11.Peres MF, Sanchez del RM, Seabra ML, et al. Hypothalamic involvement in chronic migraine. J Neurol Neurosurg Psychiatry 2001;71:747-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aksoy D, Solmaz V, Cevik B, et al. The evaluation of sexual dysfunction in male patients with migraine and tension type headache. J Headache Pain 2013; 14:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romiti A, Martelletti P, Gallo MF, et al. Low plasma testosterone levels in cluster headache. Cephalalgia 1983;3:41-4. [DOI] [PubMed] [Google Scholar]
- 14.Delaruelle Z, Ivanova TA, Khan S, et al. Male and female sex hormones in primary headaches. J Headache Pain 2018; 19:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li W, Diao X, Chen C, et al. Changes in hormones of the hypothalamic-pituitary- gonadal axis in migraine patients. J Clin Neurosci 2018;50:165-71. [DOI] [PubMed] [Google Scholar]
- 16.Spitzer M, Huang G, Basaria S, et al. Risks and benefits of testosterone therapy in older men. Nat Rev Endocrinol 2013;9:414-24. [DOI] [PubMed] [Google Scholar]
- 17.Ramasamy R, Wilken N, Scovell JM, et al. Effect of testosterone supplementation on symptoms in men with hypogonadism. Eur Urol 2015;67:176-7. [DOI] [PubMed] [Google Scholar]
- 18.Saad F, Doros G, Haider KS, et al. Hypogonadal men with moderate-tosevere lower urinary tract symptoms have a more severe cardiometabolic risk profile and benefit more from testosterone therapy than men with mild lower urinary tract symptoms. Investig Clin Urol 2018;59:399-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haider KS, Haider A, Doros G, et al. Long-term testosterone therapy improves urinary and sexual function, and quality of life in men with hypogonadism: results from a propensity matched subgroup of a controlled registry study. J Urol 2018;199:257-65. [DOI] [PubMed] [Google Scholar]
- 20.Fargo KN, Foster AM, Sengelaub DR. Neuroprotective effect of testosterone treatment on motoneuron recruitment following the death of nearby motoneurons. Dev Neurobiol 2009;69:825-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glaser R, Dimitrakakis C, Trimble N, et al. Testosterone pellet implants and migraine headaches: a pilot study. Maturitas 2012;71:385-8. [DOI] [PubMed] [Google Scholar]


