Abstract
In older persons, the origin of malnutrition is often multifactorial with a multitude of factors involved. Presently, a common understanding about potential causes and their mode of action is lacking, and a consensus on the theoretical framework on the etiology of malnutrition does not exist. Within the European Knowledge Hub “Malnutrition in the Elderly (MaNuEL),” a model of “Determinants of Malnutrition in Aged Persons” (DoMAP) was developed in a multistage consensus process with live meetings and written feedback (modified Delphi process) by a multiprofessional group of 33 experts in geriatric nutrition. DoMAP consists of three triangle-shaped levels with malnutrition in the center, surrounded by the three principal conditions through which malnutrition develops in the innermost level: low intake, high requirements, and impaired nutrient bioavailability. The middle level consists of factors directly causing one of these conditions, and the outermost level contains factors indirectly causing one of the three conditions through the direct factors. The DoMAP model may contribute to a common understanding about the multitude of factors involved in the etiology of malnutrition, and about potential causative mechanisms. It may serve as basis for future research and may also be helpful in clinical routine to identify persons at increased risk of malnutrition.
Keywords: older persons, malnutrition, determinants, etiology, model
Introduction
Protein-energy malnutrition is widespread among older persons and closely related to poor outcome and increased health care costs (Agarwal, Miller, Yaxley, & Isenring, 2013; Martínez-Reig et al., 2018; Morley, 2012; Soenen & Chapman, 2013). Prevention and treatment are thus important public health concerns.
An essential prerequisite for effective interventions to prevent and treat malnutrition is a thorough understanding of its etiology. Many factors are acknowledged as potential causes or so-called determinants of malnutrition and there is no doubt about the multifactorial origin of malnutrition. However, its etiology is complex and presently only partly understood.
In a recent systematic review about determinants of protein-energy malnutrition in community-dwelling older adults, in 28 included studies, 122 potential determinants were identified and categorized into nine domains—demographic, financial, food and appetite, lifestyle, psychological, physical functioning, disease and care, oral, and social domain (van der Pols-Vijlbrief, Wijnhoven, Schaap, Terwee, & Visser, 2014). Another current systematic review focused on 30 potentially modifiable determinants from seven domains examined in 23 prospective studies (O’Keeffe et al., 2019).
Narrative reviews about malnutrition also list and categorize potential causes (Agarwal et al., 2013; Amarya, Singh, & Sabharwal, 2015; Bell, Lee, & Tamura, 2015), and mnemonics like “Meals on Wheels” (Morley & Silver, 1995) and the nine “D’s” (dementia, dysgeusia, dysphagia, diarrhea, depression, disease, poor dentition, dysfunction, and drugs; Agarwal et al., 2013) have been developed to stimulate identification of malnutrition risk factors in clinical practice.
Several models have been developed to summarize and illustrate nutritional determinants in older persons, but their focus is on dietary intake and not on malnutrition, which may be caused by additional factors besides low intake. For example, the DONE model about Determinants Of Nutrition and Eating, recently generated within the JPI Knowledge Hub DEDIPAC, categorized more than 400 potential determinants into individual, interpersonal, environmental, and political factors for several age groups across the lifespan including older persons (Stok et al., 2017, 2019). Keller et al. (2014) developed a model of factors affecting food intake in institutionalized older persons covering meal- and resident-related, institutional, and governmental factors.
Besides knowing relevant determinants and determinant domains, the pathways and mechanisms through which these factors provoke malnutrition are of interest and importance with respect to identifying high-risk persons and subsequent adequate interventions.
At present, a common understanding about potential causes and their mode of action is weak, and theoretical framework on the etiology of protein-energy malnutrition in older persons does not exist. Thus, we aimed to create such a framework reflecting the multitude of factors involved as well as potential causative mechanisms.
Method
This research project was undertaken as part of the European Knowledge Hub “Malnutrition in the Elderly (MaNuEL),” which aimed to tackle the problem of malnutrition in the older population by targeted cooperation of 22 research groups from seven countries (Visser et al., 2017).
During a two-day live-meeting in April 2018 in Biedenkopf/Germany, determinants of malnutrition, their interrelations, and the mechanisms underlying the development of malnutrition were discussed by eight MaNuEL partners (involved in the MaNuEL work-package about determinants of protein-energy malnutrition) and eight external experts in the field of geriatric nutrition. All MaNuEL partners qualified in national competitions for participation in the MaNuEL Knowledge Hub. External experts were a convenience sample of renowned international experts with relevant scientific and/or clinical experience and complementary professional background, selected by the first and last authors of this article (D.V., R.W., M.V.). Based on presentations summarizing the current knowledge about various determinant domains, recent research results, and existing models in the field of nutrition (Agarwal et al., 2013; Keller et al., 2014; Stok et al., 2017, 2019; Volkert, 2004) and also based on the theoretical background knowledge of all participating experts, a first draft of the model was created and discussed in familiar and relaxed work atmosphere ensuring equal exchange.
This first draft encompassed the general triangle shape and three-level structure of the model with several determinants as examples of the principle that fundamental mechanisms causing malnutrition, that is, low intake, reduced nutrient bioavailability, and high requirements (Sobotka et al., 2004) need to be distinguished from factors affecting these mechanisms either directly or indirectly.
Using a list of determinants, which was based on a recent systematic review (van der Pols-Vijlbrief et al., 2014), and complemented by additional factors derived from an updated systematic literature search (O’Keeffe et al., 2019) or proposed by the group members (Supplementary Table S1), the first model draft was elaborated and extended (second draft), and then discussed with all attending MaNuEL partners (n = 26) at the final project meeting in June 2018 in Amsterdam. General agreement (>80%) by open vote was achieved about the model structure, and feedback regarding the selection and position of determinants across levels was obtained.
Subsequently, using a slightly modified model version based on discussions of the live meeting (third draft), written feedback by e-mail on which determinants to include at which level was gathered in two rounds among all MaNuEL partners and experts participating in the initial meeting, in total 57 persons (Delphi process; Boulkedid, Abdoul, Loustau, Sibony, & Alberti, 2011; Diamond et al., 2014; Jones & Hunter, 1995). For the first Delphi round, a list of 58 variables from seven domains (sociodemographic, lifestyle, mental function, physical function, oral function, health status, and nutrition) was sent out by the first author on July 17, 2018. Participants were asked to respond within 4 weeks and indicate behind each variable, if the variable should be included in the model or not and, if yes, at which level (outer or middle). Participants could place comments regarding each variable in an additional column. A total of 26 persons participated and sent their feedback: 16 nutrition scientists, four geriatricians, two dietitians, one gastroenterologist, one epidemiologist, one clinical pharmacist, and one psychologist. All except one nutrition scientist were involved in research at that time.
Responses were directly aggregated in a joint summary form in completely anonymized manner and evaluated by the first author. In the second Delphi round, 23 variables, either with poor agreement, defined as agreement <80% as proposed by Lynn (1986) to achieve valid results in consensus development, suggested to be modified or newly suggested in the first Delphi round, were sent to the same 57 experts addressed before for another evaluation on November 27, 2018, with again 4 weeks for reply. A total of 20 persons gave feedback (all participating also in the first round). Feedback was again compiled in anonymized form, and then evaluated and critically discussed by the authors (D.V., E.K., M.V.). The model was finalized accordingly.
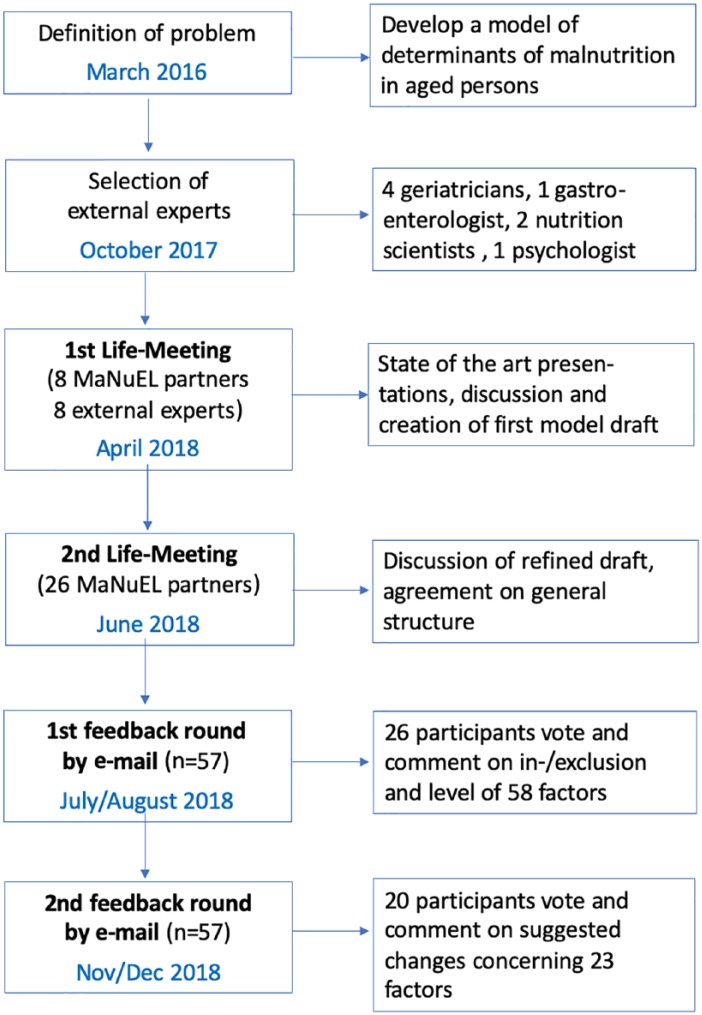
The whole development process is summarized in Figure 1.
Figure 1.
Development process of the DoMAP model on Determinants of Malnutrition in Aged Persons.
Note. MaNuEL = Malnutrition in the Elderly Knowledge Hub (Visser et al., 2017).
As only engaged experts were involved in this multistage consensus process on an entirely voluntary basis, ethical approval was deemed unnecessary.
Results
DoMAP Model
A theoretical framework of Determinants of Malnutrition in Aged Persons (DoMAP model) was developed and agreed by consensus, which is presented in Figure 2.
Figure 2.
DoMAP model.
All factors—independent of the level—are regarded as (potential) “determinants” of MN meaning that they may contribute to the development of MN in a causative manner. The levels illustrate different modes of action: Level 1 (dark green): Central etiologic mechanisms; Level 2 (light green): Factors in this level directly lead to one of the three mechanisms in Level 1 (e.g., swallowing problems may directly cause low intake); Level 3 (yellow): Factors in this level may indirectly lead to one (or more) of the three central mechanisms through one (or more) of the direct factors in the light green triangle (e.g., stroke may cause low intake via dysphagia or difficulties with eating); surrounding factors in red are age-related changes and general aspects which also contribute to the development of MN, but act even more indirectly or subtle. DoMAP = Determinants of Malnutrition in Aged Persons; MN = malnutrition.
Three DoMAP levels around malnutrition in the center were defined, which illustrate different modes of action in the development of malnutrition. The innermost level, surrounding malnutrition, consists of the three central mechanisms leading to malnutrition: low intake, high requirements, and impaired bioavailability of energy and nutrients (Level 1, dark green). The middle level (Level 2, light green) consists of factors which may directly lead to one (or more) of these central mechanisms, for example, swallowing problems may directly cause low intake, or diarrhea may directly impair bioavailability. The outermost level (Level 3, yellow) contains factors that may indirectly lead to one (or more) of the three central mechanisms through one (or more) of the direct factors in the light green triangle, for example, stroke may cause low intake, however not directly but via one or more factors in Level 2, for example, via dysphagia or difficulties with eating, or gastrointestinal disease may lead to impaired bioavailability through diarrhea.
A triangle form was preferred over a circle to reflect the three fundamental mechanisms in the innermost level and to stimulate alertness for clinical practice as a triangle also stands for “attention” due to its similarity with traffic signs.
The surrounding factors in red are considered general background variables and age-related changes that may generally contribute to a person’s risk of malnutrition, but act even more indirectly or subtle and are less or not at all modifiable through interventions.
Delphi Process
Forty-eight (83%) of the 58 variables put up for discussion in the first Delphi round received more than 80% agreement to be included in the model, 32 variables (55%) more than 90%. Four variables with poor agreement (<80%: poor self-rated health, burns, severe cough, loss of interest in life) were suggested to be removed from the model for the second Delphi round and the other six (female sex, smoking, low physical performance, increased breathing work, inflamm-aging, polypharmacy) were retained despite agreement below 80% because of strong arguments and repeatedly put up for discussion with additional explanations. Based on suggestions of participants, the naming of five factors was modified (inflammatory disease, taste/smell impairment, vision impairment, poor oral care, and oral health problems), and six variables were added (age-related functional decline, poor quality of care, delirium, tremor, lack of food, and not allowed to eat). Low education was moved from the outermost level to the surrounding space, and poverty from the middle to the outermost level. Furthermore, general explanations for the four levels were added to facilitate the understanding of the model (see Figure 2).
All modifications mentioned above were sent out for approval in the second Delphi round. In this ballot about suggested changes, four of the responding 20 persons completely agreed to all suggested changes. Nine (39%) of the 23 variables received less than 80% agreement. Of these, female sex, smoking, and inflamm-aging repeatedly received low agreement (40%, 55%, and 65%) and were therefore directly removed. After further discussions between the first, second, and last author, it was decided to remove also the other variables with less than 80% agreement: “increased breathing work” and “low physical performance” (both 70% agreement), and “delirium” and “not allowed to eat” (both 75% agreement). “Congestive heart failure” (65% agreement) was changed back to “inflammatory disease” which had received more approval (85% agreement in first Delphi round) and was judged to be more comprehensive. “Loss of interest in life” was retained in the model as the suggestion to remove it received only 75% agreement. All modifications resulting from the feedback rounds are documented in Supplementary Table S1. Finally, 18 direct factors (in the middle level) and 27 indirect factors (in the outermost level) were included in the model (Figure 2).
Discussion
The DoMAP model was developed to illustrate the multitude of potential causes and the mechanisms underlying the development of malnutrition. It highlights not only the great number and diversity of factors involved but also their relation to malnutrition and potential modes of action. The tip of the model does not indicate a specific hierarchy and should not be misunderstood as such. Factors in the upper part (about the top two thirds of the model) relate to low intake, they account by far for the largest share. Factors in the lower left and right area relate to reduced bioavailability and high requirements respectively and are less numerous. A few, more general, mostly age-related aspects in the surrounding background were added, despite the fact that they are hardly modifiable as they illustrate the broader context and, according to the experts’ view, should also be kept in mind regarding an older person’s risk of malnutrition.
The model consists of several levels to illustrate different modes of action of different factors. Currently, all factors—independent of the level—are regarded as potential “determinants” of malnutrition, meaning that they may contribute to the development of malnutrition in a causative manner, as fundamental mechanism, directly or indirectly. In our model, factors in Level 2 are suggested to be direct causes assuming that these factors will always lead to malnutrition if they persist and no countermeasures are taken, for example, chewing problems will lead to low intake and consequently malnutrition unless an intervention, for example, oral care or modification of food texture, is conducted. Thus, Level 2 factors are assumed as having superior importance, and health professionals should always be particularly alert and should immediately take action when one of these factors is present. Factors from Level 3 do not necessarily lead to malnutrition but may cause one or more factors in Level 2 and thus trigger indirectly one or more of the three central mechanisms in the first triangle. Similarly, surrounding background variables may act indirectly via one or more factors in Level 3 and/or Level 2.
The position of a variable in a specific level is not always unambiguous and was also discussed in the live meetings and Delphi rounds, as variables may be interrelated and different pathways to malnutrition are plausible, for example, a specific medication may cause dry mouth—both variables are in Level 3—leading to chewing and swallowing problems (Level 2). Tremor was placed in Level 2 as it is a consequence of Parkinson’s disease, but it could also be placed in Level 3 as it may cause difficulties eating.
Furthermore, the classification of factors according to their mode of action and the need of arrows to indicate specific pathways was thoroughly debated. Finally, it was decided to omit such a classification and also arrows for reasons of clarity and simplicity, as an indirect factor (outermost level) may impact malnutrition through several direct factors (middle level). Also, interrelations between factors are assumed, which may presumably not be completely covered.
Regarding selection and number of determinants, a comprehensive but at the same time lucid approach was followed with a main focus on personal factors, which were thought to be most relevant. Only two environmental factors were included—“poor quality of care” and “poor quality of meals”—as they are closely related to a person’s nutrition and were considered important by the experts. The selection of variables out of more than 150 potential determinants derived from literature (van der Pols-Vijlbrief et al., 2014; O’Keeffee et al., 2019; Streicher et al., 2018) and from additional brainstorming of the experts was challenging. It is mainly based on the opinion of the participating experts, who have not always been in agreement, and may be subject of further discussions. For example, we finally included seven specific diseases—gastrointestinal, cancer, Parkinson’s, stroke, depression, dementia, and COPD—as these are common diseases in older persons which typically show symptoms that may strongly affect intake, bioavailability, or requirements, and thus regarded as crucial in the development of malnutrition. Instead of these specific diseases, the more general terms “diseases,” “acute disease,” and “chronic disease” were discussed, which would however not reflect these specific mechanisms and possibly prevent specific attention for patients with these particular diseases. The term multimorbidity as a typical geriatric phenomenon was added in the background to reflect more general and indirect effects of the simultaneous presence of several chronic and/or acute diseases on appetite, intake, and requirements. Similarly, “medication” in Level 3 is thought to reflect specific drugs causing one of the specific problems in Level 2 (e.g., nausea, vomiting, malabsorption, or poor appetite) as specific side-effect, whereas “polypharmacy” in the background may exert more general impact of taking a number of different drugs with increased risk of potential negative effects on appetite, food intake, and nutrient bioavailability.
The threshold value of 80% agreement used for repeated voting and final removal of a variable from the model might also be subject of discussion, is however suggested to achieve valid results in consensus development (Lynn, 1986) and also used by others (Eubank et al., 2016; Murphy et al., 1998), while many other studies use less strict thresholds (Diamond et al., 2014). All variables finally removed because of agreement below this level were regarded to be indirectly included somehow in other terms, for example, the metabolic impact of increased breathing work in patients with chronic obstructive pulmonary disease (COPD) is covered by “increased metabolic rate” and “not allowed to eat” by “lack of food.”
In summary, there is no claim for completeness or objectivity, as by far not all factors discussed in the literature could be considered for reasons of clarity, and opinions about in- or exclusion may differ. The model is based on scientific knowledge and clinical experience of a multiprofessional, international group of renowned experts in the field of geriatric nutrition who contributed to its development. It is not evidence-based—as originally intended—as it quickly turned out that scientific evidence about determinants of malnutrition is overall limited and conflicting, and is often based on cross-sectional studies where reverse causation bias is present. Only a limited number of longitudinal studies is available (Fávaro-Moreira et al., 2016; O’Keeffe et al., 2019; van der Pols-Vijlbrief et al., 2014), varying and limited sets of determinants are examined, many determinants are not very well studied, and confounding is not sufficiently taken into account (Fávaro-Moreira et al., 2016; O’Keeffe et al., 2019; van der Pols-Vijlbrief et al., 2014). Furthermore, different definitions and assessment tools of both, determinants as well as malnutrition, and different statistical approaches are used (Fávaro-Moreira et al., 2016; O’Keeffe et al., 2019; Tamura, Bell, Masaki, & Amella, 2013; van der Pols-Vijlbrief et al., 2014). Thus, the model is primarily theory-based, and related scientific evidence needs comprehensive separate elaboration in a next step. To further develop DoMAP into an evidence-based model, longitudinal studies are needed to identify potential determinants of incident malnutrition to exclude reverse causation. The causality of the association between these determinants and incident malnutrition would need to be subsequently confirmed in intervention studies by studying whether elimination or treatment of the determinant in older persons would indeed lower the risk of developing malnutrition.
It is a clear strength of DoMAP that it highlights the diversity of factors affecting malnutrition as well as potential causative mechanisms. It includes frequent and relevant problems which might respond to interventions—either elimination or compensation—and is thus suitable for clinical practice as well as for scientific purposes. It may be used by health care professionals to check and highlight (combinations of) potential causes of malnutrition in individual patients as basis for intervention.
Limitations of the model are that the many and potentially overlapping pathways are not visible and that interrelations between factors are not addressed. Some factors might be placed in different levels, and scientific evidence and strength of the associations are not reflected. Moreover, the model was developed by a limited group of experts, which may have facilitated consensus-finding on one hand and excluded opinions and ideas of colleagues who were not involved on the other hand.
The model is however intended as a starting point and base for further discussions and developments. It may be modified in the future based on further discussions with additional experts, according to emerging scientific evidence as well as experiences from practical use. Scientific evidence (type and strength of association), prevalence, or modifiability may be indicated in the future by different colors or symbols. The model may be adapted for different health care settings considering setting-specific risk factors, and generation of intervention concepts is conceivable based on the model. As realized for the DONE model (Stok et al., 2017, 2019), an interactive version might be generated in the future (e.g., electronic version, smartphone app) where specific aspects, relations, or mechanisms may be highlighted, for example, specific determinant domains, all factors causing low intake, or factors present in an individual patient. Thus, also more or less simplified or complex versions may be developed. Posting the model on the Internet in an interactive manner may facilitate future exchange and further development.
Conclusions and Implications
Within the scope of the European MaNuEL knowledge hub, the DoMAP model was developed and consented by an international, multiprofessional group of experts to illustrate potential causes of malnutrition and potential causative mechanisms. This model of determinants of malnutrition in aged persons may contribute to a common understanding about the multitude of factors and different pathways involved in the etiology of malnutrition. It may serve as an important basis for future research, for example, to substantiate the assumed relevance of the factors considered or to develop preventive strategies for malnutrition in older persons. After further validation, it may also be helpful in clinical routine to check potential causes of malnutrition in individual patients and identify persons at increased risk of malnutrition and may serve as basis for appropriate interventions.
Supplemental Material
Supplemental material, DoMAP_Revision_SupplTableS1 for Development of a Model on Determinants of Malnutrition in Aged Persons: A MaNuEL Project by Dorothee Volkert, Eva Kiesswetter, Tommy Cederholm, Lorenzo M. Donini, Doris Eglseer, Kristina Norman, Stéphane M. M. Schneider, Nanette Ströbele-Benschop, Gabriel Torbahn, Rainer Wirth and Marjolein Visser in Gerontology and Geriatric Medicine
Acknowledgments
The authors are grateful to the following experts who contributed to the development of the model in addition to the authors (in alphabetical order): Anne Marie Beck, Clare Corish, Andrea Correa-Perez, Dominique Dardevet, Marion Flechtner-Mors, Corinna Geisler, Lisette de Groot, Mary Hickson, Sylvie Issanchou, Gabriele Nagel, Eiblhìs O’Connor, Maryam Pourhassan, Tamara Ranzenberger-Haider, Ilse Reinders, Yves Rolland, Melanie Streicher, Claire Sulmont-Rossé, Ruth Teh, and Virginie van Wymelbeke.
Footnotes
Authors’ Note: The DoMAP Model and parts of this article have been presented orally at the 40th ESPEN Congress on Clinical Nutrition and Metabolism, Madrid, Spain, September 1, 2018, in a pre-congress symposium about MaNuEL project results. A preliminary version of the model was visualized in a brochure with limited edition summarizing MaNuEL project results (“MaNuEL Toolbox”) which was sent to the project partners and funding organizations and distributed at the 14th EuGMS Congress October 10/12, 2018, in Berlin.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was initiated by the Joint Programming Initiative “A Healthy Diet for a Healthy Life” and performed within the MaNuEL (Malnutrition in the Elderly) Knowledge Hub. The funding agencies are (in alphabetical order of participating Member State) Austria: Federal Ministry of Science, Research and Economy (BMWFW; Grant No. BMWFW-10.420/0003-WF/V/3C/2016); France: Ecole Supérieure d’Agricultures (ESA) and Institut National de la Recherche Agronomique (INRA); Germany: Federal Ministry of Food and Agriculture (BMEL) represented by Federal Office for Agriculture and Food (BLE; Grant No. 2815ERA10E); Ireland: Department of Agriculture, Food and the Marine (DAFM), and the Health Research Board (HRB; Grant No. 15HDHL2); Spain: Instituto de Salud Carlos III, and the SENATOR trial (Grant No. FP7-HEALTH-2012-305930); The Netherlands: The Netherlands Organization for Health Research and Development (ZonMw; Grant No. 529051008). This work was further supported by the BANSS foundation who enabled a two-day live meeting of the experts without any obligation. The funders were not involved in the development of the model at any time.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD: Dorothee Volkert  https://orcid.org/0000-0002-1003-6395
https://orcid.org/0000-0002-1003-6395
References
- Agarwal E., Miller M., Yaxley A., Isenring E. (2013). Malnutrition in the elderly: A narrative review. Maturitas, 76, 296-302. doi: 10.1016/j.maturitas.2013.07.013 [DOI] [PubMed] [Google Scholar]
- Amarya S., Singh K., Sabharwal M. (2015). Changes during aging and their association with malnutrition. Journal of Clinical Gerontology and Geriatrics, 6, 78-84. doi: 10.1016/j.jcgg.2015.05.003 [DOI] [Google Scholar]
- Bell C. L., Lee A. S., Tamura B. K. (2015). Malnutrition in the nursing home. Current Opinion in Clinical & Nutritional Metabolic Care, 18, 17-23. doi: 10.1097/MCO.0000000000000130 [DOI] [PubMed] [Google Scholar]
- Boulkedid R., Abdoul H., Loustau M., Sibony O., Alberti C. (2011). Using and reporting the Delphi method for selecting healthcare quality indicators: A systematic review. PLoS ONE, 6(6), e20476. doi: 10.1371/journal.pone.0020476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond I. R., Grant R. C., Feldman B. M., Pencharz P. B., Ling S. C., Moore A. M., Wales P. W. (2014). Defining consensus: A systematic review recommends methodologic criteria for reporting of Delphi studies. Journal of Clinical Epidemiology, 67, 401-409. doi: 10.1016/j.jclinepi.2013.12.002 [DOI] [PubMed] [Google Scholar]
- Eubank B. H., Mohtadi N. G., Lafave M. R., Wiley J. P., Bois A. J., Boorman R. S., Sheps D. M. (2016). Using the modified Delphi method to establish clinical consensus for the diagnosis and treatment of patients with rotator cuff pathology. BMC Medical Research Methodology, 16, Article 56. doi: 10.1186/s12874-016-0165-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fávaro-Moreira N. C., Krausch-Hofmann S., Matthys C., Vereecken C., Vanhauwaert E., Declercq A., . . . Duyck J. (2016). Risk factors for malnutrition in older adults: A systematic review of the literature based on longitudinal data. Advances in Nutrition, 7, 507-522. doi: 10.3945/an.115.011254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones J., Hunter D. (1995). Consensus methods for medical and health services research. British Medical Journal, 311, 376-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller H., Carrier N., Duizer L., Lengyel C., Slaughter S., Steele C. (2014). Making the most of mealtimes (M3): Grounding mealtime interventions with a conceptual model. Journal of the American Medical Directors Association, 15, 158-161. doi: 10.1016/j.jamda.2013.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynn M. R. (1986). Determination and quantification of content validity. Nursing Research, 35, 382-385. doi: 10.1097/00006199 [DOI] [PubMed] [Google Scholar]
- Martínez-Reig M., Aranda-Reneo I., Peña-Longobardo L. M., Oliva-Moreno J., Barcons-Vilardell N., Hoogendijk E. O., Abizanda P. (2018). Use of health resources and healthcare costs associated with nutritional risk: The FRADEA study. Clinical Nutrition, 37, 1299-1305. doi: 10.1016/j.clnu.2017.05.021 [DOI] [PubMed] [Google Scholar]
- Morley J. E. (2012). Undernutrition in older adults. Family Practitioner, 29(Suppl 1), i89-i93. [DOI] [PubMed] [Google Scholar]
- Morley J. E., Silver A. J. (1995). Nutritional issues in nursing home care. Annals of Internal Medicine, 123, 850-859. [DOI] [PubMed] [Google Scholar]
- Murphy M. K., Black N. A., Lamping D. L., McKee C. M., Sanderson C. F., Askham J., Marteau T. (1998). Consensus development methods, and their use in clinical guideline development. Health Technology Assessment, 2, 1-88. [PubMed] [Google Scholar]
- O’Keeffe M., Kelly M., O’Herlihy E., O’Toole P. W., Kearney P. M., Timmons S., . . . O’Connor E. M. (2019). Potentially modifiable determinants of malnutrition in older adults: A systematic review. Clinical Nutrition. Advance online publication. doi: 10.1016/j.clnu.2018.12.007 [DOI] [PubMed] [Google Scholar]
- Sobotka L., Allison S. P., Fürst P., Meier R. F., Pertkiewicz M., Soeters P. B. (Eds.). (2004). Basics in clinical nutrition. Prague, Czech Republic: Publishing House Galen. [Google Scholar]
- Soenen S., Chapman I. M. (2013). Body weight, anorexia, and undernutrition in older people. Journal of the American Medical Directors Association, 14, 642-648. doi: 10.1016/j.jamda.2013.02.004 [DOI] [PubMed] [Google Scholar]
- Stok F. M., Hoffmann S., Volkert D., Boeing H., Ensenauer R., Stelmach-Mardas M., . . . Renner B. (2017). The DONE framework: Creation, evaluation, and updating of an interdisciplinary, dynamic framework 2.0 of determinants of nutrition and eating. PLoS ONE, 12, e0171077. doi: 10.1371/journal.pone.0171077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stok M., Renner B., Hoffmann S., Volkert D., Boeing H., Ensenauser R., Holdsworth M. (2019). DONE determinants of nutrition and eating: A DEDIPAC knowledge hub output. Retrieved from https://www.uni-konstanz.de/DONE/
- Streicher M., van Zwienen-Pot J., Bardon L., Nagel G., Teh R., Meisinger C., . . . Volkert D. (2018). Determinants of incident malnutrition in community-dwelling older adults—A MaNuEL multi-cohort meta-analysis. Journal of the American Geriatric Society, 66, 2335-2343. doi: 10.1111/jgs.15553 [DOI] [PubMed] [Google Scholar]
- Tamura B. K., Bell C. L., Masaki K. H., Amella E. J. (2013). Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: A systematic review of the literature. Journal of the American Medical Directors Association, 14, 649-655. doi: 10.1016/j.jamda.2013.02.022 [DOI] [PubMed] [Google Scholar]
- van der Pols-Vijlbrief R., Wijnhoven H. A., Schaap L. A., Terwee C. B., Visser M. (2014). Determinants of protein-energy malnutrition in community-dwelling older adults: A systematic review of observational studies. Ageing Research Reviews, 18, 112-131. doi: 10.1016/j.arr.2014.09.001 [DOI] [PubMed] [Google Scholar]
- Visser M., Volkert D., Corish C., Geisler C., de Groot L. C., Cruz-Jentoft A. J., . . . de van der Schueren M. A. (2017). Tackling the increasing problem of malnutrition in older persons: The Malnutrition in the Elderly (MaNuEL) knowledge hub. Nutrition Bulletin, 42, 178-186. doi: 10.1111/nbu.12268 [DOI] [Google Scholar]
- Volkert D. (2004). DGEM and DGG guideline enteral nutrition: Nutritional status, energy and nutrient metabolism in older persons. Aktuelle Ernährungsmedizin, 29, 190-197. (In German) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DoMAP_Revision_SupplTableS1 for Development of a Model on Determinants of Malnutrition in Aged Persons: A MaNuEL Project by Dorothee Volkert, Eva Kiesswetter, Tommy Cederholm, Lorenzo M. Donini, Doris Eglseer, Kristina Norman, Stéphane M. M. Schneider, Nanette Ströbele-Benschop, Gabriel Torbahn, Rainer Wirth and Marjolein Visser in Gerontology and Geriatric Medicine