Abstract
Background:
Ankle sprain is the most common injury in basketball players. However, in our routine clinical evaluation, we observe a high frequency of muscle injury. Currently, no reliable information is available regarding the magnitude of these types of injury.
Purpose:
To describe the type and rate of muscle injuries in male basketball players and discuss clinical management and prevention strategies.
Study Design:
Descriptive epidemiology study.
Methods:
A total of 59 professional male basketball players were evaluated over 9 seasons (2007-2015). All injuries during the study period were registered through use of a validated electronic medical record system.
Results:
We analyzed 463 injuries, of which 207 resulted in time loss and 256 required medical attention, for a total exposure time of 42,678 hours for the 59 players involved in the study. Muscle strains and ankle sprains accounted for 21.2% (n = 98) and 11.9% (n = 55) of all injuries, respectively. The global incidence rate was 10.8 injuries per 1000 player-hours (95% CI, 9.9-11.9). The global injury burden was 53.9 days lost due to injuries per 1000 hours for a total exposure time. The incidence rate of muscle strains (2.3; 95% CI, 1.9-2.8) was higher than that of ankle sprains (1.3; 95% CI, 1-1.7). The incidence rate for muscle injuries for the entire study period was 1.8 times higher (95% CI, 1.28-2.49) than that for ankle sprains.
Conclusion:
In this study, muscle injuries were more commonly observed compared with ankle sprains. Prevention strategies for muscle injuries may be worth discussing.
Keywords: basketball, ankle sprain, muscle sprain, injury epidemiology, injury prevention
Basketball has one of the highest rates of injury of all team sports, with up to 10 injuries per 1000 hours of exposure.8 However, epidemiological studies in professional basketball are generally lacking, mainly because of methodological challenges in data collection. Although evidence is limited, 1 study indicated that a large proportion of basketball-related injuries consist of lower extremity injuries.7 More precisely, injuries in the lumbar region, ankle, knee, and patella account for more than 50% of all injuries in basketball, and among them, injuries to the ankle joint are the most common (11%-17%).3,9,22,25 Given these data, sports teams have established preventive measures to minimize the risk and frequency of ankle injury, including taping the ankle or using neuromuscular exercises.14,20 However, these evidence-based recommendations were developed by limited evidence from several investigations: One study9 was relatively old (published in 2010), and 2 studies involved nonprofessional basketball players.3,22 Those limitations raise 2 major concerns. First, the type and magnitude of musculoskeletal injuries are likely to be quite different between professional and nonprofessional basketball players. Second, the sport of basketball has changed significantly in the past few years. Players have become more physically demanding, and competitions are scheduled more frequently, which results in less time to recover between matches. Additionally, recent rule changes with regard to timetables force basketball players to play more games in tight schedules, which may affect the risk of musculoskeletal injuries in these players. This leads to 2 clinical questions: What type of musculoskeletal injuries do professional basketball players sustain? How frequently those injuries occur?
The objective of this study was to describe the type and rate of muscle injuries in male basketball players and discuss clinical management and prevention strategies. Specifically, this study had 3 aims: (1) to investigate the incidence rates (IRs) of musculoskeletal injuries (during both games and training) and trends in these IRs over time; (2) to evaluate the most problematic type of injuries (ie, those that result in lost playing time) in terms of injury burden (IB) and time to return to play (RTP); and (3) to provide clinical recommendations to manage musculoskeletal injuries in male professional basketball players.
Methods
Study Design and Participants
A descriptive epidemiological study design was used. This study was based on injury data collected as a part of a previous study.5 We performed a prospective cohort analysis in 59 male players from an elite Spanish basketball club (single center) competing at the highest level of national and European leagues between the 2007-2008 and 2015-2016 seasons. The 59 study participants played professional basketball in the club during 9 seasons (2007-2008 to 2015-2016). The number of players per season varied from 12 (2008-2009, 2009-2010, 2011-2012) to 15 (2012-2013, 2014-2015, 2015-2016). All participants were informed about the study’s purpose and procedures at the preparticipation evaluation during the preseason and provided their written informed consent to participate. The study was approved by the local research ethics committee.
Data Collection
Baseline medical information was recorded from all participants at the beginning of each season through use of a periodic health examination protocol. The health examination consisted of basic medical information (history), anthropometric data (age, height, weight, ethnicity), physical examination, spirometry, basal 12-lead electrocardiography (ECG), submaximal cardiovascular exercise testing (with ECG and blood pressure monitoring), and cardiac echocardiography. Once a season started, various parameters that are potentially related to type and frequency of musculoskeletal injuries (eg, mechanism of injury) were collected. The athletes’ exposure and other variables such as playing position were recorded. We also collected clinical information and data related to type of injury, time loss (TL), medical attention (MA), and RTP.
Definitions, Categories, and Calculation of Injury Incidence and Injury Burden
The metrics TL, MA, and RTP were obtained based on consensus definitions and data collection procedures suggested by the Union of European Football Associations (UEFA).11,13,15 Game exposure (GE) was defined as the number of hours of play in competitive games, based on actual minutes played, whereas training exposure (TE) referred to the numbers of hours of training on court as well as conditioning and injury prevention workouts. Based on the sum of the GE and TE, total athletic-exposure (TAE) was computed for the entire evaluation period. All exposure measures were rigorously recorded by a physical trainer, coach, and medical director in a consistent manner.
TL injuries included any injury that occurred during a training session or match and caused the player to be absent for at least the next training session or match. In contrast, MA injuries were those that did not result in time loss from training sessions and scheduled matches. The RTP was calculated as the recovery time (in days) from the day of the injury until the player safely returned to training or competition. Reinjury was defined as any injury of the same type at the same anatomic location as a previous injury in the same individual within 2 months of RTP.11,12 The injury IR was calculated as the total number of injuries (TL + MA) per 1000 hours of TAE (player-hours exposure). This was computed for all injuries as well as for each type of injury and each season. The incidence rate ratio (IRR) was calculated as the ratio of 2 IRs, and the delta method was used to compute the corresponding confidence interval. Moreover, the IB, a combined measure of the frequency (injury rate) and severity (days of absence) of injuries, was calculated as the number of days lost due to injury (ie, time to RTP) per 1000 hours of TAE.
Injury Classification and Management
Musculoskeletal injuries that were unrelated to basketball and absences resulting from illness were not included in this study. Injury types were classified by use of the Orchard Sports Injury Classification System (OSICS) version 10, which corresponds specifically to all muscle injuries (OSICS code M) and ankle sprain (code AJ).23 Medical team personnel recorded all injuries and entered them using validated electronic medical record software (Gem version 1.2; FCB). Injury diagnoses were made by the same chief medical physician (team doctor; G.R.) during the evaluation period, which eliminated the concern of interpersonal bias. For all cases of injury, the diagnosis was based on a detailed history, physical examination, and ultrasound/Doppler assessment; where necessary, magnetic resonance imaging (MRI) was also performed. A multistage rehabilitation program was carried out based on objective criteria and progression. For muscle injuries, we applied the guidelines of the rehabilitation program established in the club’s medical practice guide for muscle injuries.24,28 For other types of injury, such as ankle sprains, a standardized rehabilitation program was implemented based on the clinical practice experience of the medical staff. This approach, standardized rehabilitative care, reduces variability among health care practitioners and provides consistency; thus, the data are reliable and usable for analysis.
Statistical Analysis
We performed a descriptive study of some study variables. Main outcome variables included (1) participants’ demographics and injury settings, (2) injury types and injured body locations, (3) injury incidence, (4) injury distribution, and (5) IB. We computed absolute and relative frequencies for categorical variables and measures of central tendency and statistical dispersion for continuous variables.
To study the injury frequency among the basketball players, IRs were computed globally as well as per injury type, per season, and per player. For the computation of the 95% CIs, the Poisson distribution was used, which assumes that all injuries occur independently of each other. IRs were compared by means of the IRR. Moreover, we calculated the average time of RTP after an injury per season and injury type.
All analyses were performed with the R statistical package (The R Foundation for Statistical Computing), version 3.3.3. In particular, to compute the average IRs and corresponding CIs, we used the epitools package (https://cran.r-project.org/web/packages/epitools/index.html).
Results
Participants’ Demographics and Injury Settings
For the 59 study participants, the mean ± SD age, height, and weight at the beginning of the first season were 26.4 ± 4.4 years, 200.9 ± 9.1 cm, and 100.5 ± 13.5 kg, respectively. Of the sample, 44 players (74.6%) were white and 15 (25.4%) were black. Regarding player position, 22% (n = 13) were centers, 28.8% (n = 17) center-forwards, 17% (n = 10) forwards, 13.6% (n = 8) guards, and 18.6% (n = 11) point-guards. The team played a mean of 86 games and had a mean of 241 training sessions per season (August to June).
A total of 463 injuries were recorded during the study period: 37.8% (n = 175) occurred during games and 62.2% (n = 288) during training. All players experienced at least 1 injury per season. Regarding muscle injuries, 48.0% (n = 47) occurred during games and 52.0% during training (n = 51). In contrast, 63.6% (n = 35) of ankle sprains occurred during games and 36.4% (n = 20) during training. During games, ankle sprains were more common than muscle strains (63.6% and 48.0%, respectively).
Injury Types and Injured Body Locations
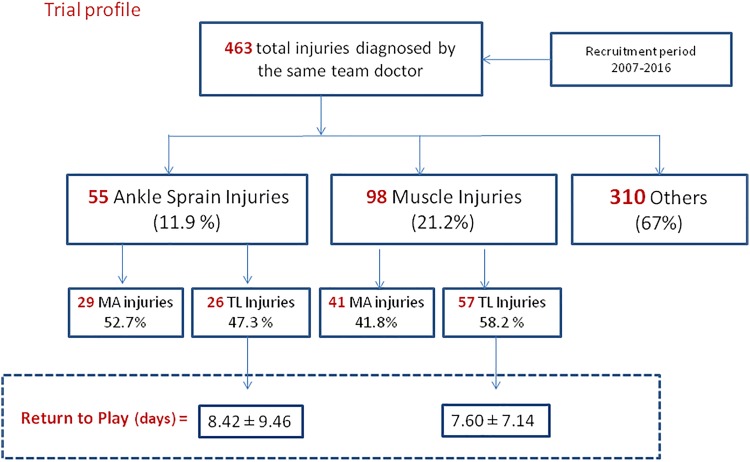
Figure 1 shows the different types of injuries and whether these required MA only or resulted in TL for play. Among the total number of injuries (N = 463), 98 (21.2%) and 55 (11.9%) were muscle strains and ankle sprains, respectively. The remaining injuries (67.0%) included tendinopathies and fasciitis (n = 97; 21.0%); foot ligament sprains (n = 54; 11.0%); lumbar spine and low back pain (n = 53; 11.0%); synovitis, meniscal, and cartilage injuries (n = 37; 8.0%); and fractures (n = 29; 6.0%). Among ankle sprain and muscle injuries, the proportions of TL injuries were 47.3% and 58.2%, respectively.
Figure 1.
Flowchart of global injury types, expressing the frequency of injuries recorded during 9 professional basketball seasons. MA, medical attention; TL, time loss.
Regarding localization of the muscle injuries, 89 (90.0%) affected the lower extremities. For MA injuries, the affected areas were the gastrocnemius-soleus (21.7%), quadriceps (20.4%), hamstrings (18.5%), adductor-groin (13.4%), and obliquus-abdominis (8.0%). For TL injuries, the affected areas were the hamstrings (28.5%), gastrocnemius-soleus (26.7%), adductor-groin (14.2%), obliquus-abdominis (12.5%), and quadriceps (8.9%).
Injury Incidence
The 59 athletes participating in the study had an overall exposure time to injury of 42,678 player-hours during the 9 seasons (2293 hours during games and 40,385 hours during training). The general injury IR during the 9 seasons (Table 1) was 10.8 injuries per 1000 player-hours (95% CI, 9.9-11.9). Muscle injuries (IR, 2.3 per 1000 player-hours; 95% CI, 1.9-2.8) were more common than ankle sprains (IR, 1.3; 95% CI, 1.0-1.7). In terms of impact on ability to play, injuries that only required MA were more common (6.0 per 1000 player-hours; 95% CI, 5.3-6.8) than those leading to TL (4.8 per 1000 player-hours; 95% CI, 4.2-5.6).
TABLE 1.
Rates of TL and MA Injuries and RTP for TL Injuries During the 9 Basketball Seasons Evaluateda
| Total Injuries | TL Injuries | MA Injuries | ||||||
|---|---|---|---|---|---|---|---|---|
| Injury Type | n (%) | ET, h | IR (95% CI) | n (%) | IR (95% CI) | RTP, mean ± SD, d | n (%) | IR (95% CI) |
| Ankle sprain | 55 (11.9) | 42,678 | 1.3 (1.0-1.7) | 26 (12.6) | 0.6 (0.4-0.9) | 8.4 ± 9.5 | 29 (11.33) | 0.7 (0.5-1.0) |
| Muscle strain | 98 (21.2) | 42,678 | 2.3 (1.9-2.8) | 57 (27.5) | 1.3 (1.0-1.7) | 7.6 ± 7.1 | 41 (16.02) | 1.0 (0.7-1.3) |
| Other | 310 (67.0) | 42,678 | 7.3 (6.5-8.1) | 124 (59.9) | 2.9 (2.4-3.5) | 13.2 ± 30.3 | 186 (72.66) | 4.4 (3.7-5.0) |
| Total | 463 (100) | 42,678 | 10.8 (9.9-11.9) | 207 (100) | 4.8 (4.2-5.6) | 11.1 ± 24.0 | 256 (100) | 6.0 (5.3-6.8) |
aET, exposure time; IR, incidence rate; MA, medical attention; RTP, return to play; TL, time loss.
As TL injuries are the most important in terms of an athlete’s ability to continue playing, we analyzed the differences in this category between the 2 most common anatomic lesions in this study, namely muscle and ankle injuries (Table 1). We found a similar pattern to that for total injuries, in that the IR for TL muscle injuries was higher (1.3 per 1000 player-hours; 95% CI, 1.0-1.7) than that for TL ankle ligament sprain injuries (0.6 per 1000 player-hours; 95% CI, 0.4-0.9). Regarding the severity of TL muscle injuries according to the UEFA consensus,15 32 injuries were minor (≤7 days TL), 24 injuries were moderate (8-28 days TL), and 1 injury was severe (>28 days TL) (a biceps femoris long head reinjury resulting in 40 days of TL). Regarding TL ankle sprain injuries, 15 were minor, 9 were moderate, and 2 were severe. The most common type of TL ankle injury was lateral ankle sprain (21/26), followed by syndesmosis (3/26) and deltoid ligament (2/26). The IRR for muscle strains for the entire study period was 1.8 (95% CI, 1.28-2.49), which indicates that players were 1.8 times more likely to have muscle strains than ankle sprains.
Injury Distribution
Analyzing injuries according to the type of activity (matches or training), we found that most injuries occurred during matches (76.4 per 1000 player-hours; 95% CI, 65.5-88.6) and considerably fewer during training (7.1 injuries per 1000 player-hours; 95% CI, 6.3-8.0). Consistent with the injury incidence results described above, muscle injuries were more common than ankle sprains in both games and training (Table 2).
TABLE 2.
Incidence Rate (IR) Analysis of Ankle, Muscle, Other, and Total Injuries During Games and Practicesa
| Ankle IR | Muscle IR | Other IR | Total IR | |
|---|---|---|---|---|
| Games | 15.3 (10.6-21.3) | 20.5 (15.1-27.3) | 40.6 (32.8-49.8) | 76.4 (65.5-88.6) |
| Practices | 0.5 (0.3-0.8) | 1.3 (0.9-1.7) | 5.4 (4.7-6.1) | 7.1 (6.3-8.0) |
aThe data consisted of a sum of 9 basketball seasons. Values in parentheses are 95% CIs.
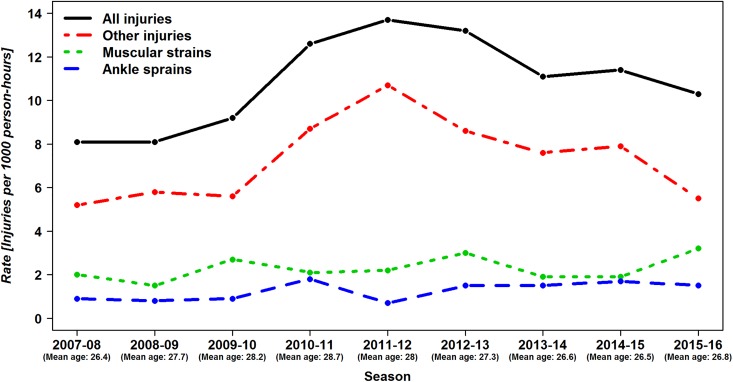
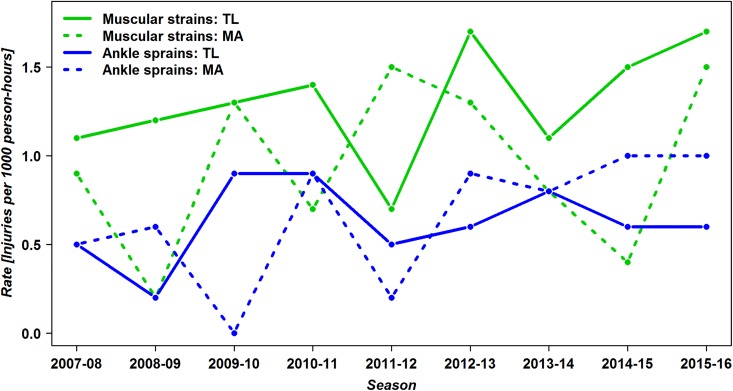
Analyzing trends in injury rate during the 2007-2015 period, we found that the IR of muscle strains was consistently higher than that of ankle sprains (Figure 2). Evaluating these trends according to injury severity, we found that the IR of muscle injuries leading to TL was consistently higher than that of ankle sprains within the same degree of severity (Figure 3). Moreover, the IR of injuries leading to TL (mainly muscle injuries) appeared to increase during the study period, although this trend was not statistically significant.
Figure 2.
Trends in incidence rates by season-year according to type of injury.
Figure 3.
Incidence rates of time loss (TL) and medical attention (MA) according to the 2 types of injuries evaluated (ankle sprains and muscle strains) by season-year.
Injury Burden and Time to Return to Play
The mean ± SD overall RTP time for TL injuries was 11.1 ± 24 days (Table 1). In terms of injury type, mean RTP time was 8.4 ± 9.5 days for ankle sprains and 7.6 ± 7.1 days for muscle injuries (Table 1). The overall IB of games and practices was 569.5 (95% CI, 355.2-783.8) and 24.4 (95% CI, 12.8-36.0) days lost due to injury per 1000 hours TAE (Table 3). The IB associated with muscle injuries was higher than that for ankle injuries, during both games and practices (Table 3).
TABLE 3.
Injury Burden (IB) of Ankle and Muscle Time Loss Injuries During Games and Practice for the 9 Basketball Seasons Evaluateda
| Ankle IB | Muscle IB | Other IB | Total IB | |
|---|---|---|---|---|
| Games | 89.1 (49.6-128.7) | 127.5 (86.6-168.4) | 352.9 (146.6-559.1) | 569.5 (355.2-783.8) |
| Practice | 0.4 (0.1-0.6) | 3.5 (2.4-4.6) | 20.5 (9.0-32.0) | 24.4 (12.8-36.0) |
| Total | 5.1 (2.9-7.3) | 10.2 (7.7-12.6) | 38.4 (22.9-53.8) | 53.9 (37.9-69.7) |
aData are reported as days lost due to injury per 1000 hours of total athletic-exposure. Values in parentheses are 95% CIs.
Discussion
In this 9-year prospective follow-up study, we observed an overall IR of 10.8 injuries per 1000 hours in a cohort of 59 male professional basketball players, which is consistent with values reported in previous studies.7,8 Ankle sprain is generally considered to be the most common injury type in basketball. For instance, Drakos et al9 reported that lateral ankle sprains were the most common injury among elite National Basketball Association players (13.2%) in the United States. Cumps et al7 reported that ankle sprains were the most commonly reported acute injuries in basketball (51.1%), although these results were based on data from just 1 season. Furthermore, Kofotolis and Kellis17 reported that ankle sprains were the most frequently reported TL injury among female professional basketball players in Greece. However, in the current study, we found that muscle injuries were more common than ankle sprains, accounting for 21.2% of all injuries, approximately double that of ankle sprains (11.9%; ∼1.8 times higher). This is a significant problem for basketball teams because muscle injuries are more difficult to manage than ankle injuries. Although even severe ankle injuries can be managed effectively so they do not cause TL for players, even minor muscle injuries can affect the player’s availability.
Why Are Injuries So Frequent in Basketball?
The competition schedule for European professional basketball is becoming more intense,12,16,27 and this has been linked to an increase in injury rates during competition at all levels.4,6 The high rate of injuries experienced by athletes appears to be directly related to the higher number of weekly games, the greater demand on sports performance, and the reduced recovery time available after injury.1,26 For example, busy schedules probably reduce players’ availability for specific conditioning training and provide insufficient time for recovery of overall well-being, both of which likely lead to increased physical fatigue and contribute to greater risk of injury.10 In fact, 1 study recommended providing adequate rest in order to reduce physical and mental fatigue and facilitate appropriate recovery.2 In the current study, the finding that IRs for muscle injuries are higher than for ankle injuries may stem from the tight match schedules. Specifically, muscle tissues might not have had enough time for proper recovery, which might have resulted in more muscle injuries.
Injury Incidence
In our study, the IR of muscle injury was much higher in games (20.5 per 1000 player-hours; 95% CI, 15.1-27.3) than during training (1.3 per 1000 player hours; 95% CI, 0.9-1.7) (Table 2), probably because game play imposes greater physical demands on athletes compared with training. Additionally, unexpected movements, formations, and circumstances are common in games compared with practice settings. Finally, substitutions of players are less frequent in games compared with practices. Collectively, those aspects likely contribute to higher muscle injury IR in games than in training. With regard to type of injuries, our results were consistent with the cohort study performed by Drakos et al,9 who also found a higher incidence of TL muscle injuries than TL ankle sprains. Interestingly, according to Drakos et al,9 the most prevalent basketball-related injuries were tendon injuries, and this is consistent with the current results. However, in the current study, we focused on the comparison between acute muscle and ankle injuries because tendon injuries are usually overuse injuries and do not significantly affect the player’s availability for games, especially TL. Basketball players frequently play with the presence of tendon pain and associated symptoms; however, they do not often miss games because of such overuse injuries. Whether these injuries hinder players’ physical function and basketball performance is unknown, and this could be an interesting area for future study.
In our study, players experienced 1.8 (IRR) times more muscle strains than ankle sprains, and the burden of muscle injuries was higher than that of ankle injuries (Table 3). This new trend was detected in this study as an increase in muscle injury rates for each season, as seen in Figure 3.
Another interesting finding observed in this study was the potential influence of age of athletes and competitive schedules of the European League. Notably, the rate for muscle and ankle injuries remained stable over the 9 seasons; however, the IR of injuries other than muscle and ankle injuries peaked during the 2010-2011 to 2012-2013 seasons (Figure 2), which coincides with an increase in the average age of the basketball players in this study. Additionally, an increase in the number of Euro League matches per season (data not shown) occurred in the same season. Those 2 aspects, increased player age and number of games during the 2010-2011 to 2012-2013 seasons, might have influenced the IRs of the other injuries.
Time to Return to Play
We did not observe any statistically significant differences between ankle and muscle injuries in terms of mean time to RTP (8.4 vs 7.6 days, respectively; see Table 1). Although our clinical practices are based on standardized, progressive rehabilitation processes, the RTP decision is complex and multifactorial. In our clinical setting, once clinical criteria are met (mainly through physical examination, ultrasonography, MRI, strength and field testing, and global positioning system outcomes), the final RTP decision is discussed and agreed upon among the player, coaching staff, and team physician. Occasionally, basketball players play with injury during a season. For instance, when players sustain a mild or moderate ankle sprain, they keep playing with the support of taping or bracing, local anti-inflammatory or anesthetic agents, and/or injections of corticosteroids or platelet-rich plasma. Although “playing with pain” is relatively well-established for ankle sprains, muscle injuries seem to have a greater influence on basketball function and overall performance, as reflected in the IB data (ankle IB vs muscle IB: 5.1 vs 10.2 days lost per 1000 hours TAE; Table 3) as opposed to the RTP results. In summary, although the RTP data did not show a significant difference between muscle and ankle injuries in RTP measures, our IRR analysis showed that ankle injuries are generally less debilitating than muscle injuries (Table 3).
Recommendations for Managing Muscle Injury in Professional Basketball Teams
Based on the findings of this study, we recommend implementing 3 basic components:
Educational Programs. Professional players have a lower frequency of ankle sprain than immature and developing players because professionals have more experience and better skill sets when performing basketball-specific movements. Conversely, among high school players, ankle sprain has been reported to be the most common injury, probably owing to a well-described collision mechanism with the opponent.19 An educational program based on transferring the experience and knowledge of high-level players to all levels of basketball athletes would help to minimize these types of injury.
Standardized Preventive Measures. Measures to minimize the risk of severe muscle injuries should be implemented, such as standardized neuromuscular protocols. For example, Longo et al18 evaluated a program of sports injury prevention for the lower extremities in male basketball teams based on the FIFA 11+ program. The investigators obtained limited improvements in terms of injury rate but encouraging results with regard to severity of injury. Additionally, a recent meta-analysis indicated that preventive programs in soccer could significantly reduce the incidence of lower extremity injuries in general and ankle sprains in particular.14 Thus, developing and implementing standardized prevention exercises tailored for basketball players may help reduce severe muscle injuries.
Standardized Rehabilitation Protocol. Development of a standardized evidence-based protocol for rehabilitation and physical therapy for basketball muscle injuries is a priority. This evidence-based program should take a multifactorial, individualized, and criteria-based approach with the support of expert consensus.21 For instance, substantial evidence exists regarding hamstring muscle injury, so the criteria for RTP following hamstring injuries should be discussed, synthesized, and standardized based on available evidence.
Limitations and Strengths
One of the limitations of this study was that there was a limited number of players from a single club team. A future study is warranted that includes a larger sample size and potentially performs the same type of investigation using a few more club teams in the European League, which will provide more power, consistency, and generalizability to the findings. When estimating injury incidences and corresponding 95% CIs, we did not distinguish between the initial injury per season and subsequent injuries within the same season. Instead of making an association between the 2 injuries (initial and subsequent injuries per player), we computed them as the overall injury IRs. Hence, injuries were assumed to be independent, implying exponentially distributed times until the occurrence of an injury. However, it is possible that, for example, a mechanism exists whereby initial injury potentially leads to subsequent injuries.
Some of the strengths of the current investigation are its duration and design; our findings were based on data from 9 consecutive seasons with a prospective study design. Another strength of this study is the consistency of record keeping and clinical practice over the study duration. The systematic approach of the standardized, progressive rehabilitation protocol was maintained during the entire study period, and the RTP time was rigorously recorded across all clinical staff members, even after the end of the season, to ensure accuracy of the data.
Conclusion
Our 9 seasons of prospective follow-up data of a group of male professional basketball players indicated that muscle injuries have higher incidence than ankle sprains, in terms of both MA and TL. The incidence of TL muscle injuries was almost twice that of ankle sprains. However, we found no marked difference in the time to RTP between muscle injuries and ankle injuries.
Considering the increasingly intense schedule of professional basketball competitions in Europe, it seems quite likely that muscle injuries are becoming more prevalent and may cause significant burdens in professional basketball players. This must be taken into account in the design of prevention programs for both preseason and in-season play. Such programs can help basketball players maintain long-lasting, competitive athletic careers.
Acknowledgment
The authors gratefully acknowledge the players involved in this study.
Footnotes
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Ethics Committee for Clinical Research of the Catalan Sports Council (Consell Català de l’Esport, Barcelona, Generalitat de Catalunya No. 162015CEICGC).
References
- 1. Bengtsson H, Ekstrand J, Walden M, Hagglund M. Muscle injury rate in professional football is higher in matches played within 5 days since the previous match: a 14-year prospective study with more than 130 000 match observations. Br J Sports Med. 2018;52(17):1116–1122. [DOI] [PubMed] [Google Scholar]
- 2. Blanch P, Gabbett TJ. Has the athlete trained enough to return to play safely? The acute:chronic workload ratio permits clinicians to quantify a player’s risk of subsequent injury. Br J Sports Med. 2016;50(8):471–475. [DOI] [PubMed] [Google Scholar]
- 3. Borowski LA, Yard EE, Fields SK, Comstock RD. The epidemiology of US high school basketball injuries, 2005-2007. Am J Sports Med. 2008;36(12):2328–2335. [DOI] [PubMed] [Google Scholar]
- 4. Borresen J, Lambert MI. The quantification of training load, the training response and the effect on performance. Sports Med. 2009;39(9):779–795. [DOI] [PubMed] [Google Scholar]
- 5. Caparrós T, Alentorn-Geli E, Myer GD, et al. The relationship of practice exposure and injury rate on game performance and season success in professional male basketball. J Sports Sci Med. 2016;15(3):397–402. [PMC free article] [PubMed] [Google Scholar]
- 6. Carling C, McCall A, Le Gall F, Dupont G. The impact of short periods of match congestion on injury risk and patterns in an elite football club. Br J Sports Med. 2016;50(12):764–768. [DOI] [PubMed] [Google Scholar]
- 7. Cumps E, Verhagen E, Meeusen R. Prospective epidemiological study of basketball injuries during one competitive season: ankle sprains and overuse knee injuries. J Sports Sci Med. 2007;6(2):204–211. [PMC free article] [PubMed] [Google Scholar]
- 8. Dick R, Hertel J, Agel J, Grossman J, Marshall SW. Descriptive epidemiology of collegiate men’s basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through. J Athl Train. 2007;42(2):194–201. [PMC free article] [PubMed] [Google Scholar]
- 9. Drakos MC, Domb B, Starkey C, Callahan L, Allen AA. Injury in the National Basketball Association: a 17-year overview. Sports Health. 2010;2(4):284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Drew MK, Cook J, Finch CF. Sports-related workload and injury risk: simply knowing the risks will not prevent injuries. Br J Sports Med. 2016;50(21):1306–1308. [DOI] [PubMed] [Google Scholar]
- 11. Ekstrand J, Hagglund M, Walden M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45(7):553. [DOI] [PubMed] [Google Scholar]
- 12. Folgado H, Duarte R, Marques P, Sampaio J. The effects of congested fixtures period on tactical and physical performance in elite football. J Sports Sci. 2015;33(12):1238–1247. [DOI] [PubMed] [Google Scholar]
- 13. Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Clin J Sport Med. 2006;16(2):97–106. [DOI] [PubMed] [Google Scholar]
- 14. Grimm NL, Jacobs JCJ, Kim J, Amendola A, Shea KG. Ankle injury prevention programs for soccer athletes are protective: a level-I meta-analysis. J Bone Joint Surg Am. 2016;98(17):1436–1443. [DOI] [PubMed] [Google Scholar]
- 15. Hagglund M, Walden M, Bahr R, Ekstrand J. Methods for epidemiological study of injuries to professional football players: developing the UEFA model. Br J Sports Med. 2005;39(6):340–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Klusemann MJ, Pyne DB, Hopkins WG, Drinkwater EJ. Activity profiles and demands of seasonal and tournament basketball competition. Int J Sports Physiol Perform. 2013;8(6):623–629. [DOI] [PubMed] [Google Scholar]
- 17. Kofotolis N, Kellis E. Ankle sprain injuries: a 2-year prospective cohort study in female Greek professional basketball players. J Athl Train. 2007;42(3):388–394. [PMC free article] [PubMed] [Google Scholar]
- 18. Longo UG, Loppini M, Berton A, Marinozzi A, Maffulli N, Denaro V. The FIFA 11+ program is effective in preventing injuries in elite male basketball players: a cluster randomized controlled trial. Am J Sports Med. 2012;40(5):996–1005. [DOI] [PubMed] [Google Scholar]
- 19. Mauntel TC, Wikstrom EA, Roos KG, Djoko A, Dompier TP, Kerr ZY. The epidemiology of high ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med. 2017;45(9):2156–2163. [DOI] [PubMed] [Google Scholar]
- 20. McGuine TA, Hetzel S, Pennuto A, Brooks A. Basketball coaches’ utilization of ankle injury prevention strategies. Sports Health. 2013;5(5):410–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mendiguchia J, Brughelli M. A return-to-sport algorithm for acute hamstring injuries. Phys Ther Sport. 2011;12(1):2–14. [DOI] [PubMed] [Google Scholar]
- 22. Pasanen K, Ekola T, Vasankari T, et al. High ankle injury rate in adolescent basketball: a 3-year prospective follow-up study. Scand J Med Sci Sports. 2017;27(6):643–649. [DOI] [PubMed] [Google Scholar]
- 23. Rae K, Orchard J. The Orchard Sports Injury Classification System (OSICS) version 10. Clin J Sport Med. 2007;17(3):201–204. [DOI] [PubMed] [Google Scholar]
- 24. Rodas G, Pruna R, Til G, Martín C. Clinical practice guide for muscular injuries: epidemiology, diagnosis, treatment and prevention. Apunts Medicina de l'Esport. 2009;44(164):149–209. [Google Scholar]
- 25. Starkey C. Injuries and illnesses in the National Basketball Association: a 10-year perspective. J Athl Train. 2000;35(2):161–167. [PMC free article] [PubMed] [Google Scholar]
- 26. Teramoto M, Cross CL, Cushman DM, Maak TG, Petron DJ, Willick SE. Game injuries in relation to game schedules in the National Basketball Association. J Sci Med Sport. 2017;20(3):230–235. [DOI] [PubMed] [Google Scholar]
- 27. Ullah S, Gabbett TJ, Finch CF. Statistical modelling for recurrent events: an application to sports injuries. Br J Sports Med. 2014;48(17):1287–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Valle X, Tol JL, Hamilton B, et al. Hamstring muscle injuries, a rehabilitation protocol purpose. Asian J Sports Med. 2015;6(4):e25411. [DOI] [PMC free article] [PubMed] [Google Scholar]