A 57-year-old male was diagnosed with a sigmoid colon perforation by an adenocarcinoma with synchronous liver metastasis (pT4aN0M1) and submitted to a Hartmann's operation with hepatic metastasectomy. After chemotherapy has been finished, the patient underwent intestinal transit reconstruction, and a colorectal anastomosis with protective ileostomy was performed. In the postoperative period, complete anastomotic stenosis developed, which was confirmed in sigmoidoscopy and computed tomography scan [Figure 1]. Leakage and fistulization were ruled out, and endoscopic treatment was scheduled after gastroenterology consultation.
Figure 1.
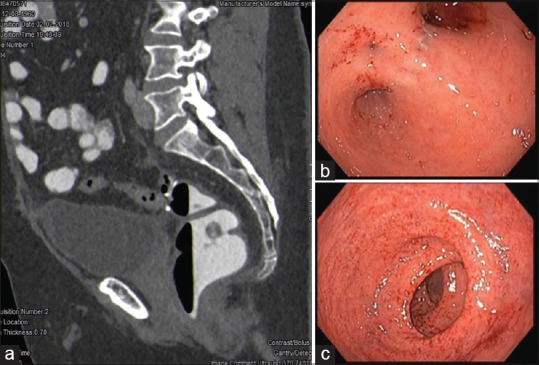
(a) Computed tomography scan (sagittal viewing) showing complete stenosis of colorectal anastomosis. Contrast administered to the anus was completely exteriorized. The contrast ingested filled small bowel loops, being excreted through the stoma. (b and c) Endoscopic viewing with derivative proctitis and complete lumen closure
A total colonoscopy was performed with anterograde progression through the ileostomy until the stricture. Mucus plugs made scope progression difficult. Gastrografin was injected to fill the lumen and to optimize ultrasound viewing. Using a forward-viewing linear echoendoscope introduced through the anus, EUS guided puncture of the upstream colon loop was accomplished with a 19G needle (EchoTip ProCore®, Cook Medical®, Ireland) that allowed further passage of the 0.035 guidewire under endoscopic control. A 6F cystotome (Endoflex®, Germany) and Through-The-Scope balloons (8 mm + 10 mm) were used for tract dilation. A lumen-apposing metal stent (LAMS) with 16 mm × 20 mm (SPAXUS®) was introduced through the fistula and deployed under endoscopic and fluoroscopic guidance. After deployment, the distal flare was placed juxta-anastomotic, being easily repositioned using a foreign body forceps. Contrast and mucus drainage confirmed lumen patency at the end of the procedure. In the control sigmoidoscopy performed after 1 week, LAMS was perpendicular to the lumen being removed. Complete recanalization of the anastomosis was achieved without extraluminal leakage [Figure 2].
Figure 2.
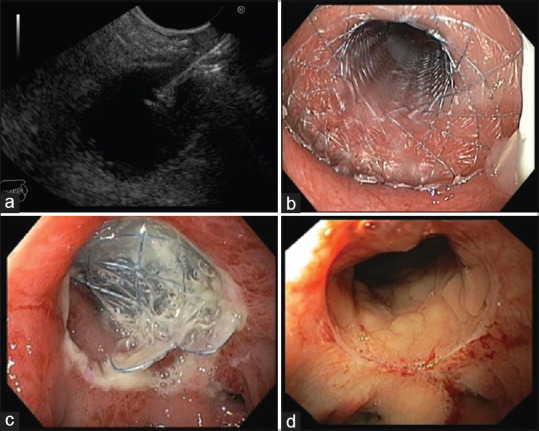
(a) EUS-guided puncture of the upstream colon loop with a 19G needle. (b) Lumen-apposing metal stent at the end of the procedure. (c) Lumen-apposing metal stent perpendicular to the lumen at the 1st week, being removed at this time. (d) Complete lumen recanalization 2 weeks after lumen-apposing metal stent removal
Anastomotic strictures usually occur after colorectal surgery. Complete lumen obstruction is uncommon and surgical reintervention may be indicated due to inability to pass conventional dilation systems and endoscopic stents.[1] Few cases of EUS-guided recanalization of complete anastomotic strictures using LAMS were described in anedoctical reports with favorable outcomes.[2,3] The present report highlights the effectiveness of this minimally invasive approach and its applicability in clinical practice.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initial will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Polese L, Vecchiato M, Frigo AC, et al. Risk factors for colorectal anastomotic stenoses and their impact on quality of life: What are the lessons to learn? Colorectal Dis. 2012;14:e124–8. doi: 10.1111/j.1463-1318.2011.02819.x. [DOI] [PubMed] [Google Scholar]
- 2.Saxena P, Azola A, Kumbhari V, et al. EUS-guided rendezvous and reversal of complete rectal anastomotic stenosis after Hartmann's reversal. Gastrointest Endosc. 2015;81:467–8. doi: 10.1016/j.gie.2014.04.055. [DOI] [PubMed] [Google Scholar]
- 3.Poincloux L, Pezet D, Rouquette O. Successful recanalization of complete anastomotic stricture using colorectal endoscopic ultrasound-guided rendezvous thus allowing stoma reversal: Two cases. Endoscopy. 2016;48:E353–4. doi: 10.1055/s-0042-118179. [DOI] [PubMed] [Google Scholar]


