Abstract
Background
The definition of tall cell variant of papillary thyroid carcinoma (TCV‐PTC) depends on the articles, and the defined cytological findings characteristic of TCV‐PTC have not yet been fully analyzed. This study aimed to establish the cytological characteristics of TCV‐PTC.
Methods
We retrospectively analyzed the smears of 19 TCV‐PTC and 50 conventional PTC (C‐PTC) cases.
Results
Palisaded pattern with the nuclei locating at the base of tall columnar carcinoma cells was seen in 94.7% of TCV‐PTCs, and the incidence was significantly higher than that of C‐PTCs (P < .0001). The palisaded pattern tended to appear at the periphery of the cell clusters. Isolated tall columnar carcinoma cells were present in 89.5% of TCV‐PTCs. The incidence was significantly higher than that of C‐PTC (P = .0001). Tombstone appearance was identified in 78.9% of TCV‐PTCs, but not in C‐PTCs. Spindle‐like carcinoma cells with tapering cytoplasmic end appeared in 68.4% and 12.0% of TCV‐PTC and C‐PTC, respectively (P < .0001). The cytoplasm of TCV‐PTC was densely stained and its cell border was distinct. Cytoplasmic elongation toward an outside of the cell clusters was observed in 89.5% of TCV‐PTCs.
Conclusion
It is the most important to identify the presence of the tall columnar carcinoma cells on the cytological preparations, in order to distinguish TCV‐PTC from C‐PTC. We propose five cytological findings indicating TCV‐PTC, (1) palisaded pattern, (2) tall columnar cells with the heights of at least three times their widths, (3) tombstone appearance, (4) spindle‐like carcinoma cells, and (5) cytoplasmic elongation.
Keywords: cytoplasmic elongation, palisaded pattern, papillary thyroid carcinoma, soap bubble appearance, tall cell variant, tombstone appearance
1. INTRODUCTION
Papillary thyroid carcinoma (PTC) is the most common malignancy arising in the thyroid, generally shows an excellent prognosis, and has several variants in addition to conventional PTC.1, 2, 3 Tall cell variant (TCV) of PTC shows aggressive biological behavior, and frequently has extrathyroidal extension, nodal metastasis, and distant metastasis.1, 2, 3, 4, 5, 6, 7, 8, 9 Histologically, TCV‐PTC is characterized by a presence of tall columnar carcinoma cells with nuclear features of PTC, but the definition and proportion of the tall columnar carcinoma cells depend on the articles. Several authors defined the tall columnar carcinoma cells as a height greater than twice its width.4, 5, 6, 8 However, WHO classification2 and the 2017 Bethesda System for Reporting Thyroid Cytopathology (2017 TBSRTC)1 described that the heights of carcinoma cells require three times their widths. The percentage of tall columnar carcinoma cells needed in TCV‐PTC varies in the literature, and ranges 10%‐75%.4, 5, 8, 9, 10, 11
Fine needle aspiration cytology (FNAC) is a reliable tool preoperatively to diagnosis PTC. According to some reports describing the cytological finding of TCV‐PTC, the carcinoma cells exhibit large polygonal cells or elongated cells with increased intranuclear cytoplasmic inclusions, abundant cytoplasm, cytoplasmic tail, and distinct cell border.1, 5, 7, 8 “Soap bubble appearance” is frequently observed in TCV‐PTCs.5, 8 However, we think that it is difficult to make a diagnosis of TCV‐PTC based on such findings. In addition, considering the controversial definition on TCV‐PTC, the defined cytological findings of the carcinoma cells characteristic of TCV‐PTC have not yet been fully analyzed. In this report, we aimed to establish the cytological characteristics of TCV‐PTC in comparing cytological specimens of 19 TCV‐PTCs and 50 conventional PTCs (C‐PTCs).
2. MATERIALS AND METHODS
We reviewed pathology report database of 8705 patients with PTC that underwent surgery at Kuma Hospital from January 2008 to December 2015, and extracted 23 patients with TCV‐PTC (0.3%) with preoperative FNAC among them. The patients included 20 women and 3 men, with a mean age of 65 years (range, 25‐85 years). We reviewed clinical data obtained from medical records of Kuma Hospital. Ultrasonographically, the greatest dimension of the tumors ranged from 0.6 to 6.5 cm (mean, 3.0 cm). A histological diagnosis of TCV‐PTC required the following: (1) tall columnar carcinoma cells (a height greater than three times its width) in greater than 50% of tumor nodules, (2) nuclear features typical of PTC, and (3) no necrosis (Figure 1). We excluded the other carcinomas composed of tall columnar carcinoma cells, such as columnar cell variant PTC, Warthin tumor‐like PTC, cribriform variant PTC, and metastatic colonic carcinoma. Ultrasound‐guided FNAC was performed using a 22‐gauge needle without local anesthesia. The smears were produced using a press and release method,12 and were stained with Papanicolaou stain. When bloody samples were aspirated, we removed the blood components by tilting the preparations immediately after the smearing.12 According to the original cytology reports, there were four nondiagnostic or unsatisfactory cases. The remaining 19 cases were reported as malignant. The estimated diagnoses were PTC in 18 and PTC or poorly differentiated carcinoma in 1. Among them, one case was suspected TCV‐PTC. Then, we retrospectively analyzed the smears of 19 TCV‐PTC cases that cytological specimens were sufficient. In addition, we examined 50 C‐PTC cases that we had experienced in 2017, in order to compare with TCV‐PTC. Statistical significance of the data was determined using Fisher's probability test; P < .05 was considered statistically significant.
Figure 1.
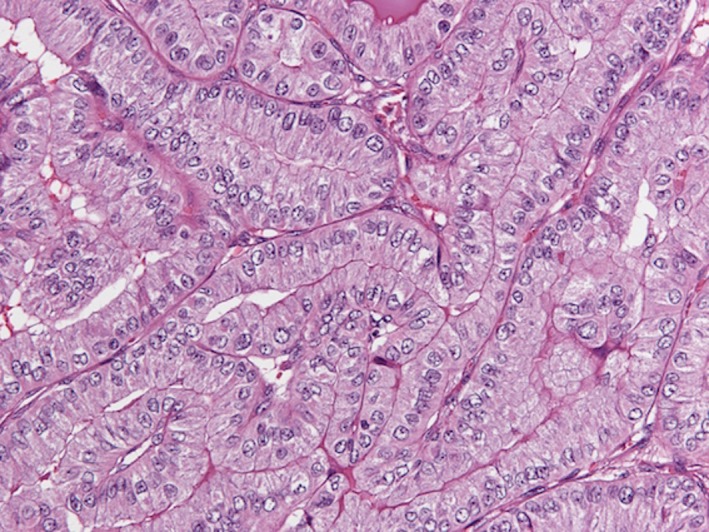
Histology of tall cell variant of papillary thyroid carcinoma. The carcinoma cells show a height greater than three times its width. (HE stain, 200×) [Color figure can be viewed at wileyonlinelibrary.com]
3. RESULTS
The cytological findings of the aspirates obtained from the 19 TCV‐PTC and 50 C‐PTC cases are summarized in Table 1.
Table 1.
Cytological findings of tall cell variant and conventional papillary thyroid carcinomas
| Cytological findings | Tall cell variant (n = 19) | Conventional (n = 50) | P | |
|---|---|---|---|---|
| Background | Foam cells | 4 (21.1%) | 11 (22.0%) | N.S. |
| Lymphocytes | 1 (5.3%) | 16 (32.0%) | .0274 | |
| Multinucleated giant cells | 13 (68.4%) | 28 (56.0%) | N.S. | |
| Watery colloid | 0 (0.0%) | 8 (16.0%) | N.S. | |
| Ropy colloid | 6 (31.6%) | 8 (16.0%) | N.S. | |
| Psammoma bodies | 0 (0.0%) | 2 (4.0%) | N.S. | |
| Arrangement | Papillary | 17 (89.5%) | 41 (82.0%) | N.S. |
| Follicular | 0 (0.0%) | 23 (46.0%) | .0001 | |
| Monolayered sheet‐like | 17 (89.5%) | 49 (98.0%) | N.S. | |
| Trabecular | 1 (5.3%) | 0 (0.0%) | N.S. | |
| Solid | 3 (15.8%) | 0 (0.0%) | .0185 | |
| Predominantly isolated | 1 (5.3%) | 6 (12.0%) | N.S. | |
| Palisaded | 18 (94.7%) | 8 (16.0%) | <.0001 | |
| Cell shape | Round or oval | 6 (31.6%) | 50 (100.0%) | <.0001 |
| Tall columnar | 17 (89.5%) | 18 (36.0%) | .0001 | |
| Tombstone appearance | 15(78.9%) | 0 (0.0%) | <.0001 | |
| Spindle‐like | 13 (68.4%) | 6 (12.0%) | <.0001 | |
| Cytoplasm | Densely stained | 18 (94.7%) | 25 (50.0%) | .0006 |
| Distinct cell border | 17 (89.5%) | 19(38.0%) | .0001 | |
| Cytoplasmic elongation | 17 (89.5%) | 24 (48.0%) | .0021 | |
| Septated intracytoplasmic vacuoles | 0 (0.0%) | 4 (8.0%) | N.S. | |
| Pseudokeratinization | 5 (26.3%) | 5 (10.0%) | N.S. | |
| Nucleus | Ground glass appearance | 1 (5.3%) | 7 (14.0%) | N.S. |
| Cytoplasmic inclusions | 17 (89.5%) | 41 (82.0%) | N.S. | |
| Soap bubble appearance | 8 (42.1%) | 14 (28.0%) | N.S. | |
| Grooves | 19 (100.0%) | 49 (98.0%) | N.S. | |
| Overlapping | 13 (68.4%) | 8 (16.0%) | .0001 | |
| Various‐sized | 1 (5.3%) | 2 (4.0%) | N.S. | |
| Multilobated | 2 (10.5%) | 7 (14.0%) | N.S. | |
| Mitotic figure | 3 (15.8%) | 7 (14.0%) | N.S. | |
N.S.: Not significant P > .05.
The characteristic findings for the tall cell variant are written in bold letters.
3.1. Background
Lymphocytes were less frequently seen in TCV‐PTC (5.3%) than C‐PTC (32.0%), and there was significantly difference (P < .05). Watery colloid was not observed in TCV‐PTC. The incidence of ropy colloid was higher in TCV‐PTC (31.6%) than C‐PTC (16.0%).
3.2. Arrangement
The carcinoma cells of TCV‐PTC were cohesive, and predominantly isolated cell pattern was rare (5.3%). Most of TCV‐PTC and C‐PTC exhibited papillary and monolayered sheet‐like pattern. The papillary pattern appeared in 89.5% of TCV‐PTC and 82.0% of C‐PTC. Follicular arrangement was not observed in TCV‐PTC, but 46.0% in C‐PTC. Palisaded pattern with the nuclei locating at the base of the tall columnar carcinoma cells was in 94.7% of TCV‐PTCs, and the incidence was significantly higher than that of C‐PTCs (P < .0001) (Figure 2). The nuclei were overlapped and located on the basal side of the carcinoma cells. Three TCV‐PTCs showed solid pattern, but no C‐PTCs showed the pattern (Figure 3).
Figure 2.
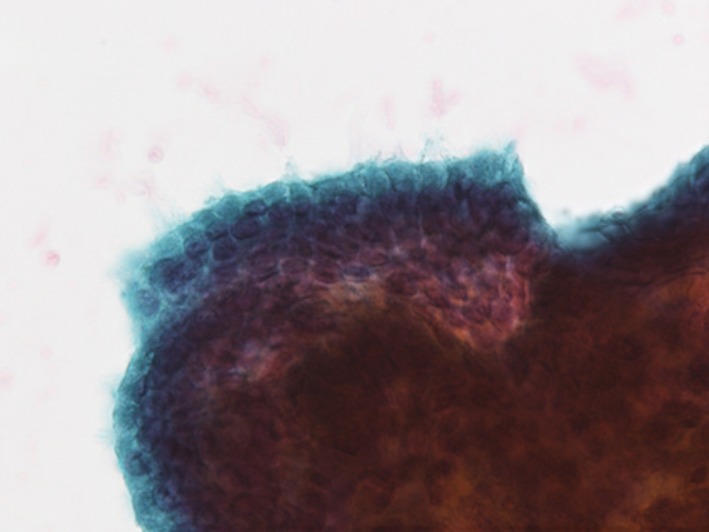
A palisaded arrangement composed of tall columnar carcinoma cells is seen at the periphery of large cell nest. The nuclei are overlapped and located on the basal side of the carcinoma cells. (Papanicolaou stain, 200×) [Color figure can be viewed at wileyonlinelibrary.com]
Figure 3.
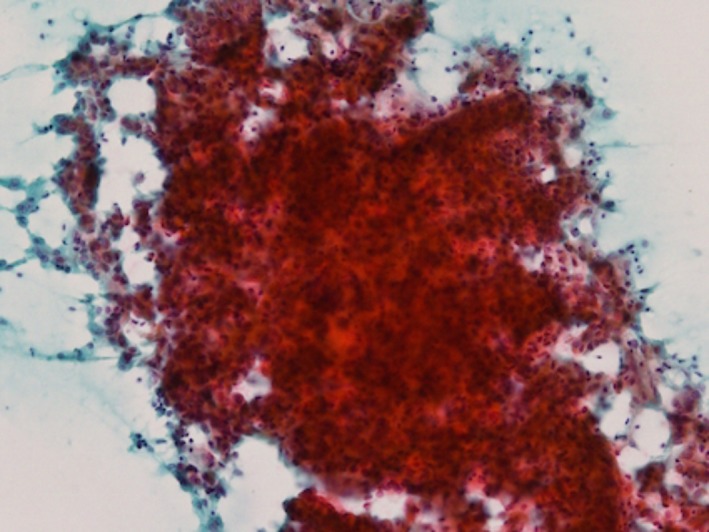
The carcinoma cells show large solid cell clusters. Neither papillary nor follicular pattern is seen. (Papanicolaou stain, 100×) [Color figure can be viewed at wileyonlinelibrary.com]
3.3. Cell shape
The tall columnar carcinoma cells were observed in 89.5% and 36.0% of TCV‐PTC and C‐PTC, respectively (P = .0001). The tall columnar cells were observed as palisaded pattern (Figure 4), isolated cells (Figure 5), or at the periphery of the large cell clusters (Figure 2). The polarity was almost preserved, and the nuclei were located at the base of the carcinoma cells. The tall columnar carcinoma cells occasionally showed tombstone appearance (Figure 5), which was identified in 78.9% of TCV‐PTCs. No C‐PTC with tombstone appearance was observed. Spindle‐like carcinoma cells with tapering cytoplasmic end appeared in 68.4% and 12.0% of TCV‐PTC and C‐PTC, respectively (P < .0001) (Figure 6). In two TCV‐PTCs, the spindle‐like carcinoma cells occupied more than half of carcinoma.
Figure 4.
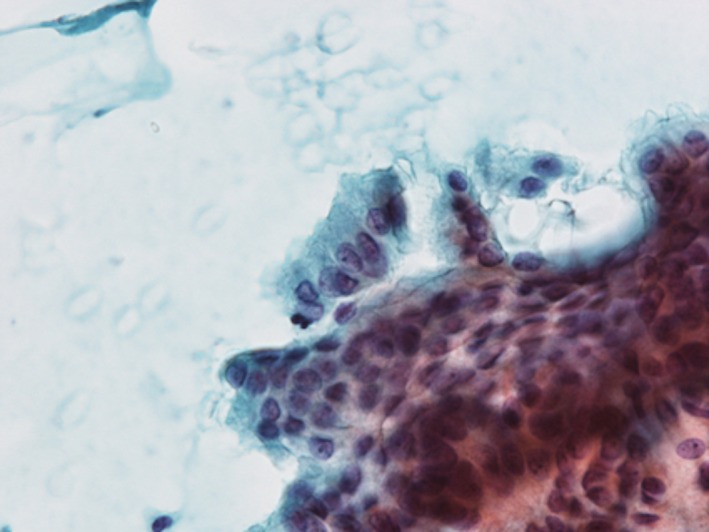
Tall columnar carcinoma cells showing palisaded pattern. The nuclei are basilary located, and the cytoplasm is densely stained. (Papanicolaou stain, 200×) [Color figure can be viewed at wileyonlinelibrary.com]
Figure 5.
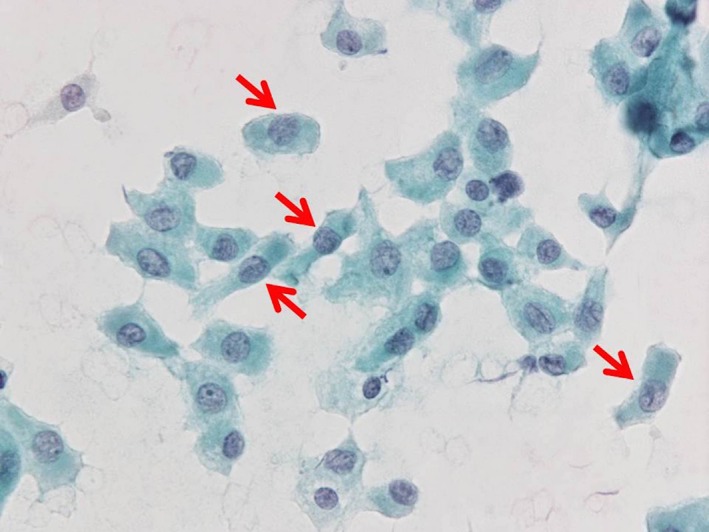
Tall columnar carcinoma cells with abundant and deeply stained cytoplasm appear as isolated cells. Some of them show tombstone appearance (arrows). (Papanicolaou stain, 400×) [Color figure can be viewed at wileyonlinelibrary.com]
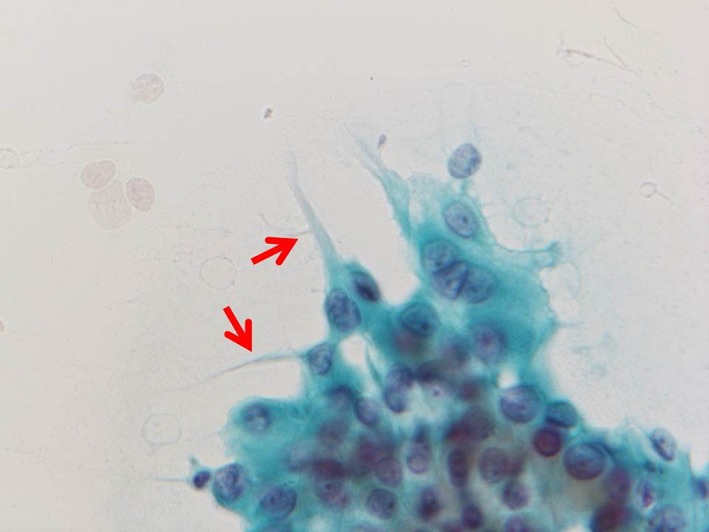
Figure 6.
Spindle‐like carcinoma cells with tapering cytoplasmic end (arrows). (Papanicolaou stain, 400×) [Color figure can be viewed at wileyonlinelibrary.com]
3.4. Cytoplasm
The cytoplasm of TCV‐PTC was densely stained and its cell border was distinct, but not typical oxyphilic (Figures 4 and 5). Cytoplasmic elongation toward an outside of the cell clusters was observed in 89.5%% of TCV‐PTCs (P = .0021) (Figure 7). Septated intracytoplasmic vacuoles were not observed in TCV‐PTCs. In 26.3% of TCV‐PTCs, the carcinoma cells with pink to orangophilic cytoplasm (pseudokeratinization) were seen (Figure 8).
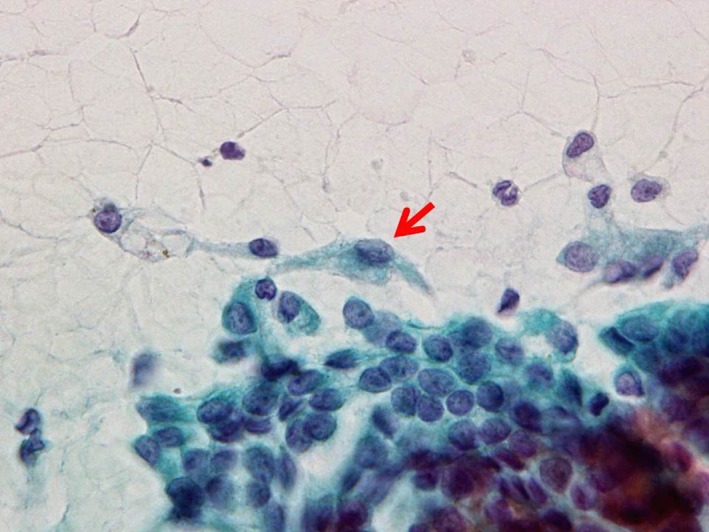
Figure 7.
The carcinoma cells show cytoplasmic elongation (arrows) toward the outside of the cluster. (Papanicolaou stain, 400×) [Color figure can be viewed at wileyonlinelibrary.com]
Figure 8.
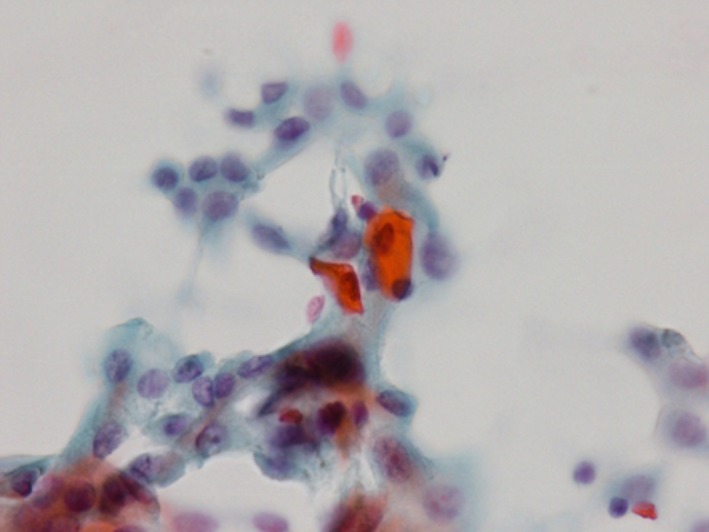
The two carcinoma cells are polyhedral in shape, and the cytoplasm is orangophilic. The appearance is similar to keratinized squamous cells, but squamous differentiation is not histologically identified in resected specimens. (Papanicolaou stain, 400×) [Color figure can be viewed at wileyonlinelibrary.com]
3.5. Nuclei
The incidences of ground glass appearance, intranuclear cytoplasmic inclusions, nuclear grooves, and nuclear overlapping in TCV‐PTC were 5.3%, 89.5%, 100.0%, and 68.4%, respectively. Among them, the incidence of overlapping nuclei in TCV‐PTCs was significantly higher (P = .0001), compared with C‐PTCs (16.0%) (Figure 9). On the incidences of the soap bubble appearance, there were no significant between TCV‐PTC and C‐PTC (Figure 10).
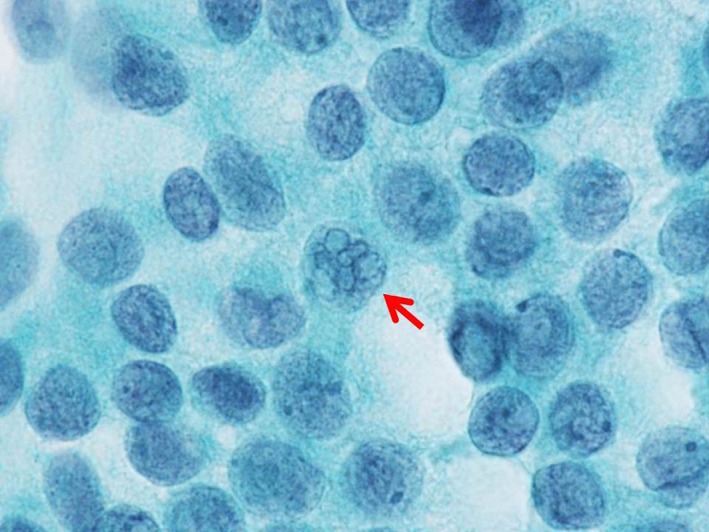
Figure 9.

The nuclei were overlapped, and the nuclear membrane (arrow) is thickened. (Papanicolaou stain, 1000×) [Color figure can be viewed at wileyonlinelibrary.com]
Figure 10.
The nuclei of the carcinoma cells show cytoplasmic inclusions and grooving. Soap bubble type cytoplasmic inclusions (arrow) are noted. (Papanicolaou stain, 1000×) [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
Diagnostic criteria of TCV‐PTC depend on the literature. The tall cells have been generally defined as at least twice as tall as their widths.4, 5, 6, 8 However, C‐PTC can be actually composed of tall columnar carcinoma cells consistent with the criterion.10 WHO classification and 2017 TBSRTC described that the heights of carcinoma cells are three times their widths.1, 2 The percentage of tall columnar carcinoma cells needed in TCV‐PTC varies, and ranges 10%‐75%.4, 5, 8, 9, 10 In this study, in order to clarify cytological features characteristic of TCV‐PTC, we adopted the strict criteria, the heights of at least three times their widths and more than 50% of the tumor, which was used in the study by Ito et al.11
In order to distinguish TCV‐PTC from C‐PTC, it is the most important to identify the presence of the tall columnar carcinoma cells on the cytological preparations. In this study, the palisaded pattern composed of the tall columnar carcinoma cells tended to be observed at the periphery of large cell clusters. The nuclei were crowded and located on the basal side of the carcinoma cells. We think that the findings are the most understandable and reliable to recognize the tall columnar configuration. Solomon et al. described that nuclear overlapping appeared to be more pronounced in specimens of C‐PTC as compared with TCV‐PTC.5 We agree with the findings on isolated carcinoma cells, because the carcinoma cells have abundant cytoplasm. However, it should be noted that the carcinoma cells appearing as cell clusters showed nuclear crowding. We think that cytoplasmic elongation toward the outside of the cell clusters also reflects the tall columnar configuration, because they appeared in the same place as the tall columnar carcinoma cells with palisaded pattern. The findings have been described as tapering cytoplasmic tail, tail‐like cell, tadpole cell, or elongated cell.5, 7, 8, 9 It is described that the cytoplasmic tails extend from the basal portion of the carcinoma cells.9 However, we disagree with the view. The tall carcinoma cells have basally located nuclei and abundant cytoplasm occupies the luminal side. The cytoplasmic elongation appears at the outside of the cell clusters. Therefore, we think that the cytoplasmic elongation must exist at the luminal side of the carcinoma cells, and the appearance is probably due to cytoplasmic degeneration during the smearing and staining. The term “tail” means the rear or bottom end of the body. Luminal and basal sides of columnar cells correspond to the head and bottom, respectively. Therefore, it is not appropriate to use the term “tail” for the cytoplasmic elongation existing at the luminal side.
When the carcinoma cells individually appeared, it is easy to recognize the tall columnar configuration. Such carcinoma cells occasionally appeared as spindle‐like carcinoma cells with tapering cytoplasmic end. The findings seem to be due to cytoplasmic degeneration. The similar findings were described as features of cribriform variant of PTC containing the tall columnar carcinoma cells.12 Some carcinoma cells showed tombstone appearance, in which both luminal and basal borders were horizontal. Tombstone cells are isolated tall columnar carcinoma cells and are described as one of cytological findings of pancreatic ductal adenocarcinoma.13 The isolated carcinoma cells with tombstone appearance might keep the cell shape without cytoplasmic degeneration.
Thyroid carcinomas composed of the tall columnar carcinoma cells, including columnar cell variant PTC, Warthin tumor‐like PTC, cribriform variant PTC, and metastatic colonic carcinoma, could be differential diagnoses of TCV‐PTC. However, it is not difficult to distinguish TCV‐PTC from the four carcinomas. Columnar cell variant PTC and metastatic colonic carcinoma are characterized by nuclear pseudostratification, a paucity of nuclear pseudoinclusions and grooves, and dark and granular chromatin pattern.14, 15 Warthin tumor‐like PTC exhibits abundant lymphocytes on the background.15 Cribriform variant of PTC occurs in young patients and shows cribriform pattern, morules, and peculiar nuclear clearing.12
Solomon et al. reported that soap‐bubble type intranuclear cytoplasmic inclusions appeared in cases of TCV‐PTC, but not observed in any C‐PTC.5 Lee et al. described that the finding is helpful in the diagnosis of TCV‐PTC.16 In our study, however, the incidence (42.1%) of soap‐bubble appearance in TCV‐PTC was higher than that (28.0%) in C‐PTC, but there was no statistical significant. Then, soap‐bubble type intranuclear cytoplasmic inclusions are not specific to TCV‐PTC. We should not overestimate them in the diagnosis of TCV‐PTC.
The cytoplasm of TCV‐PTC is often eosinophilic, but has not cytoplasmic granularity.8, 9, 10 Therefore, it does not belong to Hürthle cell carcinomas. Actually, the abundant cytoplasm seen in our cases was densely stained, but not granular. Distinct cell border is also one of the features in TCV‐PTC.5, 8, 9, 16 Concerning the finding, we demonstrated the statistical difference between TCV‐PTC and C‐PTC. However, we think that both eosinophilic cytoplasm and distinct cell border are not helpful in diagnosing TCV‐PTC, because the findings can be seen even in C‐PTC.
In conclusion, it is the most important to identify the presence of the tall columnar carcinoma cells on the cytological preparations, in order to distinguish TCV‐PTC from C‐PTC. We propose five cytological findings indicating TCV‐PTC, (1) palisaded pattern, (2) tall columnar cells with the heights of at least three times their widths, (3) tombstone appearance, (4) spindle‐like carcinoma cells, and (5) cytoplasmic elongation.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest with the contents of this article.
DISCLOSURE OF INTERESTS
The authors have no connection to any companies or products mentioned in this article.
ETHICS STATEMENT
The authors confirm that the study complies with the guidelines of the ethics committee of Kuma hospital and that all subjects provided informed consent.
Tanaka A, Hirokawa M, Higuchi M, et al. Diagnostic clues indicating tall cell variants of papillary thyroid carcinoma in fine needle aspiration. Diagn Cytopathol. 2019;47:452–457. 10.1002/dc.24122
REFERENCES
- 1. Pusztaszeri MP, Auger M, Stelow EB, Yang GCH, Sanchez MA, VA LV. Papillary thyroid carcinoma, variants, and related tumors In: Cibas ES, Ali SZ, eds. The Bethesda System for Reporting Thyroid Cytopathology. 2nd ed. New York, NY: Springer Nature; 2018:119‐156. [Google Scholar]
- 2. Lloyd RV, Osamura RY, Klöppel G, Rosai J. Classification of Tumours of Endocrine Organs. Switzerland: WHO; 2017:81‐91. [Google Scholar]
- 3. Rosai J, DeLellis RA, Carcangiu ML, Frable WJ, Tallini G. Tumors of the Thyroid and Parathyroid Glands (AFIP Atlas of Tumor Pathology Series 4). Silver Spring, MD: American Registry of Pathology; 2014:146‐149. [Google Scholar]
- 4. Wang X, Cheng W, Liu C, Li J. Tall cell variant of papillary thyroid carcinoma: current evidence on clinicopathologic features and molecular biology. Oncotarget. 2016;7:40792‐40799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Solomon A, Gupta PK, LiVolsi VA, Baloch ZW. Distinguishing tall cell variant of papillary thyroid carcinoma from usual variant of papillary thyroid carcinoma in cytologic specimens. Diagn Cytopathol. 2002;27:143‐148. [DOI] [PubMed] [Google Scholar]
- 6. Gamboa‐Domínguez A, Candanedo‐González F, Uribe‐Uribe NO, Angeles‐Angeles A. Tall cell variant of papillary thyroid carcinoma a Cytohistologic correlation. Acta Cytol. 1997;41:672‐676. [DOI] [PubMed] [Google Scholar]
- 7. Urano M, Kiriyama Y, Takakuwa Y, Kuroda M. Tall cell variant of papillary thyroid carcinoma:its characteristic features demonstrated by fine‐needle aspiration cytology and Immunohistochemical study. Diagn Cytopathol. 2009;37:732‐737. [DOI] [PubMed] [Google Scholar]
- 8. Guan H, VandenBussche CJ, Erozan YS, et al. Can the tall cell variant of papillary thyroid carcinoma be distinguished from the conventional type in fine needle aspirates? A Cytomorphologic study with assessment of diagnostic accuracy. Acta Cytol. 2013;57:534‐542. [DOI] [PubMed] [Google Scholar]
- 9. Demay RM. The Art & Science of Cytopathology. 2nd ed. Chicago, IL: American Society for Clinical Pathology; 2012:904. [Google Scholar]
- 10. LiVolsi VA. Papillary carcinoma tall cell variant (TCV): a review. Endocr Pathol. 2010;21:12‐15. [DOI] [PubMed] [Google Scholar]
- 11. Ito Y, Hirokawa M, Miyauchi A, Higashiyama T, Kihara M, Miya A. Prognostic significance of the proportion of tall cell components in papillary thyroid carcinoma. World J Surg. 2017;41:742‐747. [DOI] [PubMed] [Google Scholar]
- 12. Hirokawa M, Suzuki A, Miyauchi A. Thyroid fine‐needle aspiration and smearing techniques. VideoEndocrinology. 2018;5(2). 10.1089/ve.2018.0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Conrad R, Castelino‐Prabhu S, Cobb C, Raza A. Cytopathology of the pancreatobiliary tract‐the agony, and sometimes, the ease of it. J Gastrointest Oncol. 2013;4:210‐219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bongiovanni M, Mermod M, Canberk S, et al. Columnar cell variant of papillary thyroid carcinoma: Cytomorphological characteristics of 11 cases with histological correlation and literature review. Cancer Cytopathol. 2017;125:389‐397. [DOI] [PubMed] [Google Scholar]
- 15. Monappa V, Kudva R. Cytomorphologic diversity of papillary thyroid carcinoma. J Cytol. 2017;34:183‐187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lee SH, Jung CK, Bae JS, Jung SL, Choi YJ, Kang CS. Liquid‐based cytology improves preoperative diagnostic accuracy of the tall cell variant of papillary thyroid carcinoma. Diagn Cytopathol. 2013;42:11‐17. [DOI] [PubMed] [Google Scholar]


