Abstract
OBJECTIVES
Tracheostomy is a method of separating a patient from the mechanical ventilator in the intensive care unit (ICU). The long-term survivors among patients followed up with tracheostomy and ventilator in the respiratory ICU (RICU) outpatient clinic due to different diseases were investigated.
MATERIALS AND METHODS
This was a retrospectively designed cohort study between January 2004 and July 2018. Patients with chronic respiratory failure followed up with tracheostomy and/or ventilator at the RICU outpatient clinic were included in the study. Age, gender, indications and date of tracheostomy, use of domestic mechanical ventilation, and mortality were recorded. The groups were compared according to age, gender, and tracheostomy indication diseases, and the 1–3-year long-term mortality rates were analyzed by the Kaplan–Meier survival analysis, and the Cox regression test was performed.
RESULTS
A total of 134 (64% male) patients with a median age of 66 (54–73) years were included in the study. The indications for tracheostomy were heart failure (HF) and cerebrovascular diseases (38.1%), chronic obstructive pulmonary disease (COPD) (23.1%), neuromuscular diseases (22.4%), obesity hypoventilation (9.7%), and kyphoscoliosis (6.7%). Mortality was higher in patients >75 years old in the 3-year follow-up (p=0.022). The 3-year mortality hazard ratio (HR) factors and 95% confidence interval (CI) were as follows: age >75 years HR=1.71 (95% CI, 1.03–2.82; p<0.036) and HF and cerebrovascular disease diseases sequela HR=1.84 (95% CI, 1.03–3.29; p<0.041) significantly increased the 3-year mortality, and having COPD decreased mortality in 46% (p<0.041).
CONCLUSION
Patients with neuromuscular disorders, kyphoscoliosis, and COPD who have undergone tracheostomy were the luckiest group according to the 3-year survival rates, whereas patients with HF and cerebrovascular diseases were the unluckiest ones. The most important decision triangle is the patient’s acceptance (A), family support (B), and tracheostomy indication (C), and this may vary from country to country depending on the beliefs of subjects.
Keywords: Home mechanical ventilation, intensive care unit, mortality, tracheostomy
INTRODUCTION
In the intensive care unit (ICU), 10% of patients undergoing mechanical ventilation face prolonged mechanical ventilation problems [1]. Tracheostomy is an inevitable method when applied due to motor neuron diseases involving the respiratory muscle. The physician generally considers tracheostomy in patients with invasive mechanical ventilation due to chronic respiratory failure, such as morbid obese who have sleep disorders or obesity hypoventilation and chronic obstructive pulmonary diseases (COPDs), kyphoscoliosis that requires mechanical ventilation support, and neuromuscular diseases that require ventilation support >16 h/day. Even physicians can request opening tracheostomy in patients with advanced stage heart failure (HF; ejection fraction <20%) and sequela cerebrovascular disease (CVA; immobile, swallowing, and affected respiratory muscle motor function) [2].
Few data are available with regard to the long-term outcome of tracheostomized patients; previous studies have examined hospital stay, hospital mortality, and the 30-day mortality of patients [3–5]. Available data are also limited for evaluating survival from different diseases that required tracheostomy [6].
The aim of the present study was to investigate tracheostomized patients with different diseases that would contribute to predicting the long-term survival with tracheostomy and/or ventilator after discharge from the respiratory ICU (RICU).
MATERIALS AND METHODS
Study Design
This retrospective cohort study included patients ≥18 years old who had been referred to our RICU outpatient clinic between January 2004 and July 2018. This study was approved by the local ethics committee of Health Sciences University Süreyyapaşa Chest Diseases and Thoracic Surgery Training and Research Hospital, İstanbul, Turkey (12.07.2018/048) in accordance with the Declaration of Helsinki. Informed consent was not obtained from the patients due to the retrospective nature of the study design.
Patients
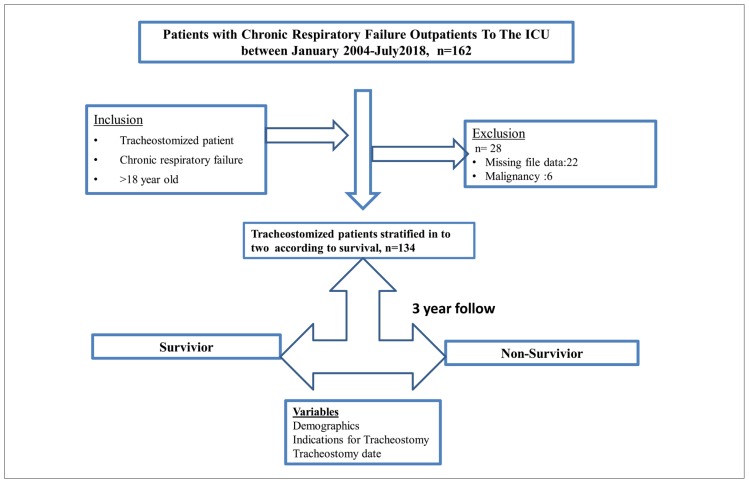
Patients who had tracheostomy due to malignancy and those whose file records were missing were excluded from the study (Figure 1). Patients with chronic respiratory failure due to advanced COPD, obesity hypoventilation syndrome (OHS), kyphoscoliosis, neuromuscular disease (amyotrophic lateral sclerosis or Duchenne muscular dystrophy) and HF and CVA diseases followed up with prolonged mechanical ventilation were included in the study. The patients were divided into two groups: survivors and non-survivors.
Figure 1.
Flowchart of patient enrollment
Definitions
Chronic Obstructive Pulmonary Diseases (COPD)
COPD was defined as a clinical history, symptom, and airflow obstruction on spirometry as a forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) ratio (FEV1/FVC) of ≤70% [7]. Patients followed up with a diagnosis of COPD also had chronic respiratory difficulty and were using a non-invasive mechanical ventilator.
Obesity Hypoventilation Syndrome (OHS)
OHS was defined by a body mass index of >30 kg/m2, daytime partial carbon dioxide pressure of ≥45 mmHg, and clinical symptoms of chronic renal failure in the absence of other known causes of hypoventilation [8].
Home Mechanical Ventilation (HMV)
HMV was defined as ventilation via a tracheostomy for a period of ≥3 months on a daily basis performed mostly in the user’s home or other long-term care facility. MV was delivered in the pressure assist-control ventilation mode and the pressure support mode [9]. Ventilatory support was administered via tracheostomy in patients who needed >16 h of daily ventilation or those with bulbar failure [10].
Prolonged mechanical ventilation as defined in the National Association for Medical Direction of Respiratory Care was the need of >21 consecutive days of mechanical ventilation [11].
Follow-up
Patients with tracheostomy were referred to follow-up visits every 1–3-month intervals for cannula replacement, depending on the type of the cannula, for at least 36 months in the ICU outpatient clinic. The physical examination findings were recorded on the patient files on each visit. In addition to cannula replacement, the tracheostomy region was also evaluated in terms of signs of infection, including redness, discharge, and bad smell on each follow-up visit. The ventilation mode and ventilator use frequency of the patients followed by HMV were evaluated, and the attempts for separation from a ventilator were questioned.
Recorded Data
Demographic data (age and gender), primary diagnosis, indication for tracheotomy, tracheostomy time, and daily home ventilator requirement were recorded retrospectively from our outpatient clinic patients’ medical files. Patient death dates were recorded in the National Death Notification System.
Statistical Analysis
All statistical analyses were performed using the portable Statistical Package for the Social Sciences version 20 (SPSS IBM Corp.; Armonk, NY, USA). When the continuous variables were distributed abnormally, they were presented as the median with interquartile range (IQR, 25%–75%), and the study groups were compared using the Mann–Whitney U test. Counts and percentages were used as applicable. We used the Pearson chi-square test for categorical variables (dichotomous variables). The Kaplan–Meier survival curves were performed for patient survivor/non-survivor and gender. The Cox regression analysis was used to define the 3-year mortality risk factors. Age >75 years, male gender, and diseases (COPD, OHS, kyphoscoliosis, neuromuscular diseases, and HF–CVA diseases) were included in the Cox regression model.
RESULTS
During the 14-year study period, 134 out of 162 patients admitted to the RICU outpatient clinic were included in the study. Twenty-two patients were excluded from the study due to missing data and six patients due to malignancy (five due to larynx cancer and one due to nasopharyngeal cancer). Figure 1 shows the flowchart of patient enrollment.
The median (IQR) age of the patients was 66 (54–73) years, and more than half of them were male. Among the indications for tracheostomy, HF–CVA sequela was the most common, followed by COPD and neuromuscular diseases. The follow-up durations of all patients were >3 years. Table 1 shows the demographic characteristics, indications for tracheostomy, and the mean follow-up durations.
Table 1.
Baseline characteristics
| Variables | Tracheostomized patients (n=134) |
|---|---|
| Gender, male, n (%) | 86(64) |
| Age, median (IQR) (years) | 66 (54–73) |
| Age, n (%) | |
| —≥65 years | 71(53) |
| —≥75 years | 31(23) |
| —≥80 years | 15(11) |
| Tracheostomy indication, n (%) | |
| —COPD | 31(23) |
| —OHS | 13(10) |
| —Kyphoscoliosis | 9(7) |
| —Neuromuscular diseases | 30(22) |
| —HF and CVA | 51(38) |
| Follow-up, median (IQR) (day) | 852(420–1538) |
Median (IQR): median and interquartile range (IQR, 25th–75th percentile); COPD: chronic obstructive pulmonary disease; OHS: obesity hypoventilation syndrome; HF and CVA: heart failure and cerebrovascular disease
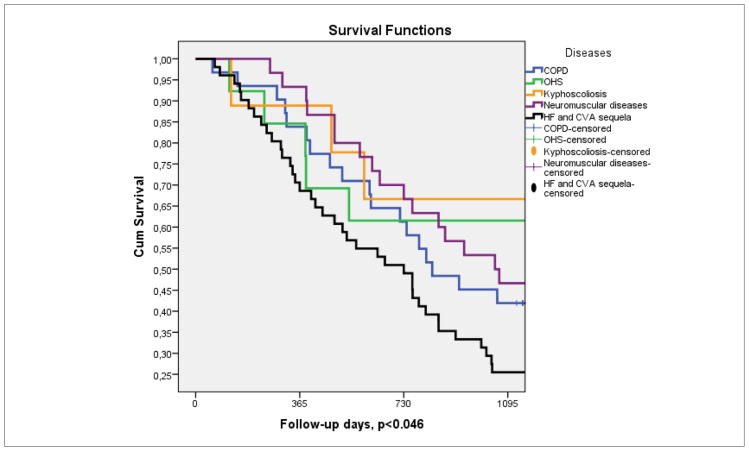
During the follow-up period, the 1-, 2-, and 3-year mortality rates were 19.4% (n=26), 41.8% (n=56), and 59.7% (n=80), respectively. Figure 2 shows the Kaplan–Meier survival curves of tracheostomized patients who had at least 3 years of follow-up with different diseases. Patients with HF and CVA sequela had the shortest survival functions in a 3-year period.
Figure 2.
Kaplan Meier Survival curves for all patients with different diseases in three year follow-up period
Table 2 summarizes the disease dispersion among patients aged below and above 65 years old. The majority of older patients with tracheostomy (≥65 years) had HF and cerebrovascular diseases sequela (32/71) and COPD (22/71). The majority of younger patients with tracheostomy (<65 years) had neuromuscular disease (24/63) and HF and cerebrovascular diseases sequela (19/63) (Table 2).
Table 2.
The comparison underlying tracheostomy indications in patients with long-term mechanical ventilation via tracheostomy of age above and below 65 years
| Diseases | Age <65 years (n=63) | Age ≥65 years (n=71) | p |
|---|---|---|---|
| COPD, n (row %) | 9 (29) | 22 (71) | <0.001 |
| OHS, n (row %) | 4 (31) | 9 (69) | |
| Kyphoscoliosis, n (row %) | 7 (78) | 2 (22) | |
| Neuromuscular disease, n (row %) | 24 (80) | 6 (20) | |
| HF and CVA, n (row %) | 19 (37) | 32 (63) |
COPD: chronic obstructive pulmonary disease; OHS: obesity hypoventilation syndrome; HF and CVA: heart failure and cerebrovascular disease
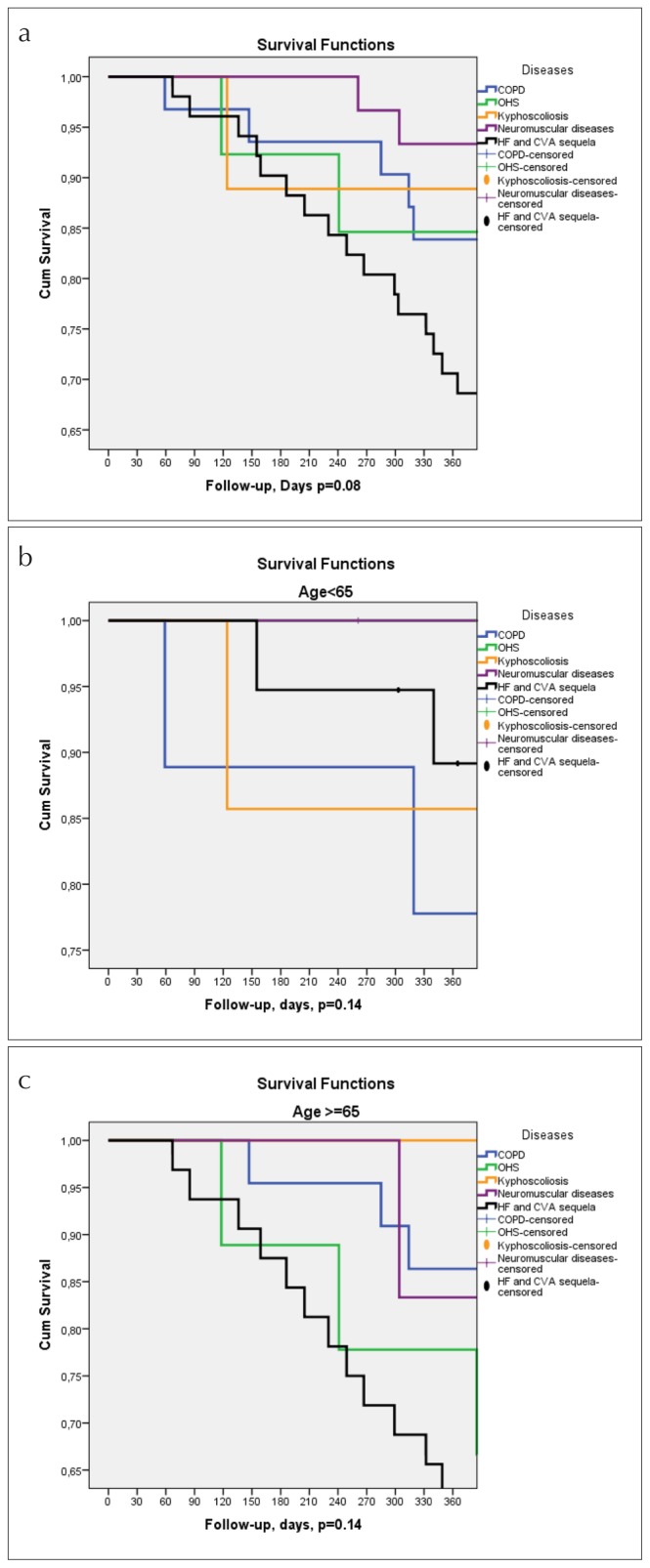
Figure 3a shows the 1-year survival of tracheostomized patients with different diseases in the 1-year follow-up period (Figure 3a). The 1-year period had similar survival among the diseases group (p=0.08). Patients were divided into subgroups according to age <65 years (Figure 3b) and >65 years (Figure 3c), and the Kaplan–Meier survival curves showed similar one survival.
Figure 3. a–c.
(a) Kaplan Meier Survival curves for all patients with different diseases in one year follow-up period. (b) Kaplan Meier Survival curves for patients under 65 age with different diseases in one year follow-up period. (c) Kaplan Meier Survival Curves for patients’ age 65 and above with different diseases in one year follow-up period
In Table 3, patients with tracheostomy who survived and died in the 3-year follow-up were compared in terms of age, gender, and tracheostomy indications. There was no difference between the two groups regarding patients’ gender. The mortality rate was statistically higher in patients with tracheostomy >65 years old than in younger patients (p=0.004). When evaluated according to the indications of tracheostomy, we found that mortality was highest in patients with HF–CVA sequela and COPD. The mortality rate was significantly lower in patients with neuromuscular disease. However, when mortality was examined according to all diseases, a statistical significance was found (p=0.037) (Table 3).
Table 3.
The comparisons of gender, age, and diseases according to mortality in the 3-year follow-up
| Variables | Survivor (n=54) | Non-survivor (n=80) | p |
|---|---|---|---|
| Male, n (%) | 31(57) | 55(69) | 0.18 |
| Age, n (%) | |||
| —≥65 years | 25(46) | 46 (58) | 0.20 |
| —≥75 years | 7(13) | 24(30) | 0.022 |
| —≥80 years | 4(7) | 11(14) | 0.25 |
| Diseases, n (row %) | |||
| —COPD | 13(42) | 18(58) | 0.037 |
| —Kyphoscoliosis | 6(67) | 3(33) | |
| —OHS | 8(62) | 5(39) | |
| —Neuromuscular disease | 14(47) | 16(53) | |
| —HF and CVA sequela | 13(26) | 38(75) | |
COPD: chronic obstructive pulmonary disease; OHS: obesity hypoventilation syndrome; HF and CVA: heart failure and cerebrovascular disease
Table 4 shows the 3-year mortality risk factors in patients with tracheostomy. Male gender and age >75 years and diseases (COPD, OHS, kyphoscoliosis, neuromuscular diseases, and HF with CVA) were included into the Cox regression model. Age >75 years and HF–CVA sequela significantly increased the 3-year mortality, and having COPD decreased mortality in 46%.
Table 4.
The long-term mortality risk analysis using Cox regression test for the 3-year follow-up in patients with tracheostomy
| HR | 95% CI for HR | p | ||
|---|---|---|---|---|
|
| ||||
| Lower | Upper | |||
| HF and CVA sequela | 1.84 | 1.03 | 3.29 | 0.041 |
| Age >75 years | 1.71 | 1.03 | 2.82 | 0.036 |
| COPD | 0.54 | 0.20 | 0.98 | 0.041 |
| OHS | 0.95 | 0.33 | 2.75 | 0.93 |
| Kyphoscoliosis | 0.66 | 0.19 | 2.28 | 0.51 |
| Neuromuscular diseases | 1.06 | 0.53 | 2.14 | 0.87 |
| Male gender | 1.54 | 0.93 | 2.56 | 0.10 |
HR: hazard ratio; CI: confidence interval; COPD: chronic obstructive pulmonary disease; OHS: obesity hypoventilation syndrome; HF and CVA: heart failure and cerebrovascular disease
DISCUSSION
In the present study, the most common tracheostomy indication in tracheostomy patients followed up at the RICU outpatient clinic was determined as HF–CVA sequela diseases due to prolonged mechanical ventilation. In the 1-year follow-up, patients with neuromuscular diseases were more fortunate than the rest, and we found that one-fourth of the deaths had occurred within the first year in patients who had undergone tracheostomy due to HF and CVA diseases and advanced COPD. Patients with HF and CVA diseases aged ≥75 years had increased mortality risk 1.8 and 1.7 times in the 3-year follow-up, respectively; however, there was no difference in mortality regarding gender.
The most frequent indication for tracheostomy has been reported as prolonged mechanical ventilation due to various diseases in the ICU [12]. Medical (respiratory, internal medicine, and neurologic ICU) and surgical ICU had different patients and had different reasons of tracheostomy [12–14]. In the study by Marchese et al. in a multicenter RICU (n=22 ICU centers), 719 tracheostomized ICU patients were included; among these patients, 34% COPD, 28% neuromuscular diseases, 24% with progressive deterioration of underlying comorbidities, 11% post-surgical patients, 4% thoracic dysmorphism, and 2% obstructive sleep apnea were found [13]. In the Turkish Tracheotomy Survey Group study conducted in 238 general ICUs (excluding pediatric and coronary ICUs), almost 75% of the indications for tracheostomy was prolonged mechanical ventilation. Other indications reported in that study were prolonged coma, need of airway protection, and aspiration [14]. In our study, the most common indications were prolonged mechanical ventilation due to HF–cerebrovascular diseases, followed by COPD and neuromuscular diseases. In a large meta-analysis, Damuth et al. [15] evaluated 124 studies for the outcomes of ICU patients with prolonged mechanical ventilations for ICU and long-term mortality. In their study, the 1-year mortality rate was 59%, and more than half of the patients with prolonged mechanical ventilation due to various reasons were found to be dead within 1 year. In the present study, the 1-year mortality rate was almost one-third of Damuth’s result, and our 3-year mortality rate was almost equal to Damuth’s 1-year mortality rate. Marchese et al. [13] showed that patients with neuromuscular diseases have statistically significant longer survival than those with pulmonary disease and found that the overall non-pulmonary patients have a longer survival trend than pulmonary patients. These findings were similar in the present study. The overall mortality rate in tracheostomized patients was 55% in a study from Turkey by Kırca et al. [16] They reported that the highest mortality rate is due to ischemic and hemorrhagic cerebral damage (22%), followed by acute or chronic pulmonary pathologies (15%), and the lowest mortality rate is found in neuromuscular diseases (0.2%). In our study, the best survival was found in patients with neuromuscular disease and kyphoscoliosis, and HF–CVA diseases that underwent tracheostomy due to prolonged mechanical ventilation had the worst outcomes in long-term survival.
A limitation of our study was the retrospective and single-centered design nature of the study. Nonetheless, it provides useful clinical information due to the large sample size and specific patient group. Only the time was taken into account in the survival of patients; we could not record any data about the quality of life of the patients and/or their caregivers, since it was not available in the medical files of the patients.
The underlying diseases that lead to tracheostomy should be the main determinant for long-term mortality risk. The most common indications for tracheostomy in the RICU were HF–cerebrovascular diseases due to prolonged mechanical ventilation and advanced COPD. In older patients (age ≥75 years), the mortality rate may increase 1.7-fold during the 3-year follow-up, whereas gender may not be different for long-term. Patients with neuromuscular diseases can benefit from tracheostomy in the long-term follow-up (1–3 years). However, the main concern about patients with neuromuscular diseases is the quality of life. According to our experience, the most important ‘ABC tracheostomy decision triangle’ consists of the patient’s request (A), family support (B), and tracheostomy indications (C) and may vary from country to country depending on the religious belief of subjects. The patient’s expectancy, quality of life, and support of caregivers are also issues to be investigated. Physicians can consider the best and worst outcomes of long-term tracheostomy decisions. Our findings may also be useful for healthcare providers and policy-makers to estimate the demand and health insurance cost.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Health Sciences University Süreyyapaşa Chest Diseases and Thoracic Surgery Training and Research Hospital (12.07.2018/048).
Informed Consent: Informed consent was not obtained from the patients due to the retrospective nature of the study design.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept –E.A., B.O.; Design –E.A., B.O.; Supervision –E.A., B.O.; Resources –B.O., E.A.; Materials –B.O., E.A.; Data Collection and/or Processing –B.O., E.A.; Analysis and/or Interpretation –E.A., B.O.; Literature Search –E.A., B.O.; Writing Manuscript –E.A., B.O.; Critical Review –E.A., B.O.; Other – E.A.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Carson SS. Outcomes of prolonged mechanical ventilation. Curr Opin Crit Care. 2006;12:405–11. doi: 10.1097/01.ccx.0000244118.08753.dc. [DOI] [PubMed] [Google Scholar]
- 2.Ambrosino N, Vitacca M. The patient needing prolonged mechanical ventilation: a narrative review. Multidiscip Respir Med. 2018;13:6. doi: 10.1186/s40248-018-0118-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trouillet JL, Collange O, Belafia F, et al. Tracheotomy in the intensive care unit: Guidelines from a French expert panel: The French Intensive Care Society and the French Society of Anaesthesia and Intensive Care Medicine. Anaesth Crit Care Pain Med. 2018;37:281–94. doi: 10.1016/j.accpm.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 4.Kollef MH, Ahrens TS, Shannon W. Clinical predictors and outcomes for patients requiring tracheostomy in the intensive care unit. Crit Care Med. 1999;27:1714–20. doi: 10.1097/00003246-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Restrepo R, Kahn D, Patel P, et al. One Year Mortality Rates of Tracheostomy Cases: Life after the Knife. J Emerg Med Trauma Surg Care. 2015;2:006. [Google Scholar]
- 6.Alabi BS, Afolabi OA, Dunmade AD, et al. Indications and outcome of tracheostomy in Ilorin, North Central Nigeria: 10 years review. Ann Afr Med. 2018;17:1–6. doi: 10.4103/aam.aam_130_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD (updated 2017) Available from: http://www.goldcopd.org.
- 8.Olson AL, Zwillich C. The obesity hypoventilation syndrome. Am J Med. 2005;118:948–56. doi: 10.1016/j.amjmed.2005.03.042. [DOI] [PubMed] [Google Scholar]
- 9.Lloyd-Owen SJ, Donaldson GC, Ambrosino N, et al. Patterns of home mechanical ventilation use in Europe: results from the Eurovent survey. Eur Respir J. 2005;25:1025–31. doi: 10.1183/09031936.05.00066704. [DOI] [PubMed] [Google Scholar]
- 10.Karakurt Z. Evde mekanik ventilasyon. Yoğun Bakım Dergisi. 2004;4:145–50. [Google Scholar]
- 11.MacIntyre NR, Epstein SK, Carson S, et al. Management of patients requiring prolonged mechanical ventilations: report of a NAMDRC concensus conference. Chest. 2005;128:3937–54. doi: 10.1378/chest.128.6.3937. [DOI] [PubMed] [Google Scholar]
- 12.MacIntyre NR, Cook DJ, Ely EW, Jr, et al. American College of Chest Physicians; American Association for Respiratory Care; American College of Critical Care Medicine. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest. 2001;120(6 Suppl):375S–95S. doi: 10.1378/chest.120.6_suppl.375S. [DOI] [PubMed] [Google Scholar]
- 13.Marchese S, Lo Coco D, Lo Coco A. Outcome and attitudes toward home tracheostomy ventilation of consecutive patients: a 10-year experience. Respir Med. 2008;102:430–6. doi: 10.1016/j.rmed.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 14.Gucyetmez B, Atalan HK, Cakar N Turkish Tracheotomy Survey Group. Elective tracheotomy practices in Turkey. PLoS One. 2016;11:e0166097. doi: 10.1371/journal.pone.0166097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Damuth E, Mitchell JA, Bartock JL, et al. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med. 2015;3:544–53. doi: 10.1016/S2213-2600(15)00150-2. [DOI] [PubMed] [Google Scholar]
- 16.Kırca H, Çakın Ö, Cengiz M, et al. Tracheotomy in the Intensive Care Unit: Indications, Complications and Prognosis. J Turk Soc Intens Care. 2018;16:17–25. doi: 10.4274/tybd.03064. [DOI] [Google Scholar]