Abstract
Objectives
Antipsychotics are used to manage the behavioral and psychological symptoms of dementia (BPSD), despite their association with greater risks for mortality and cerebrovascular events. Previous studies in Japan have estimated the prevalence of antipsychotics among older adults who took antidementia drugs. Using long‐term care (LTC) data, we aimed to obtain more accurate estimates of the prevalence of antipsychotics and to determine factors related to their use in older adults with dementia.
Methods
Medical and LTC claims data and LTC certification data between April 2012 and September 2013 were obtained from a middle‐sized suburban city. The 1‐year prevalence of antipsychotic use was estimated among individuals with probable dementia aged greater than or equal to 75 years who were prescribed antidementia drugs and/or had dementia based on LTC needs certification data.
Results
Of 25 919 participants, 4865 had probable dementia and 1506 were prescribed antidementia drugs. The prevalence of antipsychotics among participants with probable dementia was 10.7%, which was lower than that in those who were prescribed antidementia drugs (16.4%). Among participants with probable dementia with LTC certification data available (N = 4419), lower cognitive function (vs mild; adjusted odds ratio 2.16, 95% confidence interval 1.63‐2.86), antidementia drug use (2.27, 1.84‐2.81), and institutional LTC services use (2.34, 1.85‐2.97) were associated with greater odds of antipsychotic use, whereas older age (greater than or equal to 92 years) was associated with lower odds (vs less than 77 years; 0.42, 0.27‐0.65).
Conclusions
These findings may be useful for estimating the burden of BPSD and for taking measures to reduce inappropriate antipsychotic prescription.
Keywords: behavioral and psychological symptoms of dementia, antipsychotics, dementia, long‐term care
Key points.
Previous studies in Japan determined the prevalence of antipsychotics among individuals prescribed antidementia drugs because of the unavailability of reliable data.
Use of long‐term care data enabled us to obtain more accurate estimates of the prevalence of antipsychotic use in older adults with dementia.
The new population‐based estimate of the prevalence of antipsychotics (10.7%) was lower than that estimated among people prescribed antidementia drugs (16.4%).
Younger age, institutional LTC services use, antidementia drug use, and lower cognitive function were associated with greater odds of antipsychotic use.
1. INTRODUCTION
Japan has the greatest number of people with dementia among the Organisation for Economic Co‐operation and Development countries.1 This number is projected to increase markedly in the near future, reaching almost one‐fifth of the population2 over 65 years in 2025. This could impose considerable financial and social burdens on both the health care system and society.
One of the major challenges of caring for people with dementia is managing the behavioral and psychological symptoms of dementia (BPSD).3 Antipsychotics have been used for BPSD management, despite off‐label use.4 Indeed, antipsychotics are associated with greater risks for mortality and cerebrovascular events, which has led regulatory agencies to issue warnings or required pharmaceutical companies to add precautions about the use of antipsychotics for people with dementia.4, 5, 6, 7 However, antipsychotics have still been commonly prescribed in older adults with dementia in Japan8, 9, 10 and in overseas countries,11, 12 even after the issue of such warnings or precautions.
There have been several studies on the use of antipsychotics in older people with dementia in Japan. Based on analyses of large‐scale medical claims data, the prevalence of antipsychotic use among people prescribed antidementia drugs8, 9, 10 ranged from 16.8% to 24.9%. These studies limited their study cohort to those prescribed antidementia drugs partly because a diagnosis of dementia in medical claims is not considered reliable. However, the generalizability of such estimates is limited because people with dementia do not always take antidementia drugs. In fact, the indication for antidementia drugs is generally limited to Alzheimer dementia, with the exception of donepezil, which has been also approved for dementia with Lewy bodies in Japan. Moreover, antidementia drugs are not always prescribed for older adults with dementia for efficacy and safety reasons.13
Since 2000, Japan has implemented a long‐term care (LTC) insurance system that is separate from the medical insurance system.14 To become beneficiaries of LTC insurance, individuals must have their LTC needs certified through a standardized process involving an assessment of physical and cognitive functions.15 Lowered cognitive function determined through this process is potentially more clinically relevant than those diagnoses listed in medical claims data16; accordingly, LTC needs certification data might be better able to identify older people with dementia and cognitive decline.
The main objective of this study was to provide a potentially more accurate estimate of the prevalence of antipsychotic use among older adults with dementia, irrespective of whether they have been prescribed antidementia drugs, using medical and LTC data in Japan. As the medical and LTC data can be linked, we are able to identify people with dementia, regardless of whether they are being treated with antidementia drugs. The secondary objective was to determine the factors associated with antipsychotic use in older people with dementia using the LTC certification data.
2. MATERIALS AND METHODS
2.1. Data sources
Medical and LTC claims data and LTC certification data over 18 months (April 2012 to September 2013) were obtained from a middle‐sized suburban city in the Tokyo metropolitan area of Japan. Before they were obtained, all data were anonymized; however, unique identification numbers were assigned to each person to enable matching between the medical and LTC data. During the anonymization process, birth year was approximated by converting it to a 5‐year range (eg, people born between 1930 and 1934 would be 77‐81 years of age as of January 1, 2012). This study was approved by the Ethics Committee of the University of Tsukuba.
2.2. Study participants
Figure 1 presents a flow chart of participant selection. People eligible for the Late Elders' Health Insurance system at entry were included (N = 37 998). This system provides medical insurance to all residents over 75 years as well as those aged 65 to 74 years with disabilities. We attempted to simplify the dataset to those over 75; however, we were not able to exclude people aged 72 to 74 years who were eligible for the Late Elders' Health Insurance system because the birth year data were available only in 5‐year ranges. Based on the national statistics, people aged 72 to 74 years with the Late Elders' Health Insurance were estimated to account for less than 1% of the category of those aged 72 to 76 years in this study. Because the data did not include participants' insurance eligibility information, including information about their deaths, we selected participants with 12 or more months of data, based on the first and last claims records. To obtain the 1‐year prevalence of antipsychotic use for comparability with previous studies,8, 9, 10 we used the first 12 months of data for our analyses. We also excluded participants who stayed in hospitals or specific types of LTC facilities using bundled payment schemes for more than 6 months in total as their prescription data during their stay there would be unavailable. We could not obtain claims data on medical services for individuals covered by public assistance, so these individuals were not included in the study.
Figure 1.
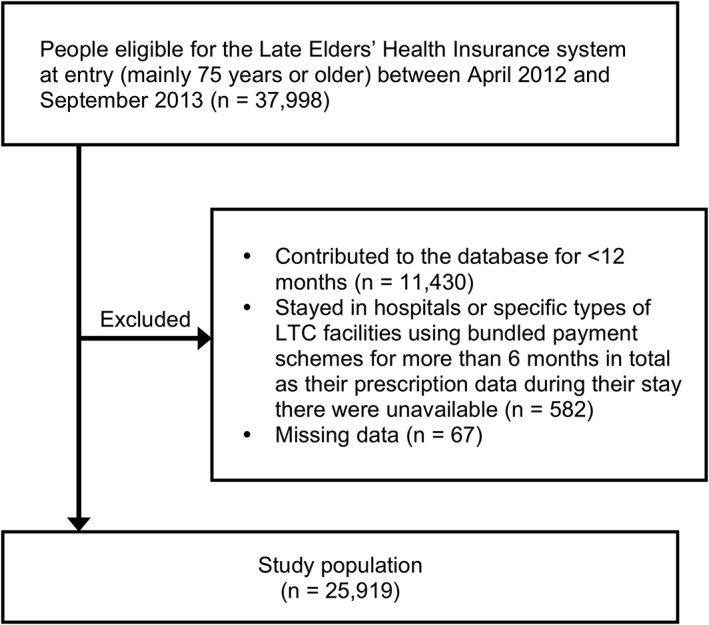
Flow diagram for participant selection. Probable dementia is defined as antidementia drug users and those with rank I or greater on the “Independence Degree of Daily Living for the Dementia.” LTC, long‐term care
We analyzed the following three cohorts based on our study aims (Figure 2).
Probable dementia (novel cohort identification): This group included both antidementia drug users and those with rank I or greater on the “Independence Degree of Daily Living for the Demented,” a measure used in the process of LTC needs certification.16, 17
Antidementia drug users (conventional cohort identification): These were participants who were prescribed antidementia drugs. We evaluated this cohort to enable a comparison with previous studies.8, 9, 10
Probable dementia with LTC needs certification data: This group was a subset of the probable dementia cohort defined above for evaluation of associations of factors, including physical and cognitive function, with antipsychotic use. Therefore, in this group, participants that were identified as having probable dementia based on antidementia drug prescription but had not been certified for their LTC needs were excluded.
Figure 2.
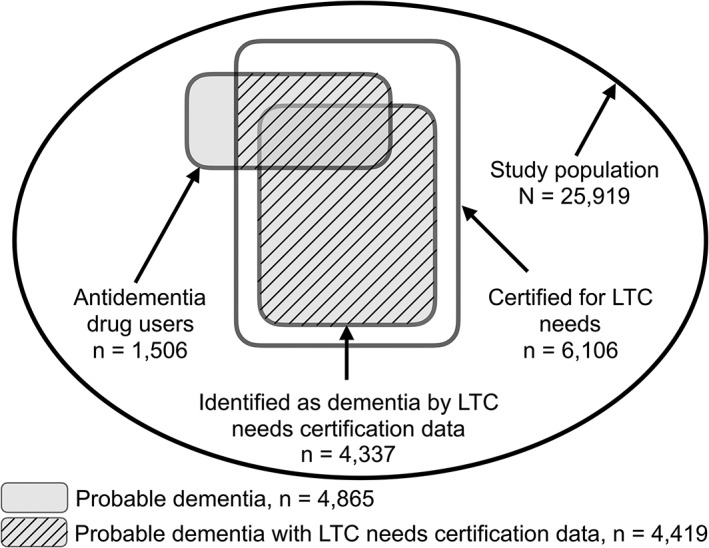
Illustration of the study cohorts. LTC, long‐term care
2.3. Antipsychotic and antidementia drugs
We included both typical and atypical antipsychotic drugs being marketed in Japan during the study period. The typical antipsychotics included bromperidol, carpipramine, chlorpromazine, clocapramine, fluphenazine, haloperidol, levomepromazine, mosapramine, nemonapride, oxypertine, perphenazine, pimozide, pipamperone, prochlorperazine, propericiazine, spiperone, sulpiride, sultopride, timiperone, trifluoperazine, and zotepine. The atypical antipsychotics included aripiprazole, blonanserin, clozapine, olanzapine, paliperidone, perospirone, quetiapine, and risperidone. As a sensitivity analysis, we repeated the analyses while excluding prochlorperazine and sulpiride, as the former is generally used as an antiemetic and the latter for gastric discomfort in Japan.
We included all four antidementia drugs to identify antidementia drug users: donepezil, rivastigmine, galantamine, and memantine. Participants who had at least one outpatient prescription of any of these antidementia drugs during the 12‐month study period were defined as antidementia drug users.
2.4. Physical and cognitive function
Activities of daily living associated with dementia and physical disability were only available for participants who had LTC needs certification data. The primary goal of LTC needs certification is to determine both eligibility and individuals' care needs level (which falls into seven grades) based on assessment of physical and cognitive functions; it is usually reassessed once every 12 or 24 months. The assessment procedures are standardized nationwide and involve interviews with the older adult in question and their primary caregiver, as well as a primary care physician's opinion. In this study, the most recent physical and cognitive functions data prior to the study entry were considered.
For cognitive disability, we used the “Independence Degree of Daily Living for the Demented.”17 This measure was validated for identifying people aged greater than or equal to 65 years with dementia in the community with reference to a diagnosis of dementia made by neuropsychiatrists as the gold standard.16 When people without LTC certification were categorized into those without dementia, the cut‐off of rank I on this measure had a 65% sensitivity and a 93% specificity. For people who received LTC services, the validity of this method was improved (83% sensitivity and 92% specificity).16 It was also reported that most people aged greater than or equal to 65 years with dementia (~80%) had applied for LTC needs certification.16 We deemed individuals with rank I (almost independent daily living is possible despite having some type of dementia) or greater as having probable dementia. More specifically, individuals were grouped into mild (rank I), moderate (rank II; independent daily life is possible under observation despite daily life‐disturbing symptoms, behaviors, and problems with communication), or severe (rank III, requiring assistance; rank IV, requiring assistance frequently; or rank M, marked psychiatric symptoms requiring expert management) cognitive disability.
Physical disability was determined according to the scale of “Independence Degree of Daily Living for the Disabled Elderly” (Independent, J1/J2, A1/A2, B1/B2, and C1/C2).17 In this study, these ratings were categorized into “not bedridden” (Independent, J1/J2, and A1/A2) and “bedridden” (B1/B2 and C1/C2).
2.5. Analysis
The demographics of the study participants were described. The main outcome measure was the prevalence of at least one outpatient prescription of an antipsychotic over the 12‐month study period. The prevalence of antipsychotic use was estimated for each study cohort defined above.
We also evaluated the associations of age, gender, antidementia drug use, residential status, hospitalization, and cognitive and physical disability with antipsychotic use among participants with probable dementia whose LTC needs certification data were available. A logistic regression analysis, assessing crude and adjusted odds ratios and 95% confidence intervals, was used for this purpose. Residential status was derived from the LTC claims data. Participants who had at least one claim for institutional LTC services use, including use of one of the three designated types of LTC facilities18 and other types of facilities or group homes for older people during the 12‐month study period, were categorized as LTC facility users. Hospitalization was derived from the medical claims data; participants who had at least one claim for inpatient treatment during the study period were categorized as people who had experienced hospitalization.
As a sensitivity analysis, we repeated the analysis of the 6‐month prevalence of antipsychotics in those who had at least 6 months of follow‐up. All analyses were performed using Stata version 14 (Stata Corp., College Station, Texas).
3. RESULTS
This study included 25 919 participants, among which a quarter were LTC beneficiaries (n = 6106). Participants with probable dementia and antidementia drug users accounted for 18.8% (n = 4865) and 5.8% (n = 1506), respectively, of the overall sample. When participants with probable dementia were first identified by the use of antidementia drugs (n = 1506; 31.0%), LTC data contributed to identifying an additional 3359 participants (69.0%). Conversely, when LTC data were first used to identify participants with probable dementia (n = 4337; 89.1%), the use of antidementia drugs contributed to identifying an additional 528 participants (10.9%).
The characteristics of people with probable dementia and antidementia drug users, and their proportions of the study population, are shown in Table 1. The proportion of people with probable dementia increased with age, ranging from 7% to 70%; the proportion of antidementia drug users ranged from 3% to 12% according to age. The difference in proportion between these two cohorts increased with age.
Table 1.
Characteristics of the study participants
| Participants With Probable Dementia | Antidementia Drug Users | All Participants | Participants Identified As: | |||||
|---|---|---|---|---|---|---|---|---|
| n = 4865 | n = 1506 | N = 25 919 | ||||||
| n | % | n | % | n | % | Having Probable Dementia, % | Antidementia Drug Users, % | |
| Age, years | ||||||||
| 72‐76a | 580 | 11.9 | 196 | 13.0 | 7812 | 30.1 | 7.4 | 2.5 |
| 77‐81 | 1198 | 24.6 | 475 | 31.5 | 9647 | 37.2 | 12.4 | 4.9 |
| 82‐86 | 1394 | 28.7 | 488 | 32.4 | 5294 | 20.4 | 26.3 | 9.2 |
| 87‐91 | 1117 | 23.0 | 278 | 18.5 | 2328 | 9.0 | 48.0 | 11.9 |
| ≥92 | 576 | 11.8 | 69 | 4.6 | 838 | 3.2 | 68.7 | 8.2 |
| Sex | ||||||||
| Male | 1400 | 28.8 | 459 | 30.5 | 10 684 | 41.2 | 13.1 | 4.3 |
| Female | 3465 | 71.2 | 1,047 | 69.5 | 15 235 | 58.8 | 22.7 | 6.9 |
| Antidementia drugs | ||||||||
| No | 3359 | 69.0 | NA | NA | 24 413 | 94.2 | 13.8 | NA |
| Yes | 1506 | 31.0 | 1506 | 100.0 | 1506 | 5.8 | 100.0 | 100.0 |
| Hospitalization | ||||||||
| No | 3961 | 81.4 | 1,285 | 85.3 | 22 746 | 87.8 | 17.4 | 5.6 |
| Yes | 904 | 18.6 | 221 | 14.7 | 3173 | 12.2 | 28.5 | 7.0 |
| LTC needs certification | ||||||||
| No | 446 | 9.2 | 446 | 29.6 | 19 813 | 76.4 | 2.3 | 2.3 |
| Yes | 4419 | 90.8 | 1060 | 70.4 | 6106 | 23.6 | 72.4 | 17.4 |
Abbreviation: LTC, long‐term care.
People <75 were included only if eligible for the Late Elders' Health Insurance system.
Table 2 shows the prevalence of antipsychotic use according to age group, sex, and LTC certification status. The prevalence of antipsychotic use was 10.7% among participants with probable dementia, 16.4% among antidementia drug users, 2.1% among participants without probable dementia, and 3.8% for the entire study population. In the sensitivity analysis that excluded prochlorperazine and sulpiride, the corresponding prevalence proportions were 9.1%, 14.8%, 0.7%, and 2.3%, respectively (Table S1). Among antidementia drug users, atypical antipsychotics were more commonly used, whereas typical antipsychotics were slightly more commonly used among participants with probable dementia (Table 2). When prochlorperazine and sulpiride were excluded, atypical antipsychotics were more commonly used among all three cohorts (Table S1). The 6‐month prevalence of antipsychotic use (N = 31 353) was 9.1% among participants with probable dementia, 14.9% among antidementia drug users, 1.8% among participants without probable dementia, and 3.1% for the entire study population.
Table 2.
One‐year prevalent users of antipsychotics according to dementia status and the characteristics of the study participants
| Participants With Probable Dementia | Antidementia Drug Users | Participants With Probable Dementia With LTC Certification Data Available | Participants Without Probable Dementia | All Participants | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n = 4865 | n = 1506 | n = 4419 | n = 21 054 | N = 25 919 | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| All | 520/4865 | 10.7 | 247/1506 | 16.4 | 478/4419 | 10.8 | 452/21 054 | 2.1 | 972/25,919 | 3.8 |
| Age, years | ||||||||||
| 72‐76a | 71/580 | 12.2 | 33/196 | 16.8 | 59/486 | 12.1 | 148/7232 | 2.0 | 219/7812 | 2.8 |
| 77‐81 | 149/1198 | 12.4 | 72/475 | 15.2 | 138/1015 | 13.6 | 196/8449 | 2.3 | 345/9647 | 3.6 |
| 82‐86 | 154/1394 | 11.1 | 87/488 | 17.8 | 141/1272 | 11.1 | 76/3900 | 1.9 | 230/5294 | 4.3 |
| 87‐91 | 106/1117 | 9.5 | 47/278 | 16.9 | 102/1076 | 9.5 | 30/1211 | 2.5 | 136/2328 | 5.8 |
| ≥92 | 40/576 | 6.9 | 8/69 | 11.6 | 38/570 | 6.7 | 2/262 | 0.8 | 42/838 | 5.0 |
| Sex | ||||||||||
| Male | 133/1400 | 9.5 | 68/459 | 14.8 | 119/1209 | 9.8 | 139/9284 | 1.5 | 272/10 684 | 2.6 |
| Female | 387/3465 | 11.2 | 179/1047 | 17.1 | 359/3210 | 11.2 | 313/11 770 | 2.7 | 700/15 235 | 4.6 |
| LTC needs certification | ||||||||||
| No | 42/446 | 9.4 | 42/446 | 9.4 | NA | NA | 403/19 367 | 2.1 | 445/19 813 | 2.3 |
| Yes | 478/4,419 | 10.8 | 205/1,060 | 19.3 | NA | NA | 49/1687 | 2.9 | 527/6106 | 8.6 |
| By type of antipsychotics | ||||||||||
| Atypical | 227/4865 | 4.7 | 120/1506 | 8.0 | 207/4419 | 4.7 | 72/21 054 | 0.3 | 299/25 919 | 1.2 |
| Typical | 243/4865 | 5.0 | 101/1506 | 6.7 | 225/4419 | 5.1 | 354/21 054 | 1.7 | 597/25 919 | 2.3 |
| Bothb | 50/4865 | 1.0 | 26/1506 | 1.7 | 46/4419 | 1.1 | 26/21 054 | 0.1 | 76/25 919 | 0.3 |
Abbreviation: LTC, long‐term care.
People <75 were included only if eligible for the Late Elders' Health Insurance system.
Concurrent or sequential use during the study period.
Among participants with probable dementia with LTC certification data available (n = 4419; 90.8% of those with probable dementia), there were slightly more people with moderate and severe cognitive disabilities than there were those with mild cognitive disability (Table 3). Furthermore, 1.5% (n = 66) were in rank M (marked psychiatric status) at the time of LTC needs assessment.
Table 3.
Associations of participant characteristics with antipsychotic use among participants with probable dementia with LTC certification data available (n = 4419)
| Crude | Adjusted | |||||||
|---|---|---|---|---|---|---|---|---|
| N | % | Odds Ratio | 95% CI | P | Odds Ratio | 95% CI | P | |
| Age, years | ||||||||
| 72‐76a | 486 | 11.0 | Reference | Reference | ||||
| 77‐81 | 1015 | 23.0 | 1.14 | 0.82‐1.58 | 0.435 | 1.03 | 0.73‐1.44 | 0.872 |
| 82‐86 | 1,272 | 28.8 | 0.90 | 0.65‐1.25 | 0.533 | 0.74 | 0.53‐1.04 | 0.080 |
| 87‐91 | 1,076 | 24.3 | 0.76 | 0.54‐1.06 | 0.110 | 0.62 | 0.43‐0.88 | 0.008 |
| ≥92 | 570 | 12.9 | 0.52 | 0.34‐0.79 | 0.002 | 0.42 | 0.27‐0.65 | <0.001 |
| Sex | ||||||||
| Male | 1,209 | 27.4 | Reference | Reference | ||||
| Female | 3,210 | 72.6 | 1.15 | 0.93‐1.44 | 0.201 | 1.18 | 0.94‐1.49 | 0.154 |
| Institutional LTC services use | ||||||||
| No | 3,749 | 84.8 | Reference | Reference | ||||
| Yes | 670 | 15.2 | 2.57 | 2.07‐3.20 | <0.001 | 2.34 | 1.85‐2.97 | <0.001 |
| Antidementia drug use | ||||||||
| No | 3,359 | 76.0 | Reference | Reference | ||||
| Yes | 1,060 | 24.0 | 2.71 | 2.23‐3.30 | <0.001 | 2.27 | 1.84‐2.81 | <0.001 |
| Hospitalization | ||||||||
| No | 3,569 | 80.8 | Reference | Reference | ||||
| Yes | 850 | 19.2 | 1.00 | 0.79‐1.27 | 0.994 | 1.03 | 0.80‐1.33 | 0.803 |
| Cognitive disability | ||||||||
| Mild | 1,288 | 29.2 | Reference | Reference | ||||
| Moderate | 1,628 | 36.8 | 1.50 | 1.14‐1.97 | 0.004 | 1.34 | 1.01‐1.77 | 0.045 |
| Severe | 1,503 | 34.0 | 2.72 | 2.10‐3.53 | <0.001 | 2.16 | 1.63‐2.86 | <0.001 |
| Physical disability | ||||||||
| Not bedridden | 3,114 | 70.5 | Reference | Reference | ||||
| Bedridden | 1,305 | 29.5 | 1.03 | 0.84‐1.27 | 0.763 | 0.93 | 0.74‐1.17 | 0.541 |
Abbreviation: LTC, long‐term care.
People <75 were included only if eligible for the Late Elders' Health Insurance system.
A multivariate logistic regression analysis revealed that severe (vs mild; adjusted odds ratio 2.16, 95% confidence interval 1.63‐2.86, P < 0.001) and moderate cognitive disability (1.34, 1.01‐1.77, P = 0.045), antidementia drug use (vs nonuse; 2.27, 1.84‐2.81, P < 0.001), and institutional LTC services use (vs nonuse; 2.34, 1.85‐2.97, P < 0.001) were associated with greater odds of antipsychotic use. By contrast, older age, including 87 to 91 years (0.62, 0.43‐0.88, P < 0.01) or greater than or equal to 92 years (0.42, 0.27‐0.65, P < 0.001), was associated with lower odds of using antipsychotics when compared with the lowest age group (less than 77 years) (Table 3).
4. DISCUSSION
By applying a comprehensive approach to dementia identification, we demonstrated that the prevalence of antipsychotic use among people with probable dementia in Japan was 10.7%. This is the first estimate of the prevalence of antipsychotic use among a large population of people with dementia that is not limited to antidementia drug users in Japan. The estimated prevalence of antipsychotic use is comparable with that in France (10.2%) but higher compared with that found in the United Kingdom (7.4%) and lower than that in the United States (14.9%), respectively.19, 20, 21
This new prevalence estimate is lower than that derived from antidementia drug users only. A previous study using a nationally representative medical claims database in Japan revealed that the prevalence of antipsychotics among people taking donepezil was about 25% (N = 15 591) and demonstrated a slightly increasing trend8 between 2002 and 2010. More recently, the prevalence of antipsychotic use among antidementia drug users after three further antidementia drugs began being marketed in Japan was determined to be 18.9% (N = 75 011) and 16.8% (N = 45 437); these latter two estimates were similar to our own among antidementia drug users (16.4%).9, 10 We also confirm a previously reported shift from typical to atypical antipsychotic use in older people with dementia in Japan.8
Possible reasons for the decreased prevalence of antipsychotic use among antidementia drug users in more recent studies are the accumulated evidence of the adverse effects of antipsychotic use in people with dementia4 and the corresponding safety warnings issued by the Japanese regulatory authority7 in 2009. Another possible reason is the increased use of memantine since its introduction9 in 2011. Although controversy remains about whether memantine has a beneficial effect on BPSD,22 previous observational studies imply that initiation of memantine reduces the consumption of psychotropics23 and antipsychotics.24 More recently, the “Primary Care Physicians' Guideline of Psychotropic Use for BPSD” was published in 2013. This guideline may contribute to reducing antipsychotics use, and further studies are needed to evaluate the use of antipsychotics for BPSD with more recent data.
We found that antipsychotic use was associated with younger age, greater cognitive disability, use of antidementia drugs, and use of institutional LTC services. The observed dose‐response relationship between cognitive disability and antipsychotic use suggests that antipsychotic prescription is partly explained by BPSD itself. Excessive use of antipsychotics in nursing homes has been an important issue internationally.25, 26, 27 The observed association of institutional LTC services use with greater antipsychotic use in the present study may suggest that nursing home residence might be conductive to antipsychotic use in Japan. The development of nonpharmacological BPSD management and antipsychotic withdrawal techniques feasible for use are strongly desired. In addition, future studies might examine the possible influence of antidementia drug prescriptions on the subsequent course of BPSD and antipsychotic prescriptions.
The strength of this new approach is that it offers greater sensitivity for identifying people with dementia in the population compared with the conventional method using medical claims data only. Antidementia drug users accounted for only 30% of people with probable dementia, suggesting that the majority of people with dementia could not have been identified in previous studies.8, 9, 10 The age‐stratified prevalence of probable dementia in our study was similar to that identified using the Diagnostic and Statistical Manual of Mental Disorders, Third Edition‐revised (DSM‐III‐R)28 in the latest epidemiological study in Japan.29 Moreover, the prevalence of antipsychotic use other than prochlorperazine and sulpiride in participants without probable dementia was similar to the prevalence of schizophrenia among individuals aged over 70 years in Japan (male 0.4%, female 0.6%).30 This suggests that the new method almost completely succeeded in identifying participants with dementia receiving antipsychotics.
However, there are several limitations in this study. First, we could not determine whether the antipsychotics were prescribed to relieve BPSD or not because of their off‐label use. Some antipsychotics could have been used for the treatment of bipolar disorder or, despite their off‐label use, for delirium or depression. Second, we did not evaluate the validity of the classification of dementia using the gold standard in our study population. While our approach could have effectively identified the majority of people with dementia, some people with dementia who did not receive antidementia drugs during the study period or did not apply for LTC needs certification could not be identified. Because people with dementia but who do not take antidementia drugs or have LTC needs certification are the least likely to receive antipsychotics, our numbers on the prevalence of antipsychotic use might be slightly overestimated. Third, we did not include individuals censored within 12 months after their entry (eg, died) or who had neither medical nor LTC services use during the study period. Fourth, we should be careful about generalizing our results, as they are based on the residents of a single city. For example, based on the association of institutional LTC services use with antipsychotic use, the prevalence of antipsychotic use may vary by region according to the availability of institutional LTC facilities. However, the prescribing of antipsychotics for BPSD in our study population is not considered to be very different from that in the entire Japanese population because the prevalence of antipsychotic use among antidementia drug users was similar to that reported in previous studies with nationwide samples.9, 10 Fifth, causal relationships between the identified factors and antipsychotic use cannot be established because of our cross‐sectional design and 1‐year time window. Finally, we did not know the precise health status of each individual when they were issued the antipsychotic prescription because there were time differences between this prescription and their assessment of cognitive and physical function for the LTC needs certification.
In conclusion, we have provided a comprehensive population‐based estimate of the prevalence of antipsychotic use and its related factors among older people with dementia in Japan. This potentially more accurate estimation of the prevalence of antipsychotic use may be useful for policymakers in estimating the burden of BPSD and in taking measures to reduce inappropriate antipsychotic prescription in older adults with dementia.
CONFLICT OF INTEREST
None declared.
Supporting information
Table S1 One‐year prevalent users of antipsychotics excluding sulpiride and prochlorperazine according to dementia status and the characteristics of the study participants
ACKNOWLEDGEMENT
This work was supported by Japan Agency for Medical Research and Development (grant number JP18dk0110026h0002).
Kuroda N, Hamada S, Sakata N, et al. Antipsychotic use and related factors among people with dementia aged 75 years or older in Japan: A comprehensive population‐based estimation using medical and long‐term care data. Int J Geriatr Psychiatry. 2019;34:472–479. 10.1002/gps.5041
REFERENCES
- 1. OECD . Health at a Glance 2017: OECD indicators, OECD Publishing, Paris 10.1787/health_glance-2017-en. Accessed June 27, 2018. [DOI]
- 2. Montgomery W, Ueda K, Jorgensen M, Stathis S, Cheng Y, Nakamura T. Epidemiology, associated burden, and current clinical practice for the diagnosis and management of Alzheimer's disease in Japan. Clinicoecon Outcomes Res. 2017;10:13‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Feast A, Moniz‐Cook E, Stoner C, Charlesworth G, Orrell M. A systematic review of the relationship between behavioral and psychological symptoms (BPSD) and caregiver well‐being. Int Psychogeriatr. 2016;28(11):1761‐1774. [DOI] [PubMed] [Google Scholar]
- 4. Tampi RR, Tampi DJ, Balachandran S, Srinivasan S. Antipsychotic use in dementia: a systematic review of benefits and risks from meta‐analyses. Ther Adv Chronic Dis. 2016;7(5):229‐245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. US Food and Drug Administration . FDA public health advisory: death with antipsychotics in elderly patients with behavioral disturbances. http://psychrights.org/drugs/FDAantipsychotics4elderlywarning.htm. Published April 11, 2005. Accessed June 23, 2018.
- 6. Wang PS, Schneeweiss S, Avorn J, et al. Risk of death in elderly users of conventional vs. atypical antipsychotic medications. N Engl J Med. 2005;353(22):2335‐2341. [DOI] [PubMed] [Google Scholar]
- 7. Pharmaceutical and Food Safety Bureau, Ministry of Health , Labour and Welfare. MHLW Pharmaceuticals and medical devices safety information (FY2009). https://www.pmda.go.jp/files/000153593.pdf. Published 2009. Accessed June 23, 2018.
- 8. Okumura Y, Togo T, Fujita J. Trends in use of psychotropic medications among patients treated with cholinesterase inhibitors in Japan from 2002 to 2010. Int Psychogeriatr. 2015;27(3):407‐415. [DOI] [PubMed] [Google Scholar]
- 9. Kadohara K, Sato I, Doi Y, et al. Prescription patterns of medications for Alzheimer's disease in Japan from 2010 to 2015: a descriptive pharmacy claims database study. Neurol Ther. 2017;6(1):25‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Murata M, Muto M, Ikeda S. Survey of psychotropic drug usage for dementia using a prescription database. Jpn J Pharmacoepidemiol. 2014;19(2):81‐89. [Google Scholar]
- 11. Sultana J, Fontana A, Giorgianni F, et al. The effect of safety warnings on antipsychotic drug prescribing in elderly persons with dementia in the United Kingdom and Italy: a population‐based study. CNS Drugs. 2016;30(11):1097‐1109. [DOI] [PubMed] [Google Scholar]
- 12. Schulze J, van den Bussche H, Glaeske G, Kaduszkiewicz H, Wiese B, Hoffmann F. Impact of safety warnings on antipsychotic prescriptions in dementia: nothing has changed but the years and the substances. Eur Neuropsychopharmacol. 2013;23(9):1034‐1042. [DOI] [PubMed] [Google Scholar]
- 13. Hashimoto M, Yatabe Y, Ishikawa T, et al. Relationship between dementia severity and behavioral and psychological symptoms of dementia in dementia with Lewy bodies and Alzheimer's disease patients. Dement Geriatr Cogn Disord Extra. 2015;5(2):244‐252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tamiya N, Noguchi H, Nishi A, et al. Population ageing and wellbeing: lessons from Japan's long‐term care insurance policy. Lancet. 2011;378(9797):1183‐1192. [DOI] [PubMed] [Google Scholar]
- 15. Tsutsui T, Muramatsu N. Care‐needs certification in the long‐term care insurance system of Japan. J Am Geriatr Soc. 2005;53(3):522‐527. [DOI] [PubMed] [Google Scholar]
- 16. Noda H, Yamagishi K, Ikeda A, Asada T, Iso H. Identification of dementia using standard clinical assessments by primary care physicians in Japan. Geriatr Gerontol Int. 2018;18(5):738‐744. [DOI] [PubMed] [Google Scholar]
- 17. Kawagoe S, Tsuda T, Doi H. Study on the factors determining home death of patients during home care: a historical cohort study at a home care support clinic: death of patients during home care. Geriatr Gerontol Int. 2013;13(4):874‐880. [DOI] [PubMed] [Google Scholar]
- 18. Ministry of Health , Labour and Welfare. Health and Welfare Services for the Elderly. http://www.mhlw.go.jp/english/wp/wp‐hw6/dl/10e.pdf. Accessed June 23, 2018.
- 19. Martinez C, Jones RW, Rietbrock S. Trends in the prevalence of antipsychotic drug use among patients with Alzheimer's disease and other dementias including those treated with antidementia drugs in the community in the UK: a cohort study. BMJ Open. 2013;3(1):e002080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gallini A, Andrieu S, Donohue JM, Oumouhou N, Lapeyre‐Mestre M, Gardette V. Trends in use of antipsychotics in elderly patients with dementia: impact of national safety warnings. Eur Neuropsychopharmacol. 2014;24(1):95‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kales HC, Zivin K, Kim HM, et al. Trends in antipsychotic use in dementia 1999‐2007. Arch Gen Psychiatry. 2011;68(2):190‐197. [DOI] [PubMed] [Google Scholar]
- 22. Matsunaga S, Kishi T, Iwata N. Memantine monotherapy for Alzheimer's disease: a systematic review and meta‐analysis. PLoS One. 2015;10(4):e0123289 10.1371/journal.pone.0123289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vidal JS, Lacombe JM, Dartigues JF, et al. Evaluation of the impact of memantine treatment initiation on psychotropics use: a study from the French national health care database. Neuroepidemiology. 2008;31(3):193‐200. [DOI] [PubMed] [Google Scholar]
- 24. Lachaine J, Beauchemin C, Crochard A, Bineau S. The impact of memantine and cholinesterase inhibitor initiation for Alzheimer disease on the use of antipsychotic agents: analysis using the Régie de l'Assurance Maladie du Québec Database. Can J Psychiatry. 2013;58(4):195‐200. [DOI] [PubMed] [Google Scholar]
- 25. Shah SM, Carey IM, Harris T, Dewilde S, Cook DG. Antipsychotic prescribing to older people living in care homes and the community in England and Wales. Int J Geriatr Psychiatry. 2011;26(4):423‐434. [DOI] [PubMed] [Google Scholar]
- 26. Foebel AD, Liperoti R, Onder G, et al. Use of antipsychotic drugs among residents with dementia in European long‐term care facilities: results from the SHELTER study. J Am Med Dir Assoc. 2014;15(12):911‐917. [DOI] [PubMed] [Google Scholar]
- 27. Gurwitz JH, Bonner A, Berwick DM. Reducing excessive use of antipsychotic agents in nursing homes. JAMA. 2017;318(2):118‐119. [DOI] [PubMed] [Google Scholar]
- 28. American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, 3rd ed., revised (DSM‐III‐R). Washington DC: American Psychiatric Association; 1987.
- 29. Ikejima C, Hisanaga A, Meguro K, et al. Multicentre population‐based dementia prevalence survey in Japan: a preliminary report: dementia prevalence survey in Japan. Psychogeriatrics. 2012;12(2):120‐123. [DOI] [PubMed] [Google Scholar]
- 30. Sado M, Inagaki A, Koreki A, et al. The cost of schizophrenia in Japan. Neuropsychiatr Dis Treat. 2013;9:787‐798. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 One‐year prevalent users of antipsychotics excluding sulpiride and prochlorperazine according to dementia status and the characteristics of the study participants


