Abstract
Background: The present study evaluated the relationship between body-roundness index (BRI) and metabolic syndrome (MetS) in type 2 diabetes.
Methods: A cross-sectional study was conducted on 585 type 2 diabetes in Qinhuangdao. MetS was defined as per the Chinese Diabetes Society.
Results: The BRI was strongly associated with the odds of having MetS in both males and females after adjustment for age, history of diabetes, and body-mass index (P<0.05). AUC of the BRI were 0.824 for males and 0.775 for females (P<0.001). The optimal cutoff points for the BRI were 3.85 in males (sensitivity 76.5%, specificity 82.1%) and 4.05 in females (sensitivity 76.4%, specificity 70.3%).
Conclusion: The BRI was correlated with MetS and was an effective indicator for the screening of MetS in type 2 diabetes.
Keywords: body-roundness index, metabolic syndrome, type 2 diabetes
Introduction
Diabetes is a growing global problem. According to the International Diabetes Federation, 8.8% of adults aged 20–79 years were estimated to have diabetes in 2017.1 Diabetes leads to increased risk of cardiovascular complications. In turn, cardiovascular diseases is a major cause of death in patients with diabetes.2 Metabolic syndrome (MetS) is a cluster of cardiometabolic risk factors. The prevalence of MetS is high 3 and further increases the risk of cardiovascular diseases in type 2 diabetes.4–6 Early identification and appropriate treatment canreduce the excess risk of MetS.
Central obesity is at the core of MetS. Therefore, simple obesity indices are used for screening MetS. Waist circumference (WC) and waist:height ratio (WHtR) are the most widely used indices. In recent years, some new indices based on WC have been proposed. Visceral adiposity index, lipid-accumulation product, and WC–triglyceride (TG) index were calculated with WC, TG, and high-density-lipoprotein cholesterol (HDL-C).7 Body-shape index, conicity index, and abdominal volume index were calculated with WC, height, weight, and hip circumference.8–10
The body-roundness index (BRI) was proposed by Thomas et al in 2013.11 It is an index estimated with the use of height, weight, WC, and hip circumference (optional). The web-based calculator gives a result for BRI and streamlines the calculation. This method is derived from geometry and provides body-type location relative to a healthy body. BRI shows a superior predictive power for MetS in the general population, obese and overweight population, and postmenopausal women.12–14
Cutoff points for the BRI are not unified across different populations.12,15,16 The BRI is closely associated with diabetes, and has been used to identify diabetes in a cross-sectional study.17,18 It can also predict diabetes.19 To our knowledge, no investigators have attempted to use the BRI for screening MetS in type 2 diabetes. Therefore, it was necessary to explore cutoff points for the BRI in type 2 diabetes. The aim of our study was to evaluate the relationship between the BRI and MetS in type 2 diabetes.
Methods
Subjects
After informed consent had been obtained, a cross-sectional study was conducted. All subjects were patients with type 2 diabetes >18 years old.20 Exclusion criteria were type 1 diabetes, clinical evidence of other endocrinopathy, pregnacy, and acute or chronic inflammation. This study was approved by the ethics committee of the First Hospital of Qinhuangdao. All subjects provided written informed consent before study initiation. This study was conducted in accordance with the Declaration of Helsinki.
Measurements
Anthropometric measurements, including height, weight, WC, and blood pressure, were obtained. WC was measured midway between the lowest rib and the top of the iliac crest. BRI was calculated with an online calculator (http://www.pbrc.edu/bodyroundness).11 The formula was BRI = 364.2–365.5×(1 – [WC/2π]2/[0.5 × height2)½.
After a 10-hour overnight fast, blood samples were collected from an antecubital vein into heparinized tubes. Fasting plasma glucose (FPG) concentrations and serum-lipid levels were measured using enzymatic assays with an autoanalyzer (Hitachi, Tokyo, Japan).
Definition of metabolic syndrome
MetS was defined as per the Chinese Diabetes Society. Participants had to meet any three or more of fivefactors: 1) WC ≥90 cm (male) and 85 cm (female), 2) FPG ≥6.1 mmol/L or 2-hour PG levels ≥7.8 mmol/L after a 75 g oral glucose-tolerance test or have been diagnosed with diabetes, 3) blood pressure ≥130/85 mmHg or had been diagnosed with hypertension, 4) TG ≥1.7 mmol/L, and 5) HDL-C <1.04 mmol/L.21
Statistical analyses
All analyses were performed using SPSS 11.5 (SPSS, Chicago, IL, USA). Comparisons were conducted between groups using independent samples t-test and χ2 analysis. For BRI, we divided them into increasing sex-specific tertiles and used multiple logistic regression analysis to calculate ORs for MetS across tertiles, with tertile 1 as the reference group, adjusting for age, history of diabetes, and body-mass index (BMI). ROC curves for BRI were drawn to show how well they were able to separate subjects into groups with or without MetS. Comparisons of AUCs were performed with MedCalc 11.4.2.0 (Ostend, Belgium). P<0.05 was considered statistically significant.
Results
This study enrolled 585 type 2 diabetes patients (339 males and 246 females, age 54.5±12.5 years). Average history of diabetes was 6.4±6.7 years. Prevalence of MetS was similar between males and females (males 75.2% vs females 74.0%, χ2=0.116; P=0.734). Characteristics of the study population are presented in Table 1. Age, history of diabetes, and FPG between the two groups were similar (P>0.05). BMI, WC, WHtR, BRI, systolic blood pressure, diastolic blood pressure, and TG were all significantly higher in the MetS group than the non-MetS group (P<0.001). HDL-C was significantly lower in the MetS group than the non-MetS group (P<0.001).
Table 1.
Basic characteristics of study population
| Variables | Non-MetS group (n=148) | MetS group (n=437) | t or χ2 | P |
|---|---|---|---|---|
| Males/females | 84/64 | 255/182 | 0.116 | 0.734 |
| Age (years) | 53.7±12.6 | 54.8±12.5 | 0.876 | 0.381 |
| History of diabetes (years) | 6.3±6.4 | 6.4±6.8 | 0.066 | 0.948 |
| BMI (kg/m2) | 23.9±3.5 | 27.1±3.3 | 9.865 | <0.001 |
| WC (cm) | 84.2±8.6 | 95.1±10.0 | 12.685 | <0.001 |
| WHtR | 0.50±0.05 | 0.57±0.05 | 11.128 | <0.001 |
| BRI | 3.5±1.0 | 4.7±1.3 | 11.486 | <0.001 |
| SBP (mmHg) | 123.6±15.3 | 131.7±18.8 | 5.243 | <0.001 |
| DBP (mmHg) | 79.4±9.1 | 83.2±10.0 | 4.189 | <0.001 |
| FPG (mmol/L) | 9.07±4.01 | 9.13±3.44 | 0.149 | 0.882 |
| TG (mmol/L) | 1.15±0.54 | 2.86±2.60 | 12.871 | <0.001 |
| HDL-C (mmol/L) | 1.31±0.26 | 1.05±0.30 | 9.257 | <0.001 |
Abbreviations: MetS, metabolic syndrome; BMI, body-mass index; WC, waist circumference; WHtR, waist:height ratio; BRI, body-roundness index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; TG, triglyceride; HDL-C, high-density-lipoprotein cholesterol.
BRI was strongly associated with the odds of having MetS in both males and females, after adjustment for age, history of diabetes, and BMI (P<0.001). In males, patients in BRI tertile 2 (OR 5.035, P<0.001) and tertile 3 (OR 7.195, P<0.001) were more likely to have MetS than those in tertile 1. In females, patients in BRI tertile 2 (OR 4.616, P<0.001) and tertile 3 (OR 3.772, P=0.012) were more likely to have MetS than those in tertile 1 (Table 2)
Table 2.
Prevalence of metabolic syndrome according to the level of body-roundness index
| Men (n=339) | n (%) | OR (95%CI) | P | Women (n=246) | n (%) | OR (95%CI) | P |
|---|---|---|---|---|---|---|---|
| Tertiles 1 (n=113) | 52 (46.0) | 1 | Tertiles 1 (n=82) | 39 (47.6) | 1 | ||
| Tertiles 2 (n=113) | 96 (85.0) | 5.035 (2.560–9.904) | <0.001 | Tertiles 2 (n=82) | 70 (85.4) | 4.616 (2.056–10.363) | <0.001 |
| Tertiles 3 (n=113) | 107 (94.7) | 7.195 (2.576–20.099) | <0.001 | Tertiles 3 (n=82) | 73 (89.0) | 3.772 (1.345–10.577) | 0.012 |
Note: Multiple logistic regression analysis, adjustment for age, history of diabetes, and body-mass index.
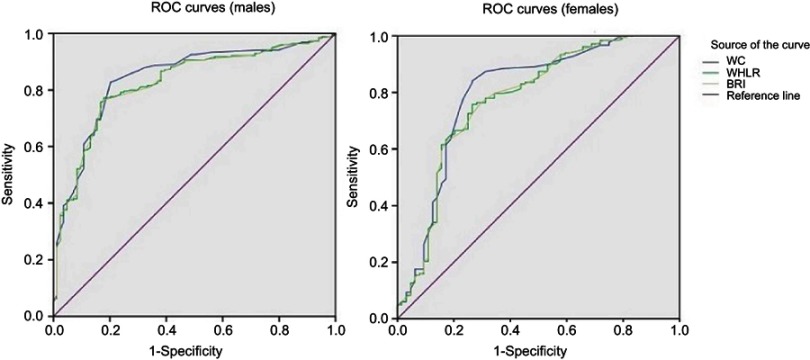
AUCs for WC were 0.842 for males and 0.798 for females (P<0.001)for WHtR 0.825 for males and 0.775 for females (P<0.001), and for BRI 0.824 for males and 0.775 for females (P<0.001; Figure 1), while they were similar among BRI, WC and WHtR (P>0.05; Table 3). Optimal cutoff points for BRI were 3.85 in males (sensitivity 76.5%, specificity 82.1%) and 4.05 in females (sensitivity 76.4%, specificity 70.3%).
Figure 1.
ROC curves of obesity indices used to identify the presence of metabolic syndrome in type 2 diabetes.
Abbreviations: WC, waist circumference; WHtR, waist:height ratio.
Table 3.
AUC and SE of each variable for screening of metabolic syndrome in type 2 diabetes
| Variables | AUC (95% CI) | SE | P | Z* | P* | Z# | P# |
|---|---|---|---|---|---|---|---|
| Men | |||||||
| WC | 0.842 (0.794–0.891) | 0.025 | <0.001 | ||||
| WHtR | 0.825 (0.776–0.875) | 0.025 | <0.001 | 0.481 | 0.630 | ||
| BRI | 0.824 (0.775–0.874) | 0.025 | <0.001 | 0.509 | 0.610 | 0.028 | 0.977 |
| Women | |||||||
| WC | 0.798 (0.726–0.870) | 0.037 | <0.001 | ||||
| WHtR | 0.775 (0.702–0.848) | 0.037 | <0.001 | 0.440 | 0.660 | ||
| BRI | 0.775 (0.702–0.848) | 0.037 | <0.001 | 0.440 | 0.660 | 0 | 1 |
Notes: *Compared with WC; #compared with WHtR. AUCs were similar among WC, WHtR, and BRI (P>0.05).
Abbreviations: WC, waist circumference; WHtR, waist:height ratio; BRI, body-roundness index.
Discussion
Our study presents evidence that the BRI may be a useful tool for the screening of MetS in type 2 diabetes, but not superior to WC and WHtR. Zhang et al found that BRI showed similar ability to detect subjects with MetS among general population.12 Similar results have also been observed in people with intermediate cardiovascular risk, postmenopausal women, and obese and overweight adults.13–15 The prevalence of MetS was 28.3%–55.7% in these studies. Type 2 diabetes is often accompanied by MetS.22 Prevalence was >70% in our study, higher than previous research, but the power of BRI was similar to previous research.
Cutoff points for the BRI have not been consistent across studies: 3.47–5.69 for males and 3.18–5.77 for females.12,15,16 This difference could be because of study populations, race, and diagnostic criteria for MetS. In our study, cutoff points for BRI were 3.85 for males and 4.05 for females in type 2 diabetes, similar to Chinese studies and lower than a Spanish study.
The capacity of the BRI to predict each component of MetS, such as dyslipidemia, hypertension, and diabetes, were comparable but not superior to the classical indicators of obesity.18,23–25 Insulin resistance and chronic inflammation are the main mechanisms of MetS. BRI showed significant correlation with insulin resistance and inflammatory factors and equivalence with traditional obesity indices.13,26,27
There are limitations to our study. First, although hip circumference was not a mandatory variable for BRI, combined hip circumference and WC can enhanced the performance of the BRI.11 There were not hip-circumference data in our database. Second, patients were recruited from a single hospital, and replicability of these results should be tested with a multicenter study. Third, other confounding factors, such as physical activity, diet, and other lifestyle factors, were not analyzed in our study. Fourth, the sample was relatively small. Studies with larger samples are necessary in future.
In summary, BRI was correlated with MetS and an effective indicator for the screening of MetS in type 2 dabetes; however, it showed no advantage over traditional obesiy indices.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Federation. ID. Idf Diabetes Atlas. 8th ed. Brussels, Belgium: International Diabetes Federation; 2017. Available from: www.diabetesatlas.org. [Google Scholar]
- 2.Federation. ID. Diabetes and Cardiovascular Disease. Brussels, Belgium: International Diabetes Federation; 2016. Available from: www.idf.org/cvd. [Google Scholar]
- 3.Udenze IC, Azinge EC, Arikawe AP, et al. The prevalence of metabolic syndrome in persons with type 2 diabetes at the Lagos university tteaching hospital, Lagos, Nigeria. West Afr J Med. 2013;32:126–132. [PubMed] [Google Scholar]
- 4.Guzder RN, Gatling W, Mullee MA, Byrne CD. Impact of metabolic syndrome criteria on cardiovascular disease risk in people with newly diagnosed type 2 diabetes. Diabetologia. 2006;49:49–55. doi: 10.1007/s00125-005-0063-9 [DOI] [PubMed] [Google Scholar]
- 5.Bonora E, Targher G, Formentini G, et al. The metabolic syndrome is an independent predictor of cardiovascular disease in type 2 diabetic subjects. prospective data from the verona diabetes complications study. Diabet Med. 2004;21:52–58. [DOI] [PubMed] [Google Scholar]
- 6.Yao MF, He J, Sun X, et al. Gender differences in risks of coronary heart disease and stroke in patients with type 2 diabetes mellitus and their association with metabolic syndrome in China. Int J Endocrinol. 2016;2016:8483405. doi: 10.1155/2016/8483405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ma CM, Lu N, Wang R, Liu XL, Lu Q, Yin FZ. Three novel obese indicators perform better in monitoring management of metabolic syndrome in type 2 diabetes. Sci Rep. 2017;7:9843. doi: 10.1038/s41598-017-10446-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haghighatdoost F, Sarrafzadegan N, Mohammadifard N, Asgary S, Boshtam M, Azadbakht L. Assessing body shape index as a risk predictor for cardiovascular diseases and metabolic syndrome among Iranian adults. Nutrition. 2014;30:636–644. doi: 10.1016/j.nut.2013.10.021 [DOI] [PubMed] [Google Scholar]
- 9.Costa EC, Sa JC, Soares EM, Lemos TM, Maranhao TM, Azevedo GD. Anthropometric indices of central obesity how discriminators of metabolic syndrome in Brazilian women with polycystic ovary syndrome. Gynecol Endocrinol. 2012;28:12–15. doi: 10.3109/09513590.2011.583956 [DOI] [PubMed] [Google Scholar]
- 10.Motamed N, Sohrabi M, Poustchi H, et al. The six obesity indices, which one is more compatible with metabolic syndrome? A population based study. Diabetes Metab Syndr. 2017;11:173–177. doi: 10.1016/j.dsx.2016.08.024 [DOI] [PubMed] [Google Scholar]
- 11.Thomas DM, Bredlau C, Bosy-Westphal A, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity (Silver Spring). 2013;21:2264–2271. doi: 10.1002/oby.20408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang J, Zhu W, Qiu L, Huang L, Fang L. Sex- and age-specific optimal anthropometric indices as screening tools for metabolic syndrome in Chinese adults. Int J Endocrinol. 2018;2018:1067603. doi: 10.1155/2018/1528437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li G, Wu HK, Wu XW, et al. The feasibility of two anthropometric indices to identify metabolic syndrome, insulin resistance and inflammatory factors in obese and overweight adults. Nutrition. 2019;57:194–201. doi: 10.1016/j.nut.2018.05.004 [DOI] [PubMed] [Google Scholar]
- 14.Liu PJ, Ma F, Lou HP, Zhu YN. Body roundness index and body adiposity index: two new anthropometric indices to identify metabolic syndrome among Chinese postmenopausal women. Climacteric. 2016;19:433–439. doi: 10.1080/13697137.2016.1202229 [DOI] [PubMed] [Google Scholar]
- 15.Gomez-Marcos MA, Gomez-Sanchez L, Patino-Alonso MC, et al. Capacity adiposity indices to identify metabolic syndrome in subjects with intermediate cardiovascular risk (MARK study). PLoS One. 2019;14:e0209992. doi: 10.1371/journal.pone.0209992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang H, Liu A, Zhao T, et al. Comparison of anthropometric indices for predicting the risk of metabolic syndrome and its components in Chinese adults: a prospective, longitudinal study. BMJ Open. 2017;7:e016062. doi: 10.1136/bmjopen-2017-016062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao Q, Zhang K, Li Y, et al. Capacity of a body shape index and body roundness index to identify diabetes mellitus in han Chinese people in Northeast China: a cross-sectional study. Diabet Med. 2018;35:1580–1587. doi: 10.1111/dme.13787 [DOI] [PubMed] [Google Scholar]
- 18.Chang Y, Guo X, Chen Y, et al. A body shape index and body roundness index: two new body indices to identify diabetes mellitus among rural populations in northeast China. BMC Public Health. 2015;15:794. doi: 10.1186/s12889-015-2150-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang J, Wang F, Wang J, et al. Using different anthropometric indices to assess prediction ability of type 2 diabetes in elderly population: a 5 year prospective study. BMC Geriatr. 2018;18:218. doi: 10.1186/s12877-018-0912-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Diabetes A. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(Suppl 1):S81–90. doi: 10.2337/dc14-S081 [DOI] [PubMed] [Google Scholar]
- 21.Society CD. Chinese guideline for type 2 diabetes. Chin J Endocrinol Metab. 2014;30:893–942. [Google Scholar]
- 22.Foroozanfar ZM, Najafipour HP, Khanjani NPM, Bahrampour APM, Ebrahimi HM. The prevalence of metabolic syndrome according to different criteria and its associated factors in type 2 diabetic patients in Kerman, Iran. Iran J Med Sci. 2015;40:522–525. [PMC free article] [PubMed] [Google Scholar]
- 23.Zaid M, Ameer F, Munir R, et al. Anthropometric and metabolic indices in assessment of type and severity of dyslipidemia. J Physiol Anthropol. 2017;36:19. doi: 10.1186/s40101-017-0134-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chang Y, Guo X, Guo L, Li Z, Li Y, Sun Y. The feasibility of two new anthropometric indices to identify hypertension in rural China: a cross-sectional study. Medicine (Baltimore). 2016;95:e5301. doi: 10.1097/MD.0000000000004864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tian S, Zhang X, Xu Y, Dong H. Feasibility of body roundness index for identifying a clustering of cardiometabolic abnormalities compared to BMI, waist circumference and other anthropometric indices: the China health and nutrition survey, 2008 to 2009. Medicine (Baltimore). 2016;95:e4642. doi: 10.1097/MD.0000000000004864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feng J, He S, Chen X. Body adiposity index and body roundness index in identifying insulin resistance among adults without diabetes. Am J Med Sci. 2019;357:116–123. doi: 10.1016/j.amjms.2018.11.006 [DOI] [PubMed] [Google Scholar]
- 27.Barazzoni R, Gortan Cappellari G, Semolic A, et al. Central adiposity markers, plasma lipid profile and cardiometabolic risk prediction in overweight-obese individuals. Clin Nutr. 2019;38:1171–1179. [DOI] [PubMed] [Google Scholar]