Abstract
Objective:
More effective transitions and transfers of young people with sickle cell disease (SCD) into the adult healthcare setting is a focus of both primary care and specialty care medical organizations. Effective transition and transfer requires six core elements: establishing a policy, tracking progress, administering transition readiness assessments, planning for adult care, transferring to adult care, and integrating into an adult practice. We developed a program using these six core elements. The objective of our report was to assess the development and implementation of this program.
Methods:
We used the six core elements to develop and implement a program at Virginia Commonwealth University for children and adolescents with SCD to transition to adult health care.
Results:
We assessed individuals’ differences by age and grade, their independent living skills, their feelings about moving to adult care, tallied and analyzed several assessment scales, and assessed transfer success and patient retention.
Conclusions:
The principles and lessons we learned in developing and implementing this program over 5 years, accompanied by caring, flexible, and dedicated care team members, often can overcome even severe barriers to care transitions.
Keywords: care coordination, medical home, pediatric-to adult-transition, sickle cell disease, transition of care
Facilitating more effective transitions and transfers of young adults into the adult healthcare setting is a central focus of both primary care and specialty care medical organizations. The American Academy of Pediatrics, the American College of Physicians, and the American Academy of Family Practice have woven transition of care into their overall medical home initiatives.1 The National Alliance to Advance Adolescent Health’s program Got Transition has developed six core elements of healthcare transition: establishing a policy, tracking progress, administering transition readiness assessments, planning for adult care, transferring, and integrating into an adult practice. The American College of Physicians Transitions initiative, in partnership with Got Transition/Center for Health Care Transition Improvement, the Society of General Internal Medicine, and the Society for Adolescent Health and Medicine, have developed a Web site with a toolkit that contains condition-specific tools, including transition-readiness assessments, self-care assessments, and medical summaries.2 Transition tools also are available for a host of specialty diseases, including sickle cell disease (SCD), in the form of the American Society of Hematology’s transition toolkit.3
The state of care and the smoothness and success of transition for patients with SCD, however, continues to lag behind the state of care for well children or those with other special healthcare needs.4,5 Decades ago, our research suggested that adults with SCD rated their quality of care as poor.6 Current research suggests that the quality of care ratings of adults with SCD seem not to have improved7,8 and that subjectively they are worse for adult versus pediatric patients.9 Quality of care indicators have been proposed, published, and/or measured for children with SCD10–14 and to some degree for young adults and older,15–18 but only recently have quality of care indicators for the transition of care of patients with SCD been proposed.19 Programs to transfer patients with SCD, therefore, deserve special emphasis and funding to determine whether quality of care is maintained pre- and posttransfer.
We describe here the processes and results of the Virginia Commonwealth University (VCU) Transition Intervention Program (TIP), a transition program focused on youth/young adults with SCD at this urban academic medical center on the US mid-Atlantic seaboard. First, we describe the policy and structural elements of the program in detail. Second, we describe evaluative elements of the program and the methods of implementation of the evaluation. Third, we report the results of patient measures using those evaluative elements. Fourth, we report early transfer success rates among program participants and early patient retention rates among transferred patients. Finally, we discuss important lessons learned from our results and from program implementation.
Methods
Establishing a Policy
VCU Medical Center serves 300 pediatric and 350 adults with SCD. Planning for TIP began in approximately 2008. In the ensuing years, at least two adult physicians, an adult advance practice provider, two or more pediatric physicians, and a pediatric advanced practice provider provided clinical care for patients with SCD. The SCD transition team included these adult and pediatric medical care providers, adult and pediatric social workers, an educational coordinator, and a clinical psychologist.
The agreed-upon TIP policy was to reach, orient, and track patients 3 years before their transfer to adult care, to transfer care at high school graduation, and to ensure at least a first visit to an adult provider. Further follow-up and tracking posttransfer, although optional, was attempted. Our primary goal at TIP implementation was to improve the percentage of pediatric patients who succesfully transferred to the adult clinic for medical care.
Beginning in 2008, TIP recruited youth approximately age 15 years with SCD who were already being seen in the VCU pediatric SCD practice. A total of 37 participants completed the TIP program during the first 3 years of the program (Fig.). The TIP program graduated its first group of participants in 2011. To measure the success of our primary goal, to improve the percentage of pediatric patients who stayed in the VCU catchment area who succesfully transferred to the adult clinic for medical care, we measured the rate of transfer for the first 3 years, beginning with 2011 and ending with 2013. We defined successful transfer as a first visit in the adult clinic within 6 months of high school graduation. Of the 37 graduates, 5 (13.5%) requested that their care be transferred to another center at the time of graduation. Those patients were moving to be with family or were attending secondary education outside the catchment area. The remaining 32 stayed in the VCU catchment area.
Fig.
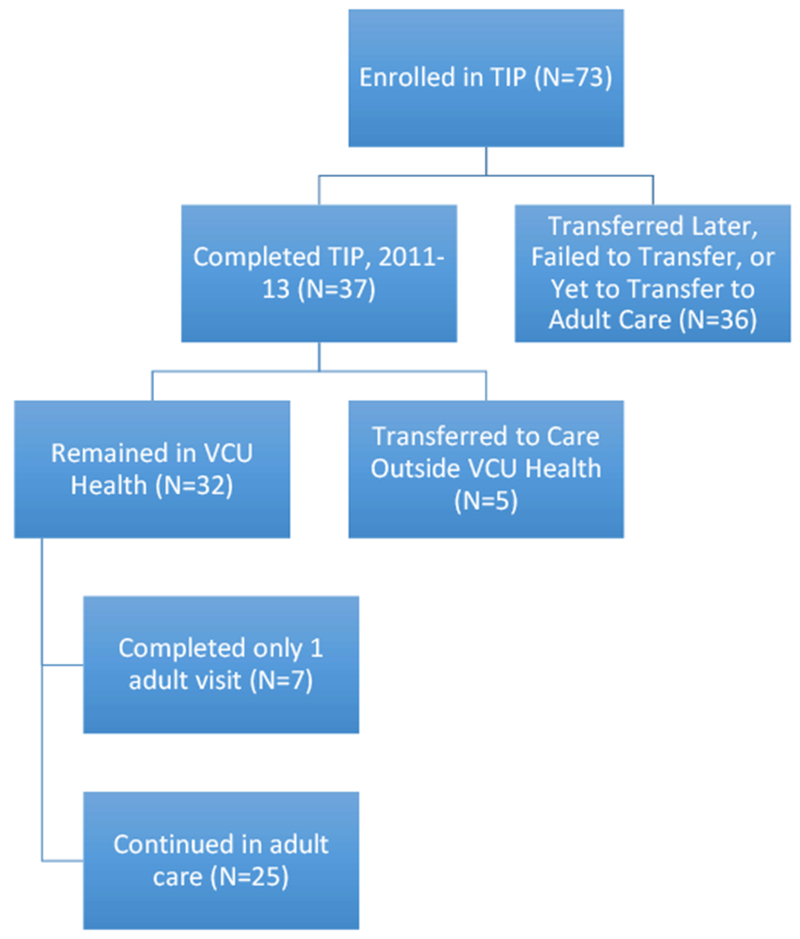
Flow diagram of TIP enrollee outcomes. TIP, Transition Intervention Program; VCU Virginia Commonwealth University.
TIP delivered a 3-year curriculum, designed to culminate at graduation from high school. An educational coordinator and a clinical psychologist worked individually with youth with SCD through high school graduation to improve their readiness for transition and safe integration into adult care. TIP delivered standardized content to all of the patients and families, as well as tailored, individual educational and support interventions during case management and care. TIP addressed knowledge, skills, attitudes, and confidence about transition in accordance with the six core elements of transition. TIP included education of families and patients about the transition policy; a clinical database to track the progress of each patient; and group and individual education about transition skills, the culture of adult medicine, and self-advocacy in obtaining support from schools and employers.
Didactic content was delivered during group educational sessions planned during prespecified clinic days by social workers, educational coordinators, and adult and pediatric medical care providers. Individualized reinforcement and targeted support was provided during other clinic visits by social workers, including the formal transition coordinator.
Tracking Progress and Administering Transition Readiness Assessments
We developed and validated a new instrument, the Transition Intervention Program-Readiness For Transition (TIP-RFT) assessment, as an SCD-specific readiness for transition assessment tool and as a way to track the transition progress of TIP participants.20,21 We assembled a draft TIP-RFT survey assessing healthcare knowledge and skills, educational/vocational skills, health benefits skills, social support, and independent living skills. The draft TIP-RFT assessment was constructed based on a literature review and provider and patient consensus. We achieved consensus about TIP-RFT content during several monthly meetings of team members, including pediatric and adult providers and the program manager at the Virginia Sickle Cell Awareness Program at VDH. Meetings consisted of conducting literature review, vetting of existing transition or transition-relevant assessment surveys, choosing and/or writing items, and debating the appropriateness of domains and items. Sample items from the draft TIP-RFT assessment are shown in Table 1. The complete question battery for the draft TIP-RFT assessment is available from the authors.
Table 1.
TIP-RFT evaluation domains and example assessment items
| Final TIP-RFT assessment domain | Draft TIP-RFT assessment domain | No. items | Example assessment item | Response categories | Source of assessment |
|---|---|---|---|---|---|
| Healthcare knowledge and skills | Healthcare knowledge and skills | 18 | I know what my hemoglobin type is (eg, SS, SC, sickle thalassemia) | Yes/no | Team members |
| I know why drinking a lot of fluid is important to management of SCD | Yes/no | Team members | |||
| Education and vocation planning | Educational/vocational skills | 11 | I have a 504 or an IEP | Yes/no/not applicable | Team members |
| I know the types of work situations that could cause problems related to SCD | Yes/no | Team members | |||
| Social support skill set | Social support | 9 | I have friends that I can talk to about SCD | Yes/no | Team members |
| I know about community-based sickle cell programs (in my area) | Yes/no | Team members | |||
| Independent living skills | Independent living skills | 10 | I know how to manage money and pay a bill | Yes/no | Children’s Hospital, Boston Transitions Initiativea |
| I know how to get my prescription medications filled | Yes/no | Children’s Hospital, Boston Transitions Initiative | |||
| I know how to make my own doctor’s appointments | Yes/no | Children’s Hospital, Boston Transitions Initiative | |||
| Health benefits skills | 6 | I carry my own copy of my health insurance card | Yes/no | Team members | |
| I have, or am working on, a portable medical history form | Yes/no | Team members |
IEP, individualized education plan; SCD, sickle cell disease; TIP-RFT, Transition Intervention Program-Readiness for Transition.
We also coadministered three existing scales. Table 2 shows sample items from each of the three scales: the Feelings About Moving to an Adult Care Program Scale of the Adolescent Sickle Cell Transfer Questionnaire (Feelings-SCTQ),22 our own internally developed sickle cell–related stress scale (Sickle Cell Stress Scale-Adolescent),23–25 and the Sickle Cell Self-Efficacy Scale.26,27
Table 2.
Assessment scales coadministered with draft TIP-RFT assessment, with example assessment items
| No. items | Example assessment item | Response categories | Source of assessment | |
|---|---|---|---|---|
| Adolescent SCTQ, Feelings About Moving to an Adult Care Program section |
12 | I feel it will be all right to move on | Not at all/a little bit/moderately/quite a bit/extremely | Telfair et al22 |
| I will feel deserted/abandoned | Not at all/a little bit/moderately/quite a bit/extremely | Telfair et al22 | ||
| Sickle Cell Stress Scale-Adolescent | 11 | I worry that I won’t be able to get insurance because of my SCD | Strongly agree/somewhat agree/neither agree or disagree/somewhat disagree/strongly disagree | Team members, Treadwell et al21 |
| I worry about my illness getting in the way of school work and/or job | Strongly agree/somewhat agree/neither agree or disagree/somewhat disagree/strongly disagree | Team members, Treadwell et al21 | ||
| Sickle Cell Self-Efficacy Scale | 9 | How sure are you that you can do something to cut down on most of the pain you have when you have a pain episode? | Not at all sure/not sure/neither/sure/very sure | Edwards et al26 and Clay et al27 |
| As compared with other people with SCD, how sure are you that you can manage your life from day to day? | Not at all sure/not sure/neither/sure/very sure | Edwards et al26 and Clay et al27 |
SCD, sickle cell disease; SCTQ, Sickle Cell Transfer Questionnaire.
We assessed how well each domain or item bank in the draft TIP-RFT predicted readiness for transition as measured by a score including all of the items and found these item banks to be somewhat predictive of the total score.28 We used principal components factor analysis to reduce the draft TIP-RFT from five domains/subscales to four reassigned/remapped domains of readiness. The validated TIP-RFT assessment assessed the domains of confidence/self-efficacy, knowledge, skills, and attitudes.
We administered the draft TIP-RFT assessment and the three additional scales to age-eligible adolescents (grade 9 or higher) in our clinics, regardless of age, amount of TIP participation, or grade. The revised 22-item instrument consisted of 4 subscales (Health Benefits Skills was eliminated)—Independent Living Skills, Healthcare Knowledge and Skills, Education and Vocation Planning, Social Support Skill Set—and demonstrated good internal consistency reliability and construct validity.26
Because we developed and validated the TIP-RFT assessment at the same time as the TIP program began, the draft, not the final TIP-RFT assessment, was the version administered to the first 73 TIP participants. Questionnaires often were not administered at baseline and not systematically repeated. For convenience, questionnaires were administered just before or after pediatric visits for medical care as part of the educational assessments and interventions performed by pediatric social workers and/or the transition coordinator. The curriculum reinforced learning through repetition. For example, a caregiver often asked patients to verify their usual hemoglobin, which the caregiver knew, if that patient’s TIP-RFT Medical Skill Set score was low. Similarly, a social worker, aware that a patient was underperforming on a TIP domain related to instrumental activities of daily living such as writing a check, often instructed a patient during a clinic visit in how to write a check. Alternatively, noting the strong endorsement of fear of transition or transfer, the social worker brought this to the attention of both the adult provider-to-be and the psychologist. Individualized assessment and individually tailored learning plans were based on these assessments. This delivery method was patient centered in that it did not require special visits for curriculum delivery or assessment. Individualized reinforcement and support attempted to address differences in personality, motivation, family support, and illness.
Planning for Adult Care, Transferring, and Integrating Into an Adult Practice
Because VCU pediatric and adult subspecialty providers already had delivered care under the same VCU governance and institution, often in the same buildings, for the past 4 decades, the TIP transfer policy was to transfer patients as a first choice from a VCU pediatric to a VCU adult SCD provider. Fully 100% of patients could stay in the VCU system because VCU accepts patients without insurance and with all forms of insurance. This structural advantage allowed VCU providers to attend to transition core elements without having to focus attention on policy issues such as availability and willingness of providers and systems of care for youth/young adults with SCD. The quality of care for SCD could be evaluated without giving attention to new payment structures for delivery of care (eg, managed care/accountable care organizations). For patients remaining in the VCU catchment area, providers did not have to wonder about the healthcare system into which patients would transition.
The plan for transfer to adult care began months before the actual transfer. Initially, patients were discussed frequently during joint case management meetings of the adult and pediatric SCD care teams, in which details of prior and future planned management and handoff planning were discussed for each patient. Later, these meetings were held less frequently, but they were held at least annually.
Just before transfer, at the end of high school, patients were invited to an annual graduation recognition ceremony at VCU Medical Center that was organized by pediatric staff jointly for graduating childhood cancer survivors and patients with SCD. Planners invited high-visibility motivational speakers. Photographs, videos, and testimonials were offered on behalf of each patient, and scholarships were awarded.
To enhance and support transfer, two community-based organizations provided key support to the TIP program. The Organization for Sickle Cell Resources provided scholarship funds upon high school graduation and offered a peer-to-peer mentoring program for young adults entering the adult SCD clinic. The Association for the Support of Kids with Cancer supported the pediatric hematology/oncology clinic. It helped fund the special graduation ceremony for patients, hosted an annual Christmas party in which transition-age patients with SCD were included, and purchased gift cards and supplies for TIP events.
Results
Assessment Differences by Age/Grade
We tested the hypothesis that adolescents in higher school grades (11, 12, or higher) were more ready than those in lower grades (9 and 10) for transition or transfer. Independent t tests were used to determine whether differences existed between the assessment results of 9th/10th graders versus 11th/12th graders/college students on the draft TIP-RFT assessment, Feelings-SCTQ, the Sickle Cell Stress Scale-Adolescent, and the Sickle Cell Self-Efficacy Scale (n = 73). In addition to testing for dichotomous group differences, simple linear regression analyses were used to determine whether the grade in school predicted the total scores for each of these assessments. All of the analyses were carried out using SPSS version 24 (IBM SPSS Statistics, Armonk, NY). We hypothesized that these results may differ because of innate maturity or because some may have had opportunities for more exposure to the TIP intervention.
No significant differences were found between 9th/10th graders and 11th/12th graders/college students on any assessment (all P > 0.05). Similarly, the grade in school did not significantly predict total scores on any assessment (all P > 0.05).
TIP-RFT Item Results
Independent Living Skills
Regarding independent living skills (mostly instrumental activities of daily living), approximately 75% of subjects said they could manage money and pay a bill. Half said they had held a job. Virtually all of the subjects said they could fix their own meals, and 94% said they could wash their own clothes. Seventy-two percent said they could write a check, and 79% reported that could use an ATM card. A total of 84% said they knew how to fill their prescriptions. Seventy-five percent said they could make their own doctor’s appointments, but only half said that they traveled to the doctor on their own.
Healthcare Knowledge and Skills
Regarding SCD healthcare knowledge and skills, almost all of the subjects understood SCD to be genetic and they knew how they could pass it on to their children. Fully 79% said they knew which of the 4 SCD genotypes they inherited, but only 37% knew their hemoglobin level. A total of 75% said they asked questions during medical appointments and kept track of their medical appointments; only 50% knew anything about hydroxyurea; only 44% knew how SCD could affect their health if they (or a female with SCD) became pregnant. A total of 25% said they did not understand how drugs, alcohol, and tobacco usage affects SCD. Only 50% said “yes” to the statement, “I am working on a medical transition plan for care when I leave Pediatrics.” Regarding health benefits, 59% carried their own copy of their health insurance card. Only 22% were working on a portable medical history form.
Education and Vocation Planning
Regarding educational and vocational planning, only 41% had a 504 or individualized education plan. Similarly, only 40% had spoken with their school counselor about an employment evaluation program.
Social Support Skill Set
Regarding social support skills, all of the subjects had hobbies, 69% participated in activities at school or outside the home, 91% had chores at home, 72% had friends they could talk to about their disease, and 85% believed that they had a good social support system.
Feelings-SCTQ
Feelings-SCTQ items were endorsed in a variety of ways. Among all of the patients, on a scale of “0, not at all” to “4, extremely,” 34% endorsed “2, moderately” regarding their excitement about transition. Similarly, among all of the patients, 33% endorsed “3, quite a bit” for the statement “it will be alright [sic] to move on” (subjective readiness for medical transfer). Fully 24% endorsed “0” regarding relief about transition. Half endorsed a “0” regarding apathy about transition. A total of 65% endorsed various degrees of nervousness, 52% expressed various degrees of fear, and 69% expressed various degrees of anxiety. Nearly 30% endorsed some degree of anger, and 25% felt abandoned/deserted to some degree.
Sickle Cell Stress Scale-Adolescent
Twenty-eight percent of patients worried strongly that their pain would not be controlled by their medication; only 15% did not worry about this. A total of 66% had at least some worry about being hospitalized for long periods of time. One-fourth of patients strongly endorsed that death was always in the back of their minds and that their disease would keep them from doing what they enjoy. Half strongly endorsed that their doctors did not trust them with narcotics, and one-third worried strongly about not having enough narcotics or running out of narcotics. Approximately half worried strongly about obtaining insurance, and one-third worried strongly about being a burden to their parents or family. Most wondered about being able to take care of themselves when they were older: 32% mildly, 13% more, 12% even more, and 21% most strongly. A total of 13% strongly endorsed being worried about the disease interfering with school or their job.
Sickle Cell Self-Efficacy Scale
Self-efficacy was good, with 70% to 75% of patients endorsing strongly or somewhat strongly questions about expectations of continued function, managing their disease, or feeling better off than others with the disease or with dealing with the frustrations of the disease.
Transfer Success and Patient Retention
Before the implementation of TIP, approximately 50% of pediatric patients with SCD had an initial visit with an adult SCD medical provider within 6 months of high school graduation. All 37 graduates of our first 3 classes (2011–2013), 32 of whom stayed in the VCU catchment area, were seen for an initial visit in an adult clinic within 6 months of high school graduation (Fig.). Among the 32 VCU adult clinic patients, despite all of them making an initial adult clinic visit, 7 (22%) failed to revisit the adult sickle cell provider and were lost to follow-up. The remaining 25 patients (78%) have continued to receive regular care in the adult clinic.
Discussion
Lessons Learned from Assessment Results
A significant limitation of our draft TIP-RFT results is that the evaluations were not administered in an equivalent stage of participation for subjects. Regarding TIP-RFT independent living skills, the majority of patients had mastered instrumental activities of daily living (managing their money, holding a job, preparing their meals, making their own doctor’s appointments, and filling their own prescriptions).
Regarding TIP-RFT SCD healthcare knowledge and skills, only one-third of the patients knew their hemoglobin level. Only half of the patients knew anything about hydroxyurea, and only half knew about pregnancy complications from SCD.
Regarding TIP-RFT social support skills, we found signs of good social adjustment. We found that all of the patients had hobbies, at least two-thirds participated in activities at school or outside the home, and almost all of them had chores at home or a good social support system.
Regarding TIP-RFT feelings about moving to adult care, we found that patients worried about transition. We found timidity about transferring to the adult clinic. We found that only one-third of patients believed subjectively that they were ready for transition, that two-thirds of patients endorsed anxiety, that half endorsed fear, and that nearly one-third endorsed feeling anger or a sense of abandonment. We therefore targeted TIP program elements toward these feelings (eg, we provided pretransfer introductions to adult providers and tours of adult facilities).
From the Sickle Cell Stress Scale-Adolescent, we found that nearly one-third of patients worried strongly that their pain would not be controlled by their medication, two-thirds worried about long hospitalizations, and one-fourth strongly endorsed that death was always at the back of their minds. Higher reported SCD stress was found to be associated with lower scores on the validated TIP-RFT education and vocation planning scale. Although we had previously administered the Sickle Cell Stress Scale to a population with an older median age,25 some of the same worries were found among TIP participants and these older patients. Self-efficacy was good. Higher levels of self-efficacy have been related to fewer physical, psychological, and total symptoms among patients with SCD.27,29
Lessons Learned from Program Implementation
Even in a single institution with both willing pediatric and willing adult sickle cell specialty providers, setting up an SCD transition program takes time, energy, and funds. The first major hurdle to constructing TIP was obtaining funding to support the time of clinicians and administrative team members that was needed to construct the program. Without this funding, we would have been reduced to referring patients using a one-time physician-to-physician consultation model, accompanied by medical record transfer. With funding, TIP consisted of a far more elaborate hand off.
The second major hurdle to constructing the TIP was scheduling times when clinicians and administrative team members could meet to create a curriculum for patients and parents/guardians, decide on how to deploy the curriculum, and develop an evaluation metric to determine the success of the curriculum. The curriculum and methods/venues of deployment evolved through years of trial and error.
The third major hurdle to constructing the TIP was properly handing off patients and continuing to do so for years, despite turnover in personnel. Among other components, the TIP called for at least annual case discussions of graduating high school seniors by pediatric and adult team members. The pediatric physicians brought records and summarized for the adult care team their detailed observations about the patient’s biopsychosocial milieu, based on years of care of the patient, often from birth.
A deficit of our program was that we provided weak instruction to TIP participants in insurance options because insurance issues did not hamper our transition program. This likely hampered adjustment for patients leaving the VCU system.
Pediatric and Adult Models of Care Make Different Assumptions
Adult and pediatric providers learned about important differences in their models of care by working together in the TIP. The pediatric model of care typically involves parents in all of their childrens’ care. The adult model of care assumes patient autonomy—patients will develop their own social and other support systems, know their disease history and medical self-care, and advocate for themselves.
To accommodate and meld these models, adult providers encouraged parents to attend adult clinic visits and participate in their child’s care, even after the first year of adult clinical care. Providers began to accept parents as critical spokespeople for young adult children, just as they accepted patient advocates for older adults. Simultaneously, adult providers reinforced the need for youth to assume more responsibility for their own care.
Psychosocial Needs Remain High During the Transition Period, but Psychosocial Resources May Be Scarce for Adults with SCD
Our comprehensive pediatric sickle cell clinic had a dedicated social worker, a psychologist, and an educational consultant who provided educational and vocational assistance. There was a pediatric psychiatrist who worked closely with our psychologist and saw patients in our clinic once per month. Our adult clinic had no dedicated social worker, and access to adult psychology and psychiatry remained suboptimal. We realized quickly that medical transfer was a one-time event but that psychosocial transfer was an ongoing process. We secured grant funding to allow our young adult patients who received medical care at the adult sickle cell clinic to continue to use the services of our pediatric psychologist, educational consultant, and social worker. Although many of our young adult patients benefited from this service after medical transition, they were not used as heavily as they were before transition, possibly because these services were not directly embedded in the adult medical setting or because some patients had fewer psychosocial needs.
Ideally, SCD transition programs should employ a transition coordinator, an ombudsperson whose job it is to ensure that the transition curriculum is built and well implemented, that transfers of care occur smoothly and on time, and that posttransfer gaps in care are bridged. The pediatric-to-adult transfer of care for a patient with a lifelong chronic illness is the responsibility of both the pediatric and adult care teams. Our team quickly learned that a single responsible party was the most efficient way to bridge the pediatric and adult systems of care, to facilitate communication between pediatric and adult providers, to ensure that the pretransfer curriculum was evenly and consistently implemented for all willing patients and families, and to provide critical follow-up services just after the transfer of care, some of which were unforeseen.
This ombudsperson, a social worker by training, quickly realized that much of the didactic content originally delivered for adolescents ages 15 to 18 years old needed to be repeated posttransfer. The adult sickle cell program obtained funds to hire and test the efficacy of patient navigators assigned to patients 15 years and older to help them through the transition period.
Actual Transfer of Medical Care Should Be Conditional
Transfer of SCD care from a pediatric to an adult setting should only occur after readiness milestones are mutually agreed upon and achieved by the patient, family, and pediatric and adult care teams. Required milestones will vary for individual patients and should take into account the SCD history and patient’s current state of health, as well as the presence of willing adult providers.
Teaching About Transition of Care Must Be Repeated Pre- and Posttransfer of Care
As part of good pedagogy, lessons about transition of care taught early to patients and parents must be retaught often, even posttransfer of care.30 Lessons are best retained when they are salient and immediately applicable to the patient’s situation.31 For example, we taught patients with SCD and their families early about special education planning and emergency and pain planning. Knowledge about school accommodations for disabilities and special circumstances resulting from SCD such as 504 plans and/or individualized education plans only became salient for and immediately applicable to students in distress during final examinations in college, however. Similarly, patients’ needs for individualized opioid and pain management plans only became salient and immediately applicable when they were experiencing a painful crisis and encountered an outlying physician who was not familiar with their tolerance or preference for specific opioids.
Conclusions
We believe that our program results will be useful as others attempt to replicate such programs around the United States, but we are aware that system differences will prevent our results from generalizing to many SCD programs or healthcare systems in which SCD transition programs are needed. We hope, however, that the principles and lessons we learned will have broader application beyond Virginia and the TIP. We believe that these principles and lessons, accompanied by caring, flexible, and dedicated care team members, can often overcome even severe barriers to care transitions.
Key Points.
Pediatric-to-adult transition of care program in sickle cell disease required special adaptations of principles of general pediatric-to-adult transitions of care.
Early lessons learned were used to adapt the program early on and to develop and test a readiness for transition instrument.
Program outcomes suggest structural success including improved retention of patients transferred to adult care
Acknowledgments
W.R.S. has received compensation from Pfizer and Novartis. S.J. has received compensation from the Richmond Memorial Health Foundation. M.J.T. has received compensation from the Health Resources and Services Administration. The remaining authors did not report any financial relationships or conflicts of interest.
References
- 1.American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians, et al. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics 2011;128:182–200. [DOI] [PubMed] [Google Scholar]
- 2.Got Transition. Got transition toolkit. www.gottransition.org Accessed December 16, 2018.
- 3.American Society of Hematology. ASH transition toolkit. http://www.hematology.org/Advocacy/Policy-News/2016/5581.aspx Accessed December 16, 2018.
- 4.Scal P, Ireland M. Addressing transition to adult health care for adolescents with special health care needs. Pediatrics 2005;115:1607–1612. [DOI] [PubMed] [Google Scholar]
- 5.Romelczyk S, Homan S, Telfair J, et al. Healthcare coordination and transition for individuals with genetic conditions. Matern Child Health J 2015;19:2215–2222. [DOI] [PubMed] [Google Scholar]
- 6.DeBaun MR, Telfair J. Transition and sickle cell disease. Pediatrics 2012;130:926–935. [DOI] [PubMed] [Google Scholar]
- 7.Treadwell M, Telfair J, Gibson RW, et al. Transition from pediatric to adult care in sickle cell disease: establishing evidence-based practice and directions for research. Am J Hematol 2011;86:116–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bobo L, Miller ST, Smith WR, et al. Health perceptions and medical care opinions of inner-city adults with sickle cell disease or asthma compared with those of their siblings. South Med J 1989;82:9–12. [DOI] [PubMed] [Google Scholar]
- 9.Aisiku IP, Penberthy LT, Smith WR, et al. Patient satisfaction in specialized versus nonspecialized adult sickle cell care centers: the PiSCES study. J Natl Med Assoc 2007;99:886–890. [PMC free article] [PubMed] [Google Scholar]
- 10.Evensen CT, Treadwell MJ, Keller S, et al. Quality of care in sickle cell disease: cross-sectional study and development of a measure for adults reporting on ambulatory and emergency department care. Medicine (Baltimore) 2016;95:e4528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith WR,McClish DK,Lottenberg R, et al. Comparison of adult and adolescent quality of ambulatory and emergency care in sickle cell disease: ASCQ-Me and the SHIP-HU study. Blood 2017;130:2258. [Google Scholar]
- 12.Wang CJ, Kavanagh PL, Little AA, et al. Quality-of-care indicators for children with sickle cell disease. Pediatrics 2011;128:484–493. [DOI] [PubMed] [Google Scholar]
- 13.Kanter J, Dampier C, Agodoa I, et al. Quality of care in United States children with sickle cell anemia. Blood 2017;130:2098. [Google Scholar]
- 14.Bundy DG, Richardson TE, Hall M, et al. Association of guideline-adherent antibiotic treatment with readmission of children with sickle cell disease hospitalized with acute chest syndrome. JAMA Pediatr 2017;171:1090–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yawn BP, Buchanan GR, Afenyi-Annan AN, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA 2014;312:1033–1048. [DOI] [PubMed] [Google Scholar]
- 16.DeBaun MR. The challenge of creating an evidence-based guideline for sickle cell disease. JAMA 2014;312:1004–1005. [DOI] [PubMed] [Google Scholar]
- 17.McCavit TL, Zhang S, Ahn C, et al. Quality of care in hospitalizations for sickle cell disease in the U.S.: do low patient volumes mean higher mortality? Blood 2008;112:166. [Google Scholar]
- 18.Oyeku SO, Faro EZ. Rigorous and practical quality indicators in sickle cell disease care. Hematology Am Soc Hematol Educ Program 2017;2017:418–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sobota AE, Shah N, Mack JW. Development of quality indicators for transition from pediatric to adult care in sickle cell disease: a modified Delphi survey of adult providers. Pediatr Blood Cancer 2017;64. [DOI] [PubMed] [Google Scholar]
- 20.Treadwell M, Johnson S, Sisler I, et al. Development of a sickle cell disease readiness for transition assessment. Int J Adolesc Med Health 2016;28:193–201. [DOI] [PubMed] [Google Scholar]
- 21.Treadwell M, Johnson S, Sisler I, et al. Self-efficacy and readiness for transition from pediatric to adult care in sickle cell disease. Int J Adolesc Med Health 2016;28:381–388. [DOI] [PubMed] [Google Scholar]
- 22.Telfair J, Ehiri JE, Loosier PS, et al. Transition to adult care for adolescents with sickle cell disease: results of a national survey. Int J Adolesc Med Health 2004;16:47–64. [DOI] [PubMed] [Google Scholar]
- 23.Smith WR, Bovbjerg VE, Penberthy LT, et al. Understanding pain and improving management of sickle cell disease: the PiSCES study. J Natl Med Assoc 2005;97:183–193. [PMC free article] [PubMed] [Google Scholar]
- 24.McClish DK, Smith WR, Levenson JL, et al. Comorbidity, pain, utilization, and psychosocial outcomes in older versus younger sickle cell adults: the PiSCES project. Biomed Res Int 2017;2017:407–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith WR, McClish DK, Dahman BA, et al. Daily home opioid use in adults with sickle cell disease: the PiSCES project. J Opioid Manag 2015;11:243–253. [DOI] [PubMed] [Google Scholar]
- 26.Edwards R, Telfair J, Cecil H, et al. Reliability and validity of a self-efficacy instrument specific to sickle cell disease. Behav Res Ther 2000;38:951–963. [DOI] [PubMed] [Google Scholar]
- 27.Clay OJ, Telfair J. Evaluation of a disease-specific self-efficacy instrument in adolescents with sickle cell disease and its relationship to adjustment. Child Neuropsychol 2007;13:188–203. [DOI] [PubMed] [Google Scholar]
- 28.Smith WR, Godder K, Sisler I, et al. Readiness for transition from pediatric sickle cell care: exploratory analyses of domains of readiness and total scores. Blood 2010;116:1066. [Google Scholar]
- 29.Edwards R, Telfair J, Cecil H, et al. Self-efficacy as a predictor of adult adjustment to sickle cell disease: one-year outcomes. Psychosom Med 2001;63:850–858. [DOI] [PubMed] [Google Scholar]
- 30.Weibell CJ. Principles of learning: 7 principles to guide personalized, student-centered learning in the technology-enhanced, blended learning environment. https://principlesoflearning.wordpress.com. Published 2011 Accessed May 7, 2018.
- 31.Rumbaugh DM, King JE, Beran MJ, et al. A salience theory of learning and behavior: with perspectives on neurobiology and cognition. Int J Primatol 2007;28:973–996. [Google Scholar]


