Abstract
Greater propensity to seek care is critical for improving health of elderly individuals with multimorbidity. We used the Medicare Current Beneficiary Survey (2012) to assess propensity to seek care among community-dwelling elderly Medicare beneficiaries (≥ 65 yrs.; N=11,270) having (1) no physical or mental illness; (2) single physical or mental condition; (3) multimorbidity with physical conditions only; and (4) multimorbidity with both physical and mental conditions. As compared to multimorbidity with physical conditions, elderly with no multimorbidity were less likely (Adjusted Odds Ratio [95% CI]: 0.50 [0.36, 0.68]) and elderly with both physical and mental conditions were more likely (1.57 [1.28, 1.93]) to have a health problem for which they should have seen a doctor but did not. Further, elderly having a usual source of care were less likely (0.53 [0.37, 0.75]) to have a health problem for which they should have seen a doctor but did not. Multimorbidity is negatively associated with propensity to seek care. The presence of both chronic mental and physical conditions worsened propensity to seek care among elderly individuals. Future efforts to increase the awareness of receiving timely care and improve the access to care can enhance propensity to seek care among elderly individuals with multimorbidity.
Keywords: Multimorbidity, Care Seeking, Elderly Population, Physical and Mental Conditions
INTRODUCTION
The population of elderly individuals aged 65 years or older in the US is projected to double over the next few decades (Ortman, Velkoff, & Hogan, 2014). The aging population will also lead to an increase in the burden of chronic physical and mental health conditions as two-thirds of older adults have two or more chronic conditions or multimorbidity (Salive, 2013). The problem of multimorbidity is especially challenging when a patient has both chronic mental and physical conditions (Mercer, Gunn, Bower, Wyke, & Guthrie, 2012). The prevalence of mental health conditions is substantially higher among those with multiple physical illnesses and leads to poorer quality of life, higher cost of care, and higher disability and mortality (Iacovides & Siamouli, 2008; Katon, 2003; Merikangas et al., 2007; Naylor et al., 2012). One key reason for the lower quality of life and untreated chronic illnesses among elderly is their low propensity to seek care (PSC) (Garrido, Kane, Kaas, & Kane, 2011; Kessler, Berglund, Bruce, Koch, Laska, Leaf, Manderscheid, Rosenheck, Walters, & Wang, 2001a). The PSC is defined as patients’ willingness to contact their medical providers for their illnesses (Shaw, Brittain, Tansey, & Williams, 2008). A high PSC can lead to timely monitoring and appropriate treatment of elderly with multimorbidity. However, there is a lack of evidence on the PSC of elderly patients who have multiple chronic physical conditions with or without a mental illness.
Existing research has investigated the PSC among older adults with a single chronic condition such as depression, myocardial infarction, stroke, or urinary incontinence (Ho, Rumsfeld, Lyons, Every, & Magid, 2002; Howard et al., 2008; Kang, 2007; Li, Cai, Glance, & Mukamel, 2007; McKinley, Moser, & Dracup, 2000; Ricci et al., 2001; Sarkisian, Lee-Henderson, & Mangione, 2003). Elderly with depression or other psychological illness have been found to have negative attitudes towards mental illness (Segal, Coolidge, Mincic, & O’riley, 2005) and a low PSC (Garrido et al., 2011; Mojtabai, 2010; Phillips & Murrell, 1994). Other significant barriers to seeking treatment for mental illness include high cost, low perceived need of medical care (Taber, Leyva, & Persoskie, 2015), belief that the disease can be managed without professional help (Endicott, 1996b; Sareen et al., 2007), and belief that depression is a part of aging (Sarkisian et al., 2003). Among adults with myocardial infarction, a lower PSC was related to older age, the presence of diabetes mellitus, low perceived severity of symptoms, worry about troubling others, and fear of consequences of seeking help (McKinley et al., 2000). Also, lower income, no history of heart condition, and no history of stroke were associated with a lower PSC among older adults with stroke (Howard et al., 2008). Among women with urinary incontinence, age, quality of life scores, beliefs about available treatments, the severity of the disease, and embarrassment significantly affected their PSC (Koch, 2006).
Inconsistent findings have been reported by previous studies on racial disparities in the PSC. Conner et al. found that African Americans were more likely to have a higher personal stigma and a lower PSC as compared to Whites (Conner et al., 2010). However, a study by Shim et al. found that African Americans had a higher PSC for mental health than non-Hispanic Whites (Shim, Compton, Rust, Druss, & Kaslow, 2009). Studies exploring the gender differences in care-seeking have found that men have a lower PSC for a diverse set of health conditions (Galdas, Cheater, & Marshall, 2005; Mackenzie, Gekoski, & Knox, 2006; Möller-Leimkühler, 2002; Stevens et al., 2012). Other factors negatively affecting the PSC include saving money for emergencies (Jacob, Arnold, Hunleth, Greiner, & James, 2014) and higher social support (Phillips & Murrell, 1994).
The impact of having multiple chronic physical and mental conditions on the PSC of the elderly is largely unknown. As the US population continues to age, it is important to examine the association of multimorbidity with the PSC to effectively manage this highly prevalent clinical complexity. Identifying the factors that affect the PSC among elderly individuals with multimorbidity may help in creating programs for the appropriate utilization of health services and improve elderly individuals’ health outcomes. We used the ‘Behavioral Model for Vulnerable Populations’ (BMVP) as the theoretical framework for this study (Gelberg, Andersen, & Leake, 2000a). This model specifically addresses the PSC of vulnerable populations such as elderly individuals who are at higher risk for illness (Aday, 1994; Andersen, 1995). The BMVP has been used in previous studies to examine the healthcare utilization of vulnerable populations such as patients with multimorbidity and homeless individuals (Gelberg, Andersen, & Leake, 2000b; Small, 2010; Stein, Andersen, & Gelberg, 2007). According to this framework, an individual’s PSC is influenced by three factors: a) predisposing, b) enabling, and c) need factors (Gelberg, Andersen, & Leake, 2000a; Kang, 2007). Predisposing factors refer to an individual’s characteristics that incline him/her towards seeking healthcare such as demographic, education, employment, and personal health behavior variables. Enabling factors represent the means that facilitate or impede the care seeking behavior, which include personal and community resources. Personal resources consist of personal income, health insurance, usual source of care, marital status, and whether the patient lives alone. Community resources include area characteristics such as census region and metropolitan area. Lastly, need factors refer to the presence of a disease or illness which is the most immediate cause for seeking healthcare. Need factors include chronic conditions, perceived health and functional status, body mass index, and worry about personal health.
In this study, we utilized the Medicare Current Beneficiary Survey (MCBS), a nationally representative survey of elderly Medicare beneficiaries, to analyze the association of multimorbidity with the PSC of elderly individuals (Centers for Medicare & Medicaid Services. Medicare Current Beneficiary Survey (MCBS)). We examined the PSC among elderly individuals having both chronic physical and mental conditions as compared to elderly having multiple chronic physical conditions without any mental illness. We further examined the elderly individuals’ self-reported reasons for having a low PSC.
METHODS
Study Design and Data Source
We conducted a retrospective cross-sectional analysis of the MCBS 2012 for this study. The MCBS is a continuous multipurpose survey of a nationally representative sample of Medicare beneficiaries. The survey represents the total Medicare population in the US, which includes beneficiaries who are aged or disabled, enrolled in managed care or fee for service (FFS), and living in a facility or community. Computer-assisted personalized interviews (CAPI) are conducted every four months with the beneficiary or a proxy chosen by the beneficiary. The MCBS data is released in two modules each year: Access to care (AC) and Cost and Use (CU) modules. The AC module consists of data from the survey and includes information on Medicare beneficiaries’ sociodemographic characteristics, health status, and access to and satisfaction with care. The CU module includes data from both the survey and the participants’ healthcare administrative claims. The CU module consists of information related to cost, use, and sources of payment for healthcare services. Further details of the MCBS are described elsewhere (Centers for Medicare & Medicaid Services. Medicare Current Beneficiary Survey (MCBS)). We utilized each participant’s responses to survey in the AC module of the MCBS 2012 for this study.
Participants
In our study, we included community-dwelling Medicare beneficiaries who were aged 65 years and above, were continuously enrolled in Medicare throughout the calendar year, and who participated in the 2012 round of MCBS (N=11,555). We excluded individuals with missing data for multimorbidity (N=26) or PSC (N=259). Our final study sample size consisted of 11,270 elderly Medicare beneficiaries.
Outcome Measure: Propensity to Seek Care
The primary outcome of this study was the elderly Medicare beneficiaries’ PSC. We utilized the following survey item from the MCBS to measure the PSC: ‘During this year, did you have any health problem or condition about which you think you should have seen a doctor or other medical person, but did not?’ (DR_HLTH) (Murgolo, 2002). The participants responded to this survey item on a binary response scale (yes/no). The elderly who answered ‘yes’ to this question were considered to have a low PSC, while those who answered ‘no’ were considered to have a high PSC. We also examined the elderly Medicare beneficiaries’ reasons for having a low PSC. Elderly participants who answered ‘true’ to DR_HLTH were asked the following survey question in the MCBS: ‘Which of these was the main reason you did not see a doctor about this condition/these conditions during this year?’ We examined the participants’ responses to this survey question to identify the most common reasons for having a low PSC.
Independent Variables
We utilized the theoretical framework of BMVP to identify elderly participants’ predisposing, enabling, and need characteristics that might influence their PSC. We used elderly participants’ responses to the survey items from the AC module of MCBS 2012 to measure these variables.
Predisposing factors.
The predisposing factors included age (65–69, 70–74, 75–79, and >80 yrs.), sex (male and female), race/ethnicity (Non-Hispanic White, Non-Hispanic African American, and other race), education (< high school, high school, and college), employment status (currently employed or not), and smoking status (never smoked, past smoker, and current smoker). The ‘other race’ category for race/ethnicity included Hispanic/Latino, Asian, Native Hawaiian or Pacific Islander, American Indian or Alaska Native, more than one, or others.
Enabling factors.
The enabling factors consisted of annual personal income (<$20k, $20–30k, $30–50k, and >$50k), insurance status, marital status (married or not married), living status (lives alone or not), access to care, and external environmental characteristics. Insurance status included Health Maintenance Organization (HMO) enrollment, Medicaid insurance, and private insurance. The participants in the MCBS indicated the number of people living in their household. We used this information to identify elderly individuals who live alone. Access to care included a usual source of care and trouble getting needed healthcare. We used the following survey item to assess usual source of care: ‘Is there a particular medical person or a clinic you usually go to when you are sick or for advice about your health (yes/no)?’ The trouble in getting needed care was measured by the following survey item: ‘Did you face any trouble in getting health care needs met during the previous year (yes/no)?’ The external environmental characteristics included metropolitan area (yes/no) and geographic region (Northeast, Midwest, South, and West).
Need factors.
The need factors included multimorbidity, perceived general health status, perceived functional status, body mass index, and worry about personal health. We examined participants’ having been told by a doctor that they had a chronic condition to assess the presence of multimorbidity. We selected chronic physical and mental conditions based on the conceptual model developed by Goodman et al. to define and analyze chronic conditions for research and policy (Goodman, 2013). The chronic physical conditions included bone and joint diseases (rheumatoid arthritis, non-rheumatoid arthritis, osteoporosis, or broken hip), cancer (skin or any other cancer), diabetes (type 1 or type 2), heart disease (coronary heart disease, heart failure, problem with heart valves or rhythm, myocardial infarction, or any other heart condition), hypertension, paralysis, respiratory diseases (asthma, chronic obstructive pulmonary disease, or emphysema), and stroke. The chronic mental conditions consisted of depression or any other mental disorder. Based on the presence of these chronic physical and mental health conditions, we defined four multimorbidity categories: (a) No PI/MI: no chronic condition; (b) 1PI/1MI: single chronic physical or mental condition; (c) MM-PI: two or more chronic physical conditions but no mental condition; and (d) MM-PI&MI: both chronic physical and mental conditions.
We measured general health status by using participants’ self-perceived general health status as compared to others of the same age (excellent/very good, good, or fair/poor). We measured functional health status by examining participants’ reported difficulty with activities of daily living (ADL) including difficulty walking, eating, bathing, dressing, getting in or out of bed or chair, or using the toilet. We classified participants’ difficulty with ADL in three categories: (a) No ADL, (b) 1–2 ADL, and (c) 3–6 ADL. The body mass index (BMI) categories included underweight/normal, overweight, and obese/morbid obese. We measured elderly participants’ worry about personal health by utilizing their responses to the survey item, ‘You worry about your health more than other people of your age (true/false)’.
Statistical Analysis
We examined the unadjusted associations of participants’ predisposing, enabling, and need factors with elderly individuals’ PSC by using chi-square tests. We then conducted multivariate logistic regression analysis of the PSC. In the multivariate logistic regression model, we did not include the variables which were conceptually similar to and highly correlated with other variables in predisposing, enabling, and need constructs of BMVP. We did not include perceived general health status, perceived functional status and body mass index in the multivariate models because they were conceptually similar to and highly correlated with multimorbidity (p<.0001 for all). We also removed Medicaid insurance, lives alone, and trouble getting needed care, because they were conceptually similar to and highly correlated with annual income, marital status, and usual source of care, respectively (p<.0001 for all). We used the MCBS sampling weights for all the statistical analyses to account for the complex sampling procedure of the MCBS and for producing nationally representative estimates for Medicare beneficiaries. We used Statistical Analysis System software version 9.3 for all the data analyses (SAS institute, SAS system for windows, SAS institute, cary, NC, USA, 2009.)
RESULTS
Study Sample Characteristics
Of 11,270 elderly Medicare beneficiaries, 12.9% of elderly individuals had No PI/MI, 26.4% had 1PI/1MI, 49.7% had MM-PI, and 11.0% had MM-PI&MI (Table 1). The majority were Non-Hispanic White (78.0%), lived in a metropolitan area (77.4%), were not currently employed (84.5%), were not enrolled in an HMO (65.8%), did not have Medicaid insurance (87.5%), did not live alone (71.5%), and did not have limitations in ADL (67.6%) (Table 2). Most elderly beneficiaries had a usual source of care (96.1%) and did not face trouble in getting needed care (96.2%). Overall, a majority of elderly beneficiaries had high PSC. Only 8.6% of the beneficiaries agreed that during the past year, they had a condition for which they should have seen a doctor, but did not.
Table 1.
Weighted Percentages for Multimorbidity among Elderly Medicare Beneficiaries. Medicare Current Beneficiary Survey, 2012.
| No PI/MI 12.9% | 1PI/1MI 26.4% | MM-PI 49.7% | MM-PI&MI 11.0% | X2, p-value | |
|---|---|---|---|---|---|
| Weighted Row% | |||||
| Predisposing factors | |||||
| Sex | <.001 | ||||
| Female | 10.3 | 25.9 | 50.6 | 13.3 | |
| Male | 16.2 | 27.0 | 48.7 | 8.1 | |
| Age group | <.001 | ||||
| 65–69 yrs. | 17.3 | 28.4 | 41.9 | 12.4 | |
| 70–74 yrs. | 12.6 | 26.5 | 50.5 | 10.5 | |
| 75–79 yrs. | 11.1 | 25.3 | 53.9 | 9.7 | |
| >80 yrs. | 9.8 | 24.9 | 54.6 | 10.8 | |
| Race/Ethnicity | <.001 | ||||
| Non-Hispanic White | 13.2 | 27.4 | 48.5 | 11.0 | |
| Non-Hispanic African American | 10.3 | 21.3 | 59.5 | 8.9 | |
| Other race† | 12.5 | 23.8 | 51.4 | 12.3 | |
| Education | <.001 | ||||
| < High school | 9.8 | 19.7 | 56.3 | 14.2 | |
| High school | 12.6 | 26.2 | 50.4 | 10.8 | |
| ≥ College | 14.5 | 29.6 | 46.3 | 9.5 | |
| Currently employed | <.001 | ||||
| Yes | 18.5 | 33.6 | 42.0 | 5.9 | |
| No | 11.9 | 25.1 | 51.2 | 11.9 | |
| Enabling factors | |||||
| Smoking status | <.001 | ||||
| Current smoker | 15.0 | 24.6 | 43.6 | 16.7 | |
| Past smoker | 11.7 | 25.2 | 52.9 | 10.2 | |
| Never smoked | 13.8 | 28.2 | 47.6 | 10.5 | |
| Annual personal income | <.001 | ||||
| <20k | 9.5 | 20.4 | 55.2 | 14.9 | |
| 20–30k | 11.5 | 27.2 | 49.9 | 11.4 | |
| 30–50k | 12.5 | 28.4 | 48.9 | 10.1 | |
| >50k | 16.4 | 31.1 | 45.1 | 7.5 | |
| Missing | 23.1 | 24.4 | 45.0 | 7.5 | |
| HMO enrollment | .014 | ||||
| Yes | 11.2 | 27.3 | 50.6 | 10.9 | |
| No | 13.8 | 25.9 | 49.3 | 11.0 | |
| Medicaid insurance | <.001 | ||||
| Yes | 6.3 | 16.4 | 57.9 | 19.4 | |
| No | 13.8 | 27.8 | 48.6 | 9.8 | |
| Private insurance | <.001 | ||||
| Yes | 13.2 | 28.6 | 49.0 | 9.2 | |
| No | 12.5 | 24.0 | 50.6 | 12.9 | |
| Marital status | <.001 | ||||
| Married | 13.9 | 27.8 | 49.0 | 9.3 | |
| Not marriedα | 11.6 | 24.6 | 50.7 | 13.2 | |
| Lives alone | .003 | ||||
| Yes | 12.0 | 26.1 | 49.0 | 12.9 | |
| No | 13.2 | 26.5 | 50.0 | 10.2 | |
| External environment | |||||
| Metropolitan area | .325 | ||||
| Yes | 13.1 | 26.8 | 49.1 | 11.0 | |
| No | 12.1 | 25.0 | 51.9 | 11.0 | |
| Geographical region | .038 | ||||
| Northeast | 13.6 | 26.6 | 48.7 | 11.1 | |
| Midwest | 13.1 | 27.5 | 49.5 | 9.9 | |
| South | 12.3 | 24.1 | 52.0 | 11.6 | |
| West | 13.2 | 29.0 | 46.9 | 10.9 | |
| Access to care | |||||
| Usual source of care | <.001 | ||||
| Yes | 11.4 | 26.4 | 51.0 | 11.3 | |
| No | 50.9 | 26.1 | 19.5 | 3.5 | |
| Trouble getting needed care | <.001 | ||||
| Yes | 9.2 | 17.7 | 51.4 | 21.7 | |
| No | 13.0 | 26.7 | 49.7 | 10.5 | |
| Need factors | |||||
| General health status | <.001 | ||||
| Excellent/Very good | 18.8 | 34.0 | 40.6 | 6.5 | |
| Good | 8.3 | 21.4 | 59.1 | 11.2 | |
| Fair/Poor | 3.4 | 12.8 | 60.6 | 23.2 | |
| Worry about health | <.001 | ||||
| Yes | 6.1 | 16.4 | 55.2 | 22.2 | |
| No | 14.4 | 28.6 | 48.5 | 8.6 | |
| Functional status | <.001 | ||||
| None | 17.0 | 31.1 | 44.8 | 7.0 | |
| 1–2 ADL | 5.1 | 18.3 | 60.5 | 16.1 | |
| 3–6 ADL | 2.5 | 12.4 | 58.7 | 26.4 | |
| Body mass index | <.001 | ||||
| Underweight/Normal | 17.6 | 30.7 | 42.6 | 9.1 | |
| Overweight | 12.5 | 27.1 | 49.7 | 10.8 | |
| Obese/Morbid obese | 7.2 | 19.9 | 59.1 | 13.8 | |
| Missing | 15.4 | 26.2 | 48.9 | 9.5 | |
Notes. Multimorbidity categories: 1) No PI/MI = no chronic condition; 2) 1PI/1MI = single physical or mental condition; 3) MM-PI = two or more physical conditions but no mental condition; 4) MM-PI&MI = both chronic physical and mental conditions.
ADL = activities of daily living; HMO = health maintenance organization; X2 = Chi-square test.
Hispanic/Latino, Asian, Native Hawaiian or Pacific Islander, American Indian or Alaska Native, more than one, or others;
Widowed/Divorced/S eparated/N ever married.
Table 2.
Weighted Percentages and Adjusted Odds Ratios for Propensity to Seek Care among Elderly Medicare Beneficiaries. Medicare Current Beneficiary Survey, 2012.
| Total | Low Propensity to Seek Care | |||||
|---|---|---|---|---|---|---|
| N = 11,270 | Yes | No | X2, p-value | AOR [95% CI] | Sig. | |
| Predisposing factors | ||||||
| Gender | .150 | |||||
| Female | 55.8 | 9.0 | 91.0 | 1.04 [0.88, 1.22] | ||
| Male | 44.2 | 8.2 | 91.8 | Ref. | ||
| Age group | .004 | |||||
| 65–69 yrs. | 28.9 | 10.1 | 89.9 | Ref. | ||
| 70–74 yrs. | 25.6 | 8.6 | 91.4 | 0.87 [0.70, 1.08] | ||
| 75–79 yrs. | 18.8 | 8.1 | 91.9 | 0.76 [0.60, 0.95] | * | |
| >80 yrs. | 26.6 | 7.4 | 92.6 | 0.68 [0.55, 0.84] | *** | |
| Race/Ethnicity | <.001 | |||||
| Non-Hispanic White | 78.0 | 7.7 | 92.3 | Ref. | ||
| Non-Hispanic African American | 7.8 | 12.1 | 87.9 | 1.24 [0.98, 1.58] | ||
| Other race† | 14.1 | 11.8 | 88.2 | 1.27 [0.98, 1.64] | ||
| Education | <.001 | |||||
| < High school | 20.7 | 11.5 | 88.5 | Ref. | ||
| High school | 34.4 | 8.9 | 91.1 | 1.10 [0.90, 1.34] | ||
| ≥ College | 45.0 | 7.2 | 92.8 | 0.96 [0.78, 1.18] | ||
| Currently employed | .085 | |||||
| Yes | 15.5 | 7.3 | 92.7 | 1.02 [0.79, 1.31] | ||
| No | 84.5 | 8.9 | 91.1 | Ref. | ||
| Smoking status | <.001 | |||||
| Current smoker | 9. 8 | 12.3 | 87.7 | Ref. | ||
| Past smoker | 48.3 | 8.5 | 91.5 | 0.83 [0.65, 1.07] | ||
| Never smoked | 42.0 | 7.9 | 92.1 | 0.72 [0.56, 0.94] | * | |
| Enabling factors | ||||||
| Annual personal income | <.001 | |||||
| <20k | 28.3 | 13.2 | 86.8 | Ref. | ||
| 20–30k | 20.0 | 8.8 | 91.2 | 0.75 [0.60, 0.94] | * | |
| 30–50k | 22.2 | 6.6 | 93.4 | 0.60 [0.47, 0.75] | *** | |
| >50k | 25.0 | 5.9 | 94.1 | 0.59 [0.44, 0.77] | *** | |
| Missing | 4.5 | 5.5 | 94.5 | |||
| HMO enrollment | .847 | |||||
| Yes | 34.2 | 8.6 | 91.4 | 0.89 [0.75, 1.06] | ||
| No | 65.8 | 8.7 | 91.3 | Ref. | ||
| Medicaid insurance | <.001 | |||||
| Yes | 12.5 | 14.9 | 85.1 | |||
| No | 87.5 | 7.8 | 92.2 | |||
| Private insurance | <.001 | |||||
| Yes | 53.4 | 7.1 | 92.9 | 0.87 [0.72, 1.07] | ||
| No | 46.6 | 10.4 | 89.6 | Ref. | ||
| Marital status | <.001 | |||||
| Married | 56.8 | 7. 7 | 92.3 | Ref. | ||
| Not marriedα | 43.2 | 9.9 | 90.1 | 0.98 [0.81, 1.19] | ||
| Lives alone | .552 | |||||
| Yes | 28.5 | 8. 9 | 91.1 | |||
| No | 71.5 | 8.5 | 91.5 | |||
| External environment | ||||||
| Metropolitan area | .754 | |||||
| Yes | 77.4 | 8.6 | 91.4 | 1.05 [0.82, 1.34] | ||
| No | 22.6 | 8.9 | 91.1 | Ref. | ||
| Geographic region | .040 | |||||
| Northeast | 18.0 | 7. 9 | 92.1 | Ref. | ||
| Midwest | 22.7 | 8.5 | 91.5 | 1.13 [0.87, 1.46] | ||
| South | 37.8 | 9.8 | 90.2 | 1.17 [0.93, 1.48] | ||
| West | 21.5 | 7.5 | 92.5 | 0.93 [0.68, 1.26] | ||
| Access to care | ||||||
| Usual source of care | .004 | |||||
| Yes | 96.1 | 8.5 | 91.5 | Ref. | *** | |
| No | 3.9 | 12.8 | 87.2 | 1.90 [1.33, 2.71] | ||
| Trouble getting needed care | <.001 | |||||
| Yes | 3.8 | 30.6 | 69.4 | - | ||
| No | 96.2 | 7.8 | 92.2 | |||
| Need factors | ||||||
| Multimorbidity | <.001 | |||||
| No PI/MI | 12.9 | 5. 1 | 94.9 | Ref. | ||
| 1PI/1MI | 49.7 | 9.3 | 90.7 | 1.42 [1.02, 1.97] | *** | |
| MM-PI | 26.4 | 6.1 | 93.9 | 2.02 [1.47, 2.76] | *** | |
| MM-PI&MI | 11.0 | 15.8 | 84.2 | 3.17 [2.25, 4.46] | *** | |
| General health status | <.001 | - | ||||
| Excellent/Very good | 52.5 | 5. 6 | 94.4 | |||
| Good | 28.8 | 8.8 | 91.2 | |||
| Fair/Poor | 18.7 | 16.6 | 83.4 | |||
| Worry about health | <.001 | |||||
| Yes | 17.0 | 14.5 | 85.5 | 1.54 [1.29, 1.83] | *** | |
| No | 83.0 | 7.3 | 92.7 | Ref. | ||
| Functional status | <.001 | - | ||||
| None | 67.6 | 5.8 | 94.2 | |||
| 1–2 ADL | 22.9 | 13.1 | 86.9 | |||
| 3–6 ADL | 9.6 | 17.8 | 82.2 | |||
| Body mass index | .002 | - | ||||
| Underweight/Normal | 33.7 | 7. 4 | 92.6 | |||
| Overweight | 36.8 | 8.5 | 91.5 | |||
| Obese/Morbid obese | 26.3 | 10.3 | 89.7 | |||
| Missing | 3.2 | 10.1 | 89.9 | |||
Notes. AOR = Adjusted odds ratio of agreeing with the survey item after adjusting for gender, age, race, education, employment status, smoking status, income, health maintenance organization enrollment, private insurance, marital status, metropolitan area, region, usual source of care, multimorbidity, and worry about personal health. Low propensity to seek care: Those who responded ‘yes’ to the question: “During this year, did you have any health problem or condition about which you think you should have seen a doctor or other medical person, but did not?” Multimorbidity categories: 1) No PI/MI = no chronic condition; 2) 1PI/1MI = single physical or mental condition; 3) MM-PI = two or more physical conditions but no mental condition; 4) MM-PI&MI = both chronic physical and mental conditions.
ADL = activities of daily living; HMO = health maintenance organization; Ref. = reference group; Sig. = statistical significance.
Hispanic/Latino, Asian, Native Hawaiian or Pacific Islander, American Indian or Alaska Native, more than one, or others;
Widowed/Divorced/Separated/Never married; X2 = Chi-square test.
p < .001.
p < .01.
p < .05.
Multimorbidity and Propensity to Seek Care
The presence and type of multimorbidity had a significant association with the PSC among elderly Medicare beneficiaries. Elderly individuals having MM-PI&MI were more likely to have a health condition for which they should have seen a doctor but did not, as compared to those with MM-PI. Further, elderly with No PI/MI were significantly less likely to have a health condition for which they should have seen a doctor but did not, as compared to those with MMPI (Table 2). Other factors significantly associated with a high PSC included higher age, non-smoking status, higher income, having a usual source of care, and lower worry about personal health (Table 2). We did not find a significant association of sex and race with propensity to seek care. Further, there was no significant interaction between multimorbidity and sex and race for propensity to seek care.
Reasons for Low Propensity to Seek Care
Low perceived severity of illness was the most common reason (35.7%) among elderly beneficiaries for having a health condition for which they should have seen a doctor but did not (Figure 1). Other reasons for a low PSC among elderly included the high cost of care (12.4%), belief that doctor could not help with the problem (11.8%), time/schedule or personal conflicts (11.0%), trouble finding or getting to a doctor (7.0%), fear of knowing the illness (6.6%), and non-acceptance of insurance by the doctor (1.6%). About 14.0% of the beneficiaries cited other reasons for a low PSC. Other reasons for low PSC were not available from the MCBS, and hence we could not report them in this study.
Figure 1.
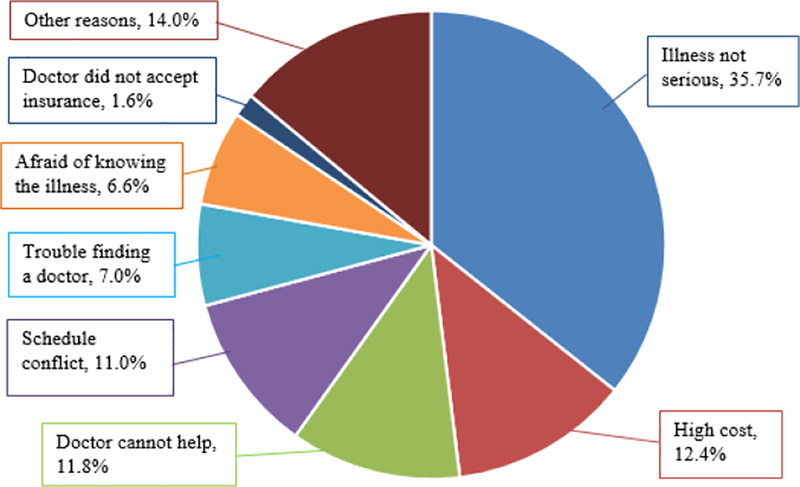
Elderly Medicare Beneficiaries’ Reasons for Low Propensity to Seek Care. Medicare Current Beneficiary Survey, 2012.
DISCUSSION
Our study investigated the association between multimorbidity and the PSC among a nationally representative sample of elderly in the US. There is a lack of appropriate clinical guidelines for elderly with multiple chronic physical and mental conditions. Improving the PSC can play an important role in increasing the quality of care of these elderly patients. Elderly with multimorbidity account for high utilization of healthcare (Iacovides & Siamouli, 2008; Katon, 2003; Merikangas et al., 2007; Naylor C, 2012). Delay in seeking care can lead to worsening of chronic conditions and hence higher hospitalizations and cost of care in the future. Understanding the factors that affect the PSC among elderly with multimorbidity is an important step towards reducing the burden of this clinical complexity.
We found that elderly with multimorbidity had a lower PSC than those having no chronic condition. We also found differences in the PSC by the type of multimorbidity. Elderly individuals having both chronic mental and physical conditions had a lower PSC as compared to those with multiple chronic physical conditions without any mental illness. Our study results expand the findings of previous studies that found a lower PSC among elderly with single chronic mental illness (Conner et al., 2010; Corrigan, 2004; Segal et al., 2005). The personal and social stigma attached to mental illness may be responsible for a lower PSC among elderly having both chronic mental and physical conditions (Endicott, 1996a; Mojtabai, Olfson, & Mechanic, 2002; Mojtabai, 2010; Sareen et al., 2007; Taber et al., 2015). Better diagnosis and communication regarding mental health issues during the visit for chronic physical conditions can improve the PSC of elderly who have both mental and physical conditions.
Two common reasons for low PSC among elderly were low perceived severity of the illness and low perceived effectiveness of seeking care from the doctor, which are consistent with previous studies among elderly with a single chronic condition (Garrido et al., 2011; Kessler, Berglund, Bruce, Koch, Laska, Leaf, Manderscheid, Rosenheck, Walters, & Wang, 2001b). There is a need to increase elderly individuals’ understanding of the severity of various chronic conditions and the importance of seeking care from their provider. Our study results also suggest that increasing the access to care for elderly can further improve their PSC. Some issues regarding access to care included difficulty finding a doctor, conflict of schedule with the doctor, and high cost of care. Better availability of doctors, higher acceptability of insurance, and lower costs of care can greatly increase PSC among elderly, especially those with multimorbidity.
An interesting finding of our study was that elderly who had higher worry regarding their personal health had significantly lower PSC. We further examined the reasons for low PSC among elderly individuals who had higher worry for their personal health. We found that those with higher worry were more likely to be afraid of finding about their illness (p = 0.003). The fear of finding about the illness may explain the failure to seek care among elderly who worry about their health more than others of their age. Future interventions to target such fears may be effective in improving the PSC among elderly.
Even though multimorbidity was a barrier to PSC, we found that the PSC of elderly increased with age. Our study results indicate that elderly with greater age (≥75 years) were more likely to visit a physician for their conditions as compared to elderly with age between 66–69 years, which is a positive finding of our study. Further, non-smokers had a higher PSC than current smokers. This result is concerning as smoking increases the risk of cardio-vascular conditions. Future interventions should target current and past smokers to increase their PSC. Our study findings should be interpreted in the context of some limitations. We utilized participants’ self-reported measures of chronic mental and physical conditions. However, it should be noted that self-reported measures have been routinely used for estimating the health and cost burden of chronic conditions (Reeves et al., 2011). Also, the MCBS uses special interview procedures such as CAPI, surveys Medicare beneficiaries at relatively short intervals, and verifies the survey information with medical claims to minimize recall bias (Sample, 1994). This study used a cross-sectional design and hence the study results do not suggest causality between multimorbidity and PSC. Our study included a large sample of Medicare beneficiaries with or without multimorbidity. Large sample size can often lead to inflated p-values. Our study results should be interpreted in conjunction with the provided effect sizes (odds ratios) and confidence intervals, which are not directly affected by the sample size (Lantz, 2013). Despite some limitations, our study has many strengths. We used participants’ responses to a question which directly assessed their PSC. Such direct measures of PSC are more accurate than indirect measures used in some of the previous studies (Codony et al., 2015; Mojtabai et al., 2002). We utilized the MCBS which is a valid multipurpose survey of Medicare beneficiaries. Also, our study included a large nationally representative sample of Medicare beneficiaries, and the study results can be generalized to elderly non-institutionalized beneficiaries in the US.
CONCLUSION
Multiple chronic conditions, also known as multimorbidity, are highly prevalent among elderly individuals in the US. However, there is a lack of research on the association of type of multimorbidity with the PSC of the elderly population. We found that the elderly having a mental condition in addition to multiple chronic physical conditions had lower PSC than those with multiple physical conditions without any mental illness. We also found that access to care was highly associated with the PSC, as elderly having a usual source of care had higher PSC. The two common reasons cited by elderly for low PSC included low perceived severity of illness and low perceived effectiveness of seeking care from a doctor. Other common reasons for having a low PSC included high cost of care, trouble finding or getting to a doctor, schedule conflict, fear of finding about the illness, and non-acceptance of insurance by the doctor. Our study findings highlight the need to create awareness regarding timely chronic care and the importance of contacting a doctor for chronic conditions. Improving the access to care can also increase the PSC among elderly individuals with multimorbidity.
Contributor Information
Rahul Garg, West Virginia University.
Chan Shen, University of Texas, MD Anderson Cancer Center.
Nethra Sambamoorthi, Northwestern University.
Usha Sambamoorthim, West Virginia University.
REFERENCES
- Aday LA (1994). Health status of vulnerable populations. Annual Review of Public Health, 15(1), 487–509. [DOI] [PubMed] [Google Scholar]
- Andersen RM (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, , 1–10. [PubMed] [Google Scholar]
- Centers for medicare & medicaid services. medicare current beneficiary survey (MCBS). Retrieved from https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS/index.html?redirect=/MCBS
- Codony M, Alonso J, Almansa J, Bernert S, Giovanni de Girolamo M, de Graaf R, … Kessler RC (2015). Perceived need for mental health care and service use among adults in western europe: Results of the ESEMeD project. Psychiatric Services, [DOI] [PubMed] [Google Scholar]
- Conner KO, Copeland VC, Grote NK, Koeske G, Rosen D, Reynolds CF, & Brown C (2010). Mental health treatment seeking among older adults with depression: The impact of stigma and race. The American Journal of Geriatric Psychiatry, 18(6), 531–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan P (2004). How stigma interferes with mental health care. American Psychologist, 59(7), 614. [DOI] [PubMed] [Google Scholar]
- Endicott J (1996a). Barriers to seeking treatment for major depression. Depression and Anxiety, 4(6), 273–278. [DOI] [PubMed] [Google Scholar]
- Endicott J (1996b). Barriers to seeking treatment for major depression. Depression and Anxiety, 4(6), 273–278. [DOI] [PubMed] [Google Scholar]
- Galdas PM, Cheater F, & Marshall P (2005). Men and health help-seeking behaviour: Literature review. Journal of Advanced Nursing, 49(6), 616–623. [DOI] [PubMed] [Google Scholar]
- Garrido MM, Kane RL, Kaas M, & Kane RA (2011). Use of mental health care by Community-Dwelling older adults. Journal of the American Geriatrics Society, 59(1), 50–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelberg L, Andersen RM, & Leake BD (2000a). The behavioral model for vulnerable populations: Application to medical care use and outcomes for homeless people. Health Services Research, 34(6), 1273–1302. [PMC free article] [PubMed] [Google Scholar]
- Gelberg L, Andersen RM, & Leake BD (2000b). The behavioral model for vulnerable populations: Application to medical care use and outcomes for homeless people. Health Services Research, 34(6), 1273–1302. [PMC free article] [PubMed] [Google Scholar]
- Goodman RA (2013). Defining and measuring chronic conditions: Imperatives for research, policy, program, and practice. Preventing Chronic Disease, 10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho PM, Rumsfeld JS, Lyons E, Every NR, & Magid DJ (2002). Lack of an association between medicare supplemental insurance and delay in seeking emergency care for patients with myocardial infarction. Annals of Emergency Medicine, 40(4), 381–387. [PubMed] [Google Scholar]
- Howard VJ, Lackland DT, Lichtman JH, McClure LA, Howard G, Wagner L, … Gomez CR (2008). Care seeking after stroke symptoms. Annals of Neurology, 63(4), 466–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacovides A, & Siamouli M (2008). Comorbid mental and somatic disorders: An epidemiological perspective. Current Opinion in Psychiatry, 21(4), 417–421. doi: 10.1097/YC0.0b013e328303ba42 [doi] [DOI] [PubMed] [Google Scholar]
- Jacob R, Arnold LD, Hunleth J, Greiner KA, & James AS (2014). Daily hassles’ role in health seeking behavior among low-income populations. American Journal of Health Behavior, 38(2), 297–306. doi: 10.5993/AJHB.38.2.15 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Y (2007). Predictors of help-seeking among community-dwelling korean american women with urinary incontinence ProQuest. [Google Scholar]
- Katon WJ (2003). Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biological Psychiatry, 54(3), 216–226. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Bruce ML, Koch JR, Laska EM, Leaf PJ, … Wang PS (2001a). The prevalence and correlates of untreated serious mental illness. Health Services Research, 36(6 Pt 1), 987–1007. [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Bruce ML, Koch JR, Laska EM, Leaf PJ, … Wang PS (2001b). The prevalence and correlates of untreated serious mental illness. Health Services Research, 36(6 Pt 1), 987–1007. [PMC free article] [PubMed] [Google Scholar]
- Koch LH (2006). Help-Seeking behaviors of women with urinary incontinence: An integrative literature review. Journal of Midwifery & Women’s Health, 51(6), e39–e44. [DOI] [PubMed] [Google Scholar]
- Lantz B (2013). The large sample size fallacy. Scandinavian Journal of Caring Sciences, 27(2), 487–492. [DOI] [PubMed] [Google Scholar]
- Li Y, Cai X, Glance LG, & Mukamel DB (2007). Gender differences in healthcare-seeking behavior for urinary incontinence and the impact of socioeconomic status: A study of the medicare managed care population. Medical Care, 45(11), 1116–1122. doi: 10.1097/MLR.0b013e31812da820 [doi] [DOI] [PubMed] [Google Scholar]
- Mackenzie C, Gekoski W, & Knox V (2006). Age, gender, and the underutilization of mental health services: The influence of help-seeking attitudes. Aging and Mental Health, 10(6), 574–582. [DOI] [PubMed] [Google Scholar]
- McKinley S, Moser DK, & Dracup K (2000). Treatment-seeking behavior for acute myocardial infarction symptoms in north america and australia. Heart & Lung: The Journal of Acute and Critical Care, 29(4), 237–247. [DOI] [PubMed] [Google Scholar]
- Mercer SW, Gunn J, Bower P, Wyke S, & Guthrie B (2012). Managing patients with mental and physical multimorbidity. BMJ (Clinical Research Ed.), 345, e5559–e5559. doi: 10.1136/bmj.e5559 [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Ames M, Cui L, Stang PE, Ustun TB, Von Korff M, & Kessler RC (2007). The impact of comorbidity of mental and physical conditions on role disability in the US adult household population. Archives of General Psychiatry, 64(10), 1180–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R (2010). Mental illness stigma and willingness to seek mental health care in the european union. Social Psychiatry and Psychiatric Epidemiology, 45(7), 705–712. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, & Mechanic D (2002). Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Archives of General Psychiatry, 59(1), 77–84. [DOI] [PubMed] [Google Scholar]
- Möller-Leimkühler AM (2002). Barriers to help-seeking by men: A review of sociocultural and clinical literature with particular reference to depression. Journal of Affective Disorders, 71(1), 1–9. [DOI] [PubMed] [Google Scholar]
- Murgolo MS (2002). MCBS highlights. Health Care Financing Review, 24(1), 177. [PMC free article] [PubMed] [Google Scholar]
- Naylor CGA (2012). Long-term conditions and meantal health the cost of co-morbidities. The King’s Fund and Centre for Mental Health 2012, [Google Scholar]
- Naylor C, Parsonage M, McDaid D, Knapp M, Fossey M, & Galea A (2012). Long-term conditions and mental health: The cost of co-morbidities The King’s Fund. [Google Scholar]
- Ortman JM, Velkoff VA, & Hogan H (2014). An aging nation: The older population in the united states. Washington, DC: US Census Bureau, , 25–1140. [Google Scholar]
- Phillips MA, & Murrell SA (1994). Impact of psychological and physical health, stressful events, and social support on subsequent mental health help seeking among older adults. Journal of Consulting and Clinical Psychology, 62(2), 270. [DOI] [PubMed] [Google Scholar]
- Reeves WC, Strine TW, Pratt LA, Thompson W, Ahluwalia I, Dhingra SS, … Safran MA (2011). Mental illness surveillance among adults in the united states. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, D.C.: 2002), 60 Suppl 3, 1–29. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=21881550&site=ehost-live [PubMed] [Google Scholar]
- Ricci JA, Baggish JS, Hunt TL, Stewart WF, Wein A, Herzog AR, & Diokno AC (2001). Coping strategies and health care—seeking behavior in a US national sample of adults with symptoms suggestive of overactive bladder. Clinical Therapeutics, 23(8), 1245–1259. [DOI] [PubMed] [Google Scholar]
- Salive ME (2013). Multimorbidity in older adults. Epidemiologic Reviews, 35, 75–83. doi: 10.1093/epirev/mxs009 [doi] [DOI] [PubMed] [Google Scholar]
- Sample M (1994). A profile of the medicare current beneficiary survey. Health Care Financing Review, 15(4), 153. [PMC free article] [PubMed] [Google Scholar]
- Sareen J, Jagdeo A, Cox BJ, Clara I, ten Have M, Belik S, …. Stein MB (2007). Perceived barriers to mental health service utilization in the united states, ontario, and the netherlands. Psychiatric Services, [DOI] [PubMed] [Google Scholar]
- Sarkisian CA, Lee-Henderson MH, & Mangione CM (2003). Do depressed older adults who attribute depression to “old age” believe it is important to seek care? Journal of General Internal Medicine, 75(12), 1001–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS institute, SAS system for windows, SAS institute, cary, NC, USA, 2009. [Google Scholar]
- Segal D, Coolidge F, Mincic M, & O’riley A (2005). Beliefs about mental illness and willingness to seek help: A cross-sectional study. Aging & Mental Health, 9(4), 363–367. [DOI] [PubMed] [Google Scholar]
- Shaw C, Brittain K, Tansey R, & Williams K (2008). How people decide to seek health care: A qualitative study. International Journal of Nursing Studies, 45(10), 1516–1524. [DOI] [PubMed] [Google Scholar]
- Shim RS, Compton MT, Rust G, Druss BG, & Kaslow NJ (2009). Race-ethnicity as a predictor of attitudes toward mental health treatment seeking. Psychiatric Services, [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small LFF (2010). Use of mental health services among people with co-occurring disorders and other mental health co-morbidities: Employing the behavioral model of vulnerable populations. Mental Health and Substance use: Dual Diagnosis, 3(2), 81–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein JA, Andersen R, & Gelberg L (2007). Applying the gelberg-andersen behavioral model for vulnerable populations to health services utilization in homeless women. Journal of Health Psychology, 72(5), 791–804. [DOI] [PubMed] [Google Scholar]
- Stevens JA, Ballesteros MF, Mack KA, Rudd RA, DeCaro E, & Adler G (2012). Gender differences in seeking care for falls in the aged medicare population. American Journal of Preventive Medicine, 43(1), 59–62. [DOI] [PubMed] [Google Scholar]
- Taber JM, Leyva B, & Persoskie A (2015). Why do people avoid medical care? A qualitative study using national data. Journal of General Internal Medicine, 30(3), 290–297. [DOI] [PMC free article] [PubMed] [Google Scholar]


