Abstract
Background
Restriction of elbow flexion significantly limits upper extremity function following brachial plexus injuries. In recent years, the double fascicular nerve transfer procedure utilizing ulnar and median nerve transfer to musculocutaneous branches has shown promising functional outcomes.
Objective
To evaluate restoration of elbow flexion following a double fascicular transfer in patients with brachial plexus injuries and identify predictors of poor outcomes.
Methods
This retrospective review included 10 consecutive patients with brachial plexus injuries involving C5-C6 root avulsions who underwent the double nerve transfer procedure. The mean follow-up was 12 months and the primary outcome was assessment of elbow flexion with the use of the Medical Research Council (MRC) scale.
Results
This procedure achieved elbow flexion of MRC grade M3 or higher in 50% of our cohort. Time interval from injury to surgery showed a statistically significant inverse association with functional recovery (r = -0.73, p = 0.016). Patients who had the surgery within six months of the injury, demonstrated higher MRC grades during the follow-up (p = 0.048). There was no association between elbow flexion recovery and age, body mass index (BMI), gender, hypertension, diabetes or smoking status.
Conclusions
The double fascicular transfer to musculocutaneous may be a safe and effective treatment for restoration of elbow flexion. The procedure is associated with superior functional outcomes when performed within the first six months from the injury.
Keywords: oberlin, elbow flexion, ulnar nerve, median nerve, musculocutaneous
Introduction
Brachial plexus injuries can result in significant physical disability, pain and psychological distress [1]. The majority of cases are attributed to motorcycle and motor vehicle traffic accidents [2]. Upper trunk or C5-C6 nerve root injuries can cause loss of elbow flexion, shoulder abduction and external rotation [3]. Despite the fact that hand function can remain intact, restriction of elbow flexion can significantly limit upper extremity usability. Restoration of elbow flexion is commonly given priority over extension, as elbow extension is aided by gravity.
Nerve transfer procedures have been a successful surgical treatment strategy for restoration of elbow flexion. Healthy donor nerves can be transferred onto the damaged musculocutaneous nerve to achieve biceps muscle re-innervation and elbow flexion [4]. The ulnar, medial pectoral, spinal accessory and intercostal nerves can act as potential nerve donors. The Oberlin procedure consists of an ulnar nerve fascicle transfer to the musculocutaneous branch to the biceps and has since been proven to be a safe and effective procedure for restoration of elbow flexion [5,6]. Several studies have shown that the additional transfer of median nerve fascicles to the motor branch to the biceps may be associated with superior outcomes compared to the traditional Oberlin procedure, without an increase in complication rates [4,7]. The aim of this study is to report restoration of elbow flexion following a double fascicular - ulnar and median to musculocutaneous nerve - nerve transfer after brachial plexus injuries and identify predictors of poor outcomes.
Materials and methods
Study design and patient population
This was a retrospective study of 10 patients with brachial plexus injuries involving the C5-C6 roots who underwent a double fascicular transfer procedure between 2010 and 2017. Medical records were retrieved from the Emory University hospital database after approval of the study protocol by the Institutional Review Board. Experienced abstractors extracted all relevant information including baseline, procedural and outcome data using the electronic medical records database.
All patients lacked elbow flexion prior to the procedure. Clinical examination was performed by the senior author (NMB) both pre- and post-operatively during the long-term follow-up. Electrophysiological studies and computerized tomography myelogram were routinely performed to establish whether lesions were pre- or post-ganglionic and identify the presence of root avulsions.
Data abstraction variables included demographic data (sex, age, body mass index (BMI), hypertension, diabetes mellitus and smoking), mechanism of injury, time interval from injury to surgery and duration of follow-up. All surgeries were performed by NMB.
Surgical technique
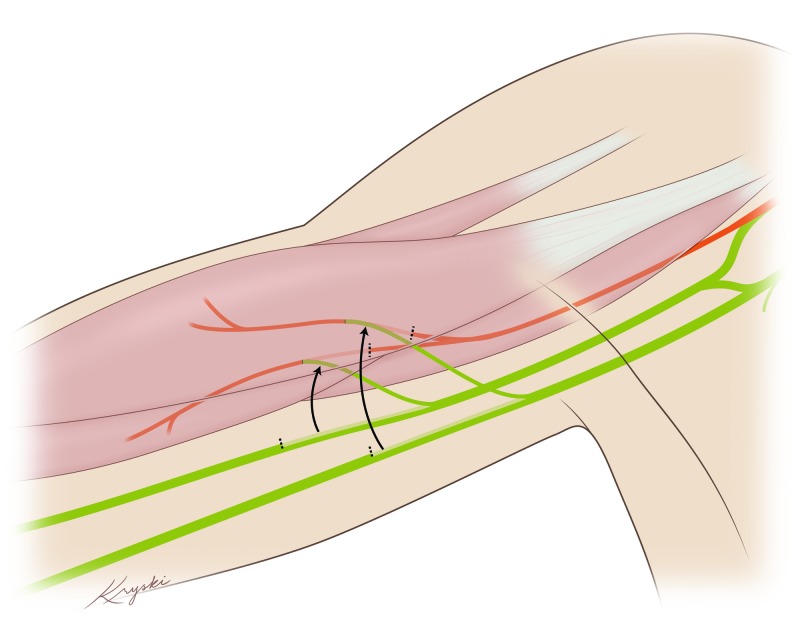
Patients are positioned supine with the right arm abducted and externally rotated. The ulnar and median nerves are identified and dissected circumferentially. Monopolar stimulation reveals muscle contractions in the median and the ulnar nerve. Next, the musculocutaneous nerve is identified and dissected proximally. An internal neurolysis is performed on the musculocutaneous nerve to separate the individual fascicles with branches to the biceps, branches of the brachialis, and the sensory branch under microscopic magnification. Nerve action potentials are performed, confirming conduction in the median and ulnar but not the musculocutaneous nerve. Provided these conditions are met, internal neurolysis of the median and ulnar nerves is performed under the microscope to separate the individual fascicles. One fascicle from each nerve determined by combined motor action potentials (CMAP) to contain the greatest percentage of wrist flexor innervation is cut distally. Nylon 9-0 is used to anastomose the median fascicle to the brachialis and ulnar fascicle to the biceps branches of the musculocutaneous nerve, respectively. Each anastomosis is then secured with Tisseel. Figure 1 illustrates the double fascicular transfer to musculocutaneous branches.
Figure 1. This illustration shows the ulnar and median fascicular transfers to the two branches of the musculocutaneous nerve.
Definitions and outcome assessment
All patients were evaluated at regular post-operative intervals (mean follow-up: 12 months, range: 4-25). Elbow flexion was assessed by the Medical Research Council (MRC) scale, with scores ranging from 0 (no evidence of contractility) to 5 (full range of motion against gravity with full resistance) [8].
Statistical analysis
Continuous variables were described with the mean ± standard deviation (SD) and compared with the Wilcoxon rank sum rest. Correlation between quantitative variables was assessed with the Spearman’s correlation coefficient test. Categorical variables were described with absolute and relative frequencies. For all tests, p < 0.05 was considered statistically significant. All analyses were performed using STATA software (Version 14.1; Stata Corporation, College Station, TX).
Results
In total, 10 patients who underwent a double fascicular transfer procedure were identified, of which nine were male (90%) (mean age: 35.6 ± 16, range: 18-56). Patient baseline demographics are presented in Table 1.
Table 1. Patient demographic characteristics.
BMI: Body mass index.
| Age (years) | 35.6 ± 16 |
| BMI | 27.1 ± 3.9 |
| Male | 90% (N = 9/10) |
| Smoking history | 40% (N = 4/10) |
| Hypertension | 60% (N = 6/10) |
| Diabetes | 1% (N = 1/10) |
All patients sustained a brachial plexus injury following road traffic accidents (90%) except for one patient who experienced a fall from height. Root involvement levels are outlined in Table 2. Electromyography (EMG) findings showed that nine patients (90%) had sustained root avulsions without axonal continuity to the biceps muscle, of which seven sustained C5-C6 root avulsions, one C5-C7 avulsions, and one patient had a C5 root avulsion. In this cohort, only one patient had no root avulsions where EMG studies showed post-ganglionic C5-C6 involvement.
Table 2. Root involvement among patients who underwent double Oberlin nerve transfer.
| Root level | N (%) |
| C5-C6 | 6 (60%) |
| C5-C7 | 3 (30%) |
| C5-C8 | 1 (10%) |
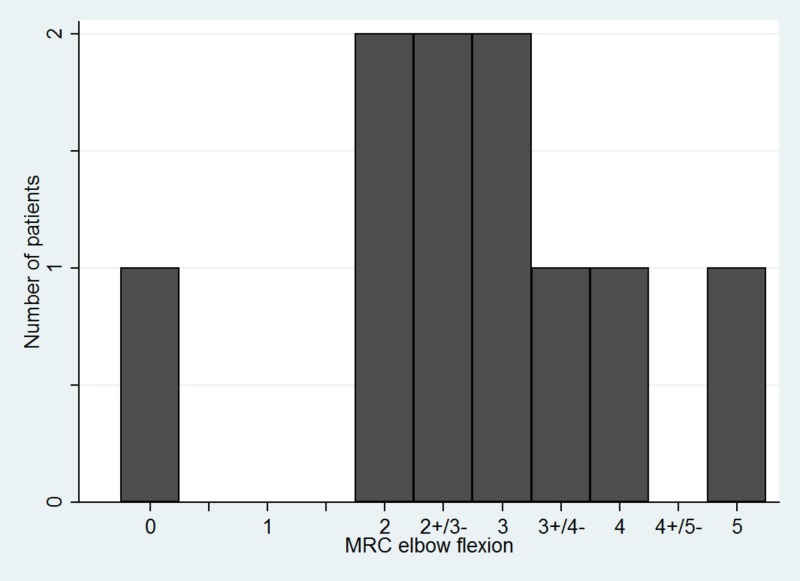
During the mean follow-up of 12 months (range: 4-25), 50% (N = 5/10) of patients achieved elbow flexion MRC grade M3 or higher which was considered a good outcome. All patients had a pre-operative MRC grade of M0. MRC grades achieved after follow-up in our cohort is shown in Figure 2.
Figure 2. Histogram demonstrating the MRC recovery grade of elbow flexion among our patient cohort.
MRC: Medical Research Council.
No motor or sensory deficits associated with the ulnar and median nerve were identified during the immediate post-operative and long-term follow-up.
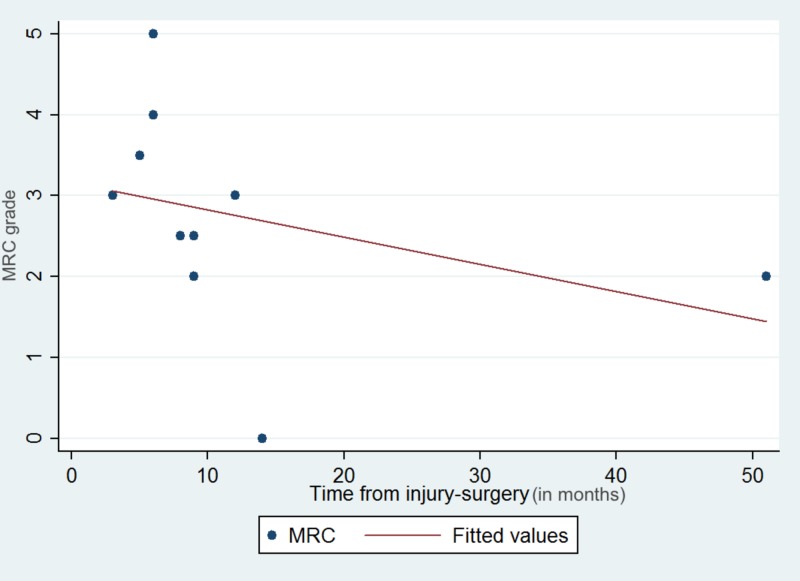
There was a statistically significant association between MRC elbow flexion grade and time interval from injury to surgery (r = -0.73, p = 0.016) (Figure 3).
Figure 3. Scatter plot with the best fit line demonstrating the negative linear association between MRC grade recovery and time from injury to surgery.
MRC: Medical Research Council.
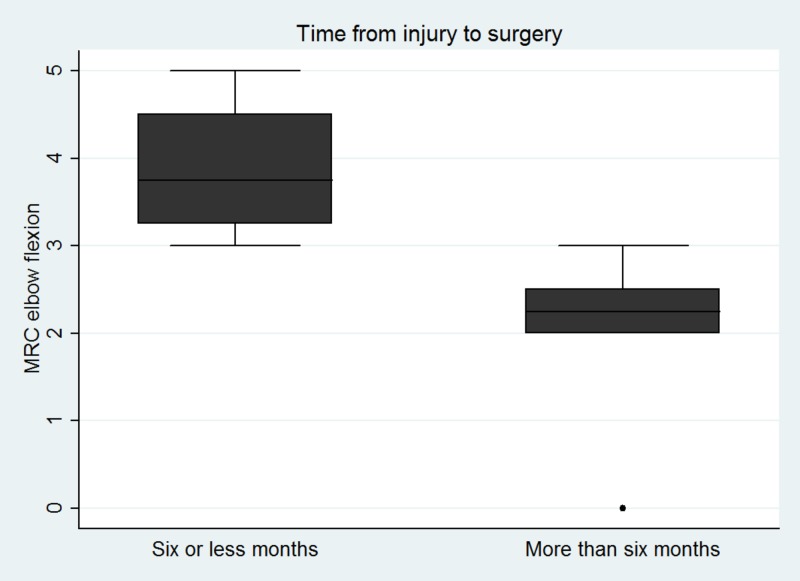
A separate analysis by categorizing patients in two groups (six or less months vs. more than six months interval between injury and surgery) demonstrated that patients who had the double fascicular transfer within a six or less month time interval from injury to surgery had statistically significant better functional MRC outcomes (p = 0.048) (Figure 4).
Figure 4. Box plots showing the distribution of MRC elbow flexion grades in patients who had the surgery with less vs. more than six months of their injury.
MRC: Medical Research Council.
No association was demonstrated between MRC grade and patients’ age (r = 0.05, p = 0.89) or BMI (r = -0.04, p = 0.90). Finally, no significant association between MRC elbow flexion and diabetes (p = 0.72), hypertension (p = 0.10), history of smoking (p = 0.74) and male gender (p = 0.21) was identified in our patient cohort.
Discussion
In this retrospective study, the double ulnar and median fascicle transfer to the musculocutaneous brachialis and biceps branches achieved functional elbow flexion (M3 or higher) in 50% of patients during a mean follow-up of 12 months. There was a statistically significant association between the time interval from injury to surgery and MRC elbow flexion recovery. As previously reported in nerve repair procedures, patients who had surgery within six or less months from their injury, had a higher MRC grade. The presence of diabetes, hypertension, history of smoking and male gender does not seem to affect recovery.
Oberlin’s technique was first described in 1994 and involved transferring ulnar fascicles to the biceps muscle [6]. In the recent years, this procedure has been modified by the addition of median nerve fascicle transfer to the musculocutaneous nerve showing promising results [9,10]. Several studies have suggested that the double transfer may in fact be associated with superior outcomes as compared to the single transfers [11,12]. The study by Mackinnon et al. reported a mean elbow flexion of MRC grade 4+ during the 5.5-month follow-up after a double nerve transfer procedure [12]. Similarly, Liverneaux et al. in a study of 10 patients showed that the double transfer procedure resulted in a mean MRC grade of M4 [11]. In contrast, a prospective study by Martins et al. did not show significant differences between the single and double nerve transfers [13]. Nevertheless, comparative studies are limited in the literature as double transfer is preferentially utilized in most institutions. Future prospective cohorts are warranted to elucidate whether the double transfer is indeed associated with superior functional elbow flexion recovery.
The present study suggested that time interval between injury and surgery can adversely affect recovery of elbow flexion (r = -0.73, p = 0.016). Additionally, this was validated when our cohort was divided into two groups; those who had surgery prior vs. after six months of their injury where we showed that patients who had the early surgery (six months or less) had superior functional outcomes in terms of MRC grade (p = 0.048). Our results are in agreement with previous studies which have reported better functional recovery when the procedure was undertaken within the first six months [5]. Unlike nerve repair procedures, Oberlin transfer involves the use of healthy donor fascicles, thus eliminating the impact of time since injury on the motor neuron. Similarly, distal transfer brings the donor fascicle close to the end plate, and thus should minimize the effect of time since injury on the distal nerve. Given these facts, one would predict that time since injury would affect distal transfers less. In contrast, the motor end plate faces significant changes after the six-month interval and might become irreversible after 12 months [14,15]. This phenomenon, along with ongoing muscle fibrosis, can render the muscle non-responsive to neural stimulation and greatly diminish the potential for re-innervation after nerve transfer procedures, potentially explaining the impact of time since injury on distal transfer [16].
It is worth highlighting that we did not find any association between MRC grade and age following the double nerve transfer procedure (r = 0.05, p = 0.89). Our results are in agreement with previous studies showing that older patients have similar restoration of elbow flexion following a double fascicular transfer [5]. However, results are inconclusive across the literature. Specifically, the study by Liverneaux et al. suggested that older patients may have a decreased potential for restoration of elbow flexion following an Oberlin transfer [11]. Future studies with a larger patient sample are needed to identify if increased age is a predictor of poor functional outcome. Lastly, the present study did not show any association between elbow flexion and patient demographics including BMI, diabetes, hypertension, smoking and gender which is line with studies examining nerve transfer procedures [17,18].
Limitations
Several limitations should be noted for this study. First, our study was retrospective and thus limited by its non-randomized nature. Second, despite the standardized follow-up schedule at our institution, its duration was not similar for all patients due to some patients missing appointments, which might have affected the outcomes. Third, this study is limited by its low patient sample, single surgeon experience and lack of matched controls.
Conclusions
The current study suggests that the double ulnar and median nerve transfer to the musculocutaneous may be a safe and effective approach for elbow flexion restoration following C5-C6 root avulsions. Also, it points out that functional outcomes are adversely affected by the increase in the time interval from injury to surgery; the double fascicular transfer within the first six months is suggested by this study. No association between MRC grades and patient demographic characteristics was identified.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study. Functional Neurosurgery Outcomes Database issued approval IRB00068818
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Comparison of objective muscle strength in C5-C6 and C5-C7 brachial plexus injury patients after double nerve transfer. Tsai YJ, Su FC, Hsiao CK, Tu YK. Microsurgery. 2015;35:107–114. doi: 10.1002/micr.22283. [DOI] [PubMed] [Google Scholar]
- 2.Brachial plexus injury in adults: diagnosis and surgical treatment strategies. Thatte MR, Babhulkar S, Hiremath A. Ann Indian Acad Neurol. 2013;16:26–33. doi: 10.4103/0972-2327.107686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Upper brachial plexus injury in adults: comparative effectiveness of different repair techniques. Ali ZS, Heuer GG, Faught RWF, et al. J Neurosurg. 2015;122:195–201. doi: 10.3171/2014.9.JNS132823. [DOI] [PubMed] [Google Scholar]
- 4.Case report: double Oberlin nerve transfer to restore elbow flexion following C5-C6 avulsion injury. Moses MJ, Dai AZ, Lowe DT, Chu A, Protopsaltis TS. Oper Neurosurg (Hagerstown) 2018;16:23–26. doi: 10.1093/ons/opy064. [DOI] [PubMed] [Google Scholar]
- 5.Functional outcome of nerve transfer for restoration of shoulder and elbow function in upper brachial plexus injury. Venkatramani H, Bhardwaj P, Faruquee SR, Sabapathy SR. J Brachial Plex Peripher Nerve Inj. 2008;3:0. doi: 10.1186/1749-7221-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nerve transfer to biceps muscle using a part of ulnar nerve for C5-C6 avulsion of the brachial plexus: anatomical study and report of four cases. Oberlin C, Beal D, Leechavengvongs S, Salon A, Dauge MC, Sarcy JJ. J Hand Surg Am. 1994;19:232–237. doi: 10.1016/0363-5023(94)90011-6. [DOI] [PubMed] [Google Scholar]
- 7.Technique of the double nerve transfer to recover elbow flexion in C5, C6, or C5 to C7 brachial plexus palsy. Goubier J-N, Teboul F. Tech Hand Up Extrem Surg. 2007;11:15–17. doi: 10.1097/01.bth.0000248360.14448.6b. [DOI] [PubMed] [Google Scholar]
- 8.Adult traumatic brachial plexus injuries. Shin AY, Spinner RJ, Steinmann SP, Bishop AT. https://journals.lww.com/jaaos/Abstract/2005/10000/Adult_Traumatic_Brachial_Plexus_Injuries.3.aspx. J Am Acad Orthop Surg. 2005;13:382–396. doi: 10.5435/00124635-200510000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Nerve transfers for adult traumatic brachial plexus palsy (brachial plexus nerve transfer) Rohde RS, Wolfe SW. HSS J. 2007;3:77–82. doi: 10.1007/s11420-006-9027-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nerve transfers to the biceps and brachialis branches to improve elbow flexion strength after brachial plexus injuries. Tung TH, Novak CB, Mackinnon SE. J Neurosurg. 2003;98:313–318. doi: 10.3171/jns.2003.98.2.0313. [DOI] [PubMed] [Google Scholar]
- 11.Preliminary results of double nerve transfer to restore elbow flexion in upper type brachial plexus palsies. Liverneaux PA, Diaz LC, Beaulieu J-Y, Durand S, Oberlin C. Plast Reconstr Surg. 2006;117:915–919. doi: 10.1097/01.prs.0000200628.15546.06. [DOI] [PubMed] [Google Scholar]
- 12.Results of reinnervation of the biceps and brachialis muscles with a double fascicular transfer for elbow flexion. Mackinnon SE, Novak CB, Myckatyn TM, Tung TH. J Hand Surg Am. 2005;30:978–985. doi: 10.1016/j.jhsa.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 13.A prospective study comparing single and double fascicular transfer to restore elbow flexion after brachial plexus injury. Martins RS, Siqueira MG, Heise CO, Foroni L, Teixeira MJ. Neurosurgery. 2013;72:709–715. doi: 10.1227/NEU.0b013e318285c3f6. [DOI] [PubMed] [Google Scholar]
- 14.Comparison between partial ulnar and intercostal nerve transfers for reconstructing elbow flexion in patients with upper brachial plexus injuries. Kakinoki R, Ikeguchi R, Dunkan SF, Nakayama K, Matsumoto T, Ohta S, Nakamura T. J Brachial Plex Peripher Nerve Inj. 2010;5:0. doi: 10.1186/1749-7221-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heterotopic nerve transfers: recent trends with expanding indication. Wood MB, Murray PM. J Hand Surg Am. 2007;32:397–408. doi: 10.1016/j.jhsa.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 16.Oberlin’s transfer: long term outcomes. Verdins K, Kapickis M. J Hand Surg (Asian-Pacific Vol) 2018;23:176–180. doi: 10.1142/S2424835518500170. [DOI] [PubMed] [Google Scholar]
- 17.Evaluation of infraspinatus reinnervation and function following spinal accessory nerve to suprascapular nerve transfer in adult traumatic brachial plexus injuries. Baltzer HL, Wagner ER, Kircher MF, Spinner RJ, Bishop AT, Shin AY. Microsurgery. 2017;37:365–370. doi: 10.1002/micr.30070. [DOI] [PubMed] [Google Scholar]
- 18.Long-term clinical outcomes of spinal accessory nerve transfer to the suprascapular nerve in patients with brachial plexus palsy. Emamhadi M, Alijani B, Andalib S. Acta Neurochir (Wien) 2016;158:1801–1806. doi: 10.1007/s00701-016-2886-1. [DOI] [PubMed] [Google Scholar]