Summary box.
Improving the quality and availability of critical care is essential for reducing the burden of preventable deaths in low-income and middle-income countries.
The conventional high-income country model, based on resource-intensive intensive care units with expensive monitoring and supportive equipment and large numbers of highly trained staff, is unlikely to be suitable for these settings.
Currently, costs severely restrict access to critical care in low-income and middle-income countries, and there is an urgent need to develop an alternative affordable critical care model for these settings.
Innovative technology and digital health may offer part of the solution and enable the development of an affordable, sustainable and scalable model of critical care in resource-limited settings.
Introduction
In 2016, an estimated 8.6 million premature deaths occurred in low-income and middle-income countries (LMICs) from causes that ‘should not occur in the presence of timely and effective healthcare’. Improving the quality and availability of critical illness care in LMICs is essential if this burden is to be reduced,1 2 and even more important over the coming years as populations age and the prevalence of comorbidities, such as cardiovascular disease and diabetes, increase.1
Currently, capacity for critical illness care in many LMICs3–5 is limited. In high-income countries, there are generally between 5 and 30 intensive care unit (ICU) beds per 100 000 people.2 3 The limited data available indicate that in LMICs, there are between 0.1 and 2.5 ICU beds per 100 000 people. Many countries are also transitioning from low to lower–middle income status, receiving less international healthcare aid6 which may limit resources available for expanding capacity. While, the expansion of private healthcare systems in LMICs may partly meet the increased demand, the quality of care delivered by such providers is variable and will be unaffordable for many.2 7
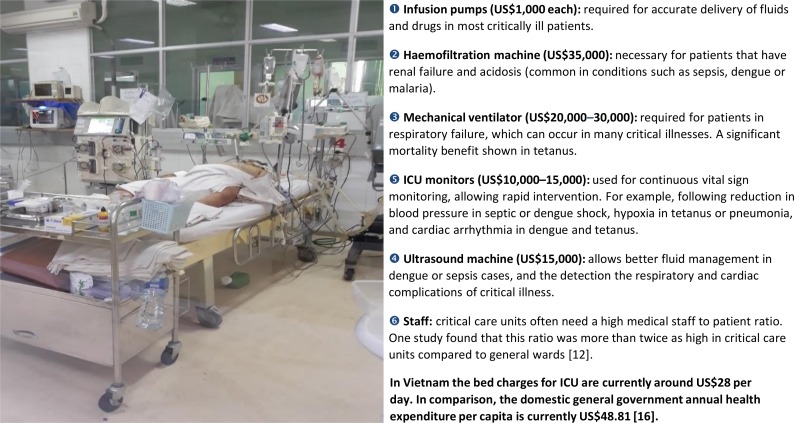
Careful physiological monitoring is the cornerstone of good critical illness care.8 In the conventional high-income setting ICU model, monitoring is achieved with expensive equipment, high-quality laboratory support and large numbers of highly trained staff. In LMICs, this model is usually impractical as the required resources are either unavailable or too expensive.4 5 9 The figure 1 shows the predicted costs of providing a high-income country model ICU bed in Vietnam. Although this is just one case study, it highlights the magnitude of those costs. Counterintuitively, equipment costs can be substantially higher than for high-income countries, due to importation taxes and non-competitive pricing structures.
Figure 1.
The costs for the monitoring and supportive equipment associated with an intensive care unit bed in Vietnam. Costs are based on quotes from commercial medical equipment distributors in Vietnam (2018 prices). Costs are not annualised.
Maintaining operability of expensive ICU equipment is a further challenge in LMICs where there may be frequent power cuts and high ambient temperatures and humidity. Restricted availability of maintenance staff and replacement parts, means that equipment is often non-functioning or cannot be used to its full potential.2 10 Additionally, the paucity of appropriately trained staff and limited infection control measures can result in more frequent complications, which may worsen outcomes and further increase costs.11 12
Costing studies conducted in high-income countries have reported average costs of ICU care between US$1700 and 4500 per day (adjusted to 2014 prices).13 14 The delivery of critical care is less expensive in LMICs largely because of much lower labour costs; for example, a study based in an Indian hospital estimated the average daily cost of ICU care was US$109 (2014 prices).15 Although this amount may appear low, the average annual healthcare expenditure per capita across LMICs is only around 5% that of high-income countries.16
Furthermore, in LMICs, critical care costs are often not fully covered by the health/insurance systems and patients’ and their families can incur high out-of-pocket expenses.17–19 Currently costs severely restrict access to ICU care in LMICs, particularly for the socioeconomically disadvantaged and uninsured, and there is an urgent need to develop an alternative affordable critical care model for LMICs.20
What can be done?
The emergence of new technologies, means there are huge opportunities to expand capacity and improve the care of critically ill patients in LMICs.10 21 22
A substantial proportion of critical care costs in LMICs are to cover staffing and fixed asset equipment costs as opposed to actual medications and laboratory tests.15 Methods impacting these may be a way of reducing costs, allowing expansion of capacity as well as improving the care quality.
Low-cost wearable devices offer a potentially affordable approach to physiological monitoring in LMICs, reducing the need for expensive commercial equipment and, combined with artificial intelligence (AI), may also improve care quality. Wearable devices, such as fitness trackers, have been used in ICU populations in high-income countries and have shown good correlation with conventionally-derived ECG data.23 AI and machine learning algorithms can be used to analyse ICU patients’ physiological data, learn from them and create computer-assisted decision-support systems.22 With simple modifications, low-cost wearables can feed data into AI systems which can then guide treatment decisions and diagnostics. A key advantage of this approach is that AI systems can compensate for the noisy, artefactual signals that typically arise from wearables. In high-income settings, AI algorithms have been shown to improve the management of sepsis and lower mortality.24 25 The ability of AI systems to continuously learn and adapt means that computer-assisted clinical decision-support systems can be tailored to the needs of a specific context or setting. Thus algorithms could be created to help in the management of diseases such as malaria, dengue and tetanus, which are uncommon in high-income ICU settings but are significant problems in LMICs. Importantly, existing libraries of analogous data sets acquired from western clinical settings can be used, along with smaller quantities of LMICs physiological data to permit ‘transfer learning’, in which complex predictive models can be retrained and recalibrated for use with low-cost sensors.
As well as physiological monitoring, point-of-care diagnostic and imaging devices are also increasingly available and affordable. Devices such as hand-held ultrasound probes connecting to a mobile phone could make equipping LMIC ICUs more feasible and cheaper, aiding diagnosis and management of patients. While a high degree of training is currently required to acquire and interpret images, future AI systems may provide operator guidance for inexperienced users and perform image interpretation, reducing requirements for highly trained staff and making the provision of critical care services outside of major urban hospitals significantly more feasible.
What should happen next?
The potential for new technology to transform healthcare in LMICs is now widely accepted, but most innovations remain at the proof-of-concept stage or have only been tested in small pilot studies.22 26 The current challenge is bridging the gap between proof-of-concept and actual large-scale implementation.22 27
Moving forward, there is an urgent need to conduct implementation trials, to assess the actual effectiveness and feasibility of using these new digital technologies for critical care in LMICs. Successful innovation can only take place in close collaboration with end-user communities and a real understanding of the contextual need. In addition, the wide variety of critical care capacity and facilities within and between many LMICs means that new technologies should be designed to fit within the existing infrastructure. This will therefore require more than a simple design process but an active two-way partnership between all stakeholders and with considerations regarding scale-up taken into account from the start of the process.
The use of these new technologies also needs to be part of broader strategies to improve ICU performance. Other potential strategies for improving the delivery of critical care in LMICs include improving organisational structures, empowerment of nurses and locally generated clinical guidelines.2 28 In addition, in most LMICs, critical care is not currently a well-developed specialty. Consequently, the development of training and capacity building programmes is particularly important—not only for ICU physicians but also for nurses and other clinical personnel.2 It is vital that these training programmes, as well as covering specific ICU clinical skills also include basic management and organisational aspects of critical care.2 Successful initiatives such as Train-the-Trainer and peer-to-peer programmes have been shown to be successful in LMICs and could be further expanded.29 30
Conclusion
Improving the quality and availability of critical care is essential for reducing the burden of preventable deaths in LMICs. There will be no one size fits all solution to this problem and a multifaceted approach is required. Nevertheless, greater utilisation of new technologies could be an important part of the solution. Through such innovation, critical care capacity could not only be increased but also be improved in quality and at a reduced cost. However, designing and implementing sustainable and scalable solutions is a significant challenge, requiring strong collaborations and real understanding between all stakeholders.
Footnotes
Handling editor: Seye Abimbola
Contributors: HCT, CLT and NVVC conceived the manuscript. All authors contributed to the writing.
Funding: HCT, SY, VMTH and GET (089276/B/09/7). AMD is supported by the Wellcome Trust (106698/B14/Z) CLT is supported by the Wellcome Trust (107367/Z/15/Z).
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data are contained within the main body of the text.
References
- 1.Adhikari NKJ, Fowler RA, Bhagwanjee S, et al. Critical care and the global burden of critical illness in adults. The Lancet 2010;376:1339–46. 10.1016/S0140-6736(10)60446-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dondorp AM, Iyer SS, Schultz MJ. Critical care in Resource-Restricted settings. JAMA 2016;315:753–4. 10.1001/jama.2016.0976 [DOI] [PubMed] [Google Scholar]
- 3.Schultz MJ, Dunser MW, Dondorp AM, et al. Current challenges in the management of sepsis in ICUs in resource-poor settings and suggestions for the future. Intensive Care Med 2017;43:612–24. 10.1007/s00134-017-4750-z [DOI] [PubMed] [Google Scholar]
- 4.Murthy S, Leligdowicz A, Adhikari NKJ. Intensive care unit capacity in low-income countries: a systematic review. Plos One 2015;10:e0116949 10.1371/journal.pone.0116949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baelani I, Jochberger S, Laimer T, et al. Availability of critical care resources to treat patients with severe sepsis or septic shock in Africa: a self-reported, continent-wide survey of anaesthesia providers. Crit Care 2011;15 10.1186/cc9410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dieleman J, Campbell M, Chapin A, et al. Evolution and patterns of global health financing 1995–2014: development assistance for health, and government, prepaid private, and out-of-pocket health spending in 184 countries. The Lancet 2017;389:1981–2004. 10.1016/S0140-6736(17)30874-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheikh K, Saligram PS, Hort K. What explains regulatory failure? analysing the architecture of health care regulation in two Indian states. Health Policy Plan 2015;30:39–55. 10.1093/heapol/czt095 [DOI] [PubMed] [Google Scholar]
- 8.Baker T, Khalid K, Acicbe O, et al. Critical care of tropical disease in low income countries: report from the task Force on tropical diseases by the World Federation of societies of intensive and critical care medicine. J Crit Care 2017;42:351–4. 10.1016/j.jcrc.2017.11.028 [DOI] [PubMed] [Google Scholar]
- 9.Dünser MW, Baelani I, Ganbold L. A review and analysis of intensive care medicine in the least developed countries. Crit Care Med 2006;34:1234–42. 10.1097/01.CCM.0000208360.70835.87 [DOI] [PubMed] [Google Scholar]
- 10.Mekontso Dessap A. Frugal innovation for critical care. Intensive Care Med 2019;45:252–4. 10.1007/s00134-018-5391-6 [DOI] [PubMed] [Google Scholar]
- 11.Arabi YM, Phua J, Koh Y, et al. Structure, organization, and delivery of critical care in Asian ICUs. Crit Care Med 2016;44:e940–8. 10.1097/CCM.0000000000001854 [DOI] [PubMed] [Google Scholar]
- 12.Dat VQ, Long NT, Giang KB, et al. Healthcare infrastructure capacity to respond to severe acute respiratory infection (SARI) and sepsis in Vietnam: a low-middle income country. J Crit Care 2017;42:109–15. 10.1016/j.jcrc.2017.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Halpern NA, Pastores SM. Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med 2010;38:65–71. 10.1097/CCM.0b013e3181b090d0 [DOI] [PubMed] [Google Scholar]
- 14.Tan SS, Bakker J, Hoogendoorn ME, et al. Direct cost analysis of intensive care unit stay in four European countries: applying a standardized costing methodology. Value in Health 2012;15:81–6. 10.1016/j.jval.2011.09.007 [DOI] [PubMed] [Google Scholar]
- 15.Agrawal A, Gandhe M, Gandhe S, et al. Study of length of stay and average cost of treatment in medicine intensive care unit at tertiary care center. J Health Res Rev 2017;4:24–9. 10.4103/2394-2010.199329 [DOI] [Google Scholar]
- 16. World Bank. World development indicators. Secondary world development indicators. Available: https://data.worldbank.org/indicator
- 17.Jayaram R, Ramakrishnan N. Cost of intensive care in India. Indian J Crit Care Med 2008;12:55–61. 10.4103/0972-5229.42558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Woldeamanuel YW, Andemeskel AT, Kyei K, et al. Case fatality of adult tetanus in Africa: systematic review and meta-analysis. J Neurol Sci 2016;368:292–9. 10.1016/j.jns.2016.07.025 [DOI] [PubMed] [Google Scholar]
- 19.Shukla VV, Nimbalkar SM, Ganjiwale JD, et al. Direct cost of critical illness associated healthcare expenditures among children admitted in pediatric intensive care unit in rural India. Indian J Pediatr 2016;83:1065–70. 10.1007/s12098-016-2165-4 [DOI] [PubMed] [Google Scholar]
- 20.Divatia JV, Iyer S. Ten major priorities for intensive care in India. Intensive Care Med 2015;41:1468–71. 10.1007/s00134-014-3618-8 [DOI] [PubMed] [Google Scholar]
- 21.Rodriguez-Manzano J, Chia PY, Yeo TW, et al. Improving dengue diagnostics and management through innovative technology. Curr Infect Dis Rep 2018;20 10.1007/s11908-018-0633-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wahl B, Cossy-Gantner A, Germann S, et al. Artificial intelligence (AI) and global health: how can AI contribute to health in resource-poor settings? BMJ Global Health 2018;3:e000798 10.1136/bmjgh-2018-000798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kroll RR, McKenzie ED, Boyd JG, et al. Use of wearable devices for post-discharge monitoring of ICU patients: a feasibility study. J Intensive Care 2017;5 10.1186/s40560-017-0261-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shimabukuro DW, Barton CW, Feldman MD, et al. Effect of a machine learning-based severe sepsis prediction algorithm on patient survival and hospital length of stay: a randomised clinical trial. BMJ Open Respir Res 2017;4 10.1136/bmjresp-2017-000234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Komorowski M, Celi LA, Badawi O, et al. The artificial intelligence clinician learns optimal treatment strategies for sepsis in intensive care. Nat Med 2018;24:1716–20. 10.1038/s41591-018-0213-5 [DOI] [PubMed] [Google Scholar]
- 26.Lundin J, Dumont G. Medical mobile technologies – what is needed for a sustainable and scalable implementation on a global scale? Global Health Action 2017;10 10.1080/16549716.2017.1344046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Norrie J. The challenge of implementing AI models in the ICU. Lancet Respir Med 2018;6:886–8. 10.1016/S2213-2600(18)30412-0 [DOI] [PubMed] [Google Scholar]
- 28.Diaz JV, Riviello ED, Papali A, et al. Global critical care: moving forward in resource-limited settings. Annals of Global Health 2019;85 10.5334/aogh.2413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beane A, Padeniya A, De Silva AP, et al. Closing the theory to practice gap for newly qualified doctors: evaluation of a peer-delivered practical skills training course for newly qualified doctors in preparation for clinical practice. Postgrad Med J 2017;93:592–6. 10.1136/postgradmedj-2016-134718 [DOI] [PubMed] [Google Scholar]
- 30.Tunpattu S, Newey V, Sigera C, et al. A short, structured skills training course for critical care physiotherapists in a lower-middle income country. Physiother Theory Pract 2018;34:714–22. 10.1080/09593985.2018.1423593 [DOI] [PubMed] [Google Scholar]