Abstract
Papilledema is optic nerve swelling caused by increased intracranial hypertension, which has the potential to cause significant vision loss. Papilledema from idiopathic intracranial hypertension (IIH) is typically bilateral and symmetric, but can sometimes be asymmetric and even unilateral. The purpose of this study was to develop ultrasound vibro-elastography (UVE) for noninvasive measurement of ocular tissue wave speed for patients with papilledema. 9 patients with papilledema from IIH and 9 age-matched healthy control subjects were enrolled in this study. A local, gentle, 0.1 second harmonic vibration was applied on the eyelid to generate wave propagation in the ocular tissue. 3 excitation frequencies of 100, 150, and 200 Hz were used to measure the wave speeds. A 6.4 MHz ultrasound probe was used to noninvasively measure wave propagation in the ocular structures. Wave speeds were analyzed in the posterior sclera of the maculae of the eyes. The magnitudes of wave speed at each frequency of the IIH patients’ posterior sclera were significantly higher than those of healthy subjects. It was found that the magnitudes of wave speed at each frequency were statistically higher in the eyes with papilledema than in the contralateral eyes without papilledema for the patients with unilateral papilledema. UVE provides a noninvasive technique to measure the wave speed of posterior sclera, which may be useful for assessing patients with papilledema.
Keywords: Ultrasound vibro-elastography, Papilledema, posterior sclera, wave speed
Introduction
Idiopathic intracranial hypertension (IIH) is a condition of increased intracranial pressure of unknown cause producing papilledema (optic nerve swelling), choroidal folds, and visual loss (Chen and Wall 2014, Friedman 2007, Kilgore, et al. 2017). While IIH was previously called benign intracranial hypertension, the term “benign” has been removed from the name because many patients can have significant permanent visual impairment (Corbett, et al. 1982, Corbett and Thompson 1989, Digre 2003, Wall and George 1991). Vision loss is dependent on the extent and severity of papilledema, which is variable in patients with IIH. Patients can sometimes have raised intracranial pressure with headaches and other signs of raised intracranial pressure (ICP) without papilledema, and therefore, have no risk of vision loss (Digre, et al. 2009, Wang, et al. 1998). Other patients can have severe papilledema with moderately elevated intracranial pressure. In addition, papilledema can be very asymmetric between the two eyes with 10% of patients with IIH showing a difference of ≥2 grades of papilledema between the two eyes (Wall and White 1998). Rarely, a patient can have severe papilledema in one eye and no swelling in the other eye (Lepore 1992, Sedwick and Burde 1983). There is also an emerging problem after long-duration space flights among astronauts who can develop space flight-associated neuro-ocular syndrome (SANS), a poorly understood condition of choroidal folds and papilledema that occurs in astronauts that mimics many elements of raised intracranial pressure (Lee, et al. 2016, Mader, et al. 2011). However, not all astronauts are affected and the degree of change is very variable. Despite the observed variability of papilledema and choroidal folds among patients with IIH and astronauts, the cause of the variability is unknown.
We hypothesize that the variability of the papilledema may be due to differences in the biomechanical tissue properties of the sclera. This may either allow or prevent raised intracranial pressure from being transmitted to the optic nerve head, which influences the amount of papilledema and choroidal folds that develop. Ultrasound elastography has been proposed for the excised cornea (Tanter, et al. 2009). We also performed UVE on ex vivo and in vivo corneas (Sit, et al. 2017, Zhou, et al. 2017). This research aims to measure the wave speed of the posterior sclera for assessing papilledema.
We have developed a novel ultrasound vibro-elastography (UVE) technique to measure tissue wave speed (Zhang, et al. 2017, Zhang, et al. 2018, Zhou, et al. 2017). In UVE, a handheld vibrator is used to generate a gentle, local, 0.1 second harmonic vibration on the skin. The resulting wave propagation on the skin and wave propagation inside the tissue are detected using an ultrasound probe. The specific goal of this study is to translate the UVE technique into clinical use for quantitative assessment of the eye wave speed of patients with papilledema.
Materials and Methods
Under an IRB approved protocol, both eyes of 9 patients with unilateral or bilateral papilledema from IIH and 9 age-matched healthy subjects were evaluated. The patients with IIH all met the modified Dandy criteria (Dandy 1937, Wall 2010), including normal neuroimaging with an elevated opening pressure of >250 mm H20. The mean age of the patients was 34.5 (range: 19 - 61, 2 male and 7 female). After obtaining informed consent, imaging was performed by placing the vertically oriented ultrasound probe in contact with the eyelid after application of coupling gel (Aquasonic, Inc.) on the probe surface. The subject was tested in a supine position with the eye in an upward direction of gaze, with both eyes closed. A sinusoidal vibration signal of 0.1 s duration was generated by a function generator (Model 33120A, Agilent, Santa Clara, CA). The vibration signals were generated at 3 frequencies of 100, 150, and 200 Hz (Zhang, et al. 2018). The excitation signal was amplified by an audio amplifier (Model D150A, Crown Audio Inc., Elkhart, IN) and then applied by a handheld shaker (Model: FG-142, Labworks Inc., Costa Mesa, CA 92626)(Clay, et al. 2018). The shaker applied a 0.1 s harmonic vibration on the eyelid using an indenter with a 3 mm diameter (Fig. 1). The generated tissue motion amplitude is typically less than 10 μm. The excitation of the shaker on the tissue is typically much less than 1N. Patients only feel very gentle motion on their eyes and experienced no discomfort. An ultrasound system (Vantage 1, Verasonics, Kirkland, WA) with an L11-5v ultrasound transducer with a central frequency of 6.4 MHz was used for detecting the wave propagation of the posterior sclera (Sit, et al. 2018). The position of the ultrasound probe on the eye and the position of the indenter of the handheld shaker on the eye could cause variation among measurement results. For this study, an ophthalmology physician trained in ultrasonography performed this test to minimize variability in the measurements. The measurement was only taken if a clear ultrasound image was available. To reduce the variations, 3 measurements were performed for each frequency.
Figure 1.
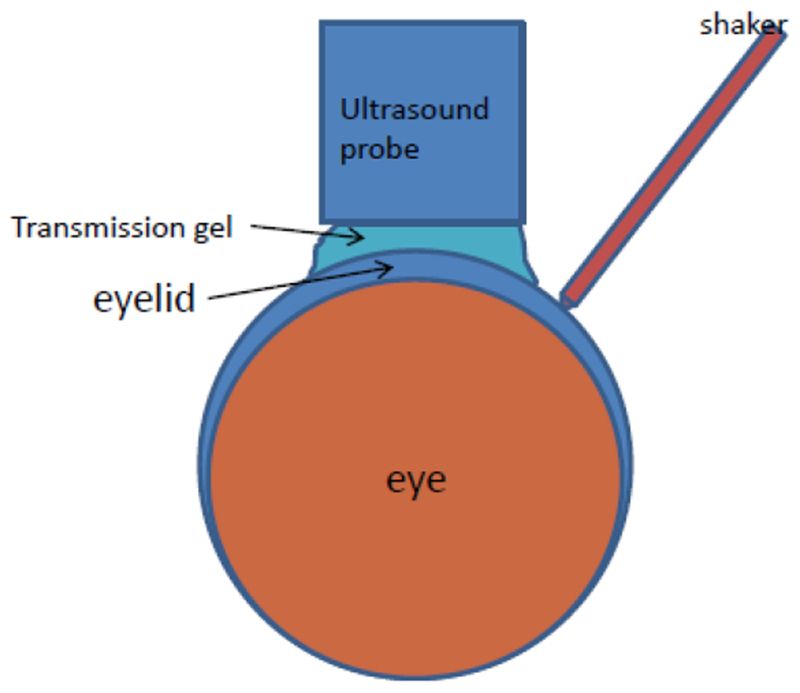
Schematic of experimental setup for UVE.
Particle velocity in the axial direction (V) caused by wave propagation was used for wave speed estimation. V was calculated from in-phase/quadrature (IQ) data of consecutive frames using a one-dimensional autocorrelation method (Kasai, et al. 1985, Zhang, et al. 2018). 3 pixels in space and 2 sampling points in the slow time direction were used for averaging. A 3 × 3 pixel spatial median-filter was then used on each frame of the wave motion image to remove noise spike points. A directional filter is then applied upon the wave field to extract the axial and lateral propagating waves. Local wave speed is recovered using a time-of-flight method based on both axial and lateral speed maps. A region-of-interest (ROI) was selected to measure wave speeds of temporal regions of the posterior sclera (Fig. 2a) and the corresponding wave speed of the ROI was calculated (Fig. 2b). Wave speed of the ROI is a combination of both the axial or lateral speed. Therefore, it is an absolute wave speed at each pixel.
Figure 2.
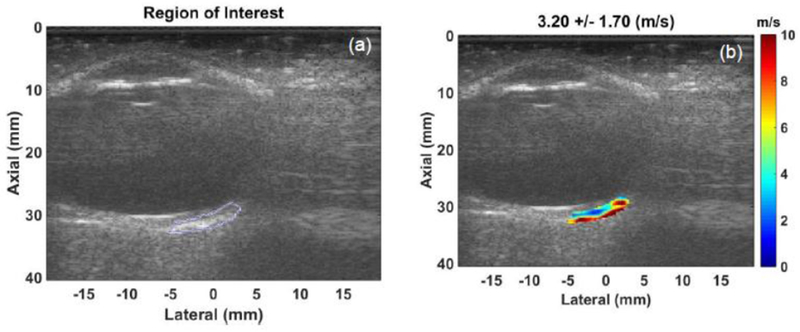
Representative selected temporal region of posterior sclera of a patient (a) and corresponding calculated wave speed (b) using speed map analysis.
Statistical analysis
We performed a Kruskal-Wallis test in MATLAB to assess statistical significance of wave speeds at 3 frequencies of both eyes between patients and healthy subjects and frequencies among left, right eyes of patients with unilateral papilledema.
Results
We evaluated 7 patients with bilateral papilledema and 2 patients with unilateral papilledema from IIH as well as 9 age-matched healthy subjects. The wave speeds of the posterior sclera at 100, 150, and 200 Hz were higher in the 9 patients with papilledema compared with the 9 healthy subjects, p<0.05 (Figure 3 and Table 1). Among the two patients with unilateral papilledema, the wave speeds of the temporal portion of posterior sclera was higher in the eye with papilledema compared to the contralateral eye without papilledema (Figs 4, 5, Table 2).
Figure 3.
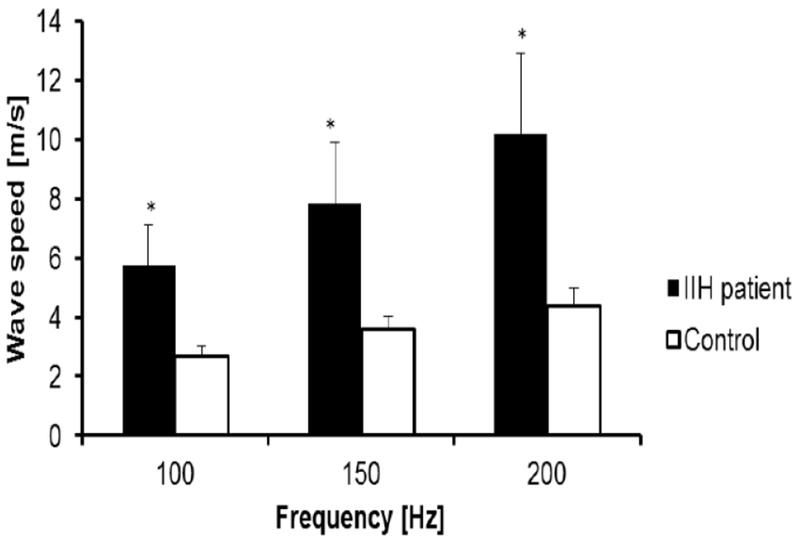
Comparison of wave speed of posterior sclera at three frequencies between healthy subjects and patients with papilledema. Asterisk indicates statistically significant difference.
Table 1.
Mean values of wave speeds of both eyes of IIH patients and healthy subjects at 100, 150, and 200 Hz.
| 100 Hz | p | 150 Hz | p | 200 Hz | p | |
|---|---|---|---|---|---|---|
| IIH Patients | 5.74 ± 1.36 | <0.01 | 7.83 ± 2.08 | <0.01 | 10.19 ± 2.72 | <0.01 |
| Healthy | 2.67 ± 0.35 | <0.01 | 3.58 ± 0.43 | <0.01 | 4.38 ± 0.62 | <0.01 |
Figure 4.
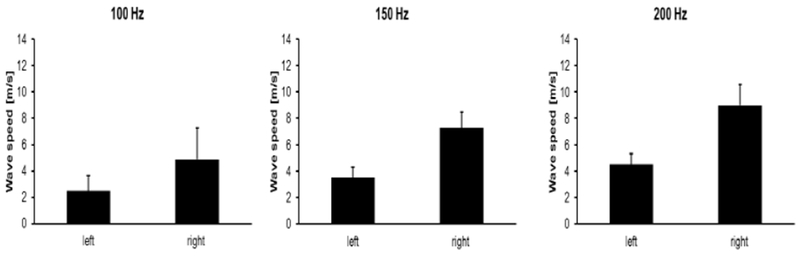
Comparison of wave speed of posterior sclera at 3 frequencies of the left and right eye of the patient with unilateral papilledema (right eye) as well as patients with bilateral papilledema.
Figure 5.

Comparison of wave speed of posterior sclera at 3 frequencies of the left and right eye of the patient with unilateral papilledema (left eye) as well as patients with bilateral papilledema.
Table 2.
Wave speeds of IIH patients with unilateral papilledema at 100, 150, and 200 Hz for both eyes. Asterisk indicates the eye with papilledema.
| Wave speed [m/s] | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 100 [Hz] | 150 [Hz] | 200 [Hz] | |||||||
| Left | Right | p | Left | Right | p | Left | Right | p | |
| 8th | 2.5 ± 1.13 | 4.85 ± 2.4 | 0.04 | 3.51 ± 0.81 | 7.28 ± 1.2* | 0.02 | 4.49 ± 0.83 | 8.99 ± 1.54* | 0.04 |
| 9th | 6.82 ± 0.51* | 4.22 ± 1.11* | 0.03 | 13.06 ± 1.58* | 6.35 ± 1.49 | 0.03 | 15.94 ± 2.84* | 7.33 ± 1.94* | 0.03 |
Discussion
The aim of this study was to translate an UVE technique into clinical use for quantitative assessment of patients with papilledema. A high pulse repetition rate of 2000 frame/s was used to detect tissue motion in response to excitations of 100, 150, and 200 Hz. The frequency ranges chosen in this study consider the wave motion amplitude, spatial resolution, and wave attenuation. A Verasonics ultrasound system was used to collect up to a few thousand imaging frames per second using a plane-wave pulse transmission technique. The wave speed of the temporal posterior sclera was measured by analyzing ultrasound data directly from the sclera. Hence, the wave speed measurement was local and independent of the location and amplitude of excitation. The wave speed of the posterior sclera of both eyes in both healthy controls and IIH patients was tested at 3 excitation frequencies.
The reason the temporal regions of the posterior sclera were selected for analysis is that the nasal region of the posterior sclera is usually not easily visible or as big as the temporal region of the posterior sclera. In addition, the sclera temporal to the optic nerve encompasses the macula, which is the region that is most affected by disease processes, including choroidal folds. The region directly posteriorly was avoided because it encompasses the optic nerve, which would introduce complexities in analysis due to the nerve.
High definition optical coherence tomography (HD-OCT) has been used for examining the biomechanical deformation of load bearing structures of the optic nerve head (ONH) resulting from raised intracranial pressure (Kupersmith, et al. 2011). Choroidal folds were studied in patients with spectral-domain OCT (SD-OCT) (Sibony, et al. 2015). However, the imaging penetration of OCT is only several millimeter deep. Deeper penetration with ultrasound is advantageous for evaluation of the biomechanical structures of the posterior sclera. The basis for relevant implementation of diagnostic imaging tools is to understand the relationship between imaging findings and the characteristic structural pathological changes. The findings in our study provide information on the wave speed of the posterior sclera of eyes with papilledema.
Papilledema is a clinical diagnosis, which is based on funduscopic examination, OCT, and ultrasound/fluorescein angiogram if necessary. MRI and lumbar puncture are also required to confirm/refute a diagnosis of idiopathic intracranial hypertension. The main goal of this study was to evaluate whether scleral rigidity is different in eyes with papilledema, not to use ultrasound elastography to diagnose papilledema. UVE demonstrated that eyes with papilledema have higher wave speed than that in healthy controls. It has yet to be determined whether eyes with papilledema have a higher wave speed that predisposes them to papilledema or if pressure transmitted to the optic nerves leads to the higher wave speed measured on UVE. It is interesting that patients with unilateral papilledema have higher wave speed in the eye with papilledema than the contralateral unaffected eye. This could suggest that the wave speed of the sclera does play a role in the susceptibility to papilledema from raised intracranial pressure, because patients with IIH have significantly raised intracranial pressure throughout the brain and would be expected to have an equal amount of pressure reaching both optic nerves despite the significant asymmetry between the two eyes. However, other studies suggest that asymmetric pressure could reach the eyes in IIH with asymmetric papilledema due to anatomic differences in optic canal size (Bidot, et al. 2015). Therefore, further studies and longitudinal follow-up will be required to determine if higher wave speed of the posterior sclera is a predisposing factor to papilledema or secondary to the increased intracranial pressure. Either finding would be helpful clinically. If these changes represent an intrinsic difference within eyes with papilledema, ultrasound elastography could predict an eye’s propensity toward the development of papilledema. If these changes are secondary to increased pressure being transmitted to the optic nerve, ultrasound elastography can be used to help differentiate papilledema from pseudopapilledema in borderline cases that remain uncertain after clinical exam and standard ophthalmic imaging, such as OCT. One limitation of this study is that given the limited number of patients with bilateral or unilateral papilledema, it is difficult to investigate the correlation between variability of the papilledema and the scleral biomechanical properties. In the future, as we recruit more patients with unilateral or bilateral papilldema, we will investigate this relationship.
This study provides a technique to measure the wave speed of the posterior sclera. We have demonstrated that eyes with papilledema have higher wave speed in the posterior sclera than eyes without papilledema. This could provide insight into the pathogenesis and susceptibility to these vision threatening changes. UVE may also be useful in predicting the susceptibility of astronauts to papilledema after space flight. We are currently exploring the role of brain elasticity in papilledema using MR elastography. Future studies combining UVE and MR elastography will provide a better understanding of the pathogenesis behind papilledema.
Conclusion
Ultrasound vibro-elastography provides a noninvasive and nonionizing technique to evaluate the wave speed of posterior sclera for patients with papilledema. The magnitudes of wave speed of the posterior sclera of patients with papilledema were significantly higher than those of healthy controls. For patients with unilateral papilledema, the magnitudes of wave speed of the posterior sclera of the eye with papilledema were higher than those of the unaffected contralateral eye. These results indicate that UVE may be useful for quantitative evaluation of papilledema development. In the future, we will investigate a larger population of patients to study the relationship between papilledema and wave speed of the posterior sclera.
Acknowledgements
We would like to acknowledge financial support from the Department of Ophthalmology Research Funding Award, Mayo Clinic, to Dr. Chen and also NIH R21 grant (EY026095, co-PIs AJS, XZ) from the National Eye Institute. Dr. Boran Zhou and Dr. John Chen contributed equally to this manuscript. We would like to thank Mrs. Jennifer Poston for her assistance in editing the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bidot S, Bruce BB, Saindane AM, Newman NJ, Biousse V. Asymmetric papilledema in idiopathic intracranial hypertension. Journal of neuro-ophthalmology: the official journal of the North American Neuro-Ophthalmology Society 2015; 35:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, Wall M. Epidemiology and risk factors for idiopathic intracranial hypertension. Int Ophthalmol Clin 2014; 54:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clay R, Bartholmai BJ, Zhou B, Karwoski R, Peikert T, Osborn T, Rajagopalan S, Kalra S, Zhang X. Assessment of Interstitial Lung Disease Using Lung Ultrasound Surface Wave Elastography: A Novel Technique With Clinicoradiologic Correlates. J Thorac Imaging 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett JJ, Savino PJ, Thompson HS, Kansu T, Schatz NJ, Orr LS, Hopson D. Visual loss in pseudotumor cerebri. Follow-up of 57 patients from five to 41 years and a profile of 14 patients with permanent severe visual loss. Arch Neurol 1982; 39:461–74. [DOI] [PubMed] [Google Scholar]
- Corbett JJ, Thompson HS. The rational management of idiopathic intracranial hypertension. Arch Neurol 1989; 46:1049–51. [DOI] [PubMed] [Google Scholar]
- Dandy WE. Intracranial pressure without brain tumor: diagnosis and treatment. Annals of surgery 1937; 106:492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Digre KB. Not so benign intracranial hypertension. Bmj 2003; 326:613–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Digre KB, Nakamoto BK, Warner JE, Langeberg WJ, Baggaley SK, Katz BJ. A comparison of idiopathic intracranial hypertension with and without papilledema. Headache 2009; 49:185–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman DI. Idiopathic intracranial hypertension. Curr Pain Headache Rep 2007; 11:62–8. [DOI] [PubMed] [Google Scholar]
- Kasai C, Namekawa K, Koyano A, Omoto R. Real-time two-dimensional blood flow imaging using an autocorrelation technique. IEEE Transactions on sonics and ultrasonics 1985; 32:458–64. [Google Scholar]
- Kilgore KP, Lee MS, Leavitt JA, Mokri B, Hodge DO, Frank RD, Chen JJ. Re-evaluating the Incidence of Idiopathic Intracranial Hypertension in an Era of Increasing Obesity. Ophthalmology 2017; 124:697–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kupersmith MJ, Sibony P, Mandel G, Durbin M, Kardon RH. Optical coherence tomography of the swollen optic nerve head: deformation of the peripapillary retinal pigment epithelium layer in papilledema. Investigative ophthalmology & visual science 2011; 52:6558–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee AG, Tarver WJ, Mader TH, Gibson CR, Hart SF, Otto CA. Neuro-Ophthalmology of Space Flight. J Neuroophthalmol 2016; 36:85–91. [DOI] [PubMed] [Google Scholar]
- Lepore FE. Unilateral and highly asymmetric papilledema in pseudotumor cerebri. Neurology 1992; 42:676–8. [DOI] [PubMed] [Google Scholar]
- Mader TH, Gibson CR, Pass AF, Kramer LA, Lee AG, Fogarty J, Tarver WJ, Dervay JP, Hamilton DR, Sargsyan A, Phillips JL, Tran D, Lipsky W, Choi J, Stern C, Kuyumjian R, Polk JD. Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight. Ophthalmology 2011; 118:2058–69. [DOI] [PubMed] [Google Scholar]
- Sedwick LA, Burde RM. Unilateral and asymmetric optic disk swelling with intracranial abnormalities. Am J Ophthalmol 1983; 96:484–7. [DOI] [PubMed] [Google Scholar]
- Sibony PA, Kupersmith MJ, Feldon SE, Wang J- K, Garvin M. Retinal and choroidal folds in papilledema. Investigative ophthalmology & visual science 2015; 56:5670–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sit AJ, Kazemi A, Zhou B, Zhang X. Comparison of Ocular Biomechanical Properties in Normal and Glaucomatous Eyes Using Ultrasound Surface Wave Elastography. Investigative Ophthalmology & Visual Science 2018; 59:1218–18. [Google Scholar]
- Sit AJ, Lin SC, Kazemi A, McLaren JW, Pruet CM, Zhang X. In Vivo Non-Invasive Measurement of Young’s Modulus of Elasticity in Human Eyes: A Feasibility Study. J Glaucoma 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanter M, Touboul D, Gennisson J-L, Bercoff J, Fink M. High-resolution quantitative imaging of cornea elasticity using supersonic shear imaging. IEEE transactions on medical imaging 2009; 28:1881–93. [DOI] [PubMed] [Google Scholar]
- Wall M Idiopathic intracranial hypertension. Neurologic clinics 2010; 28:593–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall M, George D. Idiopathic intracranial hypertension. A prospective study of 50 patients. Brain 1991; 114 ( Pt 1A):155–80. [PubMed] [Google Scholar]
- Wall M, White WN 2nd. Asymmetric papilledema in idiopathic intracranial hypertension: prospective interocular comparison of sensory visual function. Invest Ophthalmol Vis Sci 1998; 39:134–42. [PubMed] [Google Scholar]
- Wang SJ, Silberstein SD, Patterson S, Young WB. Idiopathic intracranial hypertension without papilledema: a case-control study in a headache center. Neurology 1998; 51:245–9. [DOI] [PubMed] [Google Scholar]
- Zhang X, Osborn T, Zhou B, Meixner D, Kinnick R, Bartholmai B, Greenleaf J, Kalra S. Lung ultrasound surface wave elastography: a pilot clinical study. IEEE transactions on ultrasonics, ferroelectrics, and frequency control 2017; 64:1298–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Zhou B, Kalra S, Bartholmai B, Greenleaf J, Osborn T. An Ultrasound Surface Wave Technique for Assessing Skin and Lung Diseases. Ultrasound in Medicine & Biology 2018; 44:321–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Zhou B, Miranda AF, Trost LW. A Novel Noninvasive Ultrasound Vibro-elastography Technique for Assessing Patients With Erectile Dysfunction and Peyronie Disease. Urology 2018; 116:99–105. [DOI] [PubMed] [Google Scholar]
- Zhang X, Zhou B, Osborn T, Bartholmai B, Kalra S. Lung ultrasound surface wave elastography for assessing interstitial lung disease. IEEE Transactions on Biomedical Engineering 2018:1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou B, Sit AJ, Zhang X. Noninvasive measurement of wave speed of porcine cornea in ex vivo porcine eyes for various intraocular pressures. Ultrasonics 2017; 81:86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]


