Abstract
Aims:
To assess the occurrence of disordered eating behaviours in teenagers with Type 1 diabetes and to compare characteristics according to level of disordered eating behaviours.
Methods:
In this cross-sectional study, we collected adolescents’ demographic and diabetes management data by parent–youth interview and chart review. Teenagers completed psychosocial surveys, including the Diabetes Eating Problem Survey-Revised (DEPS-R), a diabetes-specific measure of disordered eating behaviours. We categorized teenagers according to level of disordered eating behaviours: low, DEPS-R score <10; moderate, DEPS-R score 10–19; and high, DEPS-R score ≥20.
Results:
The 178 teenagers (48% girls) were aged 14.9±1.3 years, with diabetes duration of 7.4±3.7 years. Most (59%) had low, 26% had moderate, and 15% had high levels of disordered eating behaviours. Several biomedical and psychosocial characteristics differed by level of disordered eating behaviours. There were more girls in the moderate (62%) and high (65%) than in the low level of disordered eating behaviours group (37%; P=0.003) and more obese teenagers in the moderate (13%) and high (27%) groups than in the low group (4%; P=0.0003). Frequency of daily blood glucose monitoring decreased (P=0.0006) and HbA1c level increased (P=0.01) with greater level of disordered eating behaviours. A greater level of disordered eating behaviours was also associated with poorer treatment adherence, more negative affect regarding blood glucose monitoring, poorer quality of life, and more depressive symptoms (all P<0.0001), along with more diabetes-specific family conflict (P=0.01).
Conclusions:
Identifying teenagers with Type 1 diabetes who have moderate and high levels of disordered eating behaviours may prevent progression to eating disorders and substantial morbidity by directing support and intervention efforts to those in need.
Introduction
Subclinical disordered eating behaviours and clinical eating disorders occur more often in people with Type 1 diabetes than in their peers without diabetes [1–3]. Disordered eating behaviours may include dieting, excessive caloric restriction, fasting, binge-eating, intense exercise for weight control, and purging behaviours, such as abuse of laxatives or diuretics and self-induced vomiting [4]. Insulin omission or restriction for weight control is a purging behaviour specific to insulin-treated diabetes, mainly Type 1 diabetes [5].
The prevalence of disordered eating behaviours in people with Type 1 diabetes ranges from 8% to 55%, depending on the definition and method of measurement [2,3,6–9]. As in young people without Type 1 diabetes, disordered eating behaviours occur more frequently in girls and young women than in boys and young men [6,8–10], more frequently in older than in younger adolescents [8,11], and in association with family conflict [7]. Insulin omission or restriction as a purging behaviour occurs in 11–30% of girls and women with Type 1 diabetes [3,5,12–15].
Among people with Type 1 diabetes, disordered eating behaviours are associated with poor diabetes self-management and worse metabolic control, contributing to increased risk of short- and long-term diabetes complications. Adverse effects include elevated HbA1c levels and abnormal lipid profiles, while complications include diabetic ketoacidosis, retinopathy, neuropathy and nephropathy, as well as premature mortality [5,11,12,14,15]. In an 11-year follow-up study, women with Type 1 diabetes who reported intentionally under-dosing or omitting insulin at baseline had a threefold higher relative risk of death during the 11-year follow-up period than those who did not under-dose or omit insulin at baseline [15].
When untreated, disordered eating behaviours often worsen and progress to clinical eating disorders [11,13]; hence, early identification of young people with Type 1 diabetes who have disordered eating behaviours has important utility for early intervention in order to prevent progression to clinical eating disorders and development of diabetes complications. General screening measures for disordered eating behaviours, however, may not be appropriate in Type 1 diabetes populations because of the necessary emphasis on food and carbohydrate-counting for this group of people. General screening measures may misidentify some diabetes management behaviours as disordered eating behaviours. In addition, there is a need to assess the presence of insulin restriction or omission as a unique purging behaviour in people with Type 1 diabetes. The Diabetes Eating Problem Survey-Revised (DEPS-R) was created to overcome the deficiencies of general disordered eating behaviour screening measures as it was designed specifically for use in people with Type 1 diabetes [16,17].
The aims of the present study were to assess the occurrence of disordered eating behaviours, as measured by the DEPS-R, in a sample of teenagers (aged 13–17 years) with Type 1 diabetes, and to describe and compare the characteristics of participants according to level of disordered eating behaviours (i.e. number and frequency of behaviours). We also aimed to identify a threshold on the DEPS-R for a moderate level of disordered eating behaviours. We hypothesized that more disordered eating behaviours would be associated with older age, female sex, overweight/obesity, higher HbA1c, and poorer psychosocial characteristics, with the moderate group having characteristics intermediate between those with the lowest and highest levels of disordered eating behaviours.
Participants and methods
Participants
Participants were adolescents with Type 1 diabetes receiving care in a paediatric diabetes centre. The inclusion criteria included young people aged 13–17 years, Type 1 diabetes diagnosed according to American Diabetes Association criteria, diabetes duration ≥6 months, daily insulin dose ≥0.5 units/kg, HbA1c 48–97 mmol/mol (6.5–11.0%), and fluency in English to complete surveys. The exclusion criteria included any significant developmental, cognitive or medical conditions or major psychosocial/family issues that would interfere with study participation. Given the narrow participant age range of 13–17 years, a group known to be at risk for disordered eating behaviours, we estimated that at least 150 participants would provide a sufficient range of DEPS-R scores to achieve our aims. The study protocol was approved by the institutional review board. Parents/young people provided written informed consent/assent before completing any study procedures.
Data collection
Data were collected at a single study visit that occurred on the same day as a clinic appointment. Parents/teenagers self-reported diabetes management data (e.g. insulin regimen, blood glucose monitoring frequency) during a brief joint parent/teenager interview conducted by a trained research assistant. Research assistants collected additional diabetes management data from the electronic medical record. Height and weight were obtained in a standardized manner using a stadiometer and electronic scale that were appropriately calibrated. We calculated BMI percentiles using the Centers for Disease Control and Prevention growth charts [18]. We then categorized teenagers by weight status according to BMI percentile: underweight (<5th percentile), normal weight (5th to <85th percentile), overweight (85th to <95th percentile), and obese (≥95th percentile). Teenagers provided a blood sample for measurement of HbA1c (reference range: 4–6%, Roche Cobas Integra; Roche Diagnostics, Indianapolis, IN, USA). Teenagers completed the following validated surveys on a tablet computer using REDCap software [19].
The Diabetes Eating Problem Survey-Revised (DEPS-R) is a 16-item survey that assesses general and diabetes-specific disordered eating behaviours in people with Type 1 diabetes [16]. Items are answered on a six-point Likert scale (‘never’ to ‘always’). Total scores range from 0 to 80; higher scores indicate more disordered eating behaviours. The validated cut-off score of ≥20 indicates a high number and frequency of disordered eating behaviours that may warrant additional evaluation [16].
The Diabetes Management Questionnaire [20] is a 20-item survey that measures adherence to diabetes management tasks. Items are answered on a five-point Likert scale (‘almost never’ to ‘almost always’). Total scores range from 0 to 100; higher scores indicate greater adherence.
The Blood Glucose Monitoring Communication Questionnaire [21] is an eight-item survey that assesses negative affect related to blood glucose monitoring. Items are answered on a three-point Likert scale (‘almost never’ to ‘almost always’). After transformation, total scores range from 0 to 100; higher scores indicate more negative affect.
The Diabetes Family Conflict Scale [22] is a 19-item survey that assesses the level of family conflict around diabetes-specific tasks, such as blood glucose monitoring. Items are answered on a three-point Likert scale (‘never argue’ to ‘always argue’). After transformation, total scores range from 0 to 100; higher scores indicate more conflict.
The Pediatric Quality of Life Inventory (PedsQL) Generic Core Scales [23] is a 23-item survey that measures the teenager’s quality of life, including both physical and psychosocial functioning. Items are answered on a five-point Likert scale (‘never’ to ‘always’). Total scores range from 0 to 100; higher scores indicate better quality of life.
The Center for Epidemiologic Studies Depression Scale [24,25] is a 20-item survey that assesses depressive symptoms. Items are answered on a four-point Likert scale (‘rarely or none of the time’ to ‘most or all the time’). Total scores range from 0 to 60; higher scores indicate more depressive symptoms.
Statistical analysis
Statistical analyses were performed using sas software (version 9.4; SAS Institute, Cary, NC, USA). To assess characteristics associated with disordered eating behaviours, we categorized teenagers by level of disordered eating behaviours according to DEPS-R score: <10 = low number/frequency of disordered eating behaviours, 10–19 = moderate number/frequency of disordered eating behaviours, ≥20 = high number/frequency of disordered eating behaviours. This categorical variable for level of disordered eating behaviours (low, moderate, high) was used in bivariate analyses (anova, chi-squared tests, Mantel–Haenszel chi-squared tests).
Disordered eating behaviours were assessed as a continuous variable (DEPS-R score) in unpaired t-tests (male vs female DEPS-R scores) and in multivariate linear regression. Multivariate analyses with DEPS-R score as the dependent variable were performed to assess multiple factors associated with disordered eating behaviours. Variables were included in the model if their association with disordered eating behaviour had a P value <0.1. In bivariate analyses, P values ≤0.01 were considered statistically significant because of the multiple comparisons. In multivariate analyses, P values <0.05 were considered statistically significant.
Results
Participant characteristics
Table 1 describes demographic and diabetes management characteristics among the 178 participants. The mean participant age was ~15 years and the majority of participants (70%) had diabetes for ≥5 years. Approximately half of the participants (48%) were girls and 88% were white. Most came from two-parent families (87%) and had at least one parent with a college degree or higher (72%). Two thirds of teenagers used pump therapy for both basal and bolus insulin delivery. The mean daily insulin dose was ~1 unit/kg and the majority of teenagers (63%) checked blood glucose levels ≥5 times/day. The mean HbA1c concentration was 69±11 mmol/mol (8.5±1.0%); only 15% achieved HbA1c goal of <58 mmol/mol (<7.5%). About two-thirds of teenagers were of normal weight, 26% were overweight, and 10% were obese. Only two teenagers were underweight; therefore, we included these two teenagers in the normal weight group for analyses.
Table 1.
Participant characteristics: overall and by level of disordered eating behaviour
| Disordered eating behaviour level | |||||
|---|---|---|---|---|---|
| All teenagers (N=178) |
Low: DEPS-R score <10 (n=105) |
Moderate: DEPS- R score 10–19 (n=47) |
High: DEPS-R score ≥20 (n=26) |
P | |
| Age, years | 14.9±1.3 | 14.7±1.3 | 15.2±1.3 | 15.0±1.4 | 0.07 |
| Diabetes duration, years | 7.4±3.7 | 7.0±3.6 | 8.6±3.9 | 6.4±3.0 | 0.02 |
| Sex: female, % | 48 | 37 | 62 | 65 | 0.003 |
| Race/ethnicity: white, % | 88 | 89 | 85 | 88 | 0.8 |
| Family structure: from two-parent family, % | 87 | 86 | 87 | 92 | 0.4 |
| Parent education: college degree or higher, % | 72 | 83 | 62 | 50 | 0.0001 |
| Insulin regimen: pump, % | 67 | 73 | 62 | 54 | 0.1 |
| Daily insulin dose, units/kg | 0.96±0.24 | 0.94±0.22 | 0.95±0.28 | 1.07±0.24 | 0.04 |
| Blood glucose monitoring frequency, times/day | 5.3±1.9 | 5.7±1.9 | 5.0±2.0 | 4.2±1.2 | 0.0006 |
| HbA1c mmol/mol % |
69±11 8.5±1.0 |
67±10 8.3±0.9 |
72±13 8.7±1.2 |
75±13 9.0±1.2 |
0.01 |
| HbA1c <58 mmol/mol (<7.5%), % | 15 | 17 | 15 | 8 | 0.3 |
| Weight status, % Normal weight Overweight Obese |
64 26 10 |
70 26 4 |
62 26 13 |
42 31 27 |
0.0004 |
DEPS-R, Diabetes Eating Problem Survey-Revised. Data presented are mean ± sd, unless otherwise indicated. P values obtained from anova (age, diabetes duration, insulin dose, blood glucose monitoring frequency, HbA1c), chi-squared tests (sex, race/ethnicity, insulin regimen) and Mantel–Haenszel chi-squared tests (family structure, parent education, % HbA1c<58 mmol/mol, weight status).
DEPS-R scores
Figure 1 shows the distribution of DEPS-R scores by sex. Girls had a higher mean DEPS-R score than boys (12.4±10.3 vs 7.5±7.1; P=0.0003). Overall, most teenagers (59%) had a low level of disordered eating behaviours, with DEPS-R scores <10, 26% had a moderate level, with DEPS-R scores 10–19, and 15% had a high level, with DEPS-R scores ≥20. More girls than boys had moderate (34% vs 19%) and high (20% vs 10%) levels of disordered eating behaviours (P=0.003).
FIGURE 1.
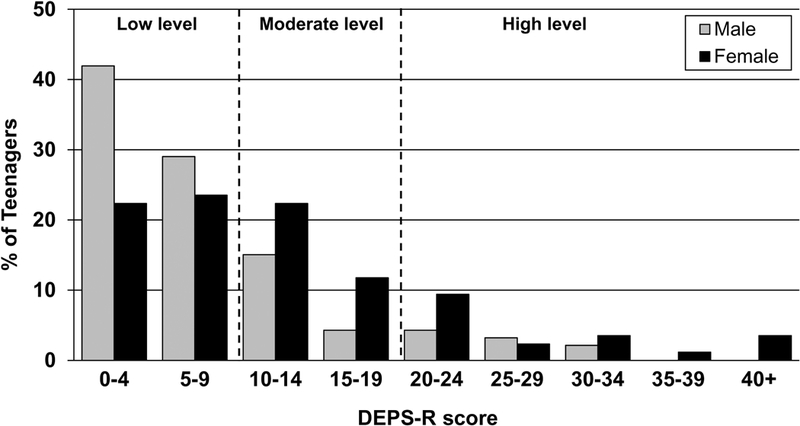
Distribution of Diabetes Eating Problem Survey-Revised (DEPS-R) scores by sex. More female than male participants had moderate (34% vs 19%) and high (20% vs 10%) levels of disordered eating behaviours (P=0.003).
Disordered eating behaviours and demographic/diabetes management characteristics
Table 1 summarizes participant characteristics according to level of disordered eating behaviours. There were no significant differences among the low, moderate, and high groups with respect to age, diabetes duration, race, family structure, insulin regimen, daily insulin dose, or HbA1c concentration. There was a higher percentage of girls in the moderate (62%) and high groups (65%) than in the low group (37%; P=0.003). Compared with teenagers in the low group, teenagers in the high group were less likely to have a parent with a college degree or higher (P=0.0001). Teenagers in the high group also checked blood glucose levels less often (P=0.0006) and had higher HbA1c concentrations (P=0.01) than teenagers in the low group. The HbA1c in the moderate group was midway between the low and high groups. There was also a greater proportion of obese teenagers in the high compared with the lower groups (P=0.0003).
In a multivariate linear model (R2=0.24, P<0.0001), controlling for age, diabetes duration, parent education, insulin regimen, insulin dose and blood glucose monitoring frequency, the variables of sex, weight status and HbA1c were significantly associated with DEPS-R score. Female sex (P=0.0004), obesity (P=0.047) and HbA1c ≥75 mmol/mol (≥9.0%) (P=0.046) were all associated with higher DEPS-R scores. In these adjusted analyses, girls scored 4.5 points higher on the DEPS-R than boys, those who were obese scored 5.3 points higher than those of normal weight, and those with elevated HbA1c ≥75 mmol/mol (≥9.0%) scored 3.0 points higher than those with lower HbA1c values (Fig. 2).
FIGURE 2.
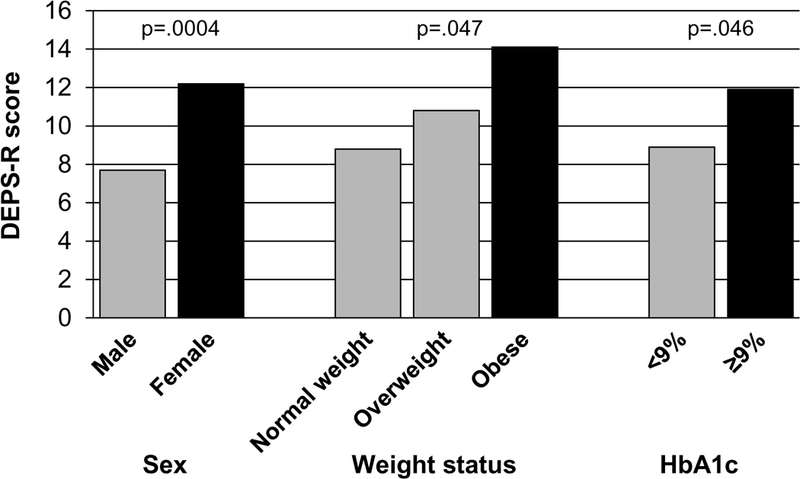
Diabetes Eating Problem Survey-Revised (DEPS-R) scores in multivariate model by sex, weight status and HbA1c. In a significant multivariate model, female sex (P=0.0004), obesity (P=0.047) and HbA1c ≥75 mmol/mol (≥9.0%; P=0.046) were significantly associated with higher DEPS-R scores.
Disordered eating behaviour and psychosocial characteristics
A number of psychosocial constructs were also associated with level of disordered eating behaviour (Table 2). Treatment adherence was significantly lower in the moderate and high groups than in the low group (P<0.0001). Negative affect regarding blood glucose monitoring differed significantly among all three groups, with more negative affect associated with higher level of disordered eating behaviours (P<0.0001). Diabetes-specific family conflict was lowest in the low group (P=0.01). Quality of life differed significantly among all three groups, with poorer quality of life associated with higher level of disordered eating behaviours (P<0.0001). Depressive symptoms differed significantly among all three groups, with more depressive symptoms associated with higher level of disordered eating behaviours (P<0.0001).
Table 2.
Psychosocial survey scores by level of disordered eating behaviours
| Disordered eating behaviour level | ||||
|---|---|---|---|---|
| Low: DEPS-R score <10 (n=105) |
Moderate: DEPS-R score 10–19 (n=47) |
High: DEPS-R score ≥20 (n=26) |
P | |
| Treatment adherence | 75±10 | 67±12 | 66±12 | <0.0001* |
| Negative affect regarding blood glucose monitoring | 27±21 | 40±20 | 54±19 | <0.0001† |
| Diabetes-specific family conflict | 15±22 | 26±28 | 23±17 | .01‡ |
| Quality of life | 89±11 | 83±9 | 71±17 | <0.0001† |
| Depressive symptoms | 5±6 | 10±8 | 19±13 | <0.0001† |
DEPS-R, Diabetes Eating Problem Survey-Revised. Data presented are mean ± sd. P values obtained from anova test.
Low group significantly different from both moderate and high groups.
Low, moderate and high groups all significantly different.
Low group significantly different from moderate group; low group vs high group, P=0.1.
In a multivariate model (R2=0.42, P<0.0001) with the psychosocial measures as the independent variables, poorer treatment adherence (P=0.0003), more negative affect regarding blood glucose monitoring (P=0.0008), and more depressive symptoms (P=0.003) were significantly associated with higher DEPS-R score. Diabetes-specific family conflict and quality of life were not significantly related to DEPS-R score in the model. The addition of sex, weight status, and HbA1c as independent variables improved the overall model (R2=0.50, P<0.0001) without changing the significance of the psychosocial measures. In this model, female sex (P=0.003) and obesity (P=0.0004) predicted higher DEPS-R score but HbA1c did not.
Discussion
In this study of 178 teenagers with Type 1 diabetes, we found that approximately two out of every five teenagers had moderate or high levels of disordered eating behaviours; 26% had moderate levels and 15% had high levels of disordered eating behaviours. Several biomedical and psychosocial factors were associated with both moderate and high levels of disordered eating behaviours, indicating that subthreshold DEPS-R scores of 10–19, below the threshold of ≥20, may identify an opportunity for intervention to prevent progression of disordered eating behaviours.
Our findings confirm recent studies that have reported associations between more disordered eating behaviours and female sex [6,8,26], higher BMI [8,9,13,26–28] and poorer glycaemic control [6,8,9,29] in people with Type 1 diabetes. In a recent large epidemiological study of 52 215 children and young adults with Type 1 diabetes, 467 individuals had an eating disorder according to the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders criteria [29]. Those with eating disorders had higher HbA1c levels as well as higher rates of diabetic ketoacidosis and risk factors for future complications compared with those without eating disorders.
In a study of 770 young people with Type 1 diabetes from the Norwegian Childhood Diabetes Registry [8], 18% scored ≥20 on the DEPS-R, similar to our rate of 15%. The Norwegian study reported that significantly more girls (28%) than boys (9%) had DEPS-R scores ≥20. Young people who scored ≥20 on the DEPS-R had higher zBMI (0.7 vs 0.2 SDS, P<0.001), higher HbA1c (77 vs. 68 mmol/mol [9.2 vs. 8.4%], P<0.001), and were older (15.6 vs. 14.4 years, P<0.001) than young people who scored <20. In a study of 60 young adults with Type 1 diabetes [9], 23% scored ≥20 on the DEPS-R (30% of women vs 18% of men), a rate slightly higher than the present study (15%), which may be attributable to the difference in ages of the two samples. The young adults who scored ≥20 on the DEPS-R had higher HbA1c (90 vs 62 mmol/mol [10.4 vs 7.8%]; P<0.001) and higher BMI (28.0 vs 25.4 kg/m2; P=0.06) than those who scored <20. None of these previous studies assessed a group with a moderate level of disordered eating behaviours as in the present study.
The present study also builds on previous studies that have reported associations between more disordered eating behaviours and poorer psychosocial attributes in individuals with Type 1 diabetes [13,27,30]. In a sample of 199 adolescents with Type 1 diabetes, Grylli et al. [27] found that young people with disordered eating behaviours had a less positive attitude toward life, more somatic complaints, lower self-esteem, and more depressive symptoms than young people without disordered eating behaviours. In a study of 83 adults with Type 1 diabetes assessed using momentary sampling, Merwin et al. [30] found that more negative affect regarding diabetes was associated with a higher likelihood of insulin restriction. Olmsted et al. [13] followed 101 girls with Type 1 diabetes for 5 years, none of whom had disordered eating behaviours at baseline, and assessed factors related to the development of disordered eating behaviours over time. They found that more concerns about body weight/shape, lower self-esteem, and more depressive symptoms predicted the onset of disordered eating behaviours.
In addition to stratifying young people by the previously validated DEPS-R score threshold of ≥20 [16], we further divided those with DEPS-R scores <20 into those with scores <10, considered as a low level of disordered eating behaviours, and those with scores of 10–19, considered as a moderate level of disordered eating behaviours. The longitudinal study by Rydall et al. [12] also classified young women into three different gradations of disordered eating behaviours, those who were non-disordered, moderately disordered, and highly disordered. These authors reported that increasing severity of disordered eating behaviours was associated with greater risk of microvascular complications during follow-up. Similarly, another study by Maharaj et al. [7] categorized adolescent girls as non-eating disturbed, mildly disturbed, and highly disturbed. These authors also reported increasing severity of disturbances in body image and eating attitudes in association with increasing severity of disturbed eating behaviours.
We found that teenagers with a moderate level of disordered eating behaviours had many biomedical and psychosocial characteristics (parent education, blood glucose monitoring frequency, HbA1c, overweight/obesity, negative affect regarding blood glucose monitoring, general quality of life, and depressive symptoms) that were different from teenagers in both the low and high groups, while for some characteristics (sex, treatment adherence and diabetes-specific family conflict), the moderate group was similar to the high group. Taken together, these data suggest that it may be possible to identify teenagers with a moderate level of disordered eating behaviours at a point in the clinical course when interventions may prevent development of more severe disordered eating behaviours and even progression to clinical eating disorders. Interventions and treatment can be tailored for those with a low or moderate level of disordered eating behaviours to prevent worsening of disordered eating behaviours.
Many of the biomedical characteristics associated with moderate and high levels of disordered eating behaviours are routinely assessed during regular diabetes clinic appointments. Clinicians should be educated on these relationships so that they can be alert to factors that may indicate elevated risk of disordered eating behaviours. For example, although low body weight is often associated with clinical eating disorders, such as anorexia nervosa, clinicians should be aware that higher BMI is associated with disordered eating behaviours in people with Type 1 diabetes [8,9,13,26–28].
A strength of the present study is the use of the validated, diabetes-specific DEPS-R screening measure [16]. When assessing disordered eating behaviours in people with Type 1 diabetes, it is important to use a diabetes-specific measure because general screening measures do not capture diabetes-specific behaviours such as intentional insulin omission or restriction. In addition, Type 1 diabetes requires attention to food and carbohydrate intake, and general screening measures may misidentify these behaviours as disordered eating behaviours. Another strength is the inclusion of both female and male participants in a study sample of adolescents, a group in which eating disorders often develop. Many studies examining disordered eating behaviours in people with Type 1 diabetes have included only female participants [5,7,11,14]. It is important, however, to include both male and female participants in order to gain a better understanding of how disordered eating behaviours may differ in boys and young men with Type 1 diabetes compared to girls and young women with Type 1 diabetes.
A limitation of the present study is its cross-sectional design; future longitudinal studies will enable a better understanding of the predictive nature of moderate levels of disordered eating behaviours for progression to high levels of disordered eating behaviours or frank eating disorders. In addition, the present study sample was relatively homogeneous and high functioning, which may limit generalizability, with 88% of participants being white, 87% being from two-parent families, and 67% receiving insulin pump therapy, although only 15% achieved target HbA1c levels of <58 mmol/mol (<7.5%).
In summary, our data suggest that there may be an opportunity to identify teenagers with moderate as well as high levels of disordered eating behaviours by using the score thresholds of 10–19 and ≥20, respectively, on the DEPS-R screening measure, a tool supported for clinical use by the American Diabetes Association in their recent position statement on the psychosocial care of people with diabetes [17]. Early identification of disordered eating behaviours may allow timely intervention to prevent progression to eating disorders and the resulting poor glycaemic control, acute and chronic diabetes complications, and premature mortality. Teenagers with either moderate or high levels of disordered eating behaviours will likely benefit from additional support to improve glycaemic control and reduce the risk of progressive disordered eating behaviours.
What’s new?
Disordered eating behaviours are common in people with Type 1 diabetes and are associated with poor glycaemic control, diabetes complications and early mortality.
This study used a diabetes-specific survey, the Diabetes Eating Problem Survey-Revised (DEPS-R), in teenagers with Type 1 diabetes to identify factors associated with varying levels of disordered eating behaviours.
Female sex, overweight/obesity, infrequent blood glucose monitoring, and poor glycaemic control were associated with more disordered eating behaviours, as were poorer quality of life and presence of depressive symptoms.
These findings may help direct support and intervention efforts to those in most need and prevent progression to clinical eating disorders.
Acknowledgments
Funding sources
This research was supported by National Institutes of Health grants R01DK095273 and P30DK036836, JDRF grant 2-SRA-2014–253-M-B, Bringing Science Home, Fundación Alicia Koplowitz, the Katherine Adler Astrove Youth Education Fund, the Maria Griffin Drury Pediatric Fund, and the Eleanor Chesterman Beatson Fund. The content is solely the responsibility of the authors and does not necessarily represent the official views of these organizations.
Footnotes
Competing interests
The authors have no relevant conflicts of interest to disclose related to this research.
Previous publication
Portions of this manuscript were presented in abstract form at the 77th Scientific Sessions of the American Diabetes Association, June 2017, San Diego, CA, USA.
References
- 1.Cooper MN, Lin A, Alvares GA, de Klerk NH, Jones TW, Davis EA. Psychiatric disorders during early adulthood in those with childhood onset type 1 diabetes: Rates and clinical risk factors from population-based follow-up. Pediatr Diabetes 2017; 18:599–606. [DOI] [PubMed] [Google Scholar]
- 2.Colton P, Olmsted M, Daneman D, Rydall A, Rodin G. Disturbed eating behavior and eating disorders in preteen and early teenage girls with type 1 diabetes: a case-controlled study. Diabetes Care 2004; 27:1654–1659. [DOI] [PubMed] [Google Scholar]
- 3.Jones JM, Lawson ML, Daneman D, Olmsted MP, Rodin G. Eating disorders in adolescent females with and without type 1 diabetes: cross sectional study. BMJ 2000; 320:1563–1566. [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association, 2004. [Google Scholar]
- 5.Goebel-Fabbri AE, Anderson BJ, Fikkan J, Franko DL, Pearson K, Weinger K. Improvement and emergence of insulin restriction in women with type 1 diabetes. Diabetes Care 2011; 34:545–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neumark-Sztainer D, Patterson J, Mellin A, Ackard DM, Utter J, Story M et al. Weight control practices and disordered eating behaviors among adolescent females and males with type 1 diabetes: associations with sociodemographics, weight concerns, familial factors, and metabolic outcomes. Diabetes Care 2002; 25:1289–1296. [DOI] [PubMed] [Google Scholar]
- 7.Maharaj SI, Rodin GM, Olmsted MP, Connolly JA, Daneman D. Eating disturbances in girls with diabetes: the contribution of adolescent self-concept, maternal weight and shape concerns and mother-daughter relationships. Psychol Med 2003; 33:525–539. [DOI] [PubMed] [Google Scholar]
- 8.Wisting L, Froisland DH, Skrivarhaug T, Dahl-Jorgensen K, Ro O. Disturbed eating behavior and omission of insulin in adolescents receiving intensified insulin treatment: a nationwide population-based study. Diabetes Care 2013; 36:3382–3387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doyle EA, Quinn SM, Ambrosino JM, Weyman K, Tamborlane WV, Jastreboff AM. Disordered Eating Behaviors in Emerging Adults With Type 1 Diabetes: A Common Problem for Both Men and Women. J Pediatr Health Care 2017; 31:327–333. [DOI] [PubMed] [Google Scholar]
- 10.Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, Loth K. Dieting and disordered eating behaviors from adolescence to young adulthood: findings from a 10-year longitudinal study. J Am Diet Assoc 2011; 111:1004–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Colton PA, Olmsted MP, Daneman D, Farquhar JC, Wong H, Muskat S et al. Eating Disorders in Girls and Women With Type 1 Diabetes: A Longitudinal Study of Prevalence, Onset, Remission, and Recurrence. Diabetes Care 2015; 38:1212–1217. [DOI] [PubMed] [Google Scholar]
- 12.Rydall AC, Rodin GM, Olmsted MP, Devenyi RG, Daneman D. Disordered eating behavior and microvascular complications in young women with insulin-dependent diabetes mellitus. N Engl J Med 1997; 336:1849–1854. [DOI] [PubMed] [Google Scholar]
- 13.Olmsted MP, Colton PA, Daneman D, Rydall AC, Rodin GM. Prediction of the onset of disturbed eating behavior in adolescent girls with type 1 diabetes. Diabetes Care 2008; 31:1978–1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peveler RC, Bryden KS, Neil HA, Fairburn CG, Mayou RA, Dunger DB et al. The relationship of disordered eating habits and attitudes to clinical outcomes in young adult females with type 1 diabetes. Diabetes Care 2005; 28:84–88. [DOI] [PubMed] [Google Scholar]
- 15.Goebel-Fabbri AE, Fikkan J, Franko DL, Pearson K, Anderson BJ, Weinger K. Insulin restriction and associated morbidity and mortality in women with type 1 diabetes. Diabetes Care 2008; 31:415–419. [DOI] [PubMed] [Google Scholar]
- 16.Markowitz JT, Butler DA, Volkening LK, Antisdel JE, Anderson BJ, Laffel LM. Brief screening tool for disordered eating in diabetes: internal consistency and external validity in a contemporary sample of pediatric patients with type 1 diabetes. Diabetes Care 2010; 33:495–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial Care for People With Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016; 39:2126–2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 2002; 11:1–190. [PubMed] [Google Scholar]
- 19.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mehta SN, Nansel TR, Volkening LK, Butler DA, Haynie DL, Laffel LM. Validation of a contemporary adherence measure for children with Type 1 diabetes: the Diabetes Management Questionnaire. Diabet Med 2015; 32:1232–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hood KK, Butler DA, Volkening LK, Anderson BJ, Laffel LM. The Blood Glucose Monitoring Communication questionnaire: an instrument to measure affect specific to blood glucose monitoring. Diabetes Care 2004; 27:2610–2615. [DOI] [PubMed] [Google Scholar]
- 22.Hood KK, Butler DA, Anderson BJ, Laffel LMB. Updated and revised Diabetes Family Conflict Scale. Diabetes Care 2007; 30:1764–1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001; 39:800–812. [DOI] [PubMed] [Google Scholar]
- 24.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psych Meas 1977; 1:385–401. [Google Scholar]
- 25.Roberts RE, Andrews JA, Lewinsohn PM, Hops H. Assessment of depression in adolescents using the Center for Epidemiologic Studies Depression Scale. Psychol Assess 1990; 2:122–128. [Google Scholar]
- 26.Markowitz JT, Alleyn CA, Phillips R, Muir A, Young-Hyman D, Laffel LM. Disordered eating behaviors in youth with type 1 diabetes: prospective pilot assessment following initiation of insulin pump therapy. Diabetes Technol Ther 2013; 15:428–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grylli V, Wagner G, Hafferl-Gattermayer A, Schober E, Karwautz A. Disturbed eating attitudes, coping styles, and subjective quality of life in adolescents with Type 1 diabetes. J Psychosom Res 2005; 59:65–72. [DOI] [PubMed] [Google Scholar]
- 28.Markowitz JT, Lowe MR, Volkening LK, Laffel LM. Self-reported history of overweight and its relationship to disordered eating in adolescent girls with type 1 diabetes. Diabet Med 2009; 26:1165–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scheuing N, Bartus B, Berger G, Haberland H, Icks A, Knauth B et al. Clinical characteristics and outcome of 467 patients with a clinically recognized eating disorder identified among 52,215 patients with type 1 diabetes: a multicenter german/austrian study. Diabetes Care 2014; 37:1581–1589. [DOI] [PubMed] [Google Scholar]
- 30.Merwin RM, Dmitrieva NO, Honeycutt LK, Moskovich AA, Lane JD, Zucker NL et al. Momentary Predictors of Insulin Restriction Among Adults With Type 1 Diabetes and Eating Disorder Symptomatology. Diabetes Care 2015; 38:2025–2032. [DOI] [PMC free article] [PubMed] [Google Scholar]


