Abstract
Animal studies suggest that caffeine may interfere with acupuncture analgesia (AA). This study investigated the modulation effect of daily caffeine intake on AA and brain activation in twenty-seven healthy subjects using a crossover design. We found that real acupuncture increased pain thresholds compared to sham acupuncture. Further, there was no association between caffeine intake measurements of daily caffeine use, duration of caffeine consumption, or their interaction and pre- and post-acupuncture pain threshold changes. Our findings suggest that daily caffeine intake may not influence AA in the cohort of healthy subjects that participated in study.
Keywords: acupuncture analgesia, caffeine, pain threshold, acupuncture, pain
Introduction
In a recent study on acupuncture analgesia (AA), investigators [2] found that adenosine levels increased at the acupuncture site and that mice lacking a key cell receptor for adenosine did not show the same analgesic response, suggesting that AA is mediated by increased adenosine, a neuromodulator produced when tissue is injured.
Caffeine is a common central nervous system stimulant that is found in coffee, tea, chocolate, soda, energy drinks, and even some medications [1], Since caffeine is a potent adenosine receptor antagonist, investigators have started to question whether caffeine consumption interferes with AA [3], In support of caffeine’s effect on analgesia, More et al. found that pre-administration of caffeine at moderate doses completely blocked analgesic effects for both manual and electrical acupuncture in mouse models of postoperative pain [4], Fujita et al. found that a low dose of caffeine administered at acupoints or ingested orally inhibited acupuncture analgesia and that withdrawing the caffeine restored the analgesic effect [5].
Nevertheless, whether the aforementioned results are applicable to humans remain to be determined. The present study examined, using a cross-over study design, if normal daily caffeine intake influenced acupuncture analgesia, as measured by heat and pressure pain thresholds in healthy individuals.
Materials and Methods
Subjects
Twenty-seven healthy, right-handed individuals who were acupuncture-naive were recruited for this study. The Partners Institutional Review Board (IRB) of Massachusetts General Hospital approved the study. All subjects provided written informed consent prior to participating in the research. Each subject received compensation for his/her participation. Of the 27 subjects who participated in this study, one male and two female subjects finished the initial training session but did not complete the intervention sessions. Thus, the final analyses included 24 subjects (mean (± SE), 25.21 ± 0.77 years, 16 female) who completed the study.
Experimental Procedures
The parent study included five sessions: a training and familiarity session and four intervention sessions, during which the subject received one of four treatments: 1) real acupuncture, 2) sham acupuncture, 3) imagery acupuncture, or 4) imagery acupuncture control condition. The order of the treatments was randomized using a Latin square with 4 sequences (Supplementary Figure 1). Each intervention was separated by at least 7 days. The aim of this manuscript is to investigate the modulation effect of caffeine intake on acupuncture analgesia, and we examined data obtained during the real and sham acupuncture interventions. A full description and results of the other interventions can be found in our recent publication [6].
Intervention sessions: Real acupuncture was applied on the right SP6 and SP9. Sham acupuncture was applied at two sham points using specially designed Streitberger needles [9-10] (Supplementary Figure 1). Treatment lasted about 25 minutes. During treatment, needles were frequently manipulated to obtain deqi. Subjects reported the sensations felt using the MGH Acupuncture Sensation Scale (MASS) [7-8]. Please see our recent publication [6] for more details on acupuncture treatment.
Outcome measurements
Outcome measures included local heat and pressure pain thresholds (primary outcomes) and distal heat and pressure pain thresholds (primary outcomes). All pain thresholds were measured before and after acupuncture in a quiet room outside the scanner. We tested both heat and pressure pain thresholds due to different fibers associated with the pain modalities (heat pain is primarily mediated by C-fibers, pressure pain is primarily mediated by A-delta fibers) [11]. We chose local and distal pain thresholds so that we could measure both segmental and suprasegmental analgesic effects produced by acupuncture [12].
Questionnaires
During the experiment, subjects were asked to report the average number of caffeine-containing items they consumed daily using a Daily Caffeine Consumption Questionnaire (DCCQ) adapted from the Caffeine Consumption Questionnaire by Preston, 2014 with an additional question to measure the duration of caffeine intake habits. Total caffeine consumption was calculated as the sum of caffeine (mg/day) from coffee, tea, chocolate, caffeine-containing medications (OTC or prescribed), and any other caffeinated foods and drinks [13]. Subjects were also asked to complete the Expectations for Relief Scale (ERS, 0-10 scale, “does not work at all” and 10 “complete pain relief”), to indicate how much pain relief they expected from each intervention after receiving the intervention, but prior to the post-intervention pain threshold testing.
Exploratory data analysis method
The primary outcome for this experiment was local pain threshold. We investigated the acupuncture analgesic effects and the modulation effects of caffeine consumption using mixed-model regression with pain threshold as the response and subjects as a random effect. Age and gender were included as covariates. The additional fixed effects for this model were intervention time (pre vs. post), intervention type (real vs. sham), and intervention order and their interactions. Three measures related to caffeine consumption were considered: daily amount of caffeine (mg), the duration of caffeine consumption (years), and their interaction (mg*years). Because we found a significant correlation between the daily amount of caffeine and duration of caffeine use, the three caffeine-related measures were included in the model to assess the influence of caffeine on acupuncture analgesia separately.
Results
Caffeine consumption and neuropsychological data
Based on the DCCQ, the mean (± SE) daily consumption of caffeine was 162.08 ± 30.36 mg (ranging from 0 to 500 mg) and the mean (± SE) duration of caffeine consumption was 6.75 ± 1.08 years (ranging from 0 to 16 years). The mean (± SE) MASS ratings were 1.46 ± 0.22 for real acupuncture and 0.76 ± 0.12 for sham acupuncture. There was a significant difference for acupuncture sensation (MASS) ratings between real and sham acupuncture interventions (p < 0.001). The mean (± SE) ratings of ERS for heat pain and pressure pain for the two interventions were 3.29 ± 0.34 and 3.83 ± 0.34 in the real acupuncture condition and 3.38 ± 0.41 and 3.29 ± 0.39 in the sham acupuncture condition. There was no significant difference for pain-relief expectancy between the real and sham acupuncture interventions (p = 0.723 for heat pain and p = 0.125 for pressure pain).
Effects of caffeine consumption on intervention-evoked threshold changes
Mixed-model regression analysis showed that there was a significant time by intervention interaction, indicating significant pre- and post-treatment pain threshold changes for real and sham acupuncture (heat pain on leg: p = 0.001; heat pain on arm: p = 0.002; pressure pain on leg: p < 0.001; pressure pain on fingernail: p < 0.001). The p-values for duration of caffeine consumption (years) were 0.80, 0.88, 0.83, 0.83; for daily caffeine amount (daily dose of caffeine (mg) 0.34, 0.55, 0.06, 0.08; for daily amount and duration interaction 0.58, 0.69, 0.13, 0.1; for heating pain threshold at the arm and leg, pressure pain threshold at the leg and fingernail, respectively).
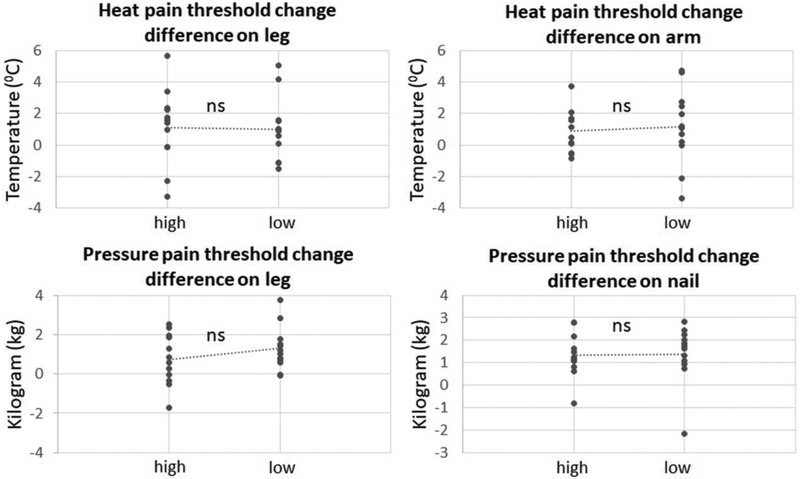
To further explore the effects of caffeine on acupuncture analgesia, we used a median split to divide the subjects into two groups based on their daily caffeine consumption (high vs. low caffeine consumption groups, n = 12 respectively). The mean (± SE) daily consumption of the high group was 272.9 ± 38.9 mg and 51.3 ± 11.6 mg for the low group. We then assessed the effects of the acupuncture interventions and caffeine consumption on subjective pain thresholds and neuropsychological ratings. Results showed the treatment responses in high and low caffeine intake groups are very similar (Figure 1)
Figure 1.
Acupuncture analgesia (AA) for the high and low caffeine consumption groups. AA is defined as the difference between real vs. sham acupuncture changes to pain threshold (post-intervention threshold - pre-intervention threshold). High = high caffeine consumption group; low = low caffeine consumption group; ns = no significant difference; dotted-lines depict the difference in mean values.
Discussion
We could not detect a modulation effect of daily caffeine consumption on the analgesic effect of acupuncture in the cohort of healthy subjects in our study. In a previous study, More et al. used two different caffeine doses that mimicked average daily consumption in Western (70 mg/kg/day) and Chinese (4 mg/kg/day) cultures. Findings indicated that that the Western dose of caffeine, which was administered for 8 days in drinking water, reversed acupuncture analgesia, whereas the Chinese dose administered during the same period did not [4]. This lack of effect following a “low” dose of caffeine on acupuncture analgesia is consistent with our findings. Our results seem inconsistent with findings from Fujita el al. [5], who found that a low dose of oral caffeine inhibited AA. We speculate that the apparent lack of effect of caffeine on AA in our study may be due to the fact that adenosine is produced when tissue is injured, the invasiveness of acupuncture stimulation in humans and rodents may differ, and most acupuncture studies of animals have used regular human acupuncture needles. In order to produce an equivalent invasiveness in humans, the needle would need to be much larger in diameter. The lack of effect may also be due to the fact that other mechanisms, such as the endogenous opioid pain modulation system, may also play an important role in AA [14-15]. It worth noting that the sample size of this study is rather small, and further studies with larger sample sizes are needed to validate our results.
Supplementary Material
Acknowledgements
Jian Kong is supported by R01 AT008563, R21 AT008707, and R61/R33 AT009310 from NIH/NCCIH.
References
- 1.Glade MJ, Caffeine-Not just a stimulant. Nutrition, 2010. 26(10): p. 932–8. [DOI] [PubMed] [Google Scholar]
- 2.Goldman N, Chen M, Fujita T, Xu Q, Peng W, Liu W, Jensen TK, Pei Y, Wang F, Han X, Chen JF, Schnermann J, Takano T, Bekar L, Tieu K, and Nedergaard M, Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nat Neurosci, 2010. 13(7): p. 883–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sawynok J, Adenosine receptor targets for pain. Neuroscience, 2016. 338: p. 1–18. [DOI] [PubMed] [Google Scholar]
- 4.More AO, Cidral-Filho FJ, Mazzardo-Martins L, Martins DF, Nascimento FP, Li SM, and Santos AR, Caffeine at Moderate Doses Can Inhibit Acupuncture-Induced Analgesia in a Mouse Model of Postoperative Pain. J Caffeine Res, 2013. 3(3): p. 143–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fujita T, Feng C, and Takano T, Presence of caffeine reversibly interferes with efficacy of acupuncture-induced analgesia. Sci Rep, 2017. 7(1): p. 3397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cao J, Tu Y, Orr SP, Lang C, Park J, Vangel M, Chen L, Gollub R, and Kong J, Analgesic Effects Evoked by Real and Imagined Acupuncture: A Neuroimaging Study. Cereb Cortex, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kong J, Gollub R, Huang T, Polich G, Napadow V, Hui K, Vangel M, Rosen B, and Kaptchuk TJ, Acupuncture de qi, from qualitative history to quantitative measurement. J Altern Complement Med, 2007. 13(10): p. 1059–70. [DOI] [PubMed] [Google Scholar]
- 8.Spaeth RB, Camhi S, Hashmi JA, Vangel M, Wasan AD, Edwards RR, Gollub RL, and Kong J, A longitudinal study of the reliability of acupuncture deqi sensations in knee osteoarthritis. Evid Based Complement Alternat Med, 2013. 2013: p. 204259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Streitberger K and Kleinhenz J, Introducing a placebo needle into acupuncture research. Lancet, 1998. 352: p. 364–365. [DOI] [PubMed] [Google Scholar]
- 10.Kong J, Gollub RL, Rosman IS, Webb JM, Vangel MG, Kirsch I, and Kaptchuk TJ, Brain activity associated with expectancy-enhanced placebo analgesia as measured by functional magnetic resonance imaging. J Neurosci, 2006. 26(2): p. 381–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Angst MS, Tingle M, Phillips NG, and Carvalho B, Determining heat and mechanical pain threshold in inflamed skin of human subjects. J Vis Exp, 2009(23). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coronado RA, Kindler LL, Valencia C, and George SZ, Thermal and pressure pain sensitivity in patients with unilateral shoulder pain: comparison of involved and uninvolved sides. J Orthop Sports Phys Ther, 2011. 41(3): p. 165–73. [DOI] [PubMed] [Google Scholar]
- 13.Preston J, O’Neal J, and Talaga M, A consumer’s guide to psychiatric drugs: Straight talk for patients and their families. 2014: New York. [Google Scholar]
- 14.Han JS, Acupuncture analgesia: areas of consensus and controversy. Pain, 2011. 152(3 Suppl): p. S41–8. [DOI] [PubMed] [Google Scholar]
- 15.Dougherty DD, Kong J, Webb M, Bonab AA, Fischman AJ, and Gollub RL, A combined [11C]diprenorphine PET study and fMRI study of acupuncture analgesia. Behav Brain Res, 2008. 193(1): p. 63–8 PMCID: PMC2538486. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.