Abstract
Background
Hyperzincemia and hypercalprotectinemia (Hz/Hc) is a distinct autoinflammatory entity involving extremely high serum concentrations of the proinflammatory alarmin myeloid-related protein (MRP) 8/14 (S100A8/S100A9 and calprotectin).
Objective
We sought to characterize the genetic cause and clinical spectrum of Hz/Hc.
Methods
Proline-serine-threonine phosphatase-interacting protein 1 (PSTPIP1) gene sequencing was performed in 14 patients with Hz/Hc, and their clinical phenotype was compared with that of 11 patients with pyogenic arthritis, pyoderma gangrenosum, and acne (PAPA) syndrome. PSTPIP1-pyrin interactions were analyzed by means of immunoprecipitation and Western blotting. A structural model of the PSTPIP1 dimer was generated. Cytokine profiles were analyzed by using the multiplex immunoassay, and MRP8/14 serum concentrations were analyzed by using an ELISA.
Results
Thirteen patients were heterozygous for a missense mutation in the PSTPIP1 gene, resulting in a p.E250K mutation, and 1 carried a mutation resulting in p.E257K. Both mutations substantially alter the electrostatic potential of the PSTPIP1 dimer model in a region critical for protein-protein interaction. Patients with Hz/Hc have extremely high MRP8/14 concentrations (2045 ± 1300 μg/mL) compared with those with PAPA syndrome (116 ± 74 μg/mL) and have a distinct clinical phenotype. A specific cytokine profile is associated with Hz/Hc. Hz/Hc mutations altered protein binding of PSTPIP1, increasing interaction with pyrin through phosphorylation of PSTPIP1.
Conclusion
Mutations resulting in charge reversal in the y-domain of PSTPIP1 (E→K) and increased interaction with pyrin cause a distinct autoinflammatory disorder defined by clinical and biochemical features not found in patients with PAPA syndrome, indicating a unique genotype-phenotype correlation for mutations in the PSTPIP1 gene. This is the first inborn autoinflammatory syndrome in which inflammation is driven by uncontrolled release of members of the alarmin family.
Keywords: Hyperzincemia and hypercalprotectinemia, myeloid-related protein 8/14, calprotectin, S100 proteins, zinc, proline-serine-threonine phosphatase-interacting protein 1, pyogenic arthritis, pyoderma gangrenosum, and acne syndrome, genotype, phenotype, autoinflammation
Myeloid-related protein (MRP) 8 (S100A8) and MRP14 (S100A9) are endogenous ligands of Toll-like receptor (TLR) 41 that are highly expressed in granulocytes, monocytes, and activated keratinocytes.2 Both proteins belong to the family of alarmins, which are danger signals released during cellular stress or damage; have strong proinflammatory effects in vitro3–7; and promote inflammation in vivo.8–10 Highly increased serum concentrations of MRP8/14 complexes (calprotectin) have been reported in patients with systemic juvenile idiopathic arthritis (SJIA) and familial Mediterranean fever (FMF; OMIM #249100).11,12
Hypercalprotectinemia and hyperzincemia (Hz/Hc) is a rare autoinflammatory condition characterized by marked dysregulation of MRP8/14 metabolism associated with accumulation of zinc caused by the zinc-binding capacities of MRP8/14.2 Together with extremely high MRP8/14 serum levels, the syndrome is characterized by severe systemic and cutaneous inflammation, hepatosplenomegaly, arthritis, pancytopenia, and failure to thrive.2 The genetic cause of the disease has not been identified thus far.2,13–15
Proline-serine-threonine phosphatase-interacting protein 1 (PSTPIP1; also known as CD2BP1) is a cytoskeleton-associated adaptor protein that modulates T-cell activation,16 cytoskeletal organization, and IL-1β release.17 Heterozygous mutations in the PSTPIP1 gene cause the dominantly inherited pyogenic arthritis, pyoderma gangrenosum, and acne (PAPA) syndrome (OMIM #604410). PAPA syndrome is a rare autosomal dominant autoinflammatory disease typically caused by the missense mutations p.A230T (c.688G>A) and p.E250Q (c.748G>C) in PSTPIP1.18 Mutations causing PAPA syndrome are thought to disrupt the interaction of PSTPIP1 with a protein tyrosin phophatese (PTP-PEST), a regulatory phosphatase, leading to uncontrolled secretion of IL-1β, probably through binding to pyrin, which is mutated in patients with FMF.19 Patients with PAPA syndrome typically present with recurrent sterile pyogenic arthritis in childhood, occurring spontaneously or after minor trauma. In adolescence the propensity for cutaneous inflammation increases, encompassing severe cystic acne, and recurrent pyoderma gangrenosum–like ulcers, including the positive pathergy phenomenon.20 In contrast, systemic inflammation, failure to thrive, and high mortality are not part of the clinical picture of PAPA syndrome.
In this study, for the first time, we identified de novo p.E250K and p.E257K mutations in the PSTPIP1 gene as the cause of Hz/Hc disease and characterized this autoinflammatory entity in comparison with PAPA syndrome. We here describe the first inherited syndrome in which the inflammatory pathogenesis is largely driven by unrestrained release of proinflammatory danger signals of the alarmin family.
Methods
Patients and samples
This study was approved by the Medical Ethics Committee at the University of Muenster, Muenster, Germany, and performed in accordance to the Helsinki Declaration. All patients or relatives provided written informed consent. Fourteen patients with Hz/Hc were enrolled. Patients P1,2 P2,13 P3,14 P4,15 and P1121 have been previously reported. Patients’ clinical symptoms are summarized in Table E1 and the Methods section in this article’s Online Repository at www.jacionline.org.
Patients with PAPA syndrome, SJIA, and FMF
As a control group, 11 patients with genetically confirmed PAPA syndrome (8 patients carrying the p.A230T mutation, 2 patients with the p.E250Q mutation, and 1 patient with the p.E256G mutation) were included (for patient’s details, see Table E2 in this article’s Online Repository at www.jacionline.org). Patients PI and PII have been reported previously.22 Furthermore, 20 patients with active SJIA (sex, 12 male/8 female; age range, 7-16 years), 20 patients with active FMF (9 male/11 female; age range, 8-17 years), and 20 healthy control subjects (11 male/9 female; age range, 7-24 years) were included for serologic studies.
Analysis of MRP8/MRP14 in serum and skin and zinc serum levels
Serum concentrations of MRP8/14 were determined by using a sandwich ELISA, as previously described. The readers of the laboratory assay were blinded for diagnosis and inflammatory activity of the patients. Skin sections of patient P1 were stained with monospecific affinity-purified rabbit antisera to MRP8 and MRP14. Immunostaining was performed with a standard 3-stage immunoperoxidase method, as previously described.3 Zinc serum levels were determined by using atomic absorption spectroscopy. Normal serum levels were defined as 11.5 to 21.4 μmol/L (95% CI).
Analysis of anti-neutrophil antibodies
Neutrophil-reactive antibodies were detected by using the agglutination, microscopic immunofluorescence, and mAb-specific immobilization of neutrophil antigen assay, as previously described.23
Genotype analysis
In patients with Hz/Hc, exons 1 to 15 of the PSTPIP1 gene and all 10 exons of the Mediterranean fever gene were sequenced. PCR amplification products of exons were purified with the ExoSAP-IT reagent (USB, Cleveland, Ohio) and sequenced with the ABI PRISM Big Dye Terminator v3.1 Ready Reaction Cycle Sequencing kit and the ABI PRISM 3130 Genetic Analyzer (Applied Biosystems, Foster City, Calif).
Structural model and sequence alignment
The PSTPIP1 sequence (residues 3-285, UniProtKB code O43586) was defined as the target, and the F-bar domain of FCHo2 (PDB ID 2V0O, residues 2-271) with a sequence identity of 23% served as the template.24 Homology models were based on an alignment using the Clustal Omega tool25 and built with the MODELLER program.26 One thousand models were calculated and clustered, and the model with the best ANOLEA score27 belonging to the largest cluster was further refined. A dimeric structure was generated by aligning 2 copies of the resulting model with chains A and B of the x-ray structure 2V0O and minimizing them by using the CHARMM22 all-atom force field.28 Structural models for the mutant proteins p.E250K and p.E257K, as well as for the PAPA syndrome mutant p.E250Q, were generated by mutating the respective amino acids of the dimer model and reminimizing the structure. For each of the 4 models, the electrostatic potential was calculated with the UHBD code.29 The FoldX program was used to perform an in silico alanine scan by mutating each residue to an alanine and estimating the resulting change in folding energy.30 Molecular visualization was done with CHIMERA.31
Immunoprecipitation and phosphorylation of PSTPIP1
HEK293 cells were transfected (PolyFect; Qiagen, Hilden, Germany) with wild-type (WT) enhanced green fluorescent protein–PSTPIP1 or p.E250Q or p.E250K mutated enhanced green fluorescent protein–PSTPIP1 and pyrin for coprecipitation or cAbl (31284;pSG5-ABL; Addgene, Cambridge, Mass) for detection of tyrosine phosphorylated proteins. Transfected HEK cells were incubated in lysis buffer (50 mmol/L Tris [pH 7.7], 300 mmol/L NaCl, 2 mmol/L MgCl, 0.1% Chaps, and protease inhibitor cocktail; Roche, Mannheim, Germany) for 20 minutes on ice and pushed through a 15-gauge cannula. For detection of phosphotyrosine, 0.4 mmol/L Na3VO4 was added to lysis buffer. After centrifugation, supernatants were incubated overnight at 4ºC for coprecipitation of pyrin or for 3 hours at 4ºC for detection of tyrosine phosphorylated proteins with antibody (mouse α-PSTPIP1 [ab88474]; Abcam, Cambridge, United Kingdom) linked to a/g agarose beads (Pierce Biotechnology, Rockford, Ill). After washing, samples were analyzed by means of SDS-PAGE and Western blotting with appropriate antibodies (rabbit α-PSTPIP1 [HPA 010600]; Atlas Antibodies, Stockholm, Sweden; mouse α-phosphotyrosine [4G10]; Merck Millipore, Darmstadt, Germany). Additionally, coimmunoprecipitation band intensities of blots from 3 independent experiments were densitometrically analyzed with ImageJ 1.46r (National Institutes of Health, Bethesda, Md). All values were normalized to the PSTPIP1 value.
Extracellular cytokine measurement
Cytokines and soluble receptors were measured in serum by using a multiplex immunoassay, as previously described.32 Acquisition of data was performed with the FlexMap3D system (Bio-Rad Laboratories, Hercules, Calif) and xPonent v4.2 software (Luminex, Austin, Tex). Data analyses were performed by using Bio-Plex Manager software version 6.1.1 with 5 parametric curve fitting (Bio-Rad Laboratories). Cytokines analyzed included IL-1α, IL-1β, IL-2, IL-4, IL-15, IL-6, IL-8, IL-10, IL-12, IL-13, IL-15, IL-17, IL-18, IL-21, IL-22, IL-33, CCL2, CCL3, CCL11, CCL17, CCL18, CCL22, CXCL9, granulocyte colony-stimulating factor, GM-CSF, macrophage colony-stimulating factor, IFN-α, IFN-γ, macrophage migration inhibitory factor (MIF), intercellular adhesion molecule, vascular cell adhesion molecule, receptor activator of nuclear factor κB ligand, IFN-γ–induced protein 10, and TNF-α. Serum samples for this analysis were immediately frozen and shipped on dry ice.
Statistical analysis
Statistical analyses were performed with Prism 5.0 software (GraphPad Software, La Jolla, Calif). Analyses between 2 groups were performed with an unpaired 2-tailed Student t test. Comparisons among 3 or more groups were performed by using 1-way ANOVA, followed by Bonferroni multiple means tests for comparing all pairs of columns. Differences in protein serum profiles were analyzed by using the Mann-Whitney U test. Differences were considered statistically significant at a P value of less than .05.
Results
Characterization of clinical phenotype in patients with Hz/Hc
Patients with Hz/Hc had a persistent early-onset (median age at disease onset, 13 months) inflammatory disease characterized by cutaneous inflammation (12/14), (hepato)splenomegaly (12/14), failure to thrive (9/14), lymphadenopathy (6/14), and joint involvement (arthritis in 7/14 and arthralgia/morning stiffness in 2/14). Most of these patients showed marked abnormalities in hematologic parameters, including neutropenia (14/14), anemia (hemoglobin, <100 g/L; n = 13/14), and thrombocytopenia (7/14, see Table E1). As a consequence of the detected pancytopenia, bone marrow biopsy specimens were analyzed in 8 patients showing dyserythropoiesis, fibrosis, and lymphocytosis. Additionally, the frequency of anti-neutrophil antibodies was screened in serum of 12 of 14 patients with Hz/Hc and 9 of 11 patients with PAPA syndrome. We found a constellation of autoimmune neutropenia (AIN) in 4 patients and a constellation consistent with AIN (without identification of antigen) in 4 other patients with Hz/Hc (66% together), whereas only in 3 patients with classical PAPA syndrome could such a constellation be found (33%, see Table E3 in this article’s Online Repository at www.jacionline.org). Analysis of B-cell subpopulations (total [CD19+], transitional [CD24++ and CD38++], naive [CD27−, IgG−, and IgA−], memory [CD27+], IgM memory [CD27+, IgG−, and IgA−], and switched memory [CD27+, IgG+, and IgA+]) did not show relevant changes in 5 patients with Hz/Hc (E250K) or 5 patients with PAPA syndrome (3 E250Q and 2 E256G) when compared directly or with healthy control subjects.
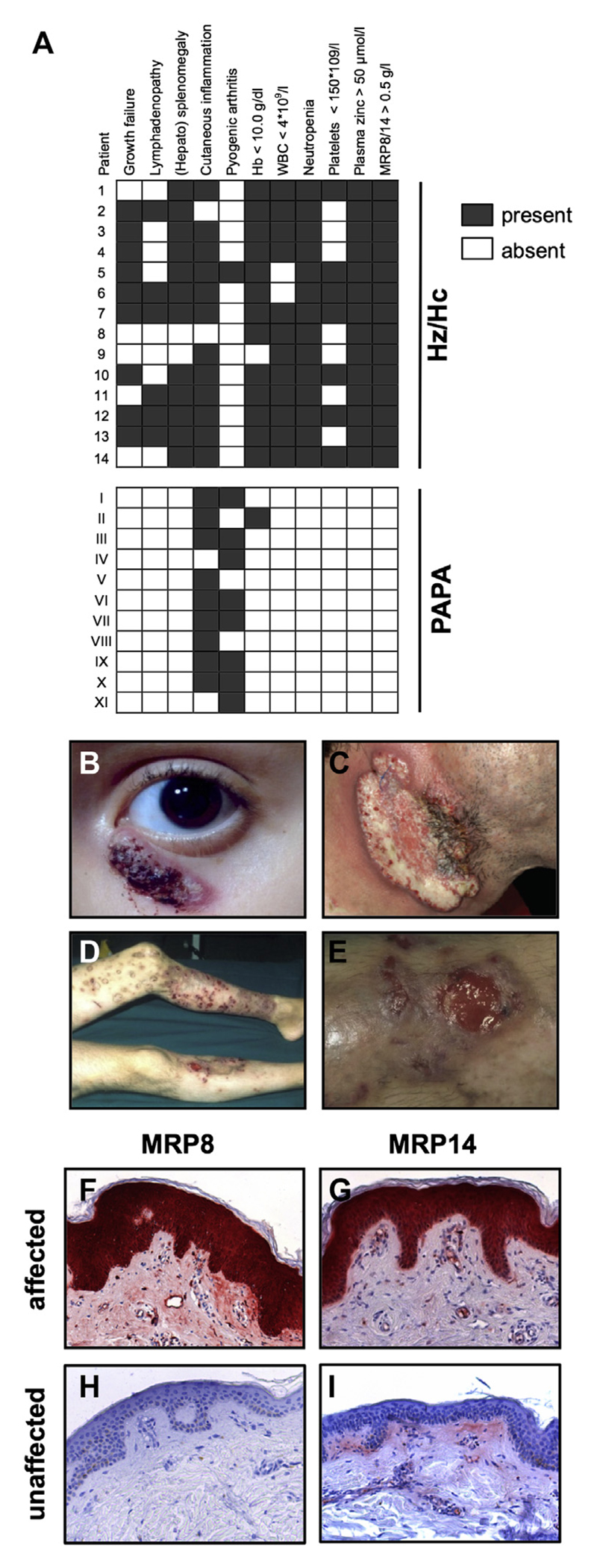
Interestingly, in the cohort of patients with PAPA syndrome (n = 11) the most relevant clinical findings of anemia, neutropenia, thrombocytopenia, (hepato)splenomegaly, and failure to thrive were absent (see Table E2). Inversely, pyogenic arthritis, a prominent clinical feature of PAPA syndrome (n = 8/11) was present in only 1 patient with Hz/Hc. The only common clinical symptom in both groups was skin inflammation (PAPA syndrome, n = 9/11; Hz/Hc, n = 12/14), which appeared in a variety of manifestations. The significance of the differences in the clinical phenotype and laboratory findings is depicted in Fig 1, A (median age at disease onset in patients with PAPA syndrome, 4 years).
Fig 1.
Hz/Hc can be distinguished from PAPA syndrome based on clinical symptoms and laboratory parameters. A, Characteristic clinical symptoms and laboratory parameters present or absent in patients with Hz/Hc and those with PAPA syndrome. B-I, Palpebral lesions (Fig 1, B), pyoderma gangrenosum–like ulcers (Fig 1, C) or ulcerative dermatitis (Fig 1, D and E), and MRP14 expression in affected (Fig 1, F and G) and unaffected (Fig 1, H and I) skin of patient 1.
Among cutaneous findings, palpebral lesions occurred in 2 patients with Hz/Hc (Fig 1, B), whereas they were absent in patients with PAPA syndrome. Patient P1 had pyoderma gangrenosum (Fig 2, C) and several ulcers in the lower extremities (Fig 1, D and E). Here, biopsy samples from affected and unaffected skin showed a dramatic upregulation of MRP8 and MRP14 in hyperproliferative epidermis and marked leukocyte infiltration in inflamed dermis (Fig 1, F and G) in contrast to clinically unaffected skin from the same patient (Fig 1, H and I).
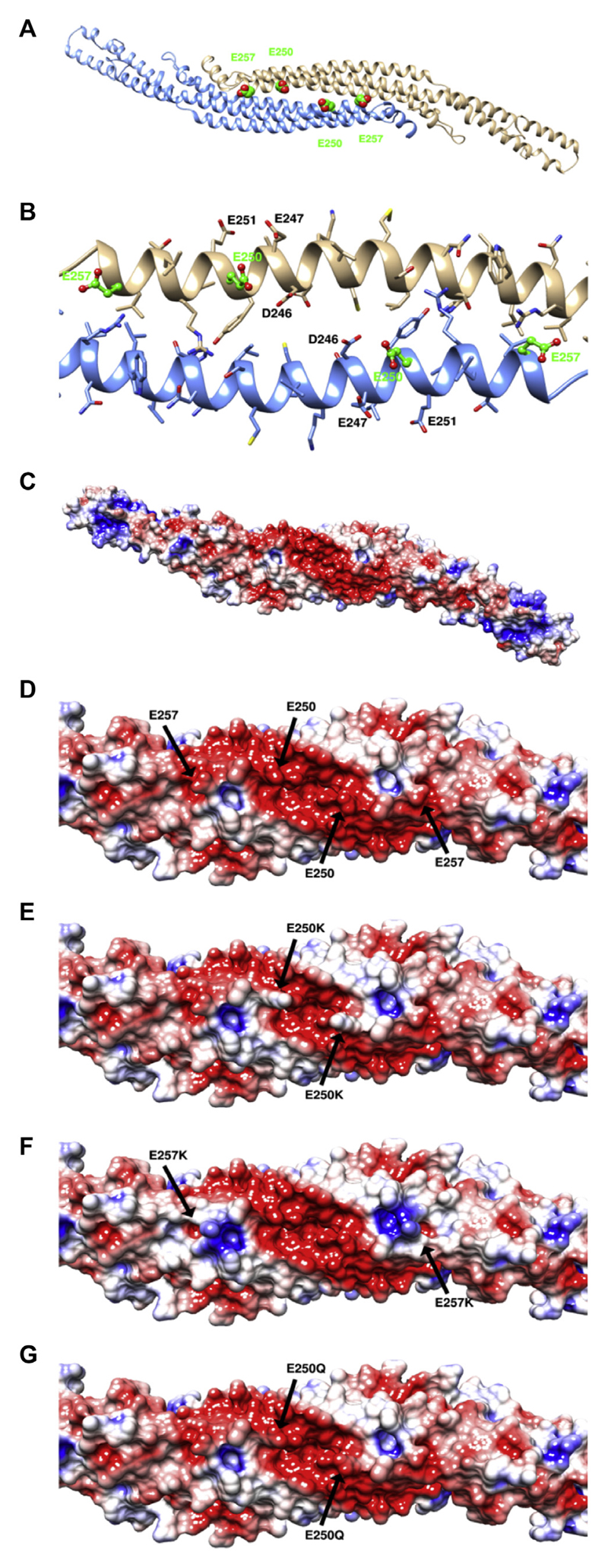
Fig 2.
Mutations of patients with Hz/Hc alter the electrostatic potential of PSTPIP1. A, PSTPIP1 FCH domain in a ribbon diagram of PSTPIP1 dimer with Hz/Hc mutations (green). B, p.E250 in a cluster of 4 negatively charged side chains. C-G, Electrostatic potential in (blue, positive charge; red, negative charge; Fig 2, C) in WT (Fig 2, D), p.E250K (Fig 2, E), p.E257K (Fig 2, F), and p.E250Q mutants (Fig 2, G).
Cutaneous inflammation was characterized by an unspecific infiltrate composed of neutrophils and macrophages admixed with plasma cells, as well as perivascular lymphocellular infiltrations in 5 patients with Hz/Hc.
Genetic studies
Interestingly, genetic analyses of patients with Hz/Hc revealed in all of them an amino acid exchanges from the acidic glutamic acid to basic lysine. In patients P1 to P13, the heterozygous G>A transition at the c.748 position in exon 11 of the PSTPIP1 gene, leading to the missense p.E250K variant, was found.21 In patient P14 the heterozygous G>A transition at c.769 position, also in exon 11 and leading to the missense p.E257K variant, was found. Multiple sets of evidence indicate that these 2 variants are very likely deleterious for the structure, function, or both of PSTPIP1: their absence in the database of genomic diversity (0% allele frequency for the 2 variants in the 1000 Genomes project), in silico analyses with the algorithms SIFT and Polyphen-2 (deleterious and probably damaging), and family-based cosegregation studies. Parental DNA was available from patients P2 to P8, P12, and P13, which confirmed a de novo mutation in 8 patients. Patients P9 (father) and P8 (son) shared the same PSTPIP1 E250K mutation, and both were affected with a variable clinical expression.
In all patients carrying the mutations, we detected excessively increased MRP8/14 and zinc serum levels compatible with earlier findings reported in patients with Hz/Hc (see Table E1).
Alteration of electrostatic potential of PSTPIP1
Both 250 and 257 residues are located on the convex face of the dimeric PSTPIP1 model, close to the dimer interface but exposed to the solvent (Fig 2, A). Because α helices have a periodicity of 3.6, both mutations point to the same face of the helix and to the outside of the structure. Moreover, copies of E250 and, to a lesser degree, E257 from chains A and B are in proximity, suggesting that their influence could be potentiated in the dimer. E250 is located in a cluster of 4 negatively charged side chains formed by D246, E247, E250, and E251 (Fig 2, B). An in silico alanine scan suggests that neither E250 nor E257 is relevant for the structural integrity of the protein. The electrostatic potential projected on the molecular surface of the PSTPIP1 model (Fig 2, C and D) displays a large negative patch in the central part of the convex face that has been proposed to be important for pyrin and PTP-PEST binding. Both mutants, p.E250K and p.E257K, substantially affect this negative patch of WT PSTPIP1 (Fig 2, E and F), whereas the influence of the PAPA syndrome mutant p.E250Q on the electrostatic potential is much less pronounced (Fig 2, G).
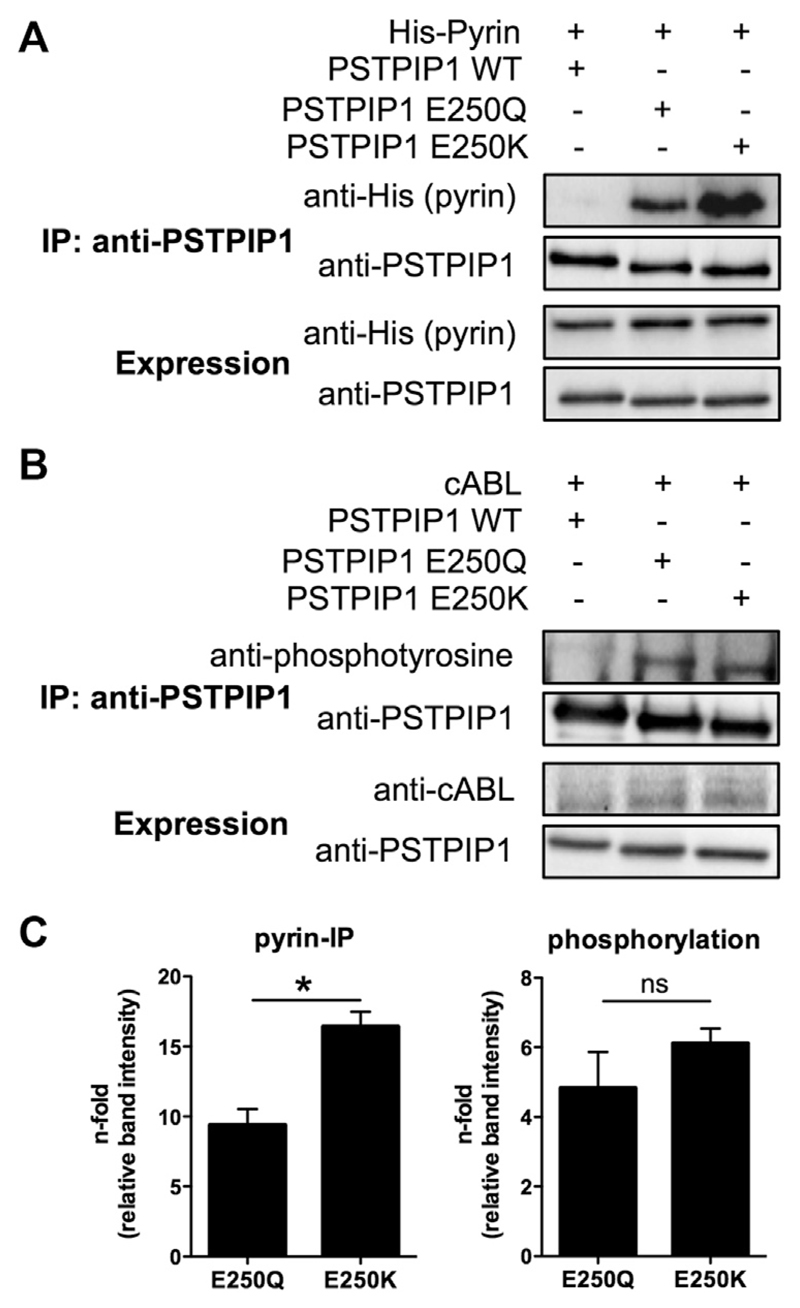
Binding of pyrin and phosphorylation of PSTPIP1
The PAPA syndrome–associated p.E250Q mutation causes increased pyrin binding and hyperphosphorylation of PSTPIP1. Therefore we tested the effect of the p.E250K mutation on phosphorylation and pyrin binding. Relative to the E250Q mutant, the E250K mutant exhibits markedly increased binding to pyrin (Fig 3, A). The 2 mutant proteins were hyperphosphorylated relative to WT in the presence of the cAbl kinase (Fig 3, B). Although the increase in PSTPIP1-pyrin binding was significant, phosphorylation only showed a tendency toward stronger p.E250K hyperphosphorylation (Fig 3, C).
Fig 3.
p.E250K mutation increases PSTPIP1-pyrin binding. A, Cotransfection with pyrin and PSTPIP1 WT or p.E250Q or p.E250K mutants. Immunoprecipitation (IP) was performed with anti-PSTPIP1 and immunoblotted with anti-pyrin and anti-PSTPIP1. B, Cotransfection with PSTPIP1 WT, p.E250Q or p.E250K mutants, and cAbl. Immunoprecipitation with anti-PSTPIP1, phosphorylation was detected with anti-phosphotyrosine. C, Relative band intensity was measured and expressed as n-fold to PSTPIP1 WT. *P < .05.
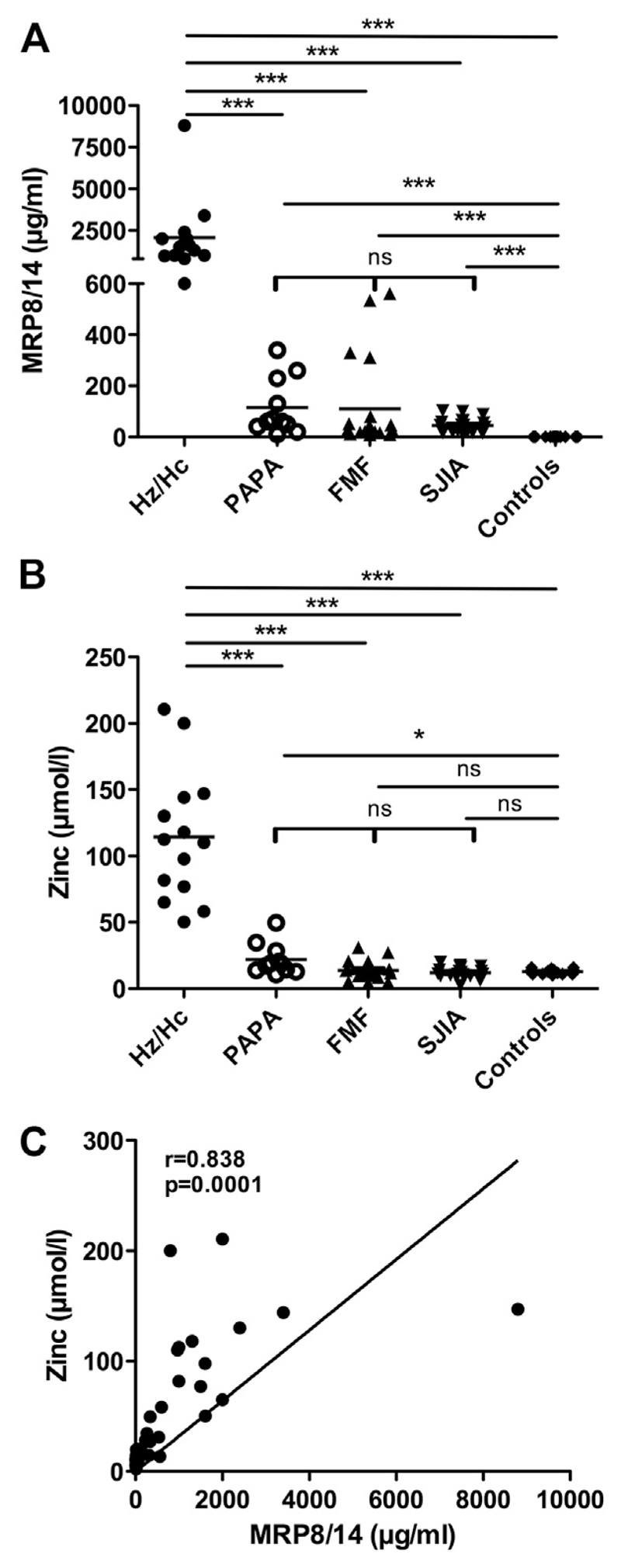
Serum concentration of MRP8/14 and zinc in patients with PSTPIP1 mutations
Serum samples were obtained at the time of clinical and serologic active disease. Serum concentrations of MRP8/14 in patients with Hz/Hc (mean ± 95% CI, 2070 ± 1190 μg/mL) were found to be significantly increased (up to 20-fold) compared with those in patients with PAPA syndrome (116 ± 74 μg/mL, P < .001; Fig 4, A). Levels in healthy control subjects were 0.48 ± 0.1 μg/mL.33 We have previously shown that MRP8/14 levels are increased in patients with SJIA and FMF at the time of clinical and serologic active disease.11,12 However, the MRP8/14 levels in patients with Hz/Hc were more than 20 or 40 times higher than those in patients with FMF (110 ± 82 μg/mL) or SJIA (45 ± 13 μg/mL, both P < .001), respectively. There were no significant differences among patients with PAPA syndrome, FMF, and SJIA. Concomitantly, zinc levels were found to be significantly increased in patients with Hz/Hc (114.5 ± 28.3 μmol/L) compared with those in patients with PAPA syndrome (21.9 ± 7.8 μmol/L), FMF (14 ± 8 μmol/L), and SJIA (12.1 ± 1.9 μmol/L) or healthy control subjects (12.8 ± 1.0 μmol/L, all P < .001; Fig 4, B). The degree of increase in MRP8/14 and zinc levels correlated closely in the entire patient cohort (r = 0.838, P <.001; Fig 4, C).
Fig 4.
Patients with Hz/Hc can be distinguished from those with PAPA syndrome, FMF, or SJIA based on MRP8/14 and zinc serum levels. A and B, MRP8/14 (Fig 4, A) and zinc (Fig 4, B) serum levels in patients with active disease (patients with Hz/Hc, n = 13; patients with PAPA syndrome, n = 11), patients with FMF (n = 20), patients with SJIA (n = 20), or healthy control subjects (n = 20). C, Correlation of MRP8/14 and zinc levels in all patients. *P < .05 and ***P < .001.
Serum cytokine profile of Hz/Hc and PAPA syndrome
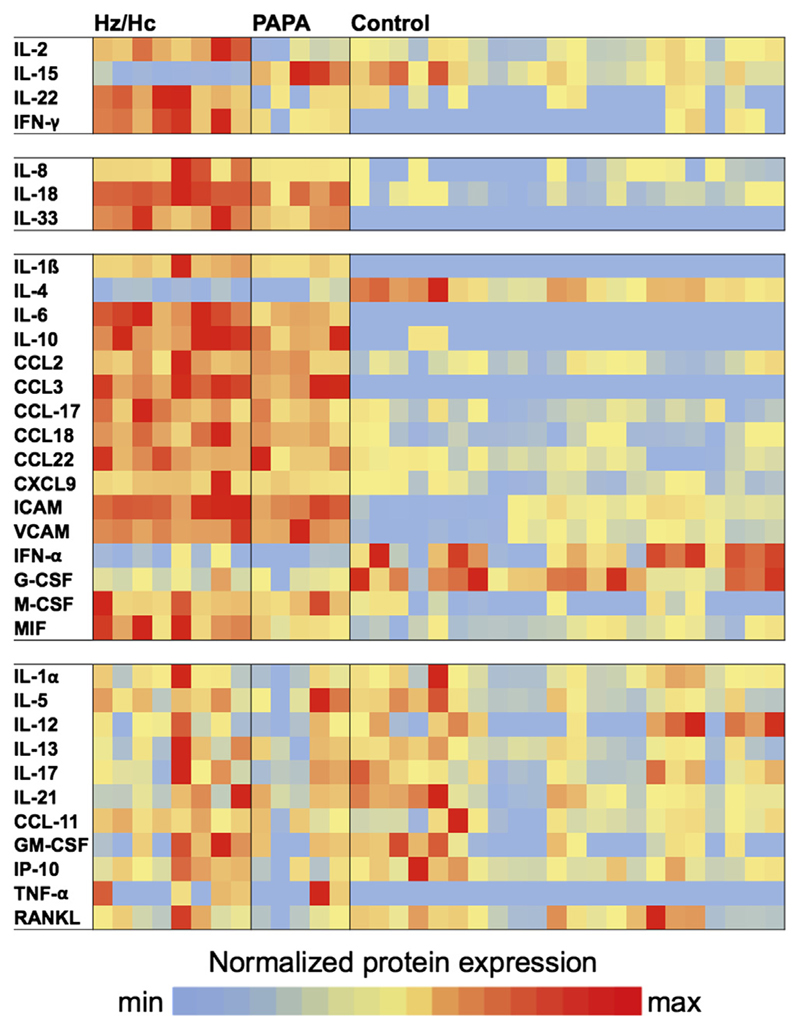
In view of the increased MRP8/14 levels detected in patients with Hz/Hc, we investigated the profile of circulating cytokines to define an inflammatory signature using serum samples obtained during active disease from 8 patients with Hz/Hc (7 with p.E250K and 1 with p.E257K), 5 patients with PAPA syndrome (2 with p.A230T, 2 with p.E250Q, and 1 with p.E256G), and 22 healthy control subjects (female/male sex, 12/10; age range, 3-16 years). All samples were obtained at the time of clinical and serologic active disease. Expression levels were stratified into (1) cytokines that were only upregulated or downregulated in patients with Hz/Hc (ie, IL-2, IL-15, IL-22, and IFN-γ); (2) cytokines that were upregulated in patients with Hz/Hc and those with PAPA syndrome but significantly higher in patients with Hz/Hc (ie, IL-8, IL-18, and IL-33); and (3) cytokines that were significantly upregulated or downregulated in patients with Hz/Hc and those with PAPA syndrome compared with control subjects (ie, IL-1β, IL-4, IL-6, IL-10, CCL2, CCL3, CCL17, CCL18, CCL22, CXCL9, intercellular adhesion molecule, vascular cell adhesion molecule, IFN-α, macrophage colony-stimulating factor, and MIF). Levels of IL-1α, IL-5, IL-12, IL-13, IL-17, IL-21, CCL11, granulocyte colony-stimulating factor, GM-CSF, IFN-γ–induced protein 10, TNF-α, and receptor activator of nuclear factor κB ligand were not significantly different from those in control subjects (Fig 5 and see Table E4 in this article’s Online Repository at www.jacionline.org).
Fig 5.
Patients with Hz/Hc can be distinguished from patients with PAPA syndrome and healthy control subjects based on serum protein expression levels. Protein serum concentration levels were classified by differential expression between patients with Hc/Hz, patients with PAPA syndrome, and control subjects. Expression values are normalized for each gene to the healthy group. Transformed expression levels are indicated by color scale with relatively high (red) and relatively low (blue) expression.
Response to treatment
Response to treatment was evaluated in all patients with Hz/Hc (see Table E5 in this article’s Online Repository at www.jacionline.org). Interestingly, no consistently effective therapy was observed. Best responses were noted when using IL-1 inhibitors, either anakinra (n = 4) or canakinumab (n = 1), but there were a few patients who were unresponsive to this therapy (n = 5). Treatment with cyclosporine (n = 5) or prednisolone (n = 6) resulted in a partial response. Of note, cutaneous symptoms, arthritis, anemia, and systemic inflammation improved, but neutropenia persisted in all patients after treatment. In 3 patients (hepato)splenomegaly resolved with treatment.
Serum profiles of cytokines, MRP8/14, and zinc were investigated in paired samples of 4 patients with a partial response to IL-1 or TNF inhibition or GM-CSF and 4 patients with no response to IL-1 or TNF inhibition and a flare under continuous treatment with cyclosporine. Partial response to treatment was accompanied in all 4 treated patients by a decrease of IL-8, IL-18, IL-33, IL-6, CCL18, MIF, MRP8/14, and zinc serum concentrations (see Figs E1 and E2 in this article’s Online Repository at www.jacionline.org).
Discussion
Hz/Hc is an autoinflammatory disorder characterized by chronic systemic inflammation, prominent skin inflammation, arthralgia/arthritis, hepatosplenomegaly, pancytopenia, and failure to thrive.2 A hallmark of the disease is the extreme increase in serum concentrations of the proinflammatory alarmins MRP8 and MRP14 and concomitantly zinc. In this study we report the genetic cause for this disorder, namely a single amino acid substitution in the y-domain of PSTPIP1 (E→K) either at position p.E250 or p.E257. Clinically, Hz/Hc is distinct from the other PSTPIP1-associated disease, PAPA syndrome, based on the presence of a severe course and early-onset disease, hepatosplenomegaly, and failure to thrive. Variable expressivity of disease was noted both in patients with Hz/Hc and those with PAPA syndrome, with patient P8 showing a weaker phenotype than his father (patient P9) in the cohort with Hz/Hc. Incomplete penetrance has been previously reported in families with PAPA syndrome21 and seems also to be a feature of the p.E250K mutation. Two patients with Hz/Hc died of postoperative complications after liver transplantation or sepsis.
Regarding laboratory findings, Hz/Hc is characterized by severe anemia and neutropenia, which is present in all patients and accompanied by thrombocytopenia in most patients. By contrast, anemia and neutropenia were not or only rarely observed in patients with PAPA syndrome. Bone marrow aspirates in patients with Hz/Hc showed evidence of dysgranulopoiesis and dyserythropoiesis, which is consistent with observed pancytopenia. It is yet unclear whether the hematologic findings are related to chronic inflammation or could be the result of altered PSTPIP1 function. PSTPIP1 is known to regulate neutrophil and macrophage functions,34,35 but its role in cell maturation has not been reported. Because of the severe neutropenia, we were not able to perform functional studies with purified neutrophils. In addition, patients with Hz/Hc could be clearly separated from patients with PAPA syndrome based on extremely high MRP8/14 and zinc serum levels. In summary, these data suggest a unique genotype-phenotype correlation for mutations in the PSTPIP1 gene.
MRP8/14 alarmins have been identified as endogenous ligands for TLR4-mediated expression of proinflammatory cytokines, chemokines, NADPH oxidase, or adherence molecules.1,6,7,11 The extremely high expression of this endogenous TLR4 ligand in patients with Hz/Hc suggests a role for MRP8/14 in the pathogenesis of severe PSTPIP1-mediated inflammation. In addition, patients with Hz/Hc could be clearly differentiated from those with PAPA syndrome based on a distinct cytokine profile (Table E3). Interestingly, many of these proteins play a role in positive inflammatory feedback mechanisms between innate immune cells and the epithelium.36–38 IL-22 and combination of IFN-γ and TNF-α are known inducers of MRP expression in epithelial cells.37–39
Hyperzincemia is caused by the zinc-capturing properties of MRP8/14,2 and zinc levels are increased in patients with Hz/Hc but not in patients with PAPA syndrome, FMF, or SJIA. Usually inflammation induces a reduction in plasma zinc concentrations because of redistribution in the cellular compartment.39 In patients with sepsis, lower plasma zinc concentrations were associated with higher illness scores and increased cytokine production.40 Therefore the unique high zinc levels in patients with Hz/Hc are interesting observations in an inflammatory context. Zinc deficiency is associated with higher IL-1β production and lower IL-2 and IL-6 production.41–44 Conversely, in promonocytic cells zinc increased both IL-6 and IL-8 levels,45 and under inflammatory conditions, IFN-γ gene expression seems to be reduced by zinc deficiency.46,47 Therefore hyperzincemia might contribute to the high IL-2, IL-6, IL-8, and IFN-γ levels found in patients with Hz/Hc.
Among the identified cytokines, some are characteristic for the T-cell compartment as IL-2 or IL-22, indicating a role of the adaptive immune system in patients with Hz/Hc. Additionally, in a murine model of systemic autoimmune disease, we have shown that MRP8 and MRP14 expression at the site of inflammation is essential for the development of autoreactive T cells and promotion of systemic autoimmunity.8 This mechanism might enhance inflammation in the chronic phase of this autoinflammatory syndrome. Although B-cell distribution was normal in patients with Hz/Hc and those with PAPA, we found serologic constellations of AIN as a result of anti-neutrophil antibody production in both phenotypes (66% vs 33% of samples). Because autoantibodies were not found in all neutropenic patients, this seems not to be the only responsible mechanism. However, AIN might contribute to neutropenia in patients with Hz/Hc and seems to be a result of the activation of the adaptive immune system within an autoinflammatory disease.
The p.E250K and p.E257K substitutions in PSTPIP1 are located within the coiled-coil region, which is important for pyrin and PTP-PEST interaction. The electrostatic modeling of PSTPIP1 displays a large negative patch in the critical region that is significantly affected by both mutations but not found for the classical PAPA-associated mutation E250Q. The PAPA-causing mutations have been shown to disrupt PSTPIP1-PEST phosphatase interactions, resulting in hyperphosphorylation of PSTPIP1 and increased pyrin avidity.19 This binding might release pyrin from its autoinhibition, triggering increased apoptosis-associated speck-like protein containing a carboxyterminal CARD oligomerization and caspase-1 activation.48 Furthermore, the increased PSTPIP1-pyrin avidity also results in altered PSTPIP1 cellular distribution and its greater colocalization with the apoptosis-associated speck-like protein containing a carboxy-terminal CARD inflammasome.19 We showed that p.E250K mutation increases PSTPIP1-pyrin interactions compared with p.E250Q. The pE250K-mutated PSTPIP1 protein shows comparable hyperphosphorylation with p.E250Q indicating that the increased PSTPIP1-pyrin binding is not just dependent on the phosphorylation status of the protein. These data are in accordance with earlier reports indicating a role of the coiled-coil domain of PSTPIP1 in addition to phosphorylation of tyrosine Y344 in the binding of pyrin.17 The fact that a single negative charge switch in PSTPIP1 causes major phenotypic changes with clinical significance is unique for this group of autoinflammatory diseases, and the analysis of the underlying molecular mechanism will be a challenging matter for future research. Because significantly increased MRP8/14 levels can be found in patients with FMF and those with PAPA syndrome and are extremely high in patients with Hz/Hc, it seems to be likely that the MRP secretion is regulated by the pyrin-PSTPIP1 axis. A link might be the involvement of tubulin in the pyrin-PSTPIP1 axis19,49 because MRPs are released in an alternative tubulin-dependent manner.4 Patients with cryopyrin-associated periodic syndromes with mutations in the NOD-like receptor family, pyrin domain, containing 3 gene have MRP8/14 levels within the range of systemic infections.50 Therefore highly increased serum levels of MRP8/14 are the first specific biomarker for diseases affecting NOD-like receptor family, pyrin domain containing 3-independent inflammasome activation.51,52
The efficacy of anti-TNF treatment and inconsistent efficacy of recombinant IL-1RA (anakinra) treatment of patients with PAPA syndrome have been reported.21 Reports about treatment of Hz/Hc are limited, with preliminary evidence for favorable treatment with cyclosporine15 and adalimumab.53 In our cohort of patients with HZ/Hc, IL-1 blockade was partially effective in 5 of 10 patients; cyclosporine or prednisolone showed reasonable responses as well. Anti-TNF treatment was only effective in 1 of 3 patients. Interestingly, improvement in cutaneous symptoms, arthritis, anemia, systemic inflammation, and hepatosplenomegaly was noted, whereas neutropenia was still present in all 3 patients. Therefore our data indicate the necessity for an individual tailored treatment regimen. Response to treatment was accompanied by a decrease in levels of serum proteins, including IL-18 and MRP8/14.
This study reports the largest cohort of patients with PSTPIP1 mutations. PSTPIP1-associated diseases show variable expressivity and are associated with a range of clinical phenotypes. To avoid confusion, we would like to suggest a novel nomenclature for this group of related diseases that is based on the causal genotypes, biochemical findings, and clinically distinct symptoms. In analogy to cryopyrin-associated periodic syndrome, we suggest the term PSTPIP1-associated inflammatory diseases (PAID) as a new class that encompasses PAPA syndrome (p.A230T, p.E250Q, and p.E256G), pyogenic arthritis, pyoderma gangrenosum, acne, and hidradenitis suppurativa syndrome (p.E277D)54 and patients with Hz/Hc (p.E250K and p.E257K). We would like to suggest the term PSTPIP1-associated myeloid-related proteinemia inflammatory syndrome (PAMI) for the latter entity. We further propose that patients with undefined autoinflammatory syndromes and significant skin inflammation (or pyoderma gangrenosum) should be tested for MRP8/14 serum levels to initiate targeted genetic testing.
In conclusion, an amino acid change in the y-domain of PSTPIP1 (E→K) causes a clinically and serologically distinct autoinflammatory disorder representing a novel and unique genotype-phenotype correlation. The PSTPIP1-associated myeloid-related proteinemia inflammatory syndrome (Hz/Hc) inflammatory phenotype is associated with a characteristic cytokine profile and characterized by extremely high levels of the proinflammatory alarmins MRP8 and MRP14.
Supplementary Material
Key messages.
The novel heterozygous missense mutations p.E250K and p.E257K in the PSTPIP1 gene are the cause for the autoinflammatory disorder Hz/Hc.
Patients with Hz/Hc can be separated from patients with PAPA syndrome based on a distinct clinical phenotype, cytokine profile, and first of all, extremely high MRP8/MRP14 expression and serum concentrations.
Acknowledgments
We thank Melanie Saers and Susanne Schleifenbaum for excellent technical assistance, Professor Jerzy-Roch Nofer for laboratory analysis, and Professor Anna Simon for providing clinical data.
Supported in part by the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Instituters of Health, Department of Health and Haman Services (to S.M.H.) and in part with federal funds from the National Cancer Institute, National Institutes of Health, under contract no. HHSN261200800001E. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government. Also supported by “Fondo de Investigaciones Sanitarias,” Ministerio de Economía y Competitividad (PI06/1031, PI10/01718), with the funding of European Regional Development Fund European Social Fund FEDER-FSE, the Interdisciplinary Centre for Clinical Research University of Münster, the German Research Foundation (SFB1009), and the Bundesministerium für Bildung und Forschung (AID-NET, project 01GM08100).
Abbreviations used
- AIN
Autoimmune neutropenia
- FMF
Familial Mediterranean fever
- Hz/Hc
Hyperzincemia and hypercalprotectinemia
- MIF
Macrophage migration inhibitory factor
- MRP
Myeloid-related protein
- PAPA
Pyogenic arthritis, pyoderma gangrenosum, and acne
- PSTPIP1
Proline-serine-threonine phosphatase-interacting protein 1
- SJIA
Systemic juvenile idiopathic arthritis
- TLR
Toll-like receptor
- WT
Wild-type
Footnotes
Disclosure of potential conflict of interest: M. Gattorno has received consultancy fees, research support, and lecture fees from Novartis and SOBI. C. Rodríguez-Gallego and C. Hinze have received lecture fees from Novartis. J. A. Bernstein has received consultancy fees from McKesson, research support from the National Institutes of Health (NIH) and CIRM, and lecture fees from the University of Minnesota. J. A. Church has received research support from Pfizer and BioProducts Laboratory. R. Skinner has provided expert testimony for the Medical Defence Union and the NHS Health Service and has received research support from Newcastle upon Tyne Hospitals NHS Foundation Trust, Malawi-Royal Victoria Infirmary, the Children’s Cancer Fund, and Children with Cancer UK. The rest of the authors declare that they have no relevant conflicts of interest.
References
- 1.Vogl T, Tenbrock K, Ludwig S, Leukert N, Ehrhardt C, van Zoelen MA, et al. Mrp8 and Mrp14 are endogenous activators of Toll-like receptor 4, promoting lethal, endotoxin-induced shock. Nat Med. 2007;13:1042–9. doi: 10.1038/nm1638. [DOI] [PubMed] [Google Scholar]
- 2.Sampson B, Fagerhol MK, Sunderkotter C, Golden BE, Richmond P, Klein N, et al. Hyperzincaemia and hypercalprotectinaemia: a new disorder of zinc metabolism. Lancet. 2002;360:1742–5. doi: 10.1016/S0140-6736(02)11683-7. [DOI] [PubMed] [Google Scholar]
- 3.Frosch M, Strey A, Vogl T, Wulffraat NM, Kuis W, Sunderkotter C, et al. Myeloid-related proteins 8 and 14 are specifically secreted during interaction of phagocytes and activated endothelium and are useful markers for monitoring disease activity in pauciarticular-onset juvenile rheumatoid arthritis. Arthritis Rheum. 2000;43:628–37. doi: 10.1002/1529-0131(200003)43:3<628::AID-ANR20>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 4.Rammes A, Roth J, Goebeler M, Klempt M, Hartmann M, Sorg C. Myeloid-related protein (MRP) 8 and MRP14, calcium-binding proteins of the S100 family, are secreted by activated monocytes via a novel, tubulin-dependent pathway. J Biol Chem. 1997;272:9496–502. doi: 10.1074/jbc.272.14.9496. [DOI] [PubMed] [Google Scholar]
- 5.Roth J, Vogl T, Sorg C, Sunderkotter C. Phagocyte-specific S100 proteins: a novel group of proinflammatory molecules. Trends Immunol. 2003;24:155–8. doi: 10.1016/s1471-4906(03)00062-0. [DOI] [PubMed] [Google Scholar]
- 6.Viemann D, Strey A, Janning A, Jurk K, Klimmek K, Vogl T, et al. Myeloid-related proteins 8 and 14 induce a specific inflammatory response in human microvascular endothelial cells. Blood. 2005;105:2955–62. doi: 10.1182/blood-2004-07-2520. [DOI] [PubMed] [Google Scholar]
- 7.Newton RA, Hogg N. The human S100 protein MRP-14 is a novel activator of the beta 2 integrin Mac-1 on neutrophils. J Immunol. 1998;160:1427–35. [PubMed] [Google Scholar]
- 8.Loser K, Vogl T, Voskort M, Lueken A, Kupas V, Nacken W, et al. The Toll-like receptor 4 ligands Mrp8 and Mrp14 are crucial in the development of autoreactive CD81 T cells. Nat Med. 2010;16:713–7. doi: 10.1038/nm.2150. [DOI] [PubMed] [Google Scholar]
- 9.van Lent PL, Grevers L, Blom AB, Sloetjes A, Mort JS, Vogl T, et al. Myeloid-related proteins S100A8/S100A9 regulate joint inflammation and cartilage destruction during antigen-induced arthritis. Ann Rheum Dis. 2008;67:1750–8. doi: 10.1136/ard.2007.077800. [DOI] [PubMed] [Google Scholar]
- 10.Vogl T, Ludwig S, Goebeler M, Strey A, Thorey IS, Reichelt R, et al. MRP8 and MRP14 control microtubule reorganization during transendothelial migration of phagocytes. Blood. 2004;104:4260–8. doi: 10.1182/blood-2004-02-0446. [DOI] [PubMed] [Google Scholar]
- 11.Frosch M, Ahlmann M, Vogl T, Wittkowski H, Wulffraat N, Foell D, et al. The myeloid-related proteins 8 and 14 complex, a novel ligand of toll-like receptor 4, and interleukin-1beta form a positive feedback mechanism in systemic-onset juvenile idiopathic arthritis. Arthritis Rheum. 2009;60:883–91. doi: 10.1002/art.24349. [DOI] [PubMed] [Google Scholar]
- 12.Wittkowski H, Kallinich T, Keitzer R, Roth J, Foell D. The endogenous TLR-4 ligands MRP8/14 as biomarkers of inflammation in Familial Mediterranean Fever (FMF) Pediatr Rheumatol Online J. 2008;6(Suppl1):P208. [Google Scholar]
- 13.Fessatou S, Fagerhol MK, Roth J, Stamoulakatou A, Kitra V, Hadarean M, et al. Severe anemia and neutropenia associated with hyperzincemia and hypercalprotectinemia. J Pediatr Hematol Oncol. 2005;27:477–80. doi: 10.1097/01.mph.0000179958.19524.9c. [DOI] [PubMed] [Google Scholar]
- 14.Isidor B, Poignant S, Corradini N, Fouassier M, Quartier P, Roth J, et al. Hyperzincemia and hypercalprotectinemia: unsuccessful treatment with tacrolimus. Acta Paediatr. 2009;98:410–2. doi: 10.1111/j.1651-2227.2008.01092.x. [DOI] [PubMed] [Google Scholar]
- 15.Sugiura T, Goto K, Ito K, Ban K, Okada S, Moriyama A, et al. Effects of cyclosporine A in hyperzincaemia and hypercalprotectinaemia. Acta Paediatr. 2006;95:857–60. doi: 10.1080/08035250500482255. [DOI] [PubMed] [Google Scholar]
- 16.Yang H, Reinherz EL. CD2BP1 modulates CD2-dependent T cell activation via linkage to protein tyrosine phosphatase (PTP)-PEST. J Immunol. 2006;176:5898–907. doi: 10.4049/jimmunol.176.10.5898. [DOI] [PubMed] [Google Scholar]
- 17.Shoham NG, Centola M, Mansfield E, Hull KM, Wood G, Wise CA, et al. Pyrin binds the PSTPIP1/CD2BP1 protein, defining familial Mediterranean fever and PAPA syndrome as disorders in the same pathway. Proc Natl Acad Sci U S A. 2003;100:13501–6. doi: 10.1073/pnas.2135380100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith EJ, Allantaz F, Bennett L, Zhang D, Gao X, Wood G, et al. Clinical, molecular, and genetic characteristics of PAPA syndrome: a review. Curr Genomics. 2010;11:519–27. doi: 10.2174/138920210793175921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Waite AL, Schaner P, Richards N, Balci-Peynircioglu B, Masters SL, Brydges SD, et al. Pyrin Modulates the Intracellular Distribution of PSTPIP1. PLoS One. 2009;4:e6147. doi: 10.1371/journal.pone.0006147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lindor NM, Arsenault TM, Solomon H, Seidman CE, McEvoy MT. A new autosomal dominant disorder of pyogenic sterile arthritis, pyoderma gangrenosum, and acne: PAPA syndrome. Mayo Clin Proc. 1997;72:611–5. doi: 10.1016/S0025-6196(11)63565-9. [DOI] [PubMed] [Google Scholar]
- 21.Demidowich AP, Freeman AF, Kuhns DB, Aksentijevich I, Gallin JI, Turner ML, et al. Genotype, phenotype, and clinical course in five patients with PAPA syndrome (pyogenic arthritis, pyoderma gangrenosum, and acne) Arthritis Rheum. 2012;64:2022–7. doi: 10.1002/art.34332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schellevis MA, Stoffels M, Hoppenreijs EP, Bodar E, Simon A, van der Meer JW. Variable expression and treatment of PAPA syndrome. Ann Rheum Dis. 2011;70:1168–70. doi: 10.1136/ard.2009.126185. [DOI] [PubMed] [Google Scholar]
- 23.Reil A, Sachs UJ, Siahanidou T, Flesch BK, Bux J. HNA-1d: a new human neutrophil antigen located on Fcgamma receptor IIIb associated with neonatal immune neutropenia. Transfusion. 2013;53:2145–51. doi: 10.1111/trf.12086. [DOI] [PubMed] [Google Scholar]
- 24.Henne WM, Kent HM, Ford MG, Hegde BG, Daumke O, Butler PJ, et al. Structure and analysis of FCHo2 F-BAR domain: a dimerizing and membrane recruitment module that effects membrane curvature. Structure. 2007;15:839–52. doi: 10.1016/j.str.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Sievers F, Wilm A, Dineen D, Gibson TJ, Karplus K, Li W, et al. Fast, scalable generation of high-quality protein multiple sequence alignments using Clustal Omega. Mol Syst Biol. 2011;7:539. doi: 10.1038/msb.2011.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sali A, Blundell TL. Comparative protein modelling by satisfaction of spatial restraints. J Mol Biol. 1993;234:779–815. doi: 10.1006/jmbi.1993.1626. [DOI] [PubMed] [Google Scholar]
- 27.Melo F, Feytmans E. Assessing protein structures with a non-local atomic interaction energy. J Mol Biol. 1998;277:1141–52. doi: 10.1006/jmbi.1998.1665. [DOI] [PubMed] [Google Scholar]
- 28.MacKerell AD, Bashford D, Bellott M, Dunbrack RL, Evanseck JD, Field MJ, et al. All-atom empirical potential for molecular modeling and dynamics studies of proteins. J Phys Chem B. 1998;102:3586–616. doi: 10.1021/jp973084f. [DOI] [PubMed] [Google Scholar]
- 29.Madura JD, Briggs JM, Wade RC, Davis ME, Luty BA, Ilin A, et al. Electrostatics and diffusion of molecules in solution: simulations with the University of Houston Brownian Dynamics program. Comput Phys Commun. 1995;91:57–95. [Google Scholar]
- 30.Guerois R, Nielsen JE, Serrano L. Predicting changes in the stability of proteins and protein complexes: a study of more than 1000 mutations. J Mol Biol. 2002;320:369–87. doi: 10.1016/S0022-2836(02)00442-4. [DOI] [PubMed] [Google Scholar]
- 31.Pettersen EF, Goddard TD, Huang CC, Couch GS, Greenblatt DM, Meng EC, et al. UCSF Chimera—a visualization system for exploratory research and analysis. J Comput Chem. 2004;25:1605–12. doi: 10.1002/jcc.20084. [DOI] [PubMed] [Google Scholar]
- 32.de Jager W, Prakken BJ, Bijlsma JW, Kuis W, Rijkers GT. Improved multiplex immunoassay performance in human plasma and synovial fluid following removal of interfering heterophilic antibodies. J Immunol Methods. 2005;300:124–35. doi: 10.1016/j.jim.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 33.Holzinger D, Frosch M, Kastrup A, Prince FH, Otten MH, Van Suijlekom-Smit LW, et al. The Toll-like receptor 4 agonist MRP8/14 protein complex is a sensitive indicator for disease activity and predicts relapses in systemic-onset juvenile idiopathic arthritis. Ann Rheum Dis. 2012;71:974–80. doi: 10.1136/annrheumdis-2011-200598. [DOI] [PubMed] [Google Scholar]
- 34.Cooper KM, Bennin DA, Huttenlocher A. The PCH family member proline-serine-threonine phosphatase-interacting protein 1 targets to the leukocyte uropod and regulates directed cell migration. Mol Biol Cell. 2008;19:3180–91. doi: 10.1091/mbc.E08-02-0225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cortesio CL, Wernimont SA, Kastner DL, Cooper KM, Huttenlocher A. Impaired podosome formation and invasive migration of macrophages from patients with a PSTPIP1 mutation and PAPA syndrome. Arthritis Rheum. 2010;62:2556–8. doi: 10.1002/art.27521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schroder K, Hertzog PJ, Ravasi T, Hume DA. Interferon-gamma: an overview of signals, mechanisms and functions. J Leukoc Biol. 2004;75:163–89. doi: 10.1189/jlb.0603252. [DOI] [PubMed] [Google Scholar]
- 37.Song X, Zhu S, Shi P, Liu Y, Shi Y, Levin SD, et al. IL-17RE is the functional receptor for IL-17C and mediates mucosal immunity to infection with intestinal pathogens. Nat Immunol. 2011;12:1151–8. doi: 10.1038/ni.2155. [DOI] [PubMed] [Google Scholar]
- 38.Zindl CL, Lai JF, Lee YK, Maynard CL, Harbour SN, Ouyang W, et al. IL-22 producing neutrophils contribute to antimicrobial defense and restitution of colonic epithelial integrity during colitis. Proc Natl Acad Sci U S A. 2013;110:12768–73. doi: 10.1073/pnas.1300318110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gaetke LM, McClain CJ, Talwalkar RT, Shedlofsky SI. Effects of endotoxin on zinc metabolism in human volunteers. Am J Physiol. 1997;272:E952–6. doi: 10.1152/ajpendo.1997.272.6.E952. [DOI] [PubMed] [Google Scholar]
- 40.Besecker BY, Exline MC, Hollyfield J, Phillips G, Disilvestro RA, Wewers MD, et al. A comparison of zinc metabolism, inflammation, and disease severity in critically ill infected and noninfected adults early after intensive care unit admission. Am J Clin Nutr. 2011;93:1356–64. doi: 10.3945/ajcn.110.008417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beck FW, Li Y, Bao B, Prasad AS, Sarkar FH. Evidence for reprogramming global gene expression during zinc deficiency in the HUT-78 cell line. Nutrition. 2006;22:1045–56. doi: 10.1016/j.nut.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 42.Prasad AS, Bao B, Beck FW, Sarkar FH. Correction of interleukin-2 gene expression by in vitro zinc addition to mononuclear cells from zinc-deficient human subjects: a specific test for zinc deficiency in humans. Transl Res. 2006;148:325–33. doi: 10.1016/j.trsl.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 43.Prasad AS, Beck FW, Grabowski SM, Kaplan J, Mathog RH. Zinc deficiency: changes in cytokine production and T-cell subpopulations in patients with head and neck cancer and in noncancer subjects. Proc Assoc Am Physicians. 1997;109:68–77. [PubMed] [Google Scholar]
- 44.Wieringa FT, Dijkhuizen MA, West CE, van der Ven-Jongekrijg J, van der Meer JW. Reduced production of immunoregulatory cytokines in vitamin A- and zinc-deficient Indonesian infants. Eur J Clin Nutr. 2004;58:1498–504. doi: 10.1038/sj.ejcn.1601998. [DOI] [PubMed] [Google Scholar]
- 45.Tsou TC, Chao HR, Yeh SC, Tsai FY, Lin HJ. Zinc induces chemokine and inflammatory cytokine release from human promonocytes. J Hazard Mater. 2011;196:335–41. doi: 10.1016/j.jhazmat.2011.09.035. [DOI] [PubMed] [Google Scholar]
- 46.Bao B, Prasad AS, Beck FW, Bao GW, Singh T, Ali S, et al. Intracellular free zinc up-regulates IFN-gamma and T-bet essential for Th1 differentiation in Con-A stimulated HUT-78 cells. Biochem Biophys Res Commun. 2011;407:703–7. doi: 10.1016/j.bbrc.2011.03.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hayashi K, Ishizuka S, Yokoyama C, Hatae T. Attenuation of interferon-gamma mRNA expression in activated Jurkat T cells by exogenous zinc via down-regulation of the calcium-independent PKC-AP-1 signaling pathway. Life Sci. 2008;83:6–11. doi: 10.1016/j.lfs.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 48.Yu JW, Fernandes-Alnemri T, Datta P, Wu J, Juliana C, Solorzano L, et al. Pyrin activates the ASC pyroptosome in response to engagement by autoinflammatory PSTPIP1 mutants. Mol Cell. 2007;28:214–27. doi: 10.1016/j.molcel.2007.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yu JW, Farias A, Hwang I, Fernandes-Alnemri T, Alnemri ES. Ribotoxic stress through p38 mitogen-activated protein kinase activates in vitro the human pyrin inflammasome. J Biol Chem. 2013;288:11378–83. doi: 10.1074/jbc.M112.448795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wittkowski H, Kuemmerle-Deschner JB, Austermann J, Holzinger D, Goldbach-Mansky R, Gramlich K, et al. MRP8 and MRP14, phagocyte-specific danger signals, are sensitive biomarkers of disease activity in cryopyrin-associated periodic syndromes. Ann Rheum Dis. 2011;70:2075–81. doi: 10.1136/ard.2011.152496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chae JJ, Cho YH, Lee GS, Cheng J, Liu PP, Feigenbaum L, et al. Gain-of-function Pyrin mutations induce NLRP3 protein-independent interleukin-1beta activation and severe autoinflammation in mice. Immunity. 2011;34:755–68. doi: 10.1016/j.immuni.2011.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hesker PR, Nguyen M, Kovarova M, Ting JP, Koller BH. Genetic loss of murine pyrin, the familial Mediterranean fever protein, increases interleukin-1beta levels. PLoS One. 2012;7:e51105. doi: 10.1371/journal.pone.0051105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee H, Park SH, Kim SK, Choe JY, Park JS. Pyogenic arthritis, pyoderma gangrenosum, and acne syndrome (PAPA syndrome) with E250K mutation in CD2BP1 gene treated with the tumor necrosis factor inhibitor adalimumab. Clin Exp Rheumatol. 2012;30:452. [PubMed] [Google Scholar]
- 54.Marzano AV, Trevisan V, Gattorno M, Ceccherini I, De Simone C, Crosti C. Pyogenic arthritis, pyoderma gangrenosum, acne, and hidradenitis suppurativa (PAPASH): a new autoinflammatory syndrome associated with a novel mutation of the PSTPIP1 gene. JAMA Dermatol. 2013;149:762–4. doi: 10.1001/jamadermatol.2013.2907. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.