Summary
There is currently scarce knowledge of the immunological profile of patients with latent autoimmune diabetes mellitus in the adult (LADA) when compared with healthy controls (HC) and patients with classical type 1 diabetes (T1D) and type 2 diabetes (T2D). The objective of this study was to investigate the cellular immunological profile of LADA patients and compare to HC and patients with T1D and T2D. All patients and age‐matched HC were recruited from Uppsala County. Peripheral blood mononuclear cells were isolated from freshly collected blood to determine the proportions of immune cells by flow cytometry. Plasma concentrations of the cytokine interleukin (IL)‐35 were measured by enzyme‐linked immunosorbent assay (ELISA). The proportion of CD11c+CD123– antigen‐presenting cells (APCs) was lower, while the proportions of CD11c+CD123+ APCs and IL‐35+ tolerogenic APCs were higher in LADA patients than in T1D patients. The proportion of CD3–CD56highCD16+ natural killer (NK) cells was higher in LADA patients than in both HC and T2D patients. The frequency of IL‐35+ regulatory T cells and plasma IL‐35 concentrations in LADA patients were similar to those in T1D and T2D patients, but lower than in HC. The proportion of regulatory B cells in LADA patients was higher than in healthy controls, T1D and T2D patients, and the frequency of IL‐35+ regulatory B cells was higher than in T1D patients. LADA presents a mixed cellular immunological pattern with features overlapping with both T1D and T2D.
Keywords: Cellular immunology, IL‐35, LADA, type 1 diabetes, type 2 diabetes
Introduction
Latent autoimmune diabetes mellitus in the adult (LADA) 1 accounts for 9% of all adult onset diabetes 1. Phenotypically, LADA patients share characteristics of both type 1 diabetes (T1D) (antibodies against the insulin‐producing β cells) and type 2 diabetes (T2D) patients (aged >35 years and non‐insulin‐dependent at onset) 2, 3. LADA also shares genetic features of both T1D and T2D 4. Despite the presence of autoantibodies, predominantly against glutamic acid decarboxylase (GAD), the disease progress is much slower than in T1D. At present, the focus on the immunological characterization of LADA has concerned the presence of autoantibodies, with only a few studies of other components of the immune system, such as low‐grade proinflammatory markers or cellular immunology 4, 5, 6. So far there are no published reports describing the cellular immunological profile that characterizes LADA patients in comparison to healthy individuals, T1D as well as T2D patients, simultaneously.
Innate immune cells, such as dendritic cells (DCs), are the main players during early development of autoimmune diabetes 7, 8, 9, 10. Allen et al. have reported that plasmacytoid dendritic cells (pDCs) are expanded during the early development of T1D and enhance the islet autoantigen presentation to T cells through an immune complex capture 11. In line with this, it has been shown that interferon (IFN)‐α‐producing pDCs augment the T helper type 1 (Th1) response in T1D and the number of IFN‐α‐producing pDCs are increased in T1D patients compared to healthy controls 12. Therefore, it is of interest to investigate CD11c+CD123–human leucocyte antigen (HLA)‐DR+Lin– (CD11c+CD123–) antigen‐presenting cells (APCs), CD11c+CD123+HLA‐DR+Lin– (CD11c+CD123+) APCs and CD11c–CD123+HLA‐DR+Lin– (CD11c–CD123+) pDCs in LADA patients. Herein, these subsets of DCs were analysed using flow cytometry, as described previously 13. Neutrophils have been found to be reduced in recent‐onset T1D 14, 15, and CD15low neutrophils (low‐density granular neutrophils) have also been shown to have a pathogenic role in systemic autoimmunity 16. In accordance with this, Neuwrith et al. have reported a role of CD15low cells in T1D development 17. Alterations in the frequency of CD16 monocytes has been associated with diabetes complications 18.
Natural killer (NK) cells participate in innate immune responses and in animal models of T1D, it has been reported that depletion of NK cells prevents the development of T1D 19, 20. An altered frequency of total number of NK cells has been found in LADA, but not in T2D, patients 21, 22. Furthermore, it has been reported in children with T1D that NK cells have defects in signalling and function that might contribute to the pathogenesis of T1D 23. NK cell subsets could be defined based on the relative expression of CD16 and CD56, i.e. CD56dim (CD56lowCD16+ and CD56lowCD16–) and CD56bright (CD56highCD16+ and CD56highCD16–), as reviewed by Poli et al. 24. CD56dim NK cells are considered to be mature NK cells and CD56bright cells are immature cells. CD56dim NK cells have cytotoxic properties while CD56bright NK cells are proinflammatory, as they produce IFN‐γ 25. In the present study we determined the proportion of both CD56dim and CD56bright NK cell subpopulations using flow cytometry.
Adaptive immune cells such as T (CD4+ and CD8+) and B (CD19+) cells also play a major role in autoimmunity and metabolic disorders 26, 27, 28, 29, 30. An altered phenotype of CD4+, CD8+ and CD19+ cells has been reported in LADA patients 5, 31, 32, 33. Therefore, in this study we determined the proportions of these cells in LADA patients when compared to T1D and T2D patients. Immune cells that produce anti‐inflammatory cytokines, e.g. interleukin (IL)‐10, transforming growth factor (TGF)‐β and IL‐35, are known as regulatory immune cells, i.e. regulatory T (Treg) cells, regulatory B (Breg) cells and tolerogenic APCs 34, 35, 36. Treg cells have received a great deal of attention, as these cells play a major role in maintaining the homeostasis of the immune system and preventing the development of autoimmune diseases 37, 38. A reduced number of Treg cells has been reported in different autoimmune diseases, including T1D 39. Treg cells can be identified by using the cell surface markers CD4, CD25 and CD127 and the intracellular forkhead box (Fox) transcription factor FoxP3 40. Breg cells can be identified by using the cell surface markers CD19, CD24, CD38 and CD40 41. Treg cells, Breg cells and APCs produce IL‐35 34, 35, 36, 42, 43, 44. This cytokine is a novel anti‐inflammatory cytokine, which belongs to the IL‐12 cytokine family, and has two subunits, Ebi3 and IL‐12p35 42, 43. It has previously been reported that IL‐35 suppresses autoimmunity and plays a putative role in tumour biology 35, 36, 42, 45, 46, 47. We have found that the systemic administration of IL‐35 prevented the development of autoimmune diabetes in the multiple low‐dose streptozotocin (MLDSTZ) mouse model, and effectively reversed established disease in both the MLDSTZ and non‐obese diabetic mouse models of T1D by maintaining the normal suppressive phenotype of Treg cells 46. We also found that IL‐35 levels were higher in T1D patients with residual C‐peptide compared to T1D patients with no measurable residual C‐peptide 48. Thus, our previous findings indicate that IL‐35 may prevent the loss of β cell mass. The possible alteration in the frequencies of IL‐35‐producing cells in LADA patients has not yet been investigated.
In this study we aimed to determine the proportions of different innate, adaptive and regulatory immune cells in order to elucidate the immunological profile that characterizes LADA in comparison to healthy controls, T1D and T2D patients.
Materials and methods
Informed consent
The Uppsala County regional ethics board approved this study, and the reported investigations were carried out in accordance with the principles of the Declaration of Helsinki, as revised in 2000. All participants were provided with oral and written information about the study, and signed a written consent.
Inclusion
The All New Diabetes in Uppsala (ANDiU) study (www.andiu.se) is an ongoing study with the aim of describing the incidence of diabetes subgroups in Uppsala County, Sweden (population approximately 300 000). Patients newly diagnosed with diabetes (ADA criteria) are included. Upon registration patients are classified into diabetes subtypes according to criteria shared with the All New Diabetics in Scania (ANDIS) study (http://andis.ludc.med.lu.se; Principle Investigator: Leif Groop) in southern Sweden. Criteria for LADA diagnosis are age ≥35 years, GAD antibody (GADA) positivity (>20 IE/ml) and fasting (f)C‐peptide levels ≥0·3 nmol/l. T1D criteria are GADA positivity and fC‐peptide <0·3 nmol/l, whereas for T2D age ≥35 years, GADA negativity and fC‐peptide >0·72 nmol/l are used as diagnostic criteria. For all three diagnoses there should be no history of pancreatitis, pancreatic cancer or other causes of secondary diabetes. There are no unified criteria for LADA diagnosis and classification, but the criteria used in ANDiU and ANDIS are in line with previous literature 3. The exception is fC‐peptide, which is used in ANDiU and ANDIS as an indicator of remaining insulin production to separate LADA from T1D 49, 50. It replaces the insulin therapy criterion (i.e. no insulin therapy within 6–12 months of diagnosis) that is often used, which is open to subjectivity as it reflects the assessment made by the treating physician. From ANDiU we recruited patients classified as LADA and T2D. T1D patients and healthy controls were recruited at Uppsala University Hospital and Eriksberg Primary Health Care Clinic, Uppsala, respectively. T1D and T2D patients, as well as healthy controls, were age‐, sex‐ and body mass index (BMI)‐matched to the LADA patients. Exclusion criteria were ongoing hormonal treatment (ATC code H01‐03), use of non‐steroid anti‐inflammatory drugs (NSAID, ATC code M01), ongoing chemotherapy treatment (ATC code L01‐04) and other autoimmune disease (e.g. hypo/hyperthyroidism, rheumatic disease, vitiligo, psoriasis, coeliac disease, Addison’s disease and inflammatory bowel disease). Table 1 provides characteristics of the included patients and Supporting information, Fig. S1 shows a flow‐chart of the inclusion process of the study.
Table 1.
Characteristics of the research subjects; patients were matched for age, sex and BMI
| Controls (n = 13) | T1D (n = 16) | LADA (n = 14) | T2D (n = 16) | |
|---|---|---|---|---|
| Age (years) | 61·6 ± 2·9 | 66·0 ± 1·4 | 65·7 ± 2·4 | 64·0 ± 2·0 |
| Sex (M%/F%) | 62%/38% | 73%/27% | 57%/43% | 70%/30% |
| BMI (kg/m2) | 28·9 ± 4·0 | 26·5 ± 0·7 | 27·9 ± 0·5 | 29·1 ± 1·0 |
| Age at onset | n.a. | 19·7 ± 1·8 | 63·6 ± 1·5b | 60·0 ± 2·0b |
| Disease duration | n.a. | 46·1 ± 2·2 | 4·9 ± 0·3b | 5·3 ± 0·3a, b |
| HbA1c (mmol/mol) | 35·8 ± 0·7 | 58·9 ± 3·2a | 45·8 ± 2·3b | 52·27 ± 4·0a |
| fC‐peptide (nmol/l) | 1·10 ± 0·11 | 0·22 ± 0·13a | 0·95 ± 0·14b | 1·30 ± 0·12b, c |
| fp‐glucose (mmol/l) | 5·9 ± 0·1 | 11·7 ± 1·0a | 8·0 ± 0·5b | 9·1 ± 0·6a, b |
| GAD antibody IgG (IE/ml) | 0 ± 0 | 508 ± 205 | 337 ± 190 | 1 ± 0 |
| IA‐2 antibody IgG (IE/ml) | 1 ± 0 | 25 ± 7 | 387 ± 295 | 1 ± 0 |
| Hb (g/l) | 145 ± 2 | 142 ± 3 | 145 ± 3 | 141 ± 4 |
| Lkc (109/l) | 6·0 ± 0·4 | 5·8 ± 0·4 | 6·6 ± 0·8 | 5·4 ± 0·2 |
| CRP (mg/l) | 1·2 ± 0·4 | 1·6 ± 0·3 | 1·3 ± 0·2 | 2·4 ± 0·8 |
All values are given as mean ± standard error of the mean (s.e.m.). Multiple comparison of means by analysis of variance (anova), Tukey’s post‐hoc test.
P‐value versus controls < 0·05;
P‐value versus T1D < 0·05;
P‐value versus LADA < 0·05.
GADA = glutamate decarboxylase 65 antibody; eGFR = creatinine estimated glomerular filtration rate; TSH = thyroid‐stimulating hormone; LADA = latent autoimmune diabetes mellitus in the adult (LADA); Ig = immunoglobulin; BMI = body mass index; n.a. = not available; HbAlc = haemoglobinA1c; CRP = C‐reactive peptide; fC‐peptide = fasting C‐peptide; fp‐glucose = fasting plasma glucose; Lkc = leucocyte count.
Routine laboratory parameters
Blood samples were collected after overnight fasting. All routine laboratory parameters were analysed at the Central Clinical Chemistry Laboratory at Uppsala University Hospital, which is certified by the External Quality Assessment Service (EQUALIS) (equalis.se/en). On inclusion, blood haemoglobin 51, blood leucocyte count (Lkc), plasma C‐reactive protein (CRP), serum transglutaminase [immunoglobulin (Ig)A] antibodies, serum thyroxine (T4), serum triiodothyronine (T3), serum thyroid‐stimulating hormone (TSH), serum TSH‐receptor 18 antibody, serum thyroid peroxidase antibody, plasma IgA antibody, serum cortisol, 21‐hydroxylase 18 antibody, serum GADA, fasting serum C‐peptide, fasting plasma glucose and blood haemoglobinA1c (HbA1c) were analysed. Glomerular filtration rate (GFR) was estimated based on creatinine‐levels calculated with the MDRD formula 52.
Flow cytometry
Freshly isolated peripheral blood mononuclear cells (PBMCs) were prepared using Histopaque‐1077 (Sigma, St Louis, MO, USA), as described earlier 48. PBMCs were stained with antibodies for surface markers (Supporting information, Table S1). The cells were thereafter fixed and permeabilized with fixation permeabilization buffer (eBioscience, San Diego, CA, USA) for intracellular markers (Supporting information, Table S1). The samples were run on LSR II Fortesa (Becton Dickinson, Franklin Lakes, NJ, USA) using DivaDacker software 53 and 1 million events were counted for analysis. Fluorescence minus one (FMO), isotype and single‐stained controls were used for gating strategies. The flow cytometry standard (FCS) files were analysed on FlowLogic software (Inivai Technologies, Mentone, Australia). Representative gating strategies are shown in Supporting information, Fig. S2–S5.
IL‐35 measurements in plasma
Plasma IL‐35 concentrations were determined by using an enzyme‐linked immunosorbent assay (ELISA) kit (Cloud‐Clone Corporation, Wuhan, China).
Statistics
Differences in means between healthy controls, T1D and T2D patients compared to LADA patients were calculated by one‐way analysis of variance (anova) with Dunnett’s post‐hoc test for immunological profiles. Comparisons between all groups were performed by anova with Tukey’s post‐hoc test for research subjects’ characteristics (Table 1). A P‐value < 0·05 was considered as a significant difference between groups. Statistical analyses were carried out in GraphPad Prism version 6.0TM.
Results
Innate immune cell responses
We observed a lower proportion of CD11c+CD123– APCs in LADA patients than in healthy controls and T1D patients (Fig. 1a). Furthermore, the proportion of CD11c+CD123– APCs among HLA‐DR+Lin– cells was lower in LADA patients than in T1D patients (Fig. 1b), whereas the proportions of pDCs and pDCs among HLA‐DR+Lin– were not altered in LADA patients (Fig. 1c,d). We did not observe any difference in the proportion of CD11c+CD123+ APCs (Fig. 1e), but the proportion of CD11c+CD123+ cells among HLA‐DR+Lin– was higher in patients with LADA than in patients with T1D (Fig. 1f).
Figure 1.
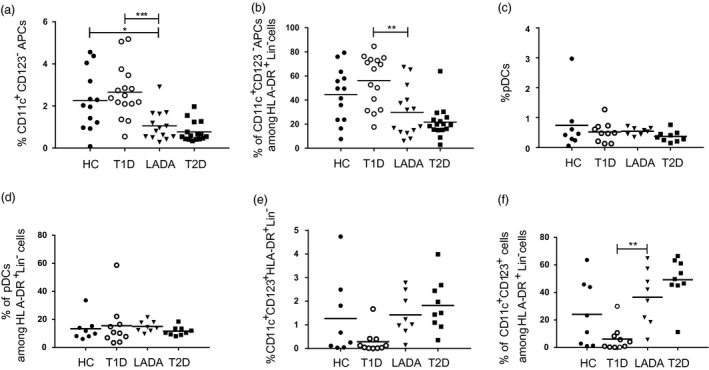
The proportions of CD11c+CD123– antigen‐presenting cells (APCs) are decreased while CD11c+CD123+ APCs are increased in latent autoimmune diabetes mellitus in the adult (LADA) compared to type 1 diabetes patients. Proportions of (a) CD11c+CD123–human leucocyte antigen (HLA)‐DR+Lin– APCs in total live cells, (b) CD11c+CD123– APCs among HLA‐DR+Lin– cells, which were gated on HLA‐DR+Lin– cells, (c) CD11c–CD123+HLA‐DR+Lin– plasmacytoid dendritic cells (pDCs) in total live cells, (d) CD11c–CD123+ pDCs among HLA‐DR+Lin– cells, which were gated on HLA‐DR+Lin– cells, (e) CD11c+CD123+HLA‐DR+Lin– APCs in total live cells and (f) CD11c+CD123+ APCs among HLA‐DR+Lin– cells, which were gated on HLA‐DR+Lin– cells. The proportions of these cells were determined by using a flow cytometer. HC = healthy controls. One‐way analysis of variance (anova) with Dunnett’s post‐hoc test comparison to patients with LADA was used, n = 13–16/group. *P < 0·05; **P < 0·01.
We did not find any alteration in the proportions of CD15low neutrophils and CD16+ monocytes in LADA patients (Supporting information, Fig. S6a,b). We also examined different subsets of NK cells and did not find any alteration in LADA patients compared to the other groups regarding the proportions of CD3–CD56lowCD16+, CD3–CD56lowCD16– and CD3–CD56highCD16– NK cells (Fig. 2a–c). However, the proportion of CD3–CD56highCD16+ NK cells was higher in LADA patients compared to both healthy controls and T2D patients (Fig. 2d). We did not observe any alteration in the proportions of CD3+CD56+ NK T cells between the groups (Supporting information, Fig. S6c).
Figure 2.
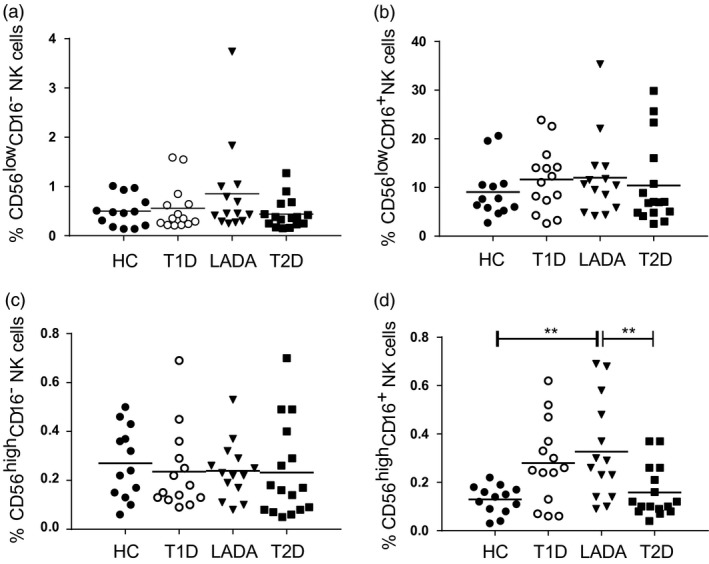
The proportion of CD3–CD56highCD16+ natural killer (NK) cells was increased in latent autoimmune diabetes mellitus in the adult (LADA) patients. The proportions of (a) CD3–CD56lowCD16– NK cells in total live cells, (b) CD3–CD56lowCD16+ NK cells in total live cells, (c) CD3–CD56highCD16– NK cells in total live cells and (d) CD3–CD56highCD16+ NK cells in total live cells were determined using a flow cytometer. HC = healthy controls. One‐way analysis of variance (anova) with Dunnett’s post‐hoc test comparison to patients with LADA was used, n = 13–16/group; **P < 0·01.
Adaptive immune cell responses
The proportions of CD3+, CD4+CD25– and CD8+ T cells were not altered in LADA patients when compared to the other groups (Supporting information, Fig. S7a–c). Similarly, the proportion of CD19+ cells was not altered (Supporting information, Fig. S7d).
Regulatory immune cell responses
The proportions of CD4+CD25+CD127–FoxP3+ cells (Treg cells) and CD4+CD25+CD127–FoxP3+Helios+thymic‐derived T cells (tTreg) were similar in all four groups (Supporting information, Fig. S8a,b). Similarly, the proportions of Treg cells as well as the tTreg cells among CD4+ T cells were similar in all four groups (Supporting information, Fig. S8c,d). However, the proportions of IL‐35+ cells among Treg and tTreg cells in patients with LADA were similar in patients with T1D and T2D, but lower when compared to healthy controls (Fig. 3a,b).
Figure 3.
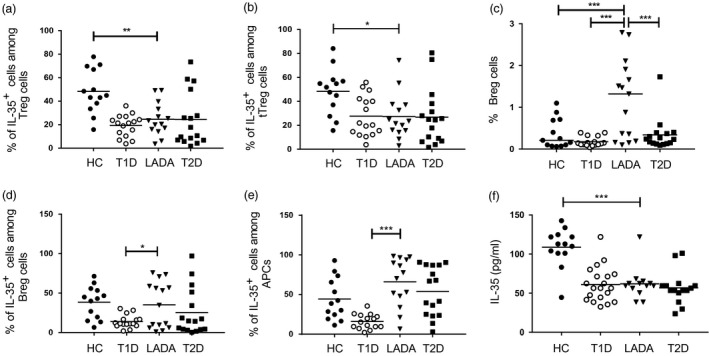
The proportion of interleukin (IL)‐35+ regulatory T cells (Treg) is decreased, but proportions of regulatory B cells (Breg) and IL‐35‐producing Breg cells and tolerogenic antigen‐presenting cells (APCs) are increased in latent autoimmune diabetes mellitus in the adult (LADA) patients. Proportions of (a) IL‐35+ cells among CD4+CD25+CD127–forkhead box protein 3 (FoxP3)+ Treg cells, (b) IL‐35+ cells among CD4+CD25+CD127–FoxP3+Helios+ thymic‐derived Tregs (tTregs), (c) CD19+CD24+CD38+CD40+ Breg cells in total live cells, (d) IL‐35+ cells among CD19+CD24+CD40+CD38+ Breg cells and (e) IL‐35+ cells among CD11c+CD123–human leucocyte antigen (HLA)‐DR+Lin– APCs. The proportions of these cells were determined using a flow cytometer. (f) IL‐35 plasma concentrations were measured by enzyme‐linked immunosorbent assay (ELISA). HC = healthy controls. One‐way analysis of variance (anova) with Dunnett’s post‐hoc test comparison to patients with LADA was used, n = 13–16/group. *P < 0·05; **P < 0·01; ***P < 0·001.
We also analysed the proportion of CD19+CD24+CD40+CD38+ cells (Breg cells), and observed a higher proportion of these cells in LADA patients when compared to healthy controls and patients with T1D and T2D (Fig. 3c). The proportion of IL‐35+ cells among Breg cells was higher in LADA patients when compared to T1D patients (Fig. 3d). Subsequently, we analysed the proportion of IL‐35+ tolerogenic APCs. Interestingly, the proportion of IL‐35+ cells among APCs was higher in patients with LADA compared to patients with T1D (Fig. 3e). Patients with LADA had IL‐35 concentrations in blood plasma that were similar to those in patients with T1D and T2D, but lower compared to those in healthy controls (Fig. 3f).
Discussion
We determined the proportions of different immune cells to elucidate the immunological patterns that distinguish patients with LADA compared not only to healthy individuals, but also to patients with T1D and T2D. With regard to the innate and adaptive immune cells, we found that LADA shares common features with both T1D and T2D. The proportion of CD11c+CD123– APCs in LADA patients was between that observed in T1D and T2D patients. Similarly, the proportion of CD11c+CD123+ cells among the HLA‐DR+Lin– was highest in T2D patients and lowest in T1D patients, whereas the proportion in LADA patients was between that of T1D and T2D patients.
Neutrophils have previously been claimed to play a role in the early development of both T1D 14, 15, 54 and T2D 55. In the present study, we did not find any alteration in the proportion of CD15low neutrophils in LADA patients when compared to the other study groups. It cannot be excluded that early transient alterations during disease development as described for T1D 14, 15 had occurred, as our study subjects with LADA had a mean disease duration of almost 5 years.
It has been reported previously that the proportion of CD3–CD56+CD16+ NK cells is decreased in LADA patients 22. Instead, we observed an increased proportion of CD3–CD56highCD16+ NK cells in LADA patients compared to both healthy controls and T2D patients. The reason for the discrepancy between the studies is unknown, but it could be because we used freshly prepared PBMCs instead of cryopreserved cell preparations. CD56high or CD56bright NK cells produce IFN‐γ 25. The proportions of these NK cells were similar in LADA and T1D patients. This result illustrates that, like T1D, LADA is also a Th1 response disorder.
The frequency of FoxP3+ Treg cells was similar in all groups. However, the proportion of IL‐35+ cells among Treg cells in patients with LADA was similar to those in patients with T1D and T2D, but lower when compared to healthy controls. This may suggest a common functional defect of Treg cells in LADA, T1D and T2D patients. This idea was further supported because the circulating concentrations of IL‐35 in patients with LADA were similar to patients with T1D and T2D, but lower than in than healthy controls. We have previously shown that decreased IL‐35 production by Treg cells is associated with a functional defect 46. Also, previous findings of a decreased frequency of FoxP3+ cells among CD4+CD25intermediate cells in LADA patients when compared to healthy controls 5, and a decreased Foxp3 gene expression in CD4+ T cells in LADA patients, are considered with defective Treg cell functionality 56. In patients with T1D, it has been reported that Treg cells lose their FoxP3 expression due to DNA methylation in the Foxp3 gene, which may cause a defective function in Treg cells and result in a decreased number of Treg cells 57. Interestingly, Li et al. also reported an abnormal DNA methylation in peripheral CD4+ T cells of LADA patients 33, which indicates a dysfunction of Treg cells 58.
Breg cells play an important role in maintaining the autoimmune and/or inflammatory response 35, 36. We found that the frequency of Breg cells was higher in LADA patients compared to all other groups. These results are in agreement with a previous report, where Deng et al. found the lowest frequency of IL‐10‐producing B cells in T1D patients when compared to LADA and T2D patients 32. Our observed lower proportion of IL‐35+ cells among Breg cells in T1D than LADA patients suggests that the response of IL‐35+ Breg cells in LADA patients is similar to that of T2D patients, which might protect against β cell destruction by immunological insults in LADA patients. Although the proportions of IL‐35+ Breg cells and IL‐35+ tolerogenic APCs were higher in LADA than in T1D patients, the circulating concentrations of IL‐35 were similar in LADA and T1D patients. This could be due to other IL‐35‐producing immune cells, such as iTr35 59 and macrophages 60. These particular populations have not been investigated in the present study.
APCs (CD123– APCs) and pDCs (CD123+ APCs) prime T cells to react against the insulin‐producing β cells. In the present study, we found that the numbers of APCs were lower in LADA than in T1D patients. This indicates that the initial immune response is lower in LADA patients, which might cause a delay in the development of an autoimmune response. Tolerogenic APCs protect β cells in animal models of T1D 44, and Dixon et al. reported that tolerogenic APCs produce IL‐35 in human peripheral blood 34. We analysed the frequency of IL‐35+ cells among APCs in our study and found that IL‐35+ cells were more frequent in LADA than in T1D patients, which may contribute to a milder disease development. In a previous study, we found that systemic treatment with IL‐35 in two different animal models of T1D prevented destruction of β cells 46. However, as this is an association study it is impossible to determine whether or not the immunological differences are causal.
We observed changes in the proportions of different immune cells in LADA patients compared to healthy controls and other diabetes patients. Our conclusion is that the changes in APC and Breg cell numbers in LADA patients are more similar to those also observed in T2D patients, whereas the changes in NK cell numbers are more similar to those found in T1D patients. There are no differences in IL‐35 concentrations and IL‐35+ Treg cell numbers in between LADA, T1D and T2D patients, but in all three conditions these are lower than the healthy individuals. Thus, our analysis of several subsets of immune cells reveals that LADA patients present a mixture of cellular immunological changes with features overlapping with both T1D and T2D.
Disclosures
The authors declare that there are no conflicts of interest associated with this paper.
Author contributions
M. M. and K. S. contributed to the design of the study, conducted experiments, acquired and analysed data, and participated in writing the manuscript. Z. L., D. E., J. S. and S. S. contributed to the design of the study, analysed data and participated in the writing of the manuscript. P. O. C. designed the study, analysed data and wrote the manuscript. All authors read and approved the final version. K. S. is the guarantor of this work and, as such, had access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Supporting information
Fig. S1. Flow‐chart of the inclusion process of study. Of the 17 registered LADA patients of the All New Diabetes in Uppsala (ANDiU) study, 13 were included. Additional patients with type 1 diabetes (T1D, n = 7), and type 2 (T2D, n = 13) diabetes) were recruited from ANDiU. Another 11 participants with T1D were included from the department of Endocrinology, Uppsala University hospital, Uppsala (UAS). Healthy controls (HC, n = 13) were recruited upon arrival (with no infection or systemic inflammation) at the Eriksberg Primary Healthcare Centre (EVC). Study subjects were matched for sex, age and body mass index (BMI).
Fig. S2. The representative gating strategies for tolerogenic APCs. The live cells were gated based on forward scatter (FSC) and side scatter (SSC). Cells were further gated for HLA‐DR and Lin mix expression. HLA‐DR+Lin‐ cells were thereafter gated for the expression of CD11c, CD123 or CD11c and CD123. CD11c+CD123‐HLA‐DR+Lin‐ cells were gated for IL‐12p35 and Ebi3 expression and gate was drawn by using FMO together with isotype controls to analyze IL‐35+ cells.
Fig. S3. The representative gating strategies for NK cells. The live cells were gated based on forward scatter (FSC) and side scatter (SSC). Cells were then gated for CD3 and CD56 expression. CD56high and CD56low cells were thereafter gated for CD16 expression.
Fig. S4. The representative gating strategies for Breg cells. The live cells were gated based on forward scatter (FSC) and side scatter (SSC). They were then gated for CD19 expression. CD19+ cells were gated for the expression of CD24 and CD40. CD19+CD24+CD40+ cells were gated for CD38 expression, CD19+CD24+CD40+CD38+ cells were thereafter gated for IL‐12p35 and Ebi3 expression. FMO together with isotype controls were used for negative control to determine IL‐ 12p35+Ebi3+ (IL‐35+) cells.
Fig. S5. Representative gating strategies for Treg cells. The live cells were gated based on side scatter (SSC) and forward scatter (FSC). The cells were then gated for the expression of CD4 and CD25. CD4+CD25+ cells were further gated for the expression of CD127. CD4+CD25+CD127‐ cells were gated for Foxp3 expression. CD4+CD25+CD127‐ Foxp3+ cells were gated for the expression of IL‐12p35 and Ebi3. IL‐12p35 and Ebi3 gates were made based on fluorescence minus one control together with isotype controls (this control was used as a negative control).
Fig. S6. The proportions of neutrophils, monocytes and NKT cells. The proportions of (a) CD15+ neutrophils in total live cells, (b) CD16+ monocytes in total live cells and (c) CD3+CD56+ NKT cells in total live cells, were determined by using a flow cytometer. HC denotes healthy controls. One‐way ANOVA with Dunnett’s post‐hoc test comparison to patients with LADA was used, n = 13‐16/group.
Fig. S7. The proportions of T‐cells and B‐lymphocytes. The proportions of (a) CD3+CD56‐ T‐cells in total live cells, (b) CD4+CD25‐ T‐cells in total live cells, (c) CD8+ T‐cells in total live cells, (d) CD19+ B‐lymphocytes in total live cells, were determined by using a flow cytometer. HC denotes healthy controls. One‐way ANOVA with Dunnett’s post‐hoc test comparison to patients with LADA was used, n = 13‐16/group.
Fig. S8. The proportions of Treg and tTreg cells among CD4+ T cells. The proportion of (a) CD4+CD25+CD127‐Foxp3+ Treg cells in total live cells, (b) CD4+CD25+CD127‐Foxp3+Helios+ tTreg cells in total live cells, (c) The proportions of CD4+CD25+CD127‐Foxp3+ Treg cells among CD4+ T‐cells and (d) CD4+CD25+CD127‐Foxp3+Helios+ tTregs among CD4+ T‐cells. The proportions of these cells were determined by using a flow cytometer. HC denotes healthy controls. One‐way ANOVA with Dunnett’s post‐hoc test was used for comparisons, n = 13‐16/group.
Table S1. Antibodies for surface and intracellular antigens used in flow cytometry staining.
Acknowledgements
The technical assistance from research nurses Violeta Armijo Del Valle, Rebecka Hilmius and Karin Kjellström is gratefully acknowledged. The present study was supported financially by the Swedish Research Council (2017‐01343, 921‐2014‐7054), EXODIAB, the Swedish Diabetes Foundation, Diabetes Wellness Sverige, the Swedish Child Diabetes Fund, SEB Diabetesfonden, O.E. och Edla Johanssons vetenskapliga stiftelse and the Novo Nordisk Foundation.
References
- 1. Hawa MI, Kolb H, Schloot N et al Adult‐onset autoimmune diabetes in Europe is prevalent with a broad clinical phenotype: action LADA 7. Diabetes Care 2013; 36:908–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tuomi T, Groop LC, Zimmet PZ, Rowley MJ, Knowles W, Mackay IR. Antibodies to glutamic acid decarboxylase reveal latent autoimmune diabetes mellitus in adults with a non‐insulin‐dependent onset of disease. Diabetes 1993; 42:359–62. [DOI] [PubMed] [Google Scholar]
- 3. Tuomi T, Santoro N, Caprio S, Cai M, Weng J, Groop L. The many faces of diabetes: a disease with increasing heterogeneity. Lancet 2014; 383:1084–94. [DOI] [PubMed] [Google Scholar]
- 4. Laugesen E, Ostergaard JA, Leslie RD, Danish Diabetes Academy Workshop and Workshop speakers . Latent autoimmune diabetes of the adult: current knowledge and uncertainty. Diabet Med 2015; 32:843–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Radenkovic M, Silver C, Arvastsson J et al Altered regulatory T cell phenotype in latent autoimmune diabetes of the adults (LADA). Clin Exp Immunol 2016; 186:46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Castelblanco E, Hernandez M, Castelblanco A et al Low‐grade inflammatory marker profile may help to differentiate patients with LADA, classic adult‐onset type 1 diabetes, and type 2 diabetes. Diabetes Care 2018; 41:862–8. [DOI] [PubMed] [Google Scholar]
- 7. Price JD, Beauchamp NM, Rahir G et al CD8+ dendritic cell‐mediated tolerance of autoreactive CD4+ T cells is deficient in NOD mice and can be corrected by blocking CD40L. J Leukoc Biol 2014; 95:325–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Calderon B, Carrero JA, Miller MJ, Unanue ER. Cellular and molecular events in the localization of diabetogenic T cells to islets of Langerhans. Proc Natl Acad Sci USA 2011; 108:1561–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Price JD, Hotta‐Iwamura C, Zhao Y, Beauchamp NM, Tarbell KV. DCIR2+ cDC2 DCs and Zbtb32 restore CD4+ T‐cell tolerance and inhibit diabetes. Diabetes 2015; 64:3521–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Billiard F, Lobry C, Darrasse‐Jeze G et al Dll4‐Notch signaling in Flt3‐independent dendritic cell development and autoimmunity in mice. J Exp Med 2012; 209:1011–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Allen JS, Pang K, Skowera A et al Plasmacytoid dendritic cells are proportionally expanded at diagnosis of type 1 diabetes and enhance islet autoantigen presentation to T‐cells through immune complex capture. Diabetes 2009; 58:138–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Xia CQ, Peng R, Chernatynskaya AV et al Increased IFN‐alpha‐producing plasmacytoid dendritic cells (pDCs) in human Th1‐mediated type 1 diabetes: pDCs augment Th1 responses through IFN‐alpha production. J Immunol 2014; 193:1024–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rovati B, Mariucci S, Manzoni M, Bencardino K, Danova M. Flow cytometric detection of circulating dendritic cells in healthy subjects. Eur J Histochem 2008; 52:45–52. [DOI] [PubMed] [Google Scholar]
- 14. Harsunen MH, Puff R, D’Orlando O et al Reduced blood leukocyte and neutrophil numbers in the pathogenesis of type 1 diabetes. Horm Metab Res 2013; 45:467–70. [DOI] [PubMed] [Google Scholar]
- 15. Valle A, Giamporcaro GM, Scavini M et al Reduction of circulating neutrophils precedes and accompanies type 1 diabetes. Diabetes 2013; 62:2072–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Carmona‐Rivera C, Kaplan MJ. Low‐density granulocytes: a distinct class of neutrophils in systemic autoimmunity. Semin Immunopathol 2013; 35:455–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Neuwirth A, Dobes J, Oujezdska J et al Eosinophils from patients with type 1 diabetes mellitus express high level of myeloid alpha‐defensins and myeloperoxidase. Cell Immunol 2012; 273:158–63. [DOI] [PubMed] [Google Scholar]
- 18. Min D, Brooks B, Wong J et al Alterations in monocyte CD16 in association with diabetes complications. Mediat Inflamm 2012; 2012:649083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rodacki M, Milech A, de Oliveira JE. NK cells and type 1 diabetes. Clin Dev Immunol 2006; 13:101–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Maruyama T, Watanabe K, Yanagawa T et al The suppressive effect of anti‐asialo GM1 antibody on low‐dose streptozotocin‐induced diabetes in CD‐1 mice. Diabetes Res 1991; 16:171–5. [PubMed] [Google Scholar]
- 21. Piatkiewicz P, Milek T, Bernat‐Karpinska M, Ohams M, Czech A, Ciostek P. The dysfunction of NK cells in patients with type 2 diabetes and colon cancer. Arch Immunol Ther Exp (Warsz) 2013; 61:245–53. [DOI] [PubMed] [Google Scholar]
- 22. Akesson C, Uvebrant K, Oderup C et al Altered natural killer (NK) cell frequency and phenotype in latent autoimmune diabetes in adults (LADA) prior to insulin deficiency. Clin Exp Immunol 2010; 161:48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Qin H, Lee IF, Panagiotopoulos C et al Natural killer cells from children with type 1 diabetes have defects in NKG2D‐dependent function and signaling. Diabetes 2011; 60:857–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Poli A, Michel T, Theresine M, Andres E, Hentges F, Zimmer J. CD56bright natural killer (NK) cells: an important NK cell subset. Immunology 2009; 126:458–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cooper MA, Fehniger TA, Caligiuri MA. The biology of human natural killer‐cell subsets. Trends Immunol 2001; 22:633–40. [DOI] [PubMed] [Google Scholar]
- 26. Xia C, Rao X, Zhong J. Role of T lymphocytes in type 2 diabetes and diabetes‐associated inflammation. J Diabetes Res 2017; 2017:6494795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Menart‐Houtermans B, Rutter R, Nowotny B et al Leukocyte profiles differ between type 1 and type 2 diabetes and are associated with metabolic phenotypes: results from the German Diabetes Study (GDS). Diabetes Care 2014; 37:2326–33. [DOI] [PubMed] [Google Scholar]
- 28. Mallone R, Martinuzzi E, Blancou P et al CD8+ T‐cell responses identify beta‐cell autoimmunity in human type 1 diabetes. Diabetes 2007; 56:613–21. [DOI] [PubMed] [Google Scholar]
- 29. Zmora N, Bashiardes S, Levy M, Elinav E. The role of the immune system in metabolic health and disease. Cell Metab 2017; 25:506–21. [DOI] [PubMed] [Google Scholar]
- 30. Hampe CS. B cell in autoimmune diseases. Scientifica (Cairo) 2012; 2012:215308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sachdeva N, Paul M, Badal D et al Preproinsulin specific CD8+ T cells in subjects with latent autoimmune diabetes show lower frequency and different pathophysiological characteristics than those with type 1 diabetes. Clin Immunol 2015; 157:78–90. [DOI] [PubMed] [Google Scholar]
- 32. Deng C, Xiang Y, Tan T et al Altered peripheral B‐lymphocyte subsets in type 1 diabetes and latent autoimmune diabetes in adults. Diabetes Care 2016; 39:434–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Li Y, Zhao M, Hou C et al Abnormal DNA methylation in CD4+ T cells from people with latent autoimmune diabetes in adults. Diabetes Res Clin Pract 2011; 94:242–8. [DOI] [PubMed] [Google Scholar]
- 34. Dixon KO, van der Kooij SW, Vignali DA, van Kooten C. Human tolerogenic dendritic cells produce IL‐35 in the absence of other IL‐12 family members. Eur J Immunol 2015; 45:1736–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Shen P, Roch T, Lampropoulou V et al IL‐35‐producing B cells are critical regulators of immunity during autoimmune and infectious diseases. Nature 2014; 507:366–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wang RX, Yu CR, Dambuza IM et al Interleukin‐35 induces regulatory B cells that suppress autoimmune disease. Nat Med 2014; 20:633–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bluestone JA, Tang Q. How do CD4+CD25+ regulatory T cells control autoimmunity? Curr Opin Immunol 2005; 17:638–42. [DOI] [PubMed] [Google Scholar]
- 38. Vignali DA, Collison LW, Workman CJ. How regulatory T cells work. Nat Rev Immunol 2008; 8:523–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Atkinson MA, Eisenbarth GS, Michels AW. Type 1 diabetes. Lancet 2014; 383:69–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sakaguchi S, Miyara M, Costantino CM, Hafler DA. FOXP3+ regulatory T cells in the human immune system. Nat Rev Immunol 2010; 10:490–500. [DOI] [PubMed] [Google Scholar]
- 41. Stolp J, Turka LA, Wood KJ. B cells with immune‐regulating function in transplantation. Nat Rev Nephrol 2014; 10:389–97. [DOI] [PubMed] [Google Scholar]
- 42. Niedbala W, Wei XQ, Cai B et al IL‐35 is a novel cytokine with therapeutic effects against collagen‐induced arthritis through the expansion of regulatory T cells and suppression of Th17 cells. Eur J Immunol 2007; 37:3021–9. [DOI] [PubMed] [Google Scholar]
- 43. Collison LW, Workman CJ, Kuo TT et al The inhibitory cytokine IL‐35 contributes to regulatory T‐cell function. Nature 2007; 450:566–9. [DOI] [PubMed] [Google Scholar]
- 44. Creusot RJ, Giannoukakis N, Trucco M, Clare‐Salzler MJ, Fathman CG. It’s time to bring dendritic cell therapy to type 1 diabetes. Diabetes 2014; 63:20–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Li X, Singh K, Luo Z et al Pro‐tumoral immune cell alterations in wild type and Shb‐deficient mice in response to 4T1 breast carcinomas. Oncotarget 2018; 9:18720–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Singh K, Kadesjo E, Lindroos J et al Interleukin‐35 administration counteracts established murine type 1 diabetes – possible involvement of regulatory T cells. Sci Rep 2015;5:12633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Turnis ME, Sawant DV, Szymczak‐Workman AL et al Interleukin‐35 limits anti‐tumor immunity. Immunity 2016; 44:316–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Espes D, Singh K, Sandler S, Carlsson PO. Increased interleukin‐35 levels in patients with type 1 diabetes with remaining C‐peptide. Diabetes Care 2017; 40:1090–5. [DOI] [PubMed] [Google Scholar]
- 49. Rasouli B, Andersson T, Carlsson PO et al Smoking and the risk of LADA: results from a Swedish population‐based case–control study. Diabetes Care 2016; 39:794–800. [DOI] [PubMed] [Google Scholar]
- 50. Hjort R, Alfredsson L, Carlsson PO et al Low birthweight is associated with an increased risk of LADA and type 2 diabetes: results from a Swedish case–control study. Diabetologia 2015; 58:2525–32. [DOI] [PubMed] [Google Scholar]
- 51. Zhou X, Bailey‐Bucktrout SL, Jeker LT et al Instability of the transcription factor Foxp3 leads to the generation of pathogenic memory T cells in vivo . Nat Immunol 2009; 10:1000–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 1999; 130:461–70. [DOI] [PubMed] [Google Scholar]
- 53. Kleffel S, Vergani A, Tezza S et al Interleukin‐10+ regulatory B cells arise within antigen‐experienced CD40+ B cells to maintain tolerance to islet autoantigens. Diabetes 2015; 64:158–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Diana J, Simoni Y, Furio L et al Crosstalk between neutrophils, B‐1a cells and plasmacytoid dendritic cells initiates autoimmune diabetes. Nat Med 2013; 19:65–73. [DOI] [PubMed] [Google Scholar]
- 55. Lou M, Luo P, Tang R et al Relationship between neutrophil‐lymphocyte ratio and insulin resistance in newly diagnosed type 2 diabetes mellitus patients. BMC Endocr Disord 2015; 15:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Yang ZF, Zhou ZG, Tang WL et al Decrease of FOXP3 mRNA in CD4+ T cells in latent autoimmune diabetes in adult. Zhonghua Yi Xue Za Zhi 2006; 86:2533–6. [PubMed] [Google Scholar]
- 57. Cabrera SM, Rigby MR, Mirmira RG. Targeting regulatory T cells in the treatment of type 1 diabetes mellitus. Curr Mol Med 2012; 12:1261–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Long SA, Buckner JH. CD4+FOXP3+ T regulatory cells in human autoimmunity: more than a numbers game. J Immunol 2011; 187:2061–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Collison LW, Chaturvedi V, Henderson AL et al IL‐35‐mediated induction of a potent regulatory T cell population. Nat Immunol 2010; 11:1093–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lee CC, Lin JC, Hwang WL et al Macrophage‐secreted interleukin‐35 regulates cancer cell plasticity to facilitate metastatic colonization. Nat Commun 2018; 9:3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig. S1. Flow‐chart of the inclusion process of study. Of the 17 registered LADA patients of the All New Diabetes in Uppsala (ANDiU) study, 13 were included. Additional patients with type 1 diabetes (T1D, n = 7), and type 2 (T2D, n = 13) diabetes) were recruited from ANDiU. Another 11 participants with T1D were included from the department of Endocrinology, Uppsala University hospital, Uppsala (UAS). Healthy controls (HC, n = 13) were recruited upon arrival (with no infection or systemic inflammation) at the Eriksberg Primary Healthcare Centre (EVC). Study subjects were matched for sex, age and body mass index (BMI).
Fig. S2. The representative gating strategies for tolerogenic APCs. The live cells were gated based on forward scatter (FSC) and side scatter (SSC). Cells were further gated for HLA‐DR and Lin mix expression. HLA‐DR+Lin‐ cells were thereafter gated for the expression of CD11c, CD123 or CD11c and CD123. CD11c+CD123‐HLA‐DR+Lin‐ cells were gated for IL‐12p35 and Ebi3 expression and gate was drawn by using FMO together with isotype controls to analyze IL‐35+ cells.
Fig. S3. The representative gating strategies for NK cells. The live cells were gated based on forward scatter (FSC) and side scatter (SSC). Cells were then gated for CD3 and CD56 expression. CD56high and CD56low cells were thereafter gated for CD16 expression.
Fig. S4. The representative gating strategies for Breg cells. The live cells were gated based on forward scatter (FSC) and side scatter (SSC). They were then gated for CD19 expression. CD19+ cells were gated for the expression of CD24 and CD40. CD19+CD24+CD40+ cells were gated for CD38 expression, CD19+CD24+CD40+CD38+ cells were thereafter gated for IL‐12p35 and Ebi3 expression. FMO together with isotype controls were used for negative control to determine IL‐ 12p35+Ebi3+ (IL‐35+) cells.
Fig. S5. Representative gating strategies for Treg cells. The live cells were gated based on side scatter (SSC) and forward scatter (FSC). The cells were then gated for the expression of CD4 and CD25. CD4+CD25+ cells were further gated for the expression of CD127. CD4+CD25+CD127‐ cells were gated for Foxp3 expression. CD4+CD25+CD127‐ Foxp3+ cells were gated for the expression of IL‐12p35 and Ebi3. IL‐12p35 and Ebi3 gates were made based on fluorescence minus one control together with isotype controls (this control was used as a negative control).
Fig. S6. The proportions of neutrophils, monocytes and NKT cells. The proportions of (a) CD15+ neutrophils in total live cells, (b) CD16+ monocytes in total live cells and (c) CD3+CD56+ NKT cells in total live cells, were determined by using a flow cytometer. HC denotes healthy controls. One‐way ANOVA with Dunnett’s post‐hoc test comparison to patients with LADA was used, n = 13‐16/group.
Fig. S7. The proportions of T‐cells and B‐lymphocytes. The proportions of (a) CD3+CD56‐ T‐cells in total live cells, (b) CD4+CD25‐ T‐cells in total live cells, (c) CD8+ T‐cells in total live cells, (d) CD19+ B‐lymphocytes in total live cells, were determined by using a flow cytometer. HC denotes healthy controls. One‐way ANOVA with Dunnett’s post‐hoc test comparison to patients with LADA was used, n = 13‐16/group.
Fig. S8. The proportions of Treg and tTreg cells among CD4+ T cells. The proportion of (a) CD4+CD25+CD127‐Foxp3+ Treg cells in total live cells, (b) CD4+CD25+CD127‐Foxp3+Helios+ tTreg cells in total live cells, (c) The proportions of CD4+CD25+CD127‐Foxp3+ Treg cells among CD4+ T‐cells and (d) CD4+CD25+CD127‐Foxp3+Helios+ tTregs among CD4+ T‐cells. The proportions of these cells were determined by using a flow cytometer. HC denotes healthy controls. One‐way ANOVA with Dunnett’s post‐hoc test was used for comparisons, n = 13‐16/group.
Table S1. Antibodies for surface and intracellular antigens used in flow cytometry staining.


