Omadacycline is a novel aminomethylcycline antibiotic with potent activity against Staphylococcus aureus, including methicillin-susceptible S. aureus (MSSA) and methicillin-resistant S. aureus (MRSA). We investigated the pharmacodynamic activity of omadacycline against 10 MSSA/MRSA strains in a neutropenic murine thigh model.
KEYWORDS: Staphylococcus aureus, omadacycline, pharmacodynamics
ABSTRACT
Omadacycline is a novel aminomethylcycline antibiotic with potent activity against Staphylococcus aureus, including methicillin-susceptible S. aureus (MSSA) and methicillin-resistant S. aureus (MRSA). We investigated the pharmacodynamic activity of omadacycline against 10 MSSA/MRSA strains in a neutropenic murine thigh model. The median 24-h area under the concentration-time curve (AUC)/MIC values associated with net stasis and 1-log kill were 21.9 and 57.7, respectively.
TEXT
Omadacycline (Nuzyra; Paratek Pharmaceuticals), an aminomethylcycline antibiotic within the tetracycline class, was approved in October 2018 in the United States for the treatment of adults with acute bacterial skin and skin structure infection (ABSSSI) and community-acquired bacterial pneumonia (CABP) based on results from three large randomized controlled trials (1, 2). Previous in vitro and in vivo studies have demonstrated potent Gram-positive activity for omadacycline that includes methicillin-susceptible Staphylococcus aureus (MSSA) and methicillin-resistant S. aureus (MRSA) (4–8). We have previously characterized the pharmacokinetics and pharmacodynamic activity of omadacycline against Streptococcus pneumoniae using a neutropenic murine pneumonia infection model (9). In the current studies, we explored the in vivo activity of omadacycline against multiple strains of S. aureus, including MRSA, to delineate its pharmacodynamic activity and target exposures for stasis and log cidal reduction in the murine thigh infection model.
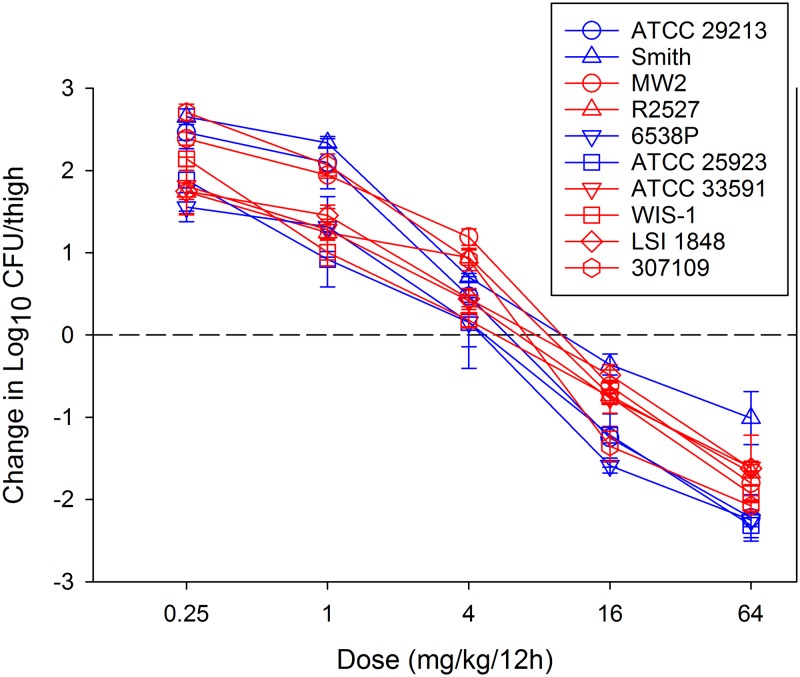
Ten S. aureus strains were utilized (Table 1) that included 6 MRSA and 4 MSSA strains. MICs were determined in triplicate according to CLSI guidelines (10). The MIC range was very narrow, at 0.25 to 0.5 mg/liter. This has been demonstrated in previous studies, with MIC50/MIC90 values that have only varied by a 2-fold dilution (6, 7, 11). The neutropenic murine thigh infection model was used for in vivo study of omadacycline. Animals were maintained in accordance with American Association for Accreditation of Laboratory Animal Care (AAALAC) criteria. All animal studies were approved by the Animal Research Committee of the William S. Middleton Memorial VA Hospital and the University of Wisconsin. Mice were infected with 6.5 ± 0.1 log10 CFU of each strain/thigh. The average in vivo fitness (growth in untreated control mice) of each strain was 2.3 ± 0.3 log10 CFU/thigh over 24 h (range, 1.89 to 2.78 log10 CFU). Two hours after thigh infection, omadacycline was administered to mice by the subcutaneous route every 12 h over the 24-h experiment duration. Omadacycline was administered according to one of five dosing regimens (dose range, 0.25 to 64 mg/kg of body weight/12 h in 4-fold increments). Net stasis and a 1-log reduction in CFU were observed over the dose range for every strain (Fig. 1). The dose-response curves were similar over the dose range, as anticipated, given the relative similarity of the MIC values for all strains. Efficacy was similar against MSSA and MRSA strains.
TABLE 1.
Staphylococcus aureus strains and susceptibility results
| Strain | Omadacycline MIC (mg/liter) | Phenotype |
|---|---|---|
| 307109 | 0.5 | MRSA |
| LSI 1848 | 0.5 | MRSA |
| WIS-1 | 0.5 | MRSA |
| ATCC 33591 | 0.5 | MRSA |
| ATCC 25923 | 0.25 | MSSA |
| ATCC 29213 | 0.25 | MSSA |
| SMITH | 0.25 | MSSA |
| MW2 | 0.5 | MRSA |
| R2527 | 0.5 | MRSA |
| 6538P | 0.25 | MSSA |
FIG 1.
Dose-response curves for omadacycline against 10 S. aureus (blue symbols, MSSA; red symbols, MRSA) strains in the neutropenic murine thigh infection model. Each symbol represents the mean and standard deviation from four thigh infection replicates. Five different dose levels were administered by subcutaneous route every 12 h. The burden of organisms was enumerated at the start and end of therapy over a 24-h experiment duration. The horizontal dashed line at 0 represents the burden of organisms at the start of therapy. Data points above the line represent a net growth (i.e., increase) in burden, and those below the line represent net cidal activity (i.e., decrease) in bacterial burden.
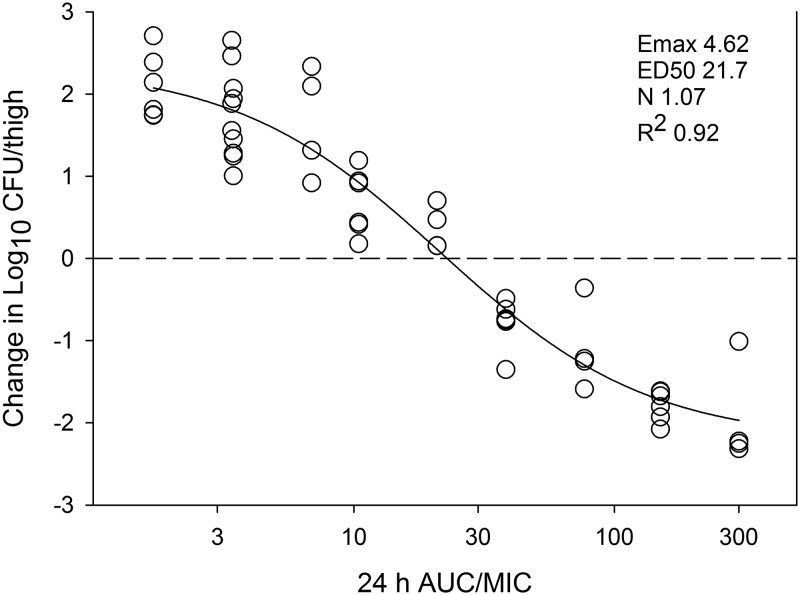
We assessed the pharmacodynamic relationship of the area under the concentration-time curve (AUC)/MIC, as this has been shown in multiple studies to be the most predictive index of therapeutic effect (12–14). Utilizing our previously characterized murine pharmacokinetics of omadacycline from this infection model (9), which demonstrated linear AUC pharmacokinetics (R2 > 0.99), we were able to estimate total drug AUC exposures over the dose range. The resultant AUC/MIC exposures are represented in Fig. 2 for each strain and dosing regimen. There was a strong relationship between AUC/MIC and therapeutic effect, with an R2 of 0.92 when modeled according to the sigmoid maximum effect (Emax) model (Hill equation). The AUC/MIC exposures associated with net stasis and 1-log kill for each strain are shown in Table 2. Stasis was demonstrated at a median 24-h AUC/MIC of approximately 22. One-log kill was noted at a median 24-h AUC/MIC of approximately 58. It should be noted only total drug concentrations were utilized in these studies, as the protein binding of omadacycline is relatively low (∼20%), similar in humans and mice, and without evidence of concentration-dependent effect that has been noted with others in the tetracycline class (15).
FIG 2.
In vivo exposure-response relationship between the pharmacodynamic parameter 24-h AUC/MIC and treatment effect for 10 S. aureus strains in the neutropenic murine thigh infection model. Each symbol is the mean of four thigh replicates. Five total drug dosing regimens were fractionated into an every-12-h regimen. The omadacycline exposure is represented on the x axis as plasma 24-h AUC/MIC. The burden of organisms was measured at the start and end of therapy over a 24-h experiment duration. The change (i.e., difference) between the start and end of therapy is represented on the y axis. The horizontal dashed line at 0 represents the burden of organisms at the start of therapy. Data points above the line represent a net increase, and those below the line represent a net decrease in bacterial burden. The line drawn through the data is the best-fit line based on the sigmoid Emax model (Hill equation). Also shown are the pharmacodynamic parameters Emax (maximum effect), ED50 (50% maximal effect point), N (slope of the line), and coefficient of determination (R2).
TABLE 2.
Omadacycline pharmacodynamic target exposures for each S. aureus strain in the murine thigh infection model
| Organism or measurement | MIC (mg/liter) | Growth in untreated controls (log10 CFU) | 24-h static dose (mg/kg) | Stasis AUC/MIC | 24-h 1-log kill dose (mg/kg) | 1-log kill AUC/MIC |
|---|---|---|---|---|---|---|
| ATCC 29213 | 0.25 | 2.63 | 11.67 | 29.64 | 24.20 | 58.83 |
| SMITH | 0.25 | 2.78 | 20.88 | 51.13 | 128.00 | 302.51 |
| MW2 | 0.5 | 2.49 | 18.78 | 23.12 | 44.07 | 52.49 |
| R2527 | 0.5 | 2.05 | 17.54 | 21.68 | 52.32 | 62.06 |
| 6538P | 0.25 | 1.96 | 8.43 | 22.05 | 19.94 | 48.95 |
| ATCC 25923 | 0.25 | 2.22 | 8.72 | 22.71 | 25.40 | 61.63 |
| ATCC 33591 | 0.5 | 2.47 | 12.84 | 16.19 | 47.62 | 56.61 |
| WIS-1 | 0.5 | 2.31 | 10.80 | 13.80 | 35.45 | 42.48 |
| LSI 1848 | 0.5 | 1.89 | 16.44 | 20.41 | 53.00 | 62.86 |
| 307109 | 0.5 | 2.84 | 13.12 | 16.52 | 26.57 | 32.17 |
| Mean | 2.33 | 13.92 | 23.73 | 45.66 | 78.06 | |
| Median | 2.31 | 12.98 | 21.87 | 39.76 | 57.72 | |
| SD | 0.34 | 4.28 | 10.61 | 31.42 | 79.47 |
These results add to our understanding of omadacycline exposure-response relationships. First, not unexpectedly, in vivo efficacy and pharmacodynamic target exposures were similar for MSSA and MRSA. This confirms in vitro evaluations that have previously demonstrated very similar potency with comparable MIC distributions for these two pathogen groups. Second, against all strains in this study, the exposure-response relationship was relatively steep, with >1-log kill achieved against all strains. The microbiological activity noted in this study helps explain the high rates of efficacy noted in patients with MSSA or MRSA infections in the omadacycline clinical trials (2, 16). Third, we demonstrated a strong relationship between AUC/MIC and therapeutic effect (R2 = 0.92). Similar results have been shown for other agents in the tetracycline class (9, 12–14, 17, 18), confirming that the pharmacokinetic/pharmacodynamic (PK/PD) driver of efficacy for this class is the AUC/MIC. Finally, previous preclinical and clinical evaluations have demonstrated the predictive value of stasis endpoints in the murine model with clinical outcome for patients with bacterial skin and skin structure infections (14, 19). Large surveillance studies have demonstrated an estimated MIC90 of ≤0.25 mg/liter (11, 20). Integrating these data with human pharmacokinetic estimates (8), the stasis AUC/MIC target identified in this study would be exceeded in almost all patients.
In sum, these results suggest that omadacycline is a promising agent against S. aureus, including MRSA. The pharmacodynamic targets identified in the murine thigh model for net stasis suggest achievability for most patients with bacterial skin and skin structure infection when examining the targets in the context of human pharmacokinetics of approved dosing regimens and epidemiological MIC distribution. Future studies are warranted to examine the pharmacodynamic activity of omadacycline against S. aureus at other sites of infection, such as pneumonia.
ACKNOWLEDGMENT
This study was funded by Paratek Pharmaceuticals.
REFERENCES
- 1.Stets R, Popescu M, Gonong JR, Mitha I, Nseir W, Madej A, Kirsch C, Das AF, Garrity-Ryan L, Steenbergen JN, Manley A, Eckburg PB, Tzanis E, McGovern PC, Loh E. 2019. Omadacycline for community-acquired bacterial pneumonia. N Engl J Med 380:517–527. doi: 10.1056/NEJMoa1800201. [DOI] [PubMed] [Google Scholar]
- 2.O’Riordan W, Green S, Overcash JS, Puljiz I, Metallidis S, Gardovskis J, Garrity-Ryan L, Das AF, Tzanis E, Eckburg PB, Manley A, Villano SA, Steenbergen JN, Loh E. 2019. Omadacycline for acute bacterial skin and skin-structure infections. N Engl J Med 380:528–538. doi: 10.1056/NEJMoa1800170. [DOI] [PubMed] [Google Scholar]
- 3.Reference deleted.
- 4.Honeyman L, Ismail M, Nelson ML, Bhatia B, Bowser TE, Chen J, Mechiche R, Ohemeng K, Verma AK, Cannon EP, Macone A, Tanaka SK, Levy S. 2015. Structure-activity relationship of the aminomethylcyclines and the discovery of omadacycline. Antimicrob Agents Chemother 59:7044–7053. doi: 10.1128/AAC.01536-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macone AB, Caruso BK, Leahy RG, Donatelli J, Weir S, Draper MP, Tanaka SK, Levy SB. 2014. In vitro and in vivo antibacterial activities of omadacycline, a novel aminomethylcycline. Antimicrob Agents Chemother 58:1127–1135. doi: 10.1128/AAC.01242-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pfaller MA, Huband MD, Rhomberg PR, Flamm RK. 2017. Surveillance of omadacycline activity against clinical isolates from a global collection (North America, Europe, Latin America, Asia-Western Pacific), 2010–2011. Antimicrob Agents Chemother 61:e00018-17. doi: 10.1128/AAC.00018-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pfaller MA, Rhomberg PR, Huband MD, Flamm RK. 2017. Activities of omadacycline and comparator agents against Staphylococcus aureus isolates from a surveillance program conducted in North America and Europe. Antimicrob Agents Chemother 61:e02411-16. doi: 10.1128/AAC.02411-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Villano S, Steenbergen J, Loh E. 2016. Omadacycline: development of a novel aminomethylcycline antibiotic for treating drug-resistant bacterial infections. Future Microbiol 11:1421–1434. doi: 10.2217/fmb-2016-0100. [DOI] [PubMed] [Google Scholar]
- 9.Lepak AJ, Zhao M, Marchillo K, VanHecker J, Andes DR. 2017. In vivo pharmacodynamic evaluation of omadacycline (PTK 0796) against Streptococcus pneumoniae in the murine pneumonia model. Antimicrob Agents Chemother 61:e02368-16. doi: 10.1128/AAC.02368-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.CLSI. 2018. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 11th ed CLSI standard M07. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 11.Huband MD, Pfaller MA, Shortridge D, Flamm RK. 27 February 2019. Surveillance of omadacycline activity tested against clinical isolates from the United States and Europe: results from the SENTRY Antimicrobial Surveillance Programme, 2017. J Glob Antimicrob Resist doi: 10.1016/j.jgar.2019.02.017. [DOI] [PubMed] [Google Scholar]
- 12.Agwuh KN, MacGowan A. 2006. Pharmacokinetics and pharmacodynamics of the tetracyclines including glycylcyclines. J Antimicrob Chemother 58:256–265. doi: 10.1093/jac/dkl224. [DOI] [PubMed] [Google Scholar]
- 13.Zhao M, Lepak AJ, Marchillo K, VanHecker J, Andes DR. 2017. In vivo pharmacodynamic target assessment of eravacycline against Escherichia coli in a murine thigh infection model. Antimicrob Agents Chemother 61:e00250-17. doi: 10.1128/AAC.00250-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Ogtrop ML, Andes D, Stamstad TJ, Conklin B, Weiss WJ, Craig WA, Vesga O. 2000. In vivo pharmacodynamic activities of two glycylcyclines (GAR-936 and WAY 152,288) against various Gram-positive and Gram-negative bacteria. Antimicrob Agents Chemother 44:943–949. doi: 10.1128/AAC.44.4.943-949.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaturvedi P, Esposito C, Koroma J, Cannon EP, Tanaka SK. 2003. In vitro assessment of plasma protein binding and metabolic stability of PTK 0796. 43rd Intersci Conf Antimicrob Agents Chemother, 14 to 17 September 2003, Washington, DC. [Google Scholar]
- 16.Bassetti M, Armstrong ES, Steenbergen JN, Das A, Eckburg PB, Sirbu A, Garrity-Ryan L, Manley A, Tzanis E, McGovern PC. 2018. Efficacy of oral omadacycline versus linezolid for treating adult subjects with ABSSSI: analysis by infection type and pathogen in the OASIS-2 study. 28th Eur Cong Clin Microbiol Infect Dis, 21 to 24 April 2018, Madrid, Spain. [Google Scholar]
- 17.Andes D, Craig W. 2007. Pharmacokinetics and pharmacodynamics of tetracyclines, p 267–278. In Nightingale CH, Ambrose PG, Drusano GL, Murakawa T (ed), Antimicrobial pharmacodynamics in theory and clinical practice, 2nd ed Informa Healthcare USA, New York, NY. [Google Scholar]
- 18.Lepak AJ, Zhao M, Liu Q, Wang P, Wang Y, Bader JC, Ambrose PG, Andes DR. 2018. Pharmacokinetic/pharmacodynamic evaluation of a novel aminomethylcycline antibiotic, KBP-7072, in the neutropenic murine pneumonia model against S. aureus and S. pneumoniae. Antimicrob Agents Chemother 63:e02404-18. doi: 10.1128/AAC.02404-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meagher AK, Passarell JA, Cirincione BB, Van Wart SA, Liolios K, Babinchak T, Ellis-Grosse EJ, Ambrose PG. 2007. Exposure-response analyses of tigecycline efficacy in patients with complicated skin and skin-structure infections. Antimicrob Agents Chemother 51:1939–1945. doi: 10.1128/AAC.01084-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pfaller MA, Huband MD, Shortridge D, Flamm RK. 2018. Surveillance of omadacycline activity tested against clinical isolates from the United States and Europe as Part of the 2016 SENTRY antimicrobial surveillance program. Antimicrob Agents Chemother 62:e02327-17. doi: 10.1128/AAC.02327-17. [DOI] [PMC free article] [PubMed] [Google Scholar]