Abstract
BACKGROUND
Femoral neck stress fractures are rarely encountered among young adults and are often associated with either repetitive excessive loading or underlying bone pathology. Preliminary research has indicated human immunodeficiency virus (HIV)/antiretroviral therapy (ART) as predisposing agents to osteopenia and osteoporosis related complications. We report a case of HIV/ART induced insufficiency fracture in a resource limited setting in Central India. Our aim is to increase awareness and promote screening of HIV/ART related osteopenia and osteoporosis in order to prevent catastrophic orthopaedic complications.
CASE SUMMARY
A 35-year-old HIV positive male presented with a stress fracture of left femoral neck. The patient was on ART and reported no comorbidities. He went on to be successfully managed surgically. However, during work-up osteopenia of the contralateral proximal femur was recognised using Singh’s Index. Six months post-op the patient presented with right-sided femoral - neck stress fracture. At this stage the patient was nonconcordant with ART and denied surgical fixation.
CONCLUSION
In the absence of co-morbidities, several mechanisms of HIV/antiretroviral therapy may have played a role in predisposing our patient towards such a presentation. We recommend routine screening all HIV-infected patients for osteopenia, especially in younger individuals. In low resource settings and district hospitals, pelvis radiograph & Singh’s index can be used for screening.
Keywords: Bilateral femoral neck stress fracture, Human immunodeficiency virus-antiretroviral therapy related osteopenia, Osteoporosis in resource limited setting, Human immunodeficiency virus related fragility fractures
Core tip: Stress fractures of the femoral neck among young adults are extremely rare. They usually result from either fatigue or predisposing conditions that give rise to weakened bones. We present a case of bilateral sequential femoral neck stress fractures in a young adult with human immunodeficiency virus (HIV) infection on antiretroviral therapy (ART) in the absence of comorbidities. Several mechanisms of HIV/ART induced osteopenia and osteoporosis are indicated to have played a role in predisposing our case towards such a presentation. Our case study adds to the paucity of evidence exploring the association between HIV/ART and reduced bone mineral density. Our case highlights the need for screening and prophylactic treatment for osteopenia and osteoporosis coexisting with HIV infection and ART.
INTRODUCTION
Evolution of antiretroviral therapy (ART), wide coverage of national acquired immunodeficiency syndrome (AIDS) policies and advances in management of opportunistic infections has enabled human immunodeficiency virus (HIV) infected individuals to live longer, stay healthier and enjoy better quality of life. However, HIV infection and ART have both been implicated in osteopenia, which can lead to catastrophic orthopaedic complications[1-3]. Limited access to healthcare and higher disease prevalence noted in resource limited areas in low-middle income countries (LMICs) are reported compounding factors[4]. Despite the huge disease burden of HIV infection as well as osteoporosis across the globe, minimal evidence exists regarding these two coexisting conditions, associated complications, screening methods and prevention. Limited awareness and lack of screening for HIV and ART related orthopaedic complications further add to the conundrum[5,6].
We present a rare report of bilateral sequential femoral neck stress fracture nonunions, evaluated and managed in a resource-limited secondary level rural mission hospital located in Central India. Our aim is to enhance awareness and highlight the need for screening, prophylactic and definitive treatment for HIV and ART related osteopenia and associated catastrophic orthopaedic complications, which can be implemented even in district hospital level healthcare setup.
CASE PRESENTATION
Chief complaint
A 35-year-old male patient presented to the orthopaedic outpatient clinic with a three months history of limp on left side.
History of present illness
Patient was unable to bear weight on the left side. He was able to walk with a walking stick and had to put full weight in the right leg. There was no antecedent history of significant trauma. Patient was unemployed and was not involved in any heavy or strenuous activity. There was no history of substance abuse or steroid intake. There was no pain on the right side.
History of past illness
Patient had been diagnosed with HIV infection more than two years ago. He has been getting the first line National AIDS Control Organization regime of AZT (Zidovudine) and 3TC (Lamivudine) for the last two years from the nearest ART centre, located more than 100 kilometres away[6]. History revealed poor ART compliance. Upon enquiry about the delay of three months in seeking treatment, patient alleged stigma related refusal of treatment elsewhere due to his seropositive status. He did not have any medical comorbidity.
Physical examination upon admission
Upon examination, the patient was comfortable and alert at rest, Patient’s weight was 74.6 kg (BMI 26.4 kg/m2). General physical examination was normal.
He had an externally rotated left lower limb, telescopy and positive Trendelenburg sign with antalgic, assisted gait pattern. No abnormalities were noted on the right lower limb.
Laboratory examinations
Serum 25(OH) vitamin D level (24.6 ng/mL), phosphorus, alkaline phosphatase (113 IU/L), renal function and liver function tests and erythrocyte sedimentation rates were within normal limit. Screening for hepatitis B and hepatitis C was negative.
Provision for bone densitometry-FRAX tool was not available locally and could not be administered due to the patient’s financial constraints. CD4 count done within the last two months was 350/mm3.
Imaging examinations
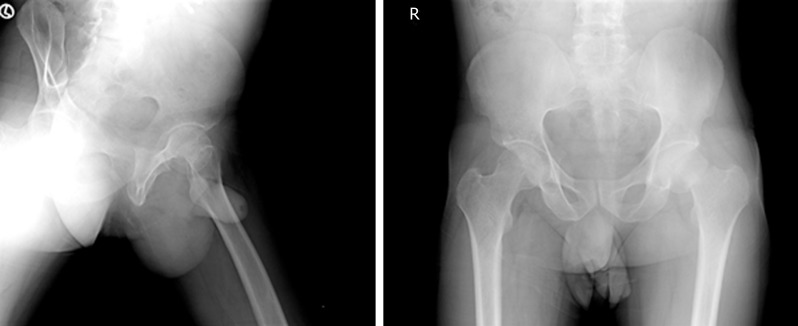
Displaced fracture neck of left femur with break in Shenton’s line, characteristic opening out on the tension side, varus settling of distal fragment and established non union was noted on the radiographs (Figure 1). Significant osteopenia (break in primary tensile trabeculae; Singh’s grade III) was noted on the right proximal femur. (Figure 1). LS spine x-rays were normal
Figure 1.
Preoperative anteroposterior and lateral X-rays demonstrating transcervical stress fracture of left femoral neck, with Singh’s grade III osteopenia noted on the right proximal femur.
Computed tomography and magnetic resonance imaging scan facilities were not performed due to local inaccessibility and patient’s financial constraints.
FINAL DIAGNOSIS
Based on clinical presentation, physical examination, relevant radiographs and laboratory work-up, most alternative causes of missed fracture or secondary osteoporosis were excluded. Non-union of left Femoral neck stress fracture was deemed the final diagnosis.
TREATMENT
Operative technique
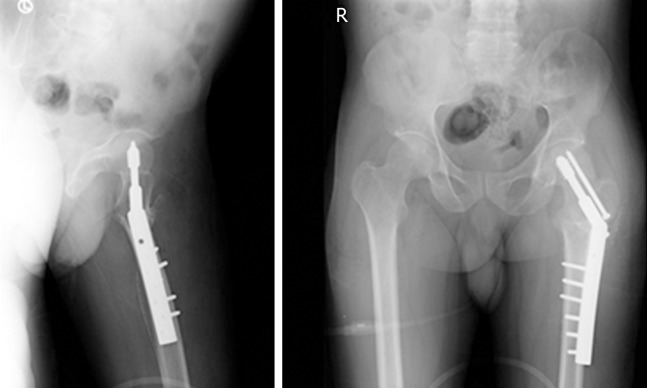
Patient underwent open reduction of left femur neck fracture, valgus osteotomy of the left proximal femur and fixation with dynamic hip screw and additional derotation screw (Figure 2). Patient was positioned supine on a fracture table. Open reduction was done - through a lateral Hardinge approach and confirmed under image in-tensifier. Fracture was fixed with a 130° dynamic hip screw (Richard’s screw) applied at 110° of neck shaft angle and augmented single partially threaded 6.5 mm cancellous screw.
Figure 2.
Postoperative AP and lateral radiographs of left proximal femur valgus Osteotomy demonstrating sliding hip screw fixation.
A twenty degree lateral closing wedge osteotomy performed at the level of lesser trochanter and the distal femur fragment was valgised and attached to the dynamic hip screw barrel plate to gain a valgus neck shaft angle. .
Postoperative management
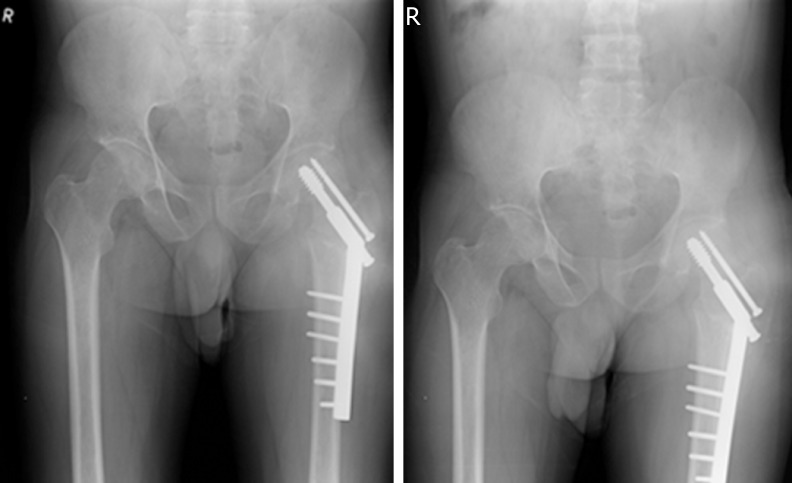
Partial weight bearing with axillary crutches was initiated on second postoperative day progressing to full weight bearing after two weeks. Postoperative convalescence was augmented with dietary and pharmaceutical calcium and calcitriol granules. Bisphosphonate was delayed as they are contraindicated in view of osteotomy and fracture. Radiological confirmation of union and return to prefracture functional status was confirmed at the three months review (Figure 3).
Figure 3.
Three months postop follow up with sound union
OUTCOME AND FOLLOW-UP
At six months follow-up, patient complained of limp and inability to weight bear on the nonoperated (right) limb for one-month duration. There was no history of significant trauma or heavy, strenuous activity. He was able to walk independently in the intervening period. Patient had noted slight pain and ‘pop’ over the right hip area following a mild twisting injury.
Clinical examination revealed external rotation deformity and telescopy of the right proximal femur. Characteristic features of stress fracture non-union of the right neck of femur were confirmed on radiograph (Figure 4). His CD4 count was 180/mm3. Patient was offered surgical fixation of the right femoral neck but declined treatment.
Figure 4.
Six months post operative follow up with stress fracture non union of the Right femur neck
DISCUSSION
Stress fractures of the femoral neck among young adults are extremely rare. They can result from fatigue or secondary to repetitive excessive force exerted over a prolonged duration on normal bone architecture. In young people, such mechanical overloading can lead to excessive bone resorption and temporary ischemic disruption with resultant impaired bone remodelling. This leads to weakening of the bone structure and microfractures. Relentless stress leads to complete fracture[7,8].
Diagnoses of stress fractures are often missed for several weeks due to lack of symptoms and absence of history of traumatic event. Besides, incomplete femoral neck stress fractures are difficult to diagnose in plain radiographs. Though complete fractures are easily identified, their rarity as well as physician’s low index of suspicion often leads to delayed diagnosis and treatment[1,7].
Sometimes, coexisting metastatic disease or metabolic conditions that contribute to weakened bones can aid in screening and diagnosing stress fractures among young adults. Associated infective diseases such as hepatitis B and hepatitis C infection, severe renal impairment, inflammatory arthritis, adrenal insufficiency, corticosteroid excess, alcohol abuse and vitamin D deficiency are often cited as contributory factors[2,9]. In our case, laboratory investigations and performance status of the patient ruled out the aforementioned conditions.
Another avenue of enquiry would be to consider stress fractures as noted in osteoporotic bones (as in postmenopausal osteoporosis or senile osteoporosis) that result from normal stress exerted on weakened bone. Yet, osteoporosis is primarily a disease of the elderly and correlates inversely with the peak bone mass noted in young. Recent evidence has postulated the role of HIV infection and ART, especially Tenofovir, Zidovudine and almost all protease inhibitors as a probable cause of osteopenia, osteoporosis and occasionally, osteonecrosis of the femoral head[2,5,10,11].
Femoral neck stress fractures associated with HIV infection or ART are rare. Even fewer reports of femoral neck stress fracture exist in current literature. Using radiographs with Singh’s Index we were able to classify osteopenia in this case, though ideally access to bone mineral density measurement and application of FRAX tools would be preferred. We hereby review the aetio-pathophysiology for HIV/ART induced secondary osteoporosis.
HIV and osteoporosis
Since the widespread availability of ART in 1996, several studies have reported an increased prevalence of osteopenia in HIV-infected patients. A cross-sectional analysis by Knobel et al[12] revealed osteopenia was present in 25% of healthy adults and in 67.5% of HIV-infected patients; whilst osteoporosis was present in 5% of healthy adults and in 21.2% of HIV-infected patients. Some studies have blamed this increased prevalence as statistically insignificant and biased by confounding covariables such as alcohol abuse, heroin use, glucocorticoid excess and hypo-gonadism[13]. A meta-analysis from Triant et al[2] reported a three times higher risk of osteoporosis among HIV-infected individuals compared to the general population and an even higher risk of osteoporosis associated with ART.
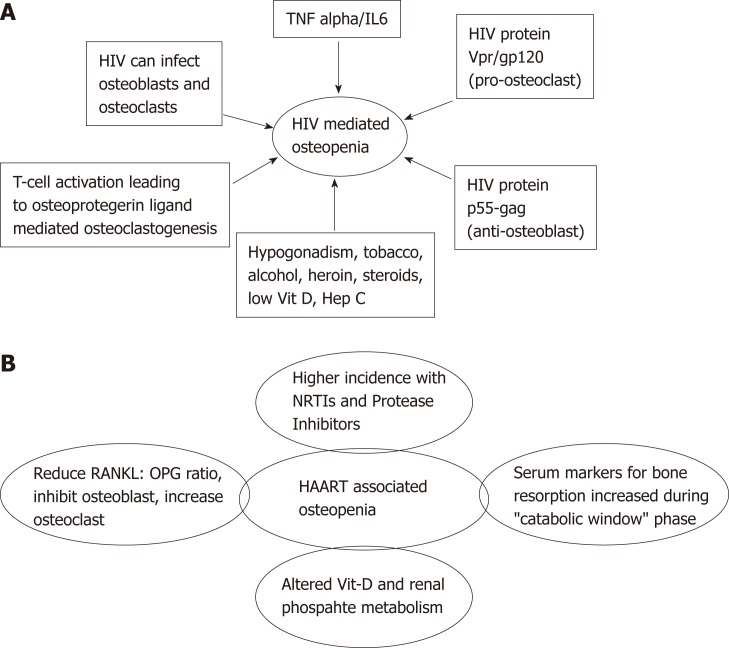
Viral induced systemic inflammation and direct viral mechanisms are alluded to as mediators of HIV-mediated osteoporosis. Specifically, elevated inflammatory cytokines such as tumor necrosis factor alpha in conjunction with HIV proteins Vpr/gp120 (pro-osteoclast) and p55-gag (anti-osteoblast) contribute to a state of enhanced bone resorption without a commensurate rise in bone formation[5,14]. T-cell activation leading to osteoprotegerin ligand mediated osteoclastogenesis, direct inhibition of osteoblasts and activation of osteoclast leading to disturbance of bone resorption/formation coupling are other proposed theories (Figure 5A).
Figure 5.
Suspected mechanisms. A: Human immunodeficiency virus and mediated osteopenia; B: Highly active antiretroviral therapy associated osteopenia. HIV: Human immunodeficiency virus; TNF alpha: Tumor necrosis factor alpha; HAART: Highly active antiretroviral therapy; Vit D: Vitamin D; Hep C: Hepatitis C; NRTIs: Nucleoside reverse transcriptase inhibitors ;OPG: Osteoprotegerin.
ART and osteoporosis
More convincing evidence is appreciated when considering the role of ART in predisposing for osteoporosis. Multiple longitudinal studies have generally shown a 2%–6% loss of bone mineral density after 48–96 wk of therapy, regardless of the type of ART initiated[12,15]. This is presumably due to a “catabolic window” phenomenon wherein the ratio of serum markers of bone resorption to bone formation is elevated during the first six months after ART initiation. Following this, a longer period of bone mineral density stability, particularly as the patient regains weight with commencement of ART, has been observed[11,16].
Mechanisms of ART-induced osteoporosis remains largely speculative (Figure 5B). For Tenofovir, a mechanism has been suggested wherein alterations in renal phosphate handling results in hypophosphatemia and osteomalacia. These effects are enhanced during concomitant vitamin D deficiency[14,17]. Protease inhibitors lead to reduction in RANKL: Osteoprotegerin ratio leading to recruitment and activation of osteoclasts and inhibition of osteoblasts. Rate of bone resorption associated with initiation of ART has been found comparable to that in the postmenopausal period. While the rate of resorption is believed to decrease after one to two years of ART initiation, return of bone mineral density to pre-ART status has not been found[11,17]. Nucleoside reverse transcriptase inhibitors such as Zidovudine and protease inhibitors are associated with vitamin D deficiency as well as altered vitamin D metabolism[11,18].
Recommendations
Our patient with long standing HIV infection with suspected ART noncompliance and with a calcium deficient diet was susceptible to osteopenia, which lead to this catastrophic event. No screening program for osteopenia exists under the National AIDS Control Organization guidelines. Lack of awareness of osteopenia and osteoporosis coexisting with HIV infection and ART could have contributed to the delay in treatment. Review of literature to evaluate the incidence and cause of bilateral femoral neck stress fractures revealed four to nine times higher risk of fractures among young adults with HIV infection and on ART.
Current AIDS control policy and ART policy does not advocate routine screening for osteopenia in HIV-infected individuals regardless if they are being treated with ART[6]. Limited evidence exists regarding prevalence of HIV/ART related osteopenia and associated catastrophic orthopaedic complications from low-middle income countries, even though more than two-thirds of the HIV-infected population hail from these geographic areas. We conducted a pilot study to assess awareness of HIV/ART related orthopaedic complications among healthcare providers. Twenty-five orthopaedic surgeons and ten infectious disease specialists from three primary, nine secondary and one tertiary level healthcare centre revealed very poor awareness about HIV/ART related osteopenia and associated catastrophic orthopaedic complications.
In the given scenario, this case report highlights the need for increasing awareness among healthcare providers as well as establishes routine screening programs and prompt intervention to avoid osteopenia related catastrophic orthopaedic com-plications in HIV-infected patients. Novel methods are necessary to overcome resource limitation such as lack of bone density measurement and FRAX tools as they continue to remain inaccessible to the majority of rural and even urban populations. In this case, we used radiological evaluation with Singh’s index for assessing osteopenia and osteoporosis to overcome the resource constraint at the healthcare centre. It may be substituted as an immediate need for screening of the susceptible population including HIV-infected patients on ART until a better accessible and affordable solution is developed[9].
CONCLUSION
In the absence of any additional discernible cause, HIV infection and ART must be considered as independent risk factors for incapacitating complications of osteopenia and osteoporosis. We recommend routine screening all HIV-infected patients for osteopenia, especially in younger individuals[4]. Radiological evaluation using Singh’s index can be used as an alternative to DEXA screening in fiscally stressed settings. Indeed, a major concerted effort between government agencies, public health and district hospitals is essential for implementation. Yet only then, further research on cost benefit analysis can be performed.
Footnotes
Informed consent statement: The patient provided informed written consent.
Conflict-of-interest statement: All authors have no conflicts of interest to report.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Peer-review started: January 25, 2019
First decision: March 14, 2019
Article in press: May 23, 2019
Specialty type: Medicine, research and experimental
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Emara KM, Ohishi T, Malik H S-Editor: Wang JL L-Editor: Filipodia E-Editor: Ma YJ
Contributor Information
Saisunder Shashank Chaganty, Faculty of Medicine and Dentistry, University of Plymouth, Plymouth PL6 8BU, United Kingdom. saisunder.chaganty@students.plymouth.ac.uk.
Deeptiman James, Assistant Professor, Department of Orthopedics, Christian Medical College, Vellore, Vellore 632004, Tamil Nadu, India.
References
- 1.Biz C, Berizzi A, Crimì A, Marcato C, Trovarelli G, Ruggieri P. Management and treatment of femoral neck stress fractures in recreational runners: a report of four cases and review of the literature. Acta Biomed. 2017;88:96–106. doi: 10.23750/abm.v88i4-S.6800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Triant VA, Brown TT, Lee H, Grinspoon SK. Fracture prevalence among human immunodeficiency virus (HIV)-infected versus non-HIV-infected patients in a large U.S. healthcare system. J Clin Endocrinol Metab. 2008;93:3499–3504. doi: 10.1210/jc.2008-0828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Compston J. HIV infection and osteoporosis. Bonekey Rep. 2015;4:636. doi: 10.1038/bonekey.2015.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matovu FK, Wattanachanya L, Beksinska M, Pettifor JM, Ruxrungtham K. Bone health and HIV in resource-limited settings: a scoping review. Curr Opin HIV AIDS. 2016;11:306–325. doi: 10.1097/COH.0000000000000274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McComsey GA, Tebas P, Shane E, Yin MT, Overton ET, Huang JS, Aldrovandi GM, Cardoso SW, Santana JL, Brown TT. Bone disease in HIV infection: a practical review and recommendations for HIV care providers. Clin Infect Dis. 2010;51:937–946. doi: 10.1086/656412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Aids Control Program. Antiretroviral Therapy Guidelines for HIV-Infected Adults and Adolescents, 2013. Available from: http://naco.gov.in/
- 7.Robertson GA, Wood AM. Femoral Neck Stress Fractures in Sport: A Current Concepts Review. Sports Med Int Open. 2017;1:E58–E68. doi: 10.1055/s-0043-103946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ly TV, Swiontkowski MF. Management of femoral neck fractures in young adults. Indian J Orthop. 2008;42:3–12. doi: 10.4103/0019-5413.38574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.James D, Williams S. Determining prevalence of osteoporosis in health-seeking population of rural central India using Singh’s Index: A resource optimization model to fight a silent epidemic. Chrismed J Health Res. 2018;5:173–177. [Google Scholar]
- 10.Brown TT, Qaqish RB. Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytic review. AIDS. 2006;20:2165–2174. doi: 10.1097/QAD.0b013e32801022eb. [DOI] [PubMed] [Google Scholar]
- 11.Kruger MJ, Nell TA. Bone mineral density in people living with HIV: a narrative review of the literature. AIDS Res Ther. 2017;14:35. doi: 10.1186/s12981-017-0162-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knobel H, Guelar A, Vallecillo G, Nogués X, Díez A. Osteopenia in HIV-infected patients: is it the disease or is it the treatment? AIDS. 2001;15:807–808. doi: 10.1097/00002030-200104130-00022. [DOI] [PubMed] [Google Scholar]
- 13.Sharma A, Flom PL, Weedon J, Klein RS. Prospective study of bone mineral density changes in aging men with or at risk for HIV infection. AIDS. 2010;24:2337–2345. doi: 10.1097/QAD.0b013e32833d7da7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walker Harris V, Brown TT. Bone loss in the HIV-infected patient: evidence, clinical implications, and treatment strategies. J Infect Dis. 2012;205 Suppl 3:S391–S398. doi: 10.1093/infdis/jis199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paton NI, Macallan DC, Griffin GE, Pazianas M. Bone mineral density in patients with human immunodeficiency virus infection. Calcif Tissue Int. 1997;61:30–32. doi: 10.1007/s002239900288. [DOI] [PubMed] [Google Scholar]
- 16.Bolland MJ, Wang TK, Grey A, Gamble GD, Reid IR. Stable bone density in HAART-treated individuals with HIV: a meta-analysis. J Clin Endocrinol Metab. 2011;96:2721–2731. doi: 10.1210/jc.2011-0591. [DOI] [PubMed] [Google Scholar]
- 17.Wheeler AL, Tien PC, Grunfeld C, Schafer AL. Teriparatide treatment of osteoporosis in an HIV-infected man: a case report and literature review. AIDS. 2015;29:245–246. doi: 10.1097/QAD.0000000000000529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Havers FP, Detrick B, Cardoso SW, Berendes S, Lama JR, Sugandhavesa P, Mwelase NH, Campbell TB, Gupta A ACTG A5175 PEARLS and NWCS319 Study Teams. Change in vitamin d levels occurs early after antiretroviral therapy initiation and depends on treatment regimen in resource-limited settings. PLoS One. 2014;9:e95164. doi: 10.1371/journal.pone.0095164. [DOI] [PMC free article] [PubMed] [Google Scholar]