Abstract
Background:
Adolescents females with severe obesity are less likely to be sexually active, yet those who are engage in risky sexual behaviors.
Objectives:
To examine patterns and predictors of sexual-risk behaviors, contraception practices, and sexual health outcomes in female adolescents with severe obesity who did/did not undergo bariatric surgery across 4 years.
Setting:
Five academic medical centers
Methods:
Utilizing a prospective observational controlled design, female adolescents undergoing bariatric surgery (n = 111;Mage =16.95±1.44 years; Body Mass Index: MBMI=50.99±8.42, 63.1% White) and nonsurgical comparators (n = 68; Mage=16.18±1.36 years; MBMI=46.47±5.83, 55.9% White) completed the Sexual Activities and Attitudes Questionnaire at pre-surgery/baseline, 24- and 48-month follow-up, with 83 surgical females (MBMI=39.27±10.08) and 49 nonsurgical females (MBMI=48.56±9.84) participating at 48-months.
Results:
Most experienced sexual debut during the 4-year study period, with a greater increase in behaviors conferring risk for sexually transmitted infections (STIs) for surgical females (p=.03). Half (50% surgical, 44.2% nonsurgical, p=.48) reported partner condom use at last sexual intercourse. Number of lifetime STIs were similar (surgical 18.7%, nonsurgical 14.3%). Surgical were more likely to report a pregnancy (25.3% surgical, 8.2% nonsurgical, p=.02) and live birth (16 births in 15 surgical, 1 nonsurgical) with 50% of surgical offspring born to teen mothers (age≤19 years).
Conclusions:
Bariatric care guidelines and practices for adolescent females must emphasize risks and consequences of teen or unintended pregnancies, sexual decision-making, as well as dual protection and STI prevention strategies to optimize health and well-being for the long-term.
Keywords: adolescent, young adult, sexual behavior, health risk, pregnancy
Unlike adult patients, an adolescent’s post-operative course unfolds across what are normative developmental phases known for engagement in risky behaviors that may threaten health and well-being. For example, sexual risk behaviors (e.g., unprotected sex, multiple partners, while “drunk or high”) are typically initiated during adolescence, peak in young adulthood and decline thereafter.1,2 Peak periods for unintended pregnancies in females and acquiring sexually transmitted infections (STIs) including human immunodeficiency virus (HIV) for both sexes follow.3–5 Theoretically, this age-based vulnerability to sexual and other high risk behaviors (i.e., substance use) is due to brain maturation patterns of heightened reward-seeking and impulsive behaviors, later tempered by developing self-regulation skills.6 From a sociological perspective, high risk behaviors during this period reflect evolving ties with peers who increasingly influence both positive and negative health behaviors.7
Interestingly, consensus from epidemiological surveillance samples indicates adolescents with obesity, particularly severe obesity, are less likely to experience romantic or sexual partnerships during adolescence than youth of healthy weight, yet for females, higher numbers of sexual risk behaviors if sexually active.8–10 We demonstrated similar patterns in a clinical sample of adolescent females with severe obesity, including those prior to undergoing bariatric surgery.11 Collectively, this literature has asserted that obesity may play a role in risks associated with adolescent females’ sexual behavior, warranting tailored sexual health care needs.
How sexual behaviors and risks emerge for adolescent females within the context of surgical weight loss is unknown. Moreover, understanding what differentiates those who engage in risk behaviors and/or experience negative sexual health outcomes (e.g., unintended pregnancy, teen child-bearing, STIs, HIV) is critical. Unfortunately, the adult literature emphasizes topics of less relevance to adolescent/young adult care pathways.12–18 Unlike adolescents, most adult patients (i.e., median age ≅ 45 years) are sexually active at time of surgery, albeit reporting sexual dissatisfaction, impairments in sexual quality of life and functioning, and negative impacts on fertility. Identifying what may be uniquely adolescent health or psychosocial risks is imperative to inform patient selection and post-operative care to maximize benefits and minimize risks for long-term health.
The present study tracked adolescent females with severe obesity undergoing bariatric surgery to 48-months post-surgery and examined sexual and HIV-risk behaviors and sexual health practices and outcomes (i.e., contraception, pregnancy, STIs) compared to a non-surgical group. Recognizing there is no prior literature, we hypothesized that relative to non-surgical females, those who had undergone bariatric surgery would engage in more normative (i.e., catch up) as well as risky sexual behaviors over time, given rapid and substantial weight loss and associated improvements in quality of life. Models of differential engagement in sexual risk behaviors were then examined which included primary surgical outcomes (i.e., percent weight loss, weight-related quality of life [WRQOL]). Based on the broader developmental literature, additional potential baseline and concurrent explanatory factors of greater sexual risk were explored, several of which are also correlates of adolescent severe obesity, and included: sensation-seeking behavior and psychological dysregulation,19,20peer engagement in risky sex,21 substance use,22,23, psychopathology,24,25 family dysfunction,26 or a history of child maltreatment.27,28
METHODS
Overview of Study Design
Participants in the Teen Longitudinal Assessment of Bariatric Surgery consortium (Teen-LABS; N=242, ages 13–19), a multi-site prospective observational safety and efficacy study,29 were invited if eligible to participate in a parallel series of independently funded ancillary studies tracking the psychosocial benefits and risks of bariatric surgery from pre-surgery and across the first four post-operative years. These ancillary studies were enhanced by the inclusion of a comparative nonsurgical group of demographically similar adolescents with severe obesity recruited from the Teen-LABS sites observed over the same course of time. Eligibility criteria and enrollment for both the parent Teen-LABS and initial ancillary (TeenView) have been previously described.11,29 Those retained at 24-months were approached to enroll in a supplemental study (TeenView2), participation in which was an eligibility criterion for a third study (TeenView3) at 48-months. Recruitment/participation rates across the TeenView series are detailed in Figure 1. Respective study protocols were approved by site Institutional Review Boards.
Figure 1.
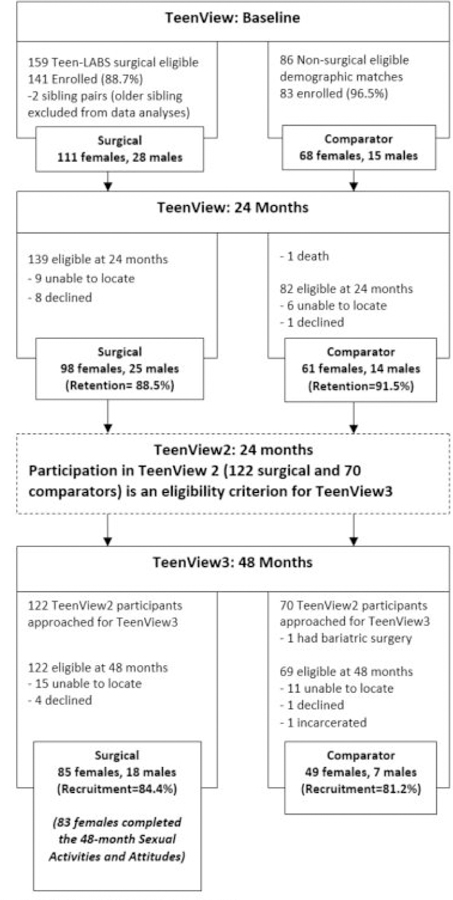
Participant recruitment and retention.
Participants and Procedures.
Pre-surgery/baseline, 24-, and 48-month data were utilized in the present analyses. Participants provided written assent/consent at each study phase. Participants were told their responses would remain confidential, including not being shared with caregivers. Baseline and 24-month assessments were completed at in-person research visits at a Teen-LABS site with trained research personnel, independent of clinical care. Several measures, including the present main outcomes (See Sexual Activities and Attitudes Questionnaire [SAAQ]30 below),were administered in computerized form via a study laptop, where responses were automatically transferred into a study secured, de-identified database, only accessible by research staff. At 24-months, if participants were unable to return to their clinical site (n=14 surgical, n=4 non-surgical), self-report measures were completed via a study secured, de-identified web-based research portal, or if internet was unavailable, as paper versions that were mailed and returned via pre-paid self-addressed envelope. Height and weight measurements were obtained via field visits by Teen-LABS study affiliates (surgical group only)29 or self-reported (non-surgical). At 48-months, all TeenView3 assessments were completed remotely with the participant at their home location. For these home-based assessments, all measures, including the SAAQ, were completed via a study secured, de-identified web-based research portal. Height and weight measurements were obtained via field visits by Teen-LABS study affiliates (n=16 surgical group only)29 or self-reported (surgical: n=4; non-surgical, n=45). Males were excluded from present analyses due to study aims and small sample size.
Measures
Outcome Measures
Sexual Activities and Attitudes Questionnaire (SAAQ).
The SAAQ30 is a self-report of the frequency of voluntary sexual and sexual risk behaviors, sexual health outcomes, and contraceptive usage, with two summary scores. Risky Sexual Behaviors (RSB) is the sum score across five behaviors within the past year (e.g., “sex while drunk or high”, See Table 2) on a scale from 0 (never) to 5 (with ≥ 10 partners). The lifetime HIV-risk score is the sum of having ever engaged in 11 HIV-risk-related behaviors (presence/absence), including sexual risk behaviors, intravenous drug use, or partner characteristics (individual items are listed in Table 1).
Table 2.
Correlates of past year risky sexual behavior and lifetime HIV risk at 48 months for females in surgical and comparator groups.
| Past Year Risky Sexual Behavior (RSB) at 48 months | Lifetime HIV Risk at 48 months | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgical | Comparator | Surgical | Comparator | |||||||||
| Concurrent Variables | B | 95 % Confidence Interval | p a | B | 95 % Confidence Interval | p a | B | 95 % Confidence Interval | p a | B | 95 % Confidence Interval | p a |
| Race | 0.03 | [−2.16, 1.84] | .98 | 0.92 | [−0.26, 3.09] | .31 | 0.07 | [−0.43, 1.69] | .91 | 1.19 | [−0.34, 3.65] | .25 |
| Age | 0.09 | [−1.61, 0.50] | .89 | −0.04 | [−0.38, 0.45] | .93 | −0.06 | [−0.68, 0.12] | .81 | 0.17 | [−0.12, 0.36] | .25 |
| Maltreatment at 24 months | −0.35 | [−2.17, 6.29] | .85 | 0.80 | [−1.36, 1.92] | .26 | −0.41 | [−1.57, 1.13] | .41 | −0.43 | [−1.78, 0.27] | .47 |
| Baseline Behavior (SAAQ)b | −0.17 | [−0.91, 0.52] | .62 | 0.60 | [−0.06, 0.82] | .01 | 0.23 | [−0.21, 0.66] | .47 | 0.26 | [−0.22, 0.69] | .25 |
| % Weight Loss | 0.01 | [−0.07, 0.06] | .78 | −0.01 | [−0.05, 0.03] | .79 | 0.02 | [−0.03, 0.07] | .39 | −0.01 | [−0.04, 0.08] | .78 |
| Total Problems (YSR/ASR) | −0.03 | [−0.06, 0.10] | .56 | −0.05 | [−0.11, 0.02] | .10 | −0.002 | [−0.03, 0.03] | .92 | −0.01 | [−0.04, 0.02] | .69 |
| Total Weight-Related Quality of Life (IWQOL-Lite) | −0.02 | [−0.06, 0.10] | .70 | 0.04 | [−0.01, 0.07] | .03 | −0.02 | [−0.09, 0.04] | .58 | 0.01 | [−0.05, 0.03] | .45 |
| Sensation Seeking | 1.88 | [−0.22, 3.61] | .06 | 2.25 | [−1.60, 3.98] | .11 | 1.70 | [0.07, 3.57] | .07 | 1.24 | [0.01, 4.40] | .34 |
| Dysregulation | 0.03 | [−0.05, 0.05] | .17 | 0.05 | [−0.03, 0.15] | .25 | 0.00 | [−0.03, 0.01] | .97 | 0.00 | [−0.05, 0.02] | .80 |
| Friends’ Risky Sexual Behavior (SAAQ) | 0.13 | [0.00, 0.20] | .01 | 0.13 | [0.06, 0.24] | .004 | 0.06 | [0.03, 0.14] | .04 | 0.08 | [0.03, 0.23] | .07 |
| Alcohol in the past 12 months | 1.75 | [1.29, 2.64] | <.01 | 1.71 | [−1.75, 3.51] | .16 | 0.80 | [0.21, 1.56] | .05 | −0.37 | [−2.76, 0.54] | .66 |
| Illicit drug use in the past 12 months | 2.14 | [0.56, 4.36] | .08 | 0.99 | [−0.54, 2.61] | .55 | 1.27 | [0.63, 2.53] | .05 | 2.03 | [−0.13, 4.68] | .07 |
Note: ASR= Adult Self Report; HIV= Human Immunodeficiency Virus; IWQOL= Impact of Quality of Life; SAAQ= Sexual Activities and Attitudes Questionnaire; YSR= Youth Self Report
p-values for multiple regression analyses completed within each group with race, age, and corresponding baseline behavior as covariates.
Baseline RSB or baseline HIV risk.
Table 1.
Self-reported engagement in past year risky sexual behavior and lifetime HIV risk at baseline, 24-months, and 48-months in female surgical patients and female comparators.
| Baseline Age range=13–19 years | 24 Months Age range=15–21 years | 48 Months Age range=17–23 years | ||||
|---|---|---|---|---|---|---|
| Sexual Activities and Attitudes Questionnaire | Surgical (n=109) n (%) M±SD | Comparator (n=68) n (%) M±SD | Surgical (n=96) n (%) M±SD | Comparator (n=60) n (%) M±SD | Surgical (n=83) n (%) M±SD | Comparator (n=49) n (%) M±SD |
| Past Year | ||||||
| Sexual Intercourse | 18 (17%) | 21 (31%) | 54 (56%) | 29 (48%) | 60 (74%)a | 31 (63%)a |
| Number of Sexual Intercourse Partners | ||||||
| 0 | 91 (84%) | 47 (69%) | 42 (44%) | 31 (52%) | 21 (26%)a | 18 (38%)a |
| 1 | 11 (10%) | 9 (13%) | 29 (30%) | 10 (17%) | 29 (36%) | 18 (38%) a |
| >2 | 7 (6%) | 12 (18%) | 25 (26%) | 19 (32%) | 31 (38%) | 12 (25%) a |
| Past Year Risky Sexual Behavior Score (RSB) | 0.81 ± 2.07 | 1.41 ± 2.78 | 2.59 ± 3.37 | 2.72 ± 4.13 | 4.31 ± 3.71 | 3.47 ± 3.80 |
| Oral Sex (Give or Receive) | 22 (20%) | 22 (32%) | 50 (52%) | 30 (50%) | 66 (80%) | 29 (59%) |
| Sexual intercourse in a one night stand | 7 (6%) | 8 (12%) | 18 (19%) | 16 (27%) | 29 (35%) | 11 (22%) |
| Unprotected sexual intercourse | 9 (8%) | 12 (18%) | 38 (40%) | 22 (37%) | 50 (60%) | 24 (49%) |
| Sexual intercourse while drunk or high | 5 (5%) | 7 (10%) | 21 (22%) | 12 (20%) | 37 (45%) | 15 (31%) |
| Lifetime HIV Risk Score (Total) | 0.65 ± 1.45 | 1.03 ± 1.81 | 1.81 ± 2.04 | 2.17 ± 2.43 | 3.21 ± 2.26 | 2.22 ± 2.23 |
| 48 (51%)b | 26 (43%) | 57 (70%)c | 24 (49%) | |||
| Intercourse without a condom | 14 (13%) | 14 (21%) | ||||
| Condom falls off/breaks during intercourse | 10 (9%) | 7 (10%) | 16 (17%)b | 18 (30%) | 26 (31%) | 10 (20%) |
| Intercourse with a homosexual male | 1 (1%) | 1 (2%) | 0 | 2 (3%) | 4 (5%) | 0 |
| Intercourse with someone with ≥2 current sexual partners | 4 (4%) | 7 (10%) | 12 (13%)b | 14 (23%) | 24 (29%)c | 11 (22%) |
| Intercourse in a one night stand | 10 (9%) | 9 (13%) | 21 (22%)b | 15 (25%) | 37 (45%)c | 13 (27%) |
| Intercourse while drunk or high | 5 (5%) | 8 (12%) | 21 (22%)b | 13 (22%) | 38 (46%)c | 14 (29%) |
| Oral sex without a condom/dental dam | 17 (16%)d | 17 (25%)d | 44 (46%)b | 25 (42%)c | 62 (75%) | 29 (59%) |
| Intercourse/oral sex with bisexual partner | 9 (8%)d | 5 (8%)d | 10 (11%)b | 12 (20%) | 13 (16%) | 7 (14%) |
| Intercourse/oral sex with intravenous drug user | 0 | 1 (2%) | 0 | 3(5%) | 2 (2%)c | 1 (2%) |
| Use intravenous drugs | 0 | 0 | 0 | 1 (2%) | 1 (1%) | 0 |
| Shared hypodermic needles with others | 0 | 0 | 0 | 1 (2%) | 1 (1%) | 0 |
| Contraceptive Used at Last Sexual Intercourse | n=23 | n=24 | n=57 | n=32 | n=64 | n=34 |
| Condom only | 4 (17%) | 6 (25%) | 4 (7%) | 3 (9%) | 9 (14%) | 4 (12%) |
| Condom and Hormonale | 8 (35%) | 6 (25%) | 16 (28%) | 13 (41%) | 15 (23%) | 9 (27%) |
| Condom and Non-Hormonalf | 4 (17%) | 2 (8%) | 10 (18%) | 2 (6%) | 8 (13%) | 2 (6%) |
| All methods without condomg | 6 (26%) | 5 (21%) | 23 (40%) | 5 (16%) | 20 (31%) | 8 (24%) |
| None | 1 (4%) | 5 (21%) | 4 (7%) | 9 (28%) | 12 (19%) | 11 (32%) |
| Confidence in Preferred Birth Control Methodh | ||||||
| Preventing Pregnancy | 19 (83%) | 16 (67%) | 44 (77%) | 16 (50%) | 48 (75%) | 18 (53%) |
| Preventing Sexually Transmitted Infections | 16 (70%) | 10 (42%) | 34 (57%) | 13 (41%) | 29 (45%) | 17 (50%) |
Note: HIV= Human Immunodeficiency Virus
Missing for n= 2 surgical, n=1 comparator
Missing for n=1 surgical, n=1 comparator
Missing for n=1 surgical
Missing for n=2 surgical, n=1 comparator
Condom used in combination with hormonal methods (birth control pills, monthly vaginal ring, “the shot” (Depo Provera), implant, contraceptive patch, or emergency contraception).
Condom used in combination with non-hormonal methods (intrauterine device (IUD), sponge, spermicides, diaphragm or cervical cap, withdrawal, rhythm method). Those cases in which use of a condom, a hormonal method and a non-hormonal method were endorsed were not counted here, but were included as part of the condom and hormonal category.
All methods (i.e., hormonal and/or non-hormonal) not used in combination with a condom.
Confidence in preferred birth control method: Somewhat to very confident (versus not at all confident, a little confident, or in between).
Participants responded, if relevant, to: age at first sexual intercourse, lifetime number of sexual partners, STI history (number of infections of chlamydia, gonorrhea, syphilis, genital warts, genital herpes, HIV, Hepatitis B or C), pregnancies, live births, and age at live birth. Contraceptive method(s) used at last sexual intercourse (0=no, 1= yes) were categorized similarly to the 2011–2015 National Survey of Family Growth (NSFG)31: condom, hormonal (birth control pills, monthly vaginal ring, Depo Provera, implant, contraceptive patch or emergency contraception), or nonhormonal (intrauterine device, sponge, spermicide, diaphragm or cervical cap, rhythm method, withdrawal). Participants rated their confidence in their preferred contraceptive method to prevent pregnancy and STIs (0= “not at all confident” to 4 = “very confident”).
Predictors, Correlates
Potential baseline predictors of RSB and HIV-risk at 48-months included: (a) history of physical or sexual abuse on the Childhood Trauma Questionnaire (CTQ: ≥ “moderate severity” classification32); (b) psychopathology from the Youth Self-Report (YSR: Total Problems33); (c) WRQOL from the Impact of Weight on Quality of Life-Kids (IWQOL-Kids: Total34); (d) family dysfunction from the Family Assessment Device (FAD; General Functioning35); and (e) friends’ engagement in sexual risk behaviors via the SAAQ.30
Potential correlates included: (a) percent weight change from baseline [weightpre-surgery – weightfollow-up] /weightpre-surgery)*100%; (b) updated history of physical/sexual abuse at 24-months32; (c) psychopathology from the YSR33 or Adult Self-Report (ASR36) if age ≥ 19 years; (d) Total WRQOL on the IWQOL-Kids34 or the IWQOL-Lite37 if age ≥ 19 years; (e) Total score of the Sensation Seeking scale;38 (f) Total score of the Dysregulation Inventory;39 (g) friends’ engagement in sexual risk behaviors;30 and (h) past year alcohol and illicit drug use via questions from the national survey, Monitoring the Future (MTF).40
Analysis Plan
Missing data were handled via maximum likelihood estimation in Mplus (Version 7.11) with nesting of participants within the five sites controlled for in hypothesized analyses via specialized variable and analysis commands. Preliminary analyses compared groups (surgical, nonsurgical) on demographics and examined potential attrition bias by comparing baseline characteristics of longitudinal participants to those only completing the baseline assessment.
Prevalence or means/standard deviations at all time-points were calculated for all SAAQ outcomes. Changes over time by group (surgical, nonsurgical) in female RSB and HIV-risk were examined via longitudinal structural equation modeling with covariates of age, race, and baseline body mass index (BMI). Linear regressions examined predictors and correlates of RSB and HIV-risk at 48-months with age, race and baseline levels of the corresponding dependent variable controlled. Given limited sample size, models were analyzed separately by group (surgical, nonsurgical). Confidence intervals (CI) were generated with a bootstrapping procedure with 5000 re-samples.
RESULTS
Sample characteristics
Participants were predominantly White (surgical:63% [n=70], nonsurgical:56% [n=38], p=.34), with surgical females significantly older (surgical: 16.95±1.44 years, nonsurgical: 16.18±1.36 years; p=.001) Surgicals presented with a higher BMI than nonsurgicals at baseline (surgical: 50.99 ± 8.42 kg/m2, nonsurgical: 46.47 ± 5.83 kg/m2; p<.001), and underwent a primary surgical procedure: 66% (n=73) Roux-en-Y gastric bypass (RYGB), 32% (n=35) sleeve gastrectomy (SG), 3% (n=3) adjustable gastric band.
At 48-months, the surgical group were again significantly older (surgical: 21.27±1.36 years, nonsurgical: 20.54±1.29 years; p=.003), with the majority continuing to live with parents or other relatives (surgical:64% [n=50], nonsurgical:71% [n=34], p=.44), not married/engaged (surgical:85.9% [n=67], nonsurgical:89.6% [n=43], p=.55), and in school or working full/part-time (surgical:81% [n=63], nonsurgical:73.% [n=35], p=.30). Surgicals experienced a greater percent change in weight (surgical: −22.77 ± 14.29, nonsurgical: +6.20 ±16.11; p<.001) and lower BMI (surgical: 39.27 ± 10.08 kg/m2, nonsurgical: 48.56 ± 9.84kg/m2; p<.001).
No significant differences were identified between females who completed the 48-month SAAQ assessment (n=132) and those who did not (n=47) for baseline RSB and HIV-risk, or for group status (surgical, nonsurgical), race, age or baseline BMI.
Sexual-and HIV-risk behaviors
At baseline, a minority of females had engaged in their first sexual intercourse (surgical: 21%, 95%CI:13–29; nonsurgical: 35%, 95%CI:24–47; p=.04). By 48-months, these numbers had increased (surgical: 81%, 95%CI:72–89; nonsurigcal: 69%, 95%CI:56–82; p=.15), with age of first sexual intercourse approximately 17 years (surgical: 17.3±2.0, nonsurgical: 16.9±2.5, p=.42). Prevalence data for sexual and risk behaviors are presented in Table 1.
Longitudinal analyses examined change over time by group in RSB and HIV-risk after controlling for age, race and baseline BMI (Figures 2a-2b). For RSB, there was a non-significant group intercept difference (p=.18) and group by time interaction (surgical: y=0.12x-2.94; nonsurgical: y=−0.16x-2.12; p=.11), indicating groups engaged in similar levels of RSB at baseline and a similar linear rate of increase over time. For HIV-risk, there was a marginally significant group intercept difference (p=.05) and a significant group by time interaction (surgical: y=0.86x-2.41; nonsurgical: y=0.58x-1.80; p=.03). While nonsurigcals’ behaviors indicated greater HIV-risk at baseline, surgical participants experienced a significantly greater linear rate of increase over time.
Figure 2.
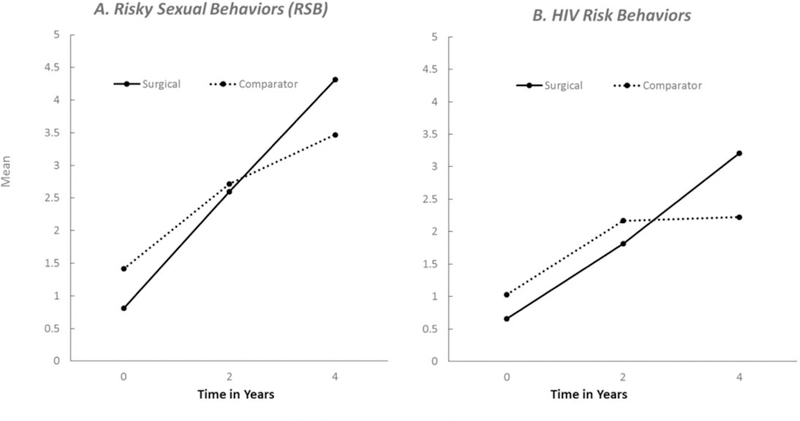
Observed means are plotted for surgical females and comparator females. A. For RSB, longitudinal analyses within a structural equation modeling framework indicated a non-significant group by time interaction (surgical: y = 0.12x-2.94; comparator: y = −0.16x-2.12; p=0.11) and group difference for the intercept (p = 0.18) B. For HIV Risk Behaviors, analyses indicated a significant linear slope for the group by time interaction (surgical: y=0.86x-2.41; comparator: y=0.58x-1.80; p=0.03) and a marginally significant group difference for the intercept (p=0.05). Age, race, and baseline BMI were controlled in both analyses.
Contraception
At 48 months, 50% (95%CI:38–62) of surgical and 44% (95%CI:27–61) of nonsurgical (p=.48) reported partner condom use at last sexual intercourse, either as the only form of contraception (surgical:14%; nonsurgical: 12%) or in combination with hormonal (surgical: 23%; nonsurgical: 27%) or non-hormonal contraception (surgical: 13%; nonsurgical: 6%). Conversely, 19% (95%CI:9–28) of surgical and 32% (95%CI:17–48; p=.13) of nonsurgical used no condom/contraception (Table 2). Significantly more surgical (75%, 95%CI:64–86) endorsed feeling somewhat/very confident that their preferred birth control would prevent pregnancy relative to nonsurgical (53%, 95%CI:36–70; p=.03), while approximately half in both groups (surgical: 45%, 95%CI:33–58; surgical: 50%, 95%CI:33–67) felt somewhat/very confident in preventing STIs.
Sexual health outcomes
Fifteen (18%, 95%CI:10–26) surgical and 7 (14%, 95%CI:4–24) nonsurgical (p=.61) reported a lifetime history of one or more STIs (surgical: 11%=1 STI, 7% ≥2 STI; nonsurgical: 12%=1 STI; n=1 ≥ 2 STI), with no reports of HIV. During the 4-year study period, 21 (25.3%, 95%CI:16–35) surgical and 4 (8%, 95%CI:0.5–16) nonsurgical (p=.02) reported a pregnancy, with a total of 16 live births occurring among 15 surgical females (19%) post-operatively relative to 1 live birth for nonsurgical (2%). Two surgical females reported a pregnancy/live birth prior to surgery. Of the 18 total offspring in the surgical sample, 9 (50%) were born to teen mothers (i.e., ≤ age 19).
Predictors and correlates of sexual health risk
Regression analyses examined baseline predictors and concurrent correlates of RSB and HIV-risk for females at 48-months by group (surgical, nonsurgical). No significant baseline predictors were identified for either outcome by group (data not presented but are available upon request). As seen in Table 2, and controlling for baseline RSB, significant concurrent correlates of surgical 48-month RSB included past-year alcohol use and friends’ risky sexual behaviors, with marginal significance for greater sensation seeking (p=.06). For nonsurgical, higher WRQOL and friends’ risky sexual behaviors were significant RSB correlates. Controlling for baseline HIV-risk, significant concurrent correlates of surgical HIV-risk at 48-months included friends’ risky sexual behavior, with marginal significance for past-year alcohol use and illicit drug use (ps=.05). No significant correlates for HIV-risk were identified for nonsurgical.
DISCUSSION
The majority of females experienced sexual debut during the 4-year study window (i.e. for surgical females, post-operatively) at an age consistent with age-normative trends (≈ 17 years) and with an increase in “past-year” sexual risk behaviors over time.1,2 However, when considering a broader set of lifetime health risk behaviors known to confer greater risk for acquiring HIV or any STI (i.e., lifetime “HIV-risk” score), surgical females demonstrated a significant surge in risk behavior engagement relative to nonsurgical. Recognizing that STI/HIV diagnostic testing practices are unknown, self-reported lifetime STI history 200 at 48 months were similar, yet notable (i.e., @ 1 in 6 surgical vs. 1 in 7 nonsurgical reported at least one STI).
Important group discrepancies were found in pregnancy and parity outcomes. During the first 4 post-operative years, approximately 1 in 4 surgical females reported a pregnancy relative to 1 in 12 nonsurgical, with a total of 16 live births occurring among 15 surgical females (19%) relative to 1 live birth for nonsurgical (2%). Comparisons of these numbers to national statistics prove challenging given differences in reporting metrics. However, to estimate a national statistic for live births across this approximate age range and time period, we computed a weighted average based on the total reported births for females ages 15–24 years in the United States divided by the total number of women in that age range for each year (2012–2016)41 and multiplied by 4 years (i.e., length of study period), resulting in a live birth rate estimate of 21%. Recognizing this is an estimate, this highlights what appear to be lower than age-normative numbers for nonsurgical females as opposed to inordinately higher risks for surgical females post-operatively. The intentionality of pregnancies is unknown and relevant given associated risks (i.e., low birth weight, less likely to be breast-fed or receive early prenatal care42). Understanding the potential role of enhanced fertility and contraception efficacy in adolescents following surgical weight loss as well as maternal and perinatal outcomes are crucial. Nevertheless, 50% of the surgical group’s offspring (9 of 18; 2 pre-operatively, 7 post-operatively) were the result of teen child-bearing, a known risk to long-term health, education, and economic outcomes for mother and child.43
Condom and/or contraception use was concerning, yet similar to national statistics. National surveillance (i.e., NSFG31) reported partner condom use at last sexual intercourse (alone or in combination with other contraception) at 56.8% for female adolescents (ages 15–19) and 33.7% young adults (ages 20–24) (surgical: 50%; nonsurgical: 44%). More positively, use of dual protection methods (condom in combination with one other method) appeared higher for surgical (36%) and nonsurgical females (32%) than NSFG statistics (adolescent: 26.6%; young adult: 16%). Nonetheless, this snapshot (i.e., most recent sexual encounter) illustrates potential risks, echoed by many (≈25–50%) who acknowledged limited confidence in their pregnancy and STI prevention practices.
Developmental science demonstrates numerous contributors to sexual risk engagement across the adolescent/young adult transition (i.e., history of abuse, family dysfunction, psychopathology), none of which explained risks in female sexual behavior post-operatively. Moreover, neither weight lost nor WRQOL outcomes were potent explanatory factors for the surgical sample. Rather, behaviors and contexts characterized as risky (i.e., risky sex, affiliation with risky peers, alcohol and illicit drug use, sensation-seeking) co-occurred post-operatively in a “risk-taking subgroup”. While statistical power limits mechanistic model testing, post hoc descriptive examination of risk-taking parameters by post-operative weight status (BMI endpoint versus amount of weight loss) offer directions for future research. Surgical females achieving overweight status at 48-months (BMI<30kg/m2, n=9) reported higher HIV-risk (M=4.00±2.18), RSB (M=5.67±4.12), and alcohol (89%) and illicit drug (44%) use in the past year, relative to surgical females with a 48-month BMI outcome ≥30kg/m2 (MHIV=3.11±2.26; MRSB=4.15±3.65, alcohol: 72%; illicit drug: 37%) and to nonsurgical females (MHIV=2.22±2.23; MRSB=3.47±3.80, alcohol: 65%; illicit drug: 43%). Perhaps when achieving optimal post-operative weight status (i.e., no longer obese), females may trade one set of risks (i.e., severe obesity) for another (i.e., risks to sexual health, substance use).
The clinical implications of these data are concerning and heightened given access to quality health care for young adults is challenging (i.e., gaps in insurance and/or a lack of a usual source of care).44 Moreover, four consecutive “best practice” guidelines published since 2005 by the Pediatric Committee of the American Association for Bariatric and Metabolic Surgery (ASMBS)45–48 only highlighted a need for reproductive counseling due to a potential increase in fertility post-operatively. The most recent 2018 update, while acknowledging “adolescent pregnancy carries its own risks”, primarily highlighted emerging adult outcome data touting that pregnancy after bariatric surgery “confers a significant health benefit for both mother and infant”.48 This sends an incomplete message to adolescent/young adult bariatric patients and providers. Missing are developmentally appropriate guidelines regarding the need for ongoing counseling on adolescents’ evolving sexual practices, including teen and unintended pregnancy, STI/HIV prevention, and the impact of substance use on sexual decision-making. Dual protection via highly efficacious pregnancy prevention methods (e.g., IUD, implant) in conjunction with STI/HIV risk reduction practices (e.g., consistent condom use, STI/HIV testing) is indicated (see Centers for Disease Control and Prevention Clinical Prevention Guidance at: https://www.cdc.gov/STI/tg2015/clinical.htm). At a minimum, pediatric bariatric providers should actively refer to adjunctive women/teen health care sources as part of standard clinical care pathways.
Teen-LABS and associated ancillaries provide the most comprehensive prospectively collected data characterizing adolescent Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) outcomes, enhanced by ancillary inclusion of nonsurgical comparators. However, consistent with bariatric enrollment trends (2008–2012),49 participants were predominantly White, female, and underwent RYGB. Understanding whether these findings generalize to females of other race/ethnic groups is important future research given known disparities for adverse sexual health outcomes.3–5 Of note, while Teen-LABS was not designed or powered as a procedural comparative trial, post hoc analyses showed no indication that female SG (n=26) and RYGB (n=54) patients differed in RSB (SG: M=4.03±2.93; RYGB: M=4.44±3.88; p=.64) or HIV-risk (SG: M=3.04±2.31; RYGB: M=3.30±2.21; p=.63), or in the number of post-operative pregnancies (SG: 6 of 26 [23%]; RYGB: 14 of 54 [26%]; p=.78) at 48-months. Additional data including partner characteristics (e.g., STI history), frequency of specific behaviors (e.g., number of unprotected sexual encounters), STI/HIV testing practices, and other STIs or high risk sexual contact (i.e., HPV, anal sex) were not obtained. Thus, these data may underestimate the extent of sexual health risk in this patient population. Finally, sexual orientation and gender identity questions were not included, yet critically important given health disparities in the lesbian, gay, bisexual, and transgender community.50
CONCLUSIONS
Reduction of teen pregnancies and child-bearing, unintended pregnancies, and STI/HIV-risks are public health priorities for all adolescents and young adults.51 Thus, while many outcomes reported herein fell within “age-normative” ranges, their impact should not be interpreted as benign. Bariatric care for adolescent females must include ongoing education on dual protection strategies, the impact of substance use on sexual decision-making, STI/HIV prevention, and risks and consequences of teen or unintended pregnancies to optimize health and well-being for the long-term.
Highlights.
Surgical and nonsurgical females were similar in many sexual health domains.
Surgical reported greater increase in lifetime HIV-risk behaviors over time.
Surgical had higher number of pregnancies/live births and teen motherhood.
Uniquely adolescent post-operative care guidelines are indicated.
Acknowledgements:
The authors would like to acknowledge the contributions of additional TeenView Study Group Co-Investigators and staff. Cincinnati Children’s Hospital Medical Center: Faye Doland, BS, Ashley Morgenthal, BS, Taylor Howarth, BS, Sara Comstock, MA, Shelley Kirk, PhD, Michael Helmrath, MD, PhD; Texas Children’s Hospital: Margaret Callie Lee, MPH, David Allen, BS, Beth Garland, PhD, Gia Washington, PhD, Carmen Mikhail, PhD, Mary L. Brandt, MD; University of Pittsburgh Medical Center: Ronette Blake, BS, Nermeen El Nokali, PhD, Dana Rofey, PhD, Silva Arslanian, MD, Anita P. Courcoulas, MD, MPH, Children’s Hospital of Alabama University of Alabama: Krishna Desai, MD, Amy Seay, PhD, Beverly Haynes, BSN, Heather Austin, PhD, Carroll Harmon, MD, PhD; Nationwide Children’s Hospital Medical Center: Melissa Ginn, BS, Amy E. Baughcum, PhD, Marc P. Michalsky, MD; Teen-LABS Data Coordinating Center: Michelle Starkey Christian, Jennifer Andringa, BS, Carolyn Powers, RD, Rachel Akers, MPH.
Funding source: The TeenView ancillary studies (R01DK080020 and R01DA033415; PI: Zeller) were conducted in collaboration with the Teen-LABS Consortium. Teen-LABS was funded by cooperative agreements with the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), through grants: U01DK072493, UM1DK072493, and UM1DK095710 (University of Cincinnati). Dr. Black’s effort was supported by an NIH post-doctoral training grant (T32 DK063929).
Financial Disclosure: Thomas H. Inge has served as a consultant for Zafgen Corporation, Biomedical Insights, and L&E Research, and received honoraria from Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services, all unrelated to this project. Anita P. Courcoulas has received research grants from Allurion Inc. David B. Sarwer has served as consultant for BARONova, Merz, and NovoNordisk.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: All authors have indicated they have no relationships relevant to this article to disclose.
References
- 1.Finer LB, Philbin JM. Trends in ages at key reproductive transitions in the United States, 1951–2010. Women’s Healt Health Issues 2014;24(3):e271–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fergus S, Zimmerman MA, Caldwell CH. Growth trajectories of sexual 310 risk behavior in adolescence and young adulthood. Am J Public Health 2007;97(6):1096–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med 2016;374(9):843–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 315 2017 Atlanta: US Department of Health and Human Services; 2018. [Google Scholar]
- 5.Centers for Disease Control and Prevention. HIV Surveillance Report, 2016 Vol 28: Available at: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html; November 2017. Accessed Februrary 2, 2018. [Google Scholar]
- 6.Steinberg L A dual systems model of adolescent risk-taking. Developmental 320 Psychobiology 2010;52(3):216–224. [DOI] [PubMed] [Google Scholar]
- 7.Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across the life course. Annu Rev Sociol 2010;36:139–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akers AY, Cohen ED, Marshal MP, Roebuck G, Yu L, Hipwell AE. Objective and perceived weight: associations with risky adolescent sexual behavior. Perspect Sex 325 Reprod Health 2016;48(3):129–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang T, Davis MM, Kusunoki Y, Ela EJ, Hall KS, Barber JS. Sexual behavior and contraceptive use among 18-to 19-year-old adolescent women by weight status: A longitudinal analysis. J Pediatr 2015;167(3):586–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ratcliff MB, Jenkins TM, Reiter-Purtill J, Noll JG, Zeller MH. Risk-taking behaviors of 330 adolescents with extreme obesity: Normative or not? Pediatrics 2011;127(5):827–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Becnel JN, Zeller MH, Noll JG, et al. Romantic, sexual, and sexual risk behaviours of adolescent females with severe obesity. Pediatric Obesity 2017;12(5):388–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kolotkin RL, Crosby RD, Gress RE, Hunt SC, Engel SG, Adam TD. Health and healthrelated quality of life: differences between men and women who seek gastric bypass surgery. Surg Obes Relat Dis 2008;4:651–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarwer DB, Spitzer JC, Wadden TA, et al. Changes in sexual functioning and sex hormone levels in women following bariatric surgery. JAMA Surg 2014;149(1):26–33. [DOI] [PubMed] [Google Scholar]
- 14.Sarwer DB, Wadden TA, Spitzer JC, et al. 4-year changes in sex hormones, sexual functioning, and psychosocial status in women who underwent bariatric surgery. Obes Surg 2018;28(4):892–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conason A, McClure Brenchley KJ, Pratt A, Geliebter A. Sexual life after weight loss surgery. Surg Obes Relat Dis 2017;13(5):855–861. [DOI] [PubMed] [Google Scholar]
- 16.Menke MN, King WC, White GE, et al. Contraception and conception after bariatric surgery. Obstetrics and Gynecology 2017;130(5):979–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steffen KJ, King WC, White GE, et al. Sexual functioning of men and women with severe obesity before bariatric surgery. Surg Obes Relat Dis 2017;13(2):334–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merhi ZO. Impact of bariatric surgery on female reproduction. Fertility and Sterility 2009;92(5):1501–1508. [DOI] [PubMed] [Google Scholar]
- 19.Charnigo R, Noar SM, Garnett C, Crosby R, Palmgreen P, Zimmerman RS. Sensation seeking and impulsivity: combined associations with risky sexual behavior in a large sample of young adults. Journal of Sex Research 2013;50(5):480–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gowey MA, Reiter-Purtill J, Becnel J, et al. Weight-related correlates of psychological dysregulation in adolescent and young adult (AYA) females with severe obesity. Appetite 2016;99:211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dishion TJ, Ha T, Veronneau MH. An ecological analysis of the effects of deviant peer clustering on sexual promiscuity, problem behavior, and childbearing from early adolescence to adulthood: an enhancement of the life history framework. Dev Psychol 2012;48(3):703–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Connell CM, Gilreath TD, Hansen NB. A multiprocess latent class analysis of the co-occurrence of substance use and sexual risk behavior among adolescents. J Stud Alcohol Drugs 2009;70(6):943–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zeller MH, Washington GA, Mitchell JE, et al. Alcohol use risk in adolescents 2 years after bariatric surgery. Surg Obes Relat Dis 2017;13(1):85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lansford JE, Dodge KA, Fontaine RG, Bates JE, Pettit GS. Peer rejection, affiliation with deviant peers, delinquency, and risky sexual behavior. J Youth Adolesc 2014;43(10):1742–1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hunsaker S, Garland B, Rofey D, et al. Prevalence and correlates of psychopathology among adolescents who did or did not undergo weight loss surgery. Journal of Adolecent Health 2018;63(2):142–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zeller MH, Hunsaker S, Mikhail C, et al. Family factors that characterize adolescents with severe obesity and their role in weight loss surgery outcomes. Obesity 2016;24(12):2562–2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Noll JG, Guastaferro K, Beal SJ, et al. Is Sexual Abuse a Unique Predictor of Sexual Risk Behaviors, Pregnancy, and Motherhood in Adolescence? Journal of Research on Adolescence 2018. July 18. doi: 10.1111/jora.12436. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zeller MH, Noll JG, Sarwer DB, et al. Child Maltreatment and the Adolescent Patient With Severe Obesity: Implications for Clinical Care. J Pediatr Psychol 2015;40(7):640–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Inge TH, Courcoulas AP, Jenkins TM, et al. Weight Loss and Health Status 3 Years after Bariatric Surgery in Adolescents. N Engl J Med 2016;374(2):113–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Noll JG, Trickett PK, Putnam FW. A prospective investigation of the impact of childhood sexual abuse on the development of sexuality. Journal of Consulting & Clinical Psychology 2003;71(3):575–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Copen CE. Condom Use During Sexual Intercourse Among Women and Men Aged 15–44 in the United States: 2011–2015 National Survey of Family Growth. National Health Statistics Reports 2017(105):1–18. [PubMed] [Google Scholar]
- 32.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl 2003;27(2):169–190. [DOI] [PubMed] [Google Scholar]
- 33.Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms & Profiles Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- 34.Kolotkin RL, Zeller MH, Modi AC, et al. Assessing weight-related quality of life in adolescents. Obesity 2006;14(3):448–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Epstein N, Baldwin L, Bishop D. The McMaster Family Assessment Device. Journal of Marital and Family Therapy 1983;9(2):171–180. [Google Scholar]
- 36.Achenbach TMR LA . Manual for the ASEBA Adult Forms & Profiles Burlington, VT: University of Vermont, Research Center for Children, Youth , & Families; 2003. [Google Scholar]
- 37.Kolotkin RL, Crosby RD, Kosloski KD, Williams GR. Development of a brief measure to assess quality of life in obesity. Obes Res 2001;9:102–111. [DOI] [PubMed] [Google Scholar]
- 38.Steinberg L, Albert D, Cauffman E, Banich M, Graham S, Woolard J. Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: Evidence for a dual systems model. Developmental Psychology 2008;44(6):1764–1778. [DOI] [PubMed] [Google Scholar]
- 39.Mezzich AC, Tarter RE, Giancola PR, Kirisci L. The Dysregulation Inventory: A new scale to assess the risk for substance use disorder. Journal of Child 405 and Adolescent Substance Use 2001;10(4):35–43. [Google Scholar]
- 40.Johnston L, O’Malley P, Bachman J, Schulenberg J. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2010 Ann Arbor: Institute for Social Research, The University of Michigan; 2011. [Google Scholar]
- 41.National Center for Health Statistics. User guide to the 2012–2016 natality public use file Hyattsville, MD: National Center for Health Statistics; Published annually:https://www.cdc.gov/nchs/data_access/vitalstatsonline.htm. [Google Scholar]
- 42.Kost K, Lindberg L. Pregnancy intentions, maternal behaviors, and infant health: investigating relationships with new measures and propensity score analysis. Demography 2015;52(1):83–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hoffman S Counting it up: The public costs of teen childbearing 2013; https://powertodecide.org/sites/default/files/resources/primary-download/counting-it-upkey-data-2013.pdf.
- 44.Lau JS, Adams SH, Irwin CE Jr., Ozer EM. Receipt of preventive health services in young adults. J Adolesc Health 2013;52(1):42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Apovian CM, Baker C, Ludwig DS, et al. Best practice guidelines in pediatric/adolescent weight loss surgery. Obesity Research 2005;13(2):274–282. [DOI] [PubMed] [Google Scholar]
- 46.Pratt JSA, Lenders CM, Dionne EA, et al. Best Practice Updates for Pediatric/Adolescent Weight Loss Surgery. Obesity 2009;17(5):901–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Michalsky M, Reichard K, Inge T, et al. ASMBS pediatric committee best practice guidelines. Surg Obes Relat Dis 2012;8(1):1–7. [DOI] [PubMed] [Google Scholar]
- 48.Pratt JSA, Browne A, Browne NT, et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis 2018;14(7):882–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Griggs CL, Perez NP Jr, Goldstone RN, et al. National trends in the use of metabolic and bariatric surgery among pediatric patients with severe obesity. JAMA Pediatrics 2018. October 22. doi: 10.1001/jamapediatrics.2018.3030. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Herbst JH, Jacobs ED, Finlayson TJ, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS and Behavior 2008;12(1):1–17. [DOI] [PubMed] [Google Scholar]
- 51.U.S. Department of Health and Human Services. 2020 LHI Topics 2011; https://www.healthypeople.gov/2020/leading-health-indicators/2020-LHI-Topics. Accessed September 13, 2018.


