Abstract
Several studies demonstrated that visit-to-visit variability of blood pressure (BP) predicted future events of total death, stroke and cardiovascular disease. Little is known about factors associated with visit-to-visit BP variability in different countries. We recruited participants aged 40–59 years from four countries (Japan, the People’s Republic of China [PRC], the United Kingdom [UK] and the United States [US]). At each study visit, BP was measured twice by trained observers using random zero sphygmomanometers after five minutes resting. We defined visit-to-visit BP variability as variation independent of mean (VIM) by using average systolic BP of 1st and 2nd measurement across four study visits. Data on 4680 men and women were analyzed. Mean ± standard deviation of VIM values among participants in Japan, the PRC, the UK and the US were 5.44 ± 2.88, 6.85 ± 3.49, 5.65 ± 2.81 and 5.84 ± 3.01, respectively; VIM value in the PRC participants was significantly higher. Sensitivity analyses among participants without antihypertensive treatment or past history of cardiovascular disease yielded similar results. Higher VIM value was associated with older age, female gender, lower pulse rate and urinary sodium excretion and use of antihypertensive agents such as angiotensin converting enzyme inhibitors, beta blockers and calcium channel blockers. The difference of visit-to-visit BP variability between PRC and other countries remained significant after adjustment for possible confounding factors. In this large international study across four countries, visit-to-visit BP variability in the PRC was higher than in the other three countries. Reproducibility and mechanisms of these findings remain to be elucidated.
Numerous cohort studies have reported that blood pressure (BP) predicts long-term future cardiovascular events [1–3], dementia [4] and disability [5]. Recent studies including meta-analyses indicate that visit-to-visit BP variability may also be an important risk factor for total mortality [6–8], cardiovascular diseases (CVD) [7–13], coronary heart disease [7–9, 13], stroke [8, 14], diabetic nephropathy [15], and dementia [16]. Most of these studies were based in populations carrying a high risk of CVD, and similar observations were reported in studies based on general and/or elderly populations [6, 8, 13, 14]. Recent studies have suggested that BP variability is a causal factor for atherosclerosis [17, 18] and diastolic function [17]. However, no studies compared visit-to-visit BP variability across Western and Asian countries, and little is known about race/ethnicity or differences in visit-to-visit BP variability between countries. Moreover, few studies have reported the factors associated with visit-to-visit BP variability [6, 19].
We therefore examined the distribution of visit-to-visit BP variability among middle aged men and women in Japan, the People’s Republic of China (PRC), the United Kingdom (UK) and the United States (US), from the International Collaborative Study of Macronutrients, Micronutrients and Blood Pressure (INTERMAP) [20, 21], conducted with a highly standardized study protocol including BP measurements.
Methods
The INTERMAP study methods have been reported in detail [20, 21]. Briefly, INTERMAP surveyed 4680 men and women aged 40–59, from 17 population samples in Japan, the PRC, the UK and the US (1996–1999). Participants were selected randomly from communities or work-places. Participants visited study centers four times, with visits one and two on consecutive days, and visits three and four on consecutive days an average three weeks later. Trained staff measured BP twice per visit with a random-zero sphygmomanometer. Pulse was measured three times per visit. Height and weight were measured at the first and third visit. Each participant provided two 24-h urine collections with start and end times recorded by research staff. Twenty-four hour urinary excretions of sodium and potassium were means of two measurements. In the present study, four participants were excluded due to missing values of outside temperature. Thus, 4676 participants without missing values were included in this analysis. The study received institutional ethics committee approval for each site, and all participants gave written informed consent. The mean participation rate was 49%.
We defined within-individual visit-to-visit BP variability as variation independent of mean (VIM) of systolic BP since coefficient of variation is correlated with mean BP. VIM was derived from standard deviation(SD)/meanx where the value of x was estimated from non-linear regression analysis for all individuals by the PROC NLIN procedure of SAS [20, 21]. With respect to the primary analysis, VIM of average BP by using average systolic BP of 1st and 2nd measurements across four study visits was calculated. With regard to the secondary analysis, we also calculated VIM of 1st and 2nd BP measurements by using systolic BP of 1st measurement and systolic BP of 2nd measurement across four study visits, respectively. We additionally calculated VIM of BP of all measurements by using BP of all measurements (eight). Finally, we calculated coefficient of variation (CV) of BP by using average systolic BP of 1st and 2nd measurements across four study visits.
Analysis of variance for continuous variables or chi-square tests for proportions were used for comparing baseline characteristics. The associations between VIMs of BP and participant characteristics were assessed using multiple linear regression analysis. Participants from Japan were defined as reference group. We also examined the associations stratified by countries as sensitivity analyses. Characteristics included BMI, smoking status (never, past, current), drinking status (never, past, moderate [<300 g alcohol intake per week], heavy [≥300 g alcohol intake per week]), pulse, mean inside and outside temperature (Celsius) across four study visits, family history of high blood pressure, number of hours of moderate and heavy physical activity per day, 24-h urinary sodium and potassium excretion (mean of two 24-h urine collections), past history of CVD and treatment of hypertension (angiotensin converting enzyme [ACE] inhibitors, angiotensin II receptor blockers, beta blockers, calcium channel blockers, diuretics, direct vasodilators and others). The initial regression models (model 1) included age, sex, country, and study center. Subsequent models of association between BP variability and participant characteristics included variables in model 1 plus pulse, outside temperature, urinary potassium and sodium excretions, past history of CVD and anti-hypertensive medication drug class (model 2). In sensitivity analyses, we excluded participants with past history of CVD and/or antihypertension medication (N = 958). Analysis of covariance (ANCOVA) was used to compare the VIMs of the four countries, with adjustment for confounding factors using the Bonferroni adjustment for multiple comparisons.
All analyses were performed with SAS 9.4 (SAS, NC) and SPSS 18.0 (IBM, NY). A two-tailed P value of equal to or less than 0.05 was considered statistically significant.
Results
Characteristics of the study populations are shown in Table 1. By design, age and proportion of men were similar across the four countries. Compared with UK and US, Japan and PRC had lower BMI, higher prevalence of smoking, higher urinary sodium excretion and lower urinary potassium excretion. Prevalence of current drinker in Japan and the UK was higher than in the other two countries, approximately 90%. Highest average systolic BP was observed among participants in the PRC and lowest systolic BP in participants in Japan. Prevalence of anti-hypertensive treatment was highest in the US and lowest in Japan. The pulse rate (PR) was higher in participants among the PRC and the US samples than the other two countries.
Table 1.
Characteristics of study participants by country: INTERMAP, 1996–1999
| Japan | PRC | UK | US | P valuea | |||||
|---|---|---|---|---|---|---|---|---|---|
| Total (n) | 1145 | 839 | 497 | 2195 | |||||
| Men (n) | 574 | (50.1) | 416 | (49.6) | 264 | (53.1) | 1103 | (50.3) | 0.627 |
| Age (years) | 49.4 | (5.3) | 49.0 | (5.8) | 49.2 | (5.6) | 49.1 | (5.4) | 0.423 |
| Body mass index (kg/sq.m) | 23.4 | (2.9) | 23.1 | (3.4) | 27.5 | (4.6) | 28.9 | (5.9) | <0.001 |
| Pulse rate | |||||||||
| Mean of 4 visits (beats/min) | 71.4 | (8.8) | 73.9 | (8.4) | 71.3 | (9.4) | 73.3 | (9.4) | <0.001 |
| 1st visit (beats/min) | 71.4 | (10.1) | 74.2 | (9.9) | 70.0 | (10.4) | 72.6 | (10.6) | <0.001 |
| 2nd visit (beats/min) | 71.5 | (9.8) | 73.6 | (9.8) | 71.5 | (10.5) | 73.8 | (11.0) | <0.001 |
| 3rd visit (beats/min) | 71.2 | (10.1) | 74.0 | (9.9) | 71.5 | (10.8) | 73.0 | (10.6) | <0.001 |
| 4th visit (beats/min) | 71.4 | (10.0) | 73.9 | (9.9) | 72.2 | (10.4) | 73.9 | (10.4) | <0.001 |
| Systolic blood pressure | |||||||||
| Mean of 4 visits (mmHg) | 117.2 | (13.8) | 121.3 | (17.4) | 120.4 | (14.6) | 118.6 | (13.9) | <0.001 |
| 1st visit (mmHg) | 119.5 | (15.5) | 124.7 | (20.3) | 123.8 | (16.6) | 120.7 | (15.8) | <0.001 |
| 2nd visit (mmHg) | 116.6 | (14.6) | 120.2 | (18.1) | 119.2 | (15.3) | 118.2 | (14.7) | <0.001 |
| 3rd visit (mmHg) | 116.5 | (14.4) | 120.8 | (18.7) | 120.2 | (15.5) | 118.1 | (14.9) | <0.001 |
| 4th visit (mmHg) | 116.3 | (14.4) | 119.3 | (17.6) | 118.3 | (14.5) | 117.3 | (14.6) | <0.001 |
| VIM of average BP across four study visits | 5.44 | (2.88) | 6.85 | (3.49) | 5.65 | (2.81) | 5.84 | (3.01) | <0.001 |
| CV of average BP across four study visits | 6.58 | (3.53) | 7.07 | (3.54) | 6.64 | (3.41) | 6.50 | (3.82) | 0.002 |
| Diastolic blood pressure | |||||||||
| Mean of 4 visits (mmHg) | 73.6 | (10.3) | 73.2 | (10.2) | 77.2 | (9.9) | 73.4 | (9.7) | <0.001 |
| 1st visit (mmHg) | 74.7 | (11.4) | 74.3 | (11.8) | 78.8 | (11.1) | 74.4 | (10.9) | <0.001 |
| 2nd visit (mmHg) | 73.5 | (11.1) | 72.7 | (11.4) | 76.7 | (10.8) | 73.1 | (10.5) | <0.001 |
| 3rd visit (mmHg) | 73.1 | (11.0) | 73.1 | (11.0) | 77.1 | (10.4) | 73.1 | (10.5) | <0.001 |
| 4th visit (mmHg) | 73.4 | (11.0) | 72.6 | (10.9) | 76.3 | (10.7) | 73.0 | (10.4) | <0.001 |
| Urinary sodium (mmol/24 h) | 198.3 | (56.2) | 227.5 | (100.3) | 145.0 | (49.1) | 162.6 | (59.4) | <0.001 |
| Urinary potassium (mmol/24 h) | 48.9 | (13.6) | 38.3 | (12.7) | 68.2 | (20.1) | 57.7 | (20.9) | <0.001 |
| Drinking status | |||||||||
| Heavy drinker (n) | 236 | (20.6) | 78 | (9.3) | 63 | (12.6) | 98 | (4.5) | <0.001 |
| Moderate drinker (n) | 803 | (70.1) | 304 | (36.2) | 377 | (75.9) | 1435 | (65.4) | |
| Ex-drinker (n) | 26 | (2.3) | 41 | (4.9) | 24 | (4.8) | 427 | (19.5) | |
| Nondrinker (n) | 80 | (7.0) | 416 | (49.6) | 33 | (6.6) | 235 | (10.7) | |
| Smoking status | |||||||||
| Smoker (n) | 346 | (30.2) | 305 | (36.4) | 87 | (17.4) | 369 | (16.8) | <0.001 |
| Ex-smoker (n) | 157 | (13.7) | 69 | (8.2) | 146 | (29.4) | 677 | (30.8) | |
| Non-smoker (n) | 642 | (56.1) | 465 | (55.4) | 264 | (53.1) | 1149 | (52.3) | |
| Mean inside temperature (°C) | 22.5 | (3.3) | 16.3 | (3.4) | 21.4 | (1.9) | 23.1 | (1.1) | <0.001 |
| Mean outside temperature (°C) | 14.5 | (6.9) | 12.3 | (5.0) | 8.6 | (4.5) | 18.8 | (9.9) | <0.001 |
| Physical activity (hours/week)a | 2.6 | (3.6) | 6.0 | (3.8) | 2.2 | (2.4) | 3.2 | (3.2) | <0.001 |
| Year of education | |||||||||
| 6 years or less | 0 | (0.0) | 580 | (69.1) | 6 | (1.2) | 17 | (0.8) | <0.001 |
| 12 years or less | 894 | (78.1) | 257 | (30.6) | 267 | (53.7) | 522 | (23.8) | |
| More than 13 year | 251 | (21.9) | 2 | (0.2) | 224 | (45.1) | 1656 | (75.4) | |
| Past history of CVD (n) | 98 | (8.6) | 45 | (5.4) | 45 | (9.1) | 193 | (8.8) | 0.013 |
| Family history of HBP (n) | 528 | (46.1) | 298 | (35.5) | 241 | (48.5) | 1491 | (67.9) | <0.001 |
| Anti-hypertension drug class | |||||||||
| ACE inhibitor (n) | 20 | (1.7) | 11 | (1.3) | 26 | (5.2) | 196 | (8.9) | <0.001 |
| Angiotensin II receptor blocker (n) | 0 | (0.0) | 0 | (0.0) | 5 | (1.0) | 18 | (0.8) | 0.001 |
| Beta blocker (n) | 13 | (1.1) | 4 | (0.5) | 24 | (4.8) | 116 | (5.3) | <0.001 |
| Calcium channel blocker (n) | 50 | (4.4) | 23 | (2.7) | 16 | (3.2) | 137 | (6.2) | <0.001 |
| Diuretic (n) | 5 | (0.4) | 19 | (2.3) | 19 | (3.8) | 160 | (7.3) | <0.001 |
| Direct vasodilators (n) | 5 | (0.4) | 14 | (1.7) | 0 | (0.0) | 9 | (0.4) | <0.001 |
| Other (n) | 5 | (0.4) | 3 | (0.4) | 2 | (0.4) | 27 | (1.2) | 0.017 |
Values are number (proportion [%]) or mean (standard deviation)
Analysis of variance for continuous variables or chi-square tests for proportions. Physical activity was defined as number of hours with moderate and heavy physical activity per week
BP blood pressure, VIM variation independent of mean, CV coefficient of variation, CVD cardiovascular disease, HBP high blood pressure, PRC People’s Republic of China, UK United Kingdom, US United States
Table 2 shows the relationships between VIM of average BP across four study visits and various participant characteristics. In the age, sex and center adjusted model, older age, female gender, lower PR, past history of CVD, higher outside temperature, lower urinary sodium excretion, lower urinary potassium excretion, being PRC or the US participants and use of ACE inhibitors, beta blockers and calcium channel blockers were independently associated with higher VIM of BP. In multivariable models, older age, female gender, lower PR, lower urinary sodium excretion, being from the PRC and use of ACE inhibitors, beta blockers and calcium channel blockers were independently associated with higher VIM of BP. Being a PRC participant was independently associated with higher VIM after adjustment for these factors (P < 0.001). Similar results were found when stratified by countries (supplemental Table 2). Being PRC participant was independently associated with higher VIM after further adjustment for mean BP (data not shown).
Table 2.
Relationship between VIM of average BP across four study visits and various characteristics: INTERMAP, 1996–1999
| VIM of average BP | ||||
|---|---|---|---|---|
| Model 1 | Model 2 | |||
| Beta | P-value | Beta | P-value | |
| Age (5 years) | 0.312 | <0.001 | 0.256 | <0.001 |
| Women | 0.576 | <0.001 | 0.497 | <0.001 |
| Country | ||||
| Japan | Reference | Reference | ||
| PRC | 1.358 | <0.001 | 1.377 | <0.001 |
| UK | 0.061 | 0.817 | −0.058 | 0.836 |
| US | 0.591 | 0.017 | 0.308 | 0.230 |
| BMI | −0.014 | 0.122 | ||
| Pulse rate (10 beats/min) | −0.209 | <0.001 | −0.204 | <0.001 |
| Smoking | ||||
| Non-smoker | Reference | |||
| Ex-smoker | 0.010 | 0.934 | ||
| Smoker | 0.061 | 0.603 | ||
| Drinking | ||||
| Non-drinker | Reference | |||
| Ex-drinker | −0.187 | 0.311 | ||
| Moderate drinker | −0.118 | 0.396 | ||
| Heavy drinker | −0.222 | 0.266 | ||
| Mean inside temperature (°C) | −0.001 | 0.964 | ||
| Mean outside temperature (°C) | 0.014 | 0.036 | 0.012 | 0.086 |
| Physical activity (h/week)a | 0.002 | 0.876 | ||
| Years of education | ||||
| 6 years or less | Reference | |||
| 12 years or less | −0.009 | 0.968 | ||
| More than 13 years | 0.115 | 0.636 | ||
| Family history of hypertension | 0.126 | 0.171 | ||
| Past history of CVD | 0.498 | 0.002 | 0.287 | 0.075 |
| Urinary Sodium (20 mmol/24 h) | −0.038 | 0.011 | −0.036 | 0.022 |
| Urinary Potassium (10 mmol/24 h) | −0.051 | 0.049 | −0.033 | 0.233 |
| Antihypertensive medication drug class | ||||
| ACE inhibitor | 0.478 | 0.017 | 0.527 | 0.009 |
| Angiotensin II receptor blocker | 0.603 | 0.340 | 0.625 | 0.322 |
| Beta blocker | 0.993 | <0.001 | 0.805 | 0.001 |
| Calcium channel blocker | 0.826 | <0.001 | 0.843 | <0.001 |
| Diuretic | 0.248 | 0.281 | 0.289 | 0.207 |
| Vasodilation drug | 0.789 | 0.167 | 0.750 | 0.188 |
| Other | 1.091 | 0.028 | 1.074 | 0.030 |
The associations between VIMs of BP and participant characteristics were assessed using multiple linear regression analysis. Model 1 included adjustment for age, sex, countries and study centers. Model 2 included age, sex, countries, study centers and all variables associated with VIM of visit-to-visit BP variability (P < 0.05) in Model 1
Physical activity was defined as number of hours with moderate and heavy physical activity per week
BP blood pressure, VIM variation independent of mean, CVD cardiovascular diseases, BMI body mass index, PRC People’s Republic of Chin, UK United Kingdom, US United States, h hour, ACE angiotensin-converting-enzyme
We also examined the association between BP variability and various characteristics stratified by sex. The results were similar in men and women (Supplemental Table 4). Sensitivity analyses among participants without anti-hypertensive treatment or past history of CVD are shown in Table 3. In the age and center adjusted model, VIM of BP in PRC was significantly higher than the other countries, while further adjustment for other possible confounding factors did not affect the results (P < 0.001). In multivariable models, older age, female gender, lower PR, lower BMI and being a participant from the PRC were independently associated with higher VIM of BP.
Table 3.
Relationship between VIM of average BP across four study visits and various characteristics among participants without antihypertensive treatment or past history of CVD: INTERMAP, 1996–1999
| VIM of average BP | ||||
|---|---|---|---|---|
| Model 1 | Model 3 | |||
| Beta | P-value | Beta | P-value | |
| Age (5 years) | 0.231 | <0.001 | 0.229 | <0.001 |
| Women | 0.631 | <0.001 | 0.589 | <0.001 |
| Country | ||||
| Japan | Reference | Reference | ||
| PRC | 1.225 | <0.001 | 1.276 | <0.001 |
| UK | −0.024 | 0.931 | −0.025 | 0.931 |
| US | 0.235 | 0.392 | 0.262 | 0.365 |
| BMI (kg/sq.m) | −0.038 | 0.001 | −0.031 | 0.008 |
| Pulse (10 beats/min) | −0.145 | 0.008 | −0.122 | 0.029 |
| Smoking | ||||
| Non-smoker | Reference | |||
| Ex-smoker | −0.003 | 0.985 | ||
| Smoker | 0.075 | 0.548 | ||
| Drinking | ||||
| Non-drinker | Reference | |||
| Ex-drinker | −0.354 | 0.085 | ||
| Moderate drinker | −0.185 | 0.218 | ||
| Heavy drinker | −0.327 | 0.125 | ||
| Mean inside temperature (°C) | 0.003 | 0.919 | ||
| Mean outside temperature (°C) | 0.015 | 0.039 | 0.014 | 0.062 |
| Physical activity (h/week)a | 0.018 | 0.249 | ||
| Years of education | ||||
| 6 years or less | Reference | |||
| 12 years or less | 0.025 | 0.909 | ||
| More than 13 years | 0.174 | 0.496 | ||
| Family history of hypertension | −0.003 | 0.972 | ||
| Urinary sodium (20 mmol/24 h) | −0.035 | 0.031 | −0.022 | 0.192 |
| Urinary potassium (10 mmol/24 h) | −0.036 | 0.203 | ||
The associations between VIMs of BP and participant characteristics were assessed using multiple linear regression analysis
BP blood pressure, VIM variation independent of mean, CVD cardiovascular disease, BMI body mass index, PRC People’s Republic of China, UK United Kingdom, US United States, h hour
Physical activity was defined as number of hours with moderate and heavy physical activity per week. Model 1 included age, sex, countries and study centers. Model 3 included age, sex, countries, study centers and all variables associated with VIM of visit-to-visit BP variability (P 0.05) in Model 1
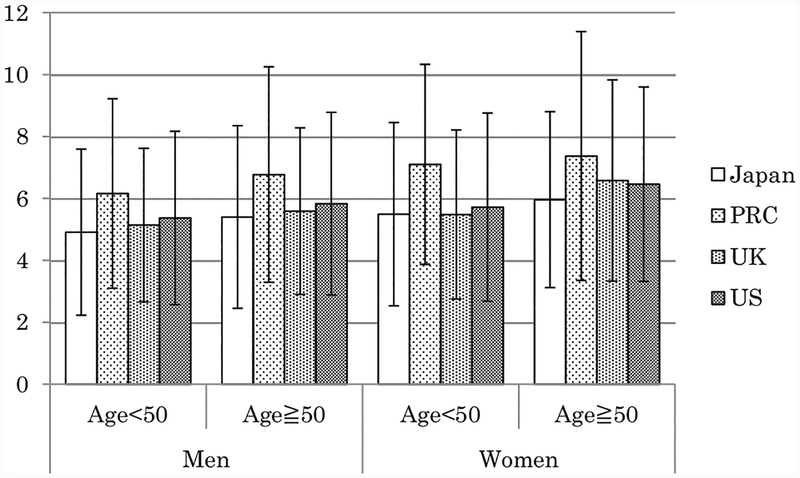
Figure 1 shows the mean and SD of VIMs of average BP across four study visits stratified by country, age and sex. VIMs of BP were higher in older age groups.
Fig. 1.
The mean and standard deviation of VIMs of average BP measurement across four study visits stratified by country, age-group and sex are shown. BP, blood pressure; VIM, variation independent of mean; PRC, People’s Republic of China; UK, United Kingdom; US, United States
Table 4 shows country-specific VIM values of BP. VIM values of visit-to-visit BP variability in the PRC (6.85 ± 3.49) were the highest among the four countries (5.44 ± 2.88 in Japan, 5.65 ± 2.81 in the UK and 5.84 ± 3.01 in the US). In multivariable adjusted models, VIM of BP in PRC remained significantly higher than that for the other countries. Further adjustment for other possible confounding factors did not affect the results. Stratified by sex, the results were similar (Supplemental Table 4).
Table 4.
VIM values of BP stratified by country: INTERMAP, 1996–1999
| Number | Japan | PRC | UK | US | ||||
|---|---|---|---|---|---|---|---|---|
| 1145 | 839 | 497 | 2195 | |||||
| VIM of average SBP of 1st and 2nd measurement across 4study visits | 5.44 | ± 2.88b | 6.85 | ± 3.49a,c | 5.65 | ± 2.81b | 5.84 | ± 3.01b |
| VIM of 1st SBP measurement across 4 study visits | 6.14 | ± 3.15b | 7.20 | ± 3.62a,c | 6.10 | ± 2.97b | 6.39 | ± 3.22b,c |
| VIM of 2nd SBP measurement across 4 study visits | 5.89 | ± 3.02b | 7.02 | ± 3.51a,c | 5.92 | ± 3.01b | 6.22 | ± 3.16b |
| VIM of SBP of all measurement (8 times) | 5.92 | ± 2.53b,c | 6.76 | ± 3.13a,c | 5.82 | ± 2.53a,b | 6.14 | ± 2.67b,c, |
Values are number or mean ± SD
ANCOAVA was used to tests for differences of VIMs of BP among countries
Adjusted for age, sex, study centers, pulse, outside temperature, urinary potassium excretion, urinary sodium excretion, past history of CVD and antihypertensive medication drug class
Significantly different from Japan (Followed by Bonferroni post hoc testing)
Significantly different from PRC (Followed by Bonferroni post hoc testing)
Significantly different from UK (Followed by Bonferroni post hoc testing)
BP blood pressure, VIM variation independent of mean, SBP systolic blood pressure, PRC People’s Republic of China, UK United Kingdom, US United States, SD standard deviation, ANCOVA analysis of covariance
Discussion
Main finding of this study was: VIM values of visit-to-visit BP variability in the PRC (6.85) was the highest among four countries (5.44 in Japan, 5.65 in UK and 5.84 in US). Visit-to-visit BP variability was higher in older, female, PRC participants and users of ACE inhibitors, beta blockers and calcium channel blockers, and was inversely associated with PR and urinary sodium excretion. The difference of visit-to-visit BP variability between PRC and the other countries remained significant after adjustment for those associated factors.
Visit-to-visit BP variability is a relatively new risk factor for total mortality [6] and CVD [7, 9–14], and differences in visit-to-visit BP variability in different countries have not been examined. To compare visit-to-visit BP variability among different regions, high standardization of BP measurements is needed. The INTERMAP study was carried out using highly standardized methods including random zero mercury manometers in all four countries [22, 23]. Participants were selected randomly from communities or workplaces. In the present study, we assessed differences in visit-to-visit variability among participants in Japan, the PRC, the UK and the US. Therefore, the INTERMAP study is suitable to investigate differences in visit-to-visit BP variability in Asian and Western regions. Japan had the lowest visit-to-visit BP variability and PRC the highest. With adjustment for possible confounding factors, visit-to-visit BP variability in the PRC was significantly higher than in the other countries. We did not find any significant association between BP variability and education, a marker of socioeconomic status.
There were few studies to report the short-term visit-to-visit BP and future events [6]. Both long-term (every several months or annually) visit-to-visit BP variability [7] and day-by-day BP variability [24] has been reported as a predictor of future morality and/or CVD events. These findings may indicate the association between short-term visit-to-visit BP variability and future CVD events. However, the evidence for short-term visit-to-visit BP variability assessed at weekly intervals is limited. Further studies are needed to clarify the association between short-term visit-to-visit BP variability and CVD.
BP variability is commonly calculated as the SD or CV of BP. However, these indices are dependent on BP levels. The VIM of BP is a relatively new index of BP variability and is independent of mean of BP [20]. Thus to avoid the confounding by BP level, we used VIM of BP as an index of BP variability in this study. Three indices of BP variability (SD, CV and VIM) are derived from the same formula (SD/meanx). Although the values of x for SD and CV are fixed (0 for SD and 1 for CV), the value of x for VIM is estimated for study population and different in different study population. Therefore, VIM values might be affected by the distribution of mean BP in the study population. In the present study, similar results were observed both for VIM and for CV of visit-to-visit BP variability indicating that our findings are not dependent on the method of variability estimation.
Previous studies reported that white coat hypertension or masked hypertension are associated with BP variability [22, 23]. These factors might influence the BP variability in different countries. Further studies are needed to clarify mechanisms, including those underlying the between-country differences.
In the present study, we found that older age and female sex were independently associated with visit-to-visit BP variability, consistent with results from previous studies [6, 19]. We did not find significant associations between visit-to-visit BP variability and smoking status and physical activity, also consistent with previous results [6].
In multivariable adjusted models, higher 24 h urinary excretion of sodium was significantly associated with lower visit-to-visit BP variability. The association was similar, but not significant, when stratified by countries. However, this inverse association was not found among participants without past history of CVD and/or hypertension medication. Therefore, the inverse association between urinary sodium excretion and visit-to-visit BP variability may be due to reverse causality. An intervention study reported that weight reduction and salt reduction did not reduce visit-to-visit BP variability of persons with high normal DBP [25].
The use of ACE inhibitor, beta blocker, and calcium channel blocker were associated with visit-to-visit BP variability, a finding consistent with a previous observational study [6]. Recent clinical trials reported the use of calcium channel blocker was associated with lower visit-to visit BP variability [26, 27]. Our result was not consistent with these recent results. The discrepancy might be due to the different characteristics of participants with or without using calcium channel blocker and/or the different combination of antihypertensive drug type.
Although we did not find a significant association between visit-to-visit BP variability and diuretic use, a previous study reported a significant association between thiazide-type diuretic and SD of visit-to-visit BP [6]. Due to lack of information about type of diuretic, we could not examine the association between visit-to-visit BP variability and loop and thiazide-type diuretic.
The present study has limitations. We used systolic BP measurements across only four study visits on average of only 3 weeks apart: i.e., only the distribution of short term visit-to-visit BP variability. Moreover, the first and second study visits, and third and fourth study visits, were on consecutive days. Previous findings on short-term visit-to-visit BP variability and day-by-day BP variability indicated that both one associated with future CVD events.
In summary, from a highly standardized international collaborative study, INTERMAP, we found that visit-to-visit BP variability in Japan was lowest and that in the PRC was highest among the four study countries.
Supplementary Material
Summary Table.
What is known about topic
Recent studies including meta-analyses indicate that visit-to-visit BP variability may also be an important risk factor for total mortality, cardiovascular diseases, coronary heart disease, stroke, diabetic nephropathy and dementia.
However, no studies compared visit-to-visit BP variability across Western and Asian countries and few studies have reported factors associated with BP variability.
What this study adds
Variation independent of mean (VIM) values of visit-to-visit BP variability was significantly higher in participants from the People’s Republic of China (PRC) than in participants from other countries.
VIM value was associated with age, gender, pulse rate and urinary sodium excretion and use of antihypertensive agents.
The difference of visit-to-visit BP variability between PRC and other countries remained significant after adjustment for these possible confounding factors.
Acknowledgements
This research was supported by Grant 2-RO1-HL50490–06 from the US National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD; by the Chicago Health Research Foundation; and by national agencies in PRC, Japan (the Ministry of Education, Science, Sports, and Culture, Grant-in-Aid for Scientific Research A090357003), and in the UK. PE is Director of the Medical Research Council-Public Health England (MRC-PHE) Center for Environment and Health and acknowledges support from the Medical Research Council and Public Health England (MR/L01341X/1). PE acknowledges support from the National Institute for Health Research (NIHR) Biomedical Research Center at Imperial College Healthcare NHS Trust and Imperial College London, and the NIHR Health Protection Research Unit in Health Impact of Environmental Hazards (HPRU-2012–10141). PE is a UK Dementia Research Institute (DRI) Professor, UK DRI at Imperial College London, funded by the MRC, Alzheimer’s Society and Alzheimer’s Research UK.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Stamler J, Stamler R, Neaton JD. Blood pressure, systolic and diastolic, and cardiovascular risks. US population data. Arch Intern Med. 1993;153:598–615. [DOI] [PubMed] [Google Scholar]
- 2.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. [DOI] [PubMed] [Google Scholar]
- 3.Takashima N, Ohkubo T, Miura K, Okamura T, Murakami Y, Fujiyoshi A, et al. Long-term risk of BP values above normal for cardiovascular mortality: a 24-year observation of Japanese aged 30 to 92 years. J Hypertens. 2012;30:2299–306. [DOI] [PubMed] [Google Scholar]
- 4.Perrotta M, Lembo G, Carnevale D. Hypertension and dementia: epidemiological and experimental evidence revealing a detrimental relationship. Int J Mol Sci. 2016;17:347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hozawa A, Okamura T, Murakami Y, Kadowaki T, Okuda N, Takashima N, et al. High blood pressure in middle age is associated with a future decline in activities of daily living. NIPPON DATA80. J Hum Hypertens. 2009;23:546–52. [DOI] [PubMed] [Google Scholar]
- 6.Muntner P, Shimbo D, Tonelli M, Reynolds K, Arnett DK, Oparil S. The relationship between visit-to-visit variability in systolic blood pressure and all-cause mortality in the general population: findings from NHANES III, 1988 to 1994. Hypertension. 2011;57:160–6. [DOI] [PubMed] [Google Scholar]
- 7.Diaz KM, Tanner RM, Falzon L, Levitan EB, Reynolds K, Shimbo D, et al. Visit-to-visit variability of blood pressure and cardiovascular disease and all-cause mortality: A systematic review and meta-analysis. Hypertension. 2014;64:965–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muntner P, Whittle J, Lynch AI, Colantonio LD, Simpson LM, Einhorn PT, et al. Visit-to-visit variability of blood pressure and coronary heart disease, stroke, heart failure, and mortality: a cohort study. Ann Intern Med. 2015;163:329–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlof B, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905. [DOI] [PubMed] [Google Scholar]
- 10.Eguchi K, Hoshide S, Schwartz JE, Shimada K, Kario K. Visit-to-visit and ambulatory blood pressure variability as predictors of incident cardiovascular events in patients with hypertension. Am J Hypertens. 2012;25:962–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mancia G, Facchetti R, Parati G, Zanchetti A. Visit-to-visit blood pressure variability, carotid atherosclerosis, and cardiovascular events in the European Lacidipine Study on Atherosclerosis. Circulation. 2012;126:569–78. [DOI] [PubMed] [Google Scholar]
- 12.Rossignol P, Cridlig J, Lehert P, Kessler M, Zannad F. Visit-to-visit blood pressure variability is a strong predictor of cardiovascular events in hemodialysis: insights from FOSIDIAL. Hypertension. 2012;60:339–46. [DOI] [PubMed] [Google Scholar]
- 13.Suchy-Dicey AM, Wallace ER, SVE M, Aguilar M, Gottesman RF, Rice K, et al. Blood pressure variability and the risk of all-cause mortality, incident myocardial infarction, and incident stroke in the cardiovascular health study. Am J Hypertens. 2013;26:1210–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shimbo D, Newman JD, Aragaki AK, Lamonte MJ, Bavry AA, Allison M, et al. Association between annual visit-to-visit blood pressure variability and stroke in postmenopausal women: data from the Women’s Health Initiative. Hypertension. 2012;60:625–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okada H, Fukui M, Tanaka M, Matsumoto S, Mineoka Y, Nakanishi N, et al. Visit-to-visit blood pressure variability is a novel risk factor for the development and progression of diabetic nephropathy in patients with type 2 diabetes. Diabetes Care. 2013;36:1908–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lattanzi S, Luzzi S, Provinciali L, Silvestrini M. Blood pressure variability in Alzheimer’s disease and frontotemporal dementia: the effect on the rate of cognitive decline. J Alzheimers Dis. 2015;45:387–94. [DOI] [PubMed] [Google Scholar]
- 17.Okada R, Okada A, Okada T, Nanasato M, Wakai K. Visit-to-visit blood pressure variability is a marker of cardiac diastolic function and carotid atherosclerosis. BMC Cardiovasc Disord. 2014;14:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hisamatsu T, Miura K, Ohkubo T, Arima H, Fujiyoshi A, Satoh A, et al. Home blood pressure variability and subclinical atherosclerosis in multiple vascular beds: a population-based study. J. Hypertens 2018;36:2193–2203. [DOI] [PubMed] [Google Scholar]
- 19.Shin JH, Shin J, Kim BK, Lim YH, Park HC, Choi SI, et al. Within-visit blood pressure variability: relevant factors in the general population. J Hum Hypertens. 2013;27:328–34. [DOI] [PubMed] [Google Scholar]
- 20.Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlof B, et al. Effects of beta blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol. 2010;9:469–80. [DOI] [PubMed] [Google Scholar]
- 21.Asayama K, Kikuya M, Schutte R, Thijs L, Hosaka M, Satoh M, et al. Home blood pressure variability as cardiovascular risk factor in the population of Ohasama. Hypertension. 2013;61:61–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stamler J, Elliott P, Appel L, Chan Q, Buzzard M, Dennis B, et al. Higher blood pressure in middle-aged American adults with less education-role of multiple dietary factors: the INTERMAP study. J Hum Hypertens. 2003;17:655–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dennis B, Stamler J, Buzzard M, Conway R, Elliott P, Moag-Stahlberg A, et al. INTERMAP: the dietary data--process and quality control. J Hum Hypertens. 2003;17:609–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Juhanoja EP, Niiranen TJ, Johansson JK, Puukka PJ, Thijs L, Asayama K, et al. Outcome-driven thresholds for increased home blood pressure variability. Hypertension. 2017;69:599–607. [DOI] [PubMed] [Google Scholar]
- 25.Diaz KM, Muntner P, Levitan EB, Brown MD, Babbitt DM, Shimbo D. The effects of weight loss and salt reduction on visit-to-visit blood pressure variability: results from a multicenter randomized controlled trial. J Hypertens. 2014;32:840–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith TR, Drozda JP Jr., Vanslette JA, Hoeffken AS, Nicholson RA. Medication class effects on visit-to-visit variability of blood pressure measurements: analysis of electronic health record data in the “real world”. J Clin Hypertens. 2013;15:655–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kollias A, Stergiou GS, Kyriakoulis KG, Bilo G, Parati G. Treating visit-to-visit blood pressure variability to improve prognosis: is amlodipine the drug of choice? Hypertension. 2017;70:862–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.