Abstract
Objective:
The study sought to describe a Canadian sample of university students’ medicinal use of cannabis, including prevalence of cannabis use disorder (CUD) and replacement of traditional treatments with cannabis.
Method:
A random sample of 4000 university students was asked to complete a cross-sectional web-based survey. The survey was completed by 2212 (average age 23.2 years, SD = 5.2 years), representing a 55.3% response rate. To be eligible, students had to be enrolled in a class on campus and were 18 years or older.
Result:
Half (52%) of respondents used cannabis at least once in their lifetime, with ∼11% reporting medicinal cannabis use. Recreational motives to use cannabis were common among medicinal users (85%), several (38%) replaced traditional medication with cannabis, and more than a third received authorization by a health care provider. Of the medicinal users, 13.6% met the criteria for CUD. Common ailments for medicinal cannabis use were anxiety, sleep problems, depression, and pain. When mental health–related categories are combined, 78.2% of medicinal users used for at least 1 mental health condition.
Conclusions:
Medicinal cannabis use occurs among university students. None of the ailments listed by medicinal users meet the Canadian Family Physicians prescribing guidelines, and most are not among those viewed by the National Academies of Science, Engineering, and Medicine as having strong evidence for therapeutic value. The results raise concerns for health care providers who are authorizing or counselling patients’ considering medicinal cannabis.
Keywords: cannabis, marijuana motives, medicinal cannabis use, cannabis prescription guidelines, postsecondary students, emerging adults
Abstract
Objectif:
L’étude visait à décrire l’utilisation de cannabis à des fins médicales dans un échantillon canadien d’étudiants universitaires, y compris la prévalence du trouble d’utilisation du cannabis (TUC) et le remplacement des traitements traditionnels par du cannabis.
Méthode:
On a demandé à un échantillon aléatoire de 4 000 étudiants universitaires de répondre à un sondage transversal en ligne, et 2 212 personnes (âge moyen 23,2, ET = 5,2) y ont répondu, ce qui représente un taux de réponse de 55,3%. Pour être admissibles, les étudiants devaient être inscrits à un cours sur le campus et devaient être âgés de 18 ans et plus.
Résultat:
La moitié (52%) des répondants avaient utilisé du cannabis au moins une fois de durée de vie, et ∼11% déclaraient utiliser du cannabis à des fins médicales. Les motifs récréationnels d’utiliser du cannabis étaient répandus chez les utilisateurs à des fins médicales (85%), plusieurs (38%) remplaçaient des médicaments traditionnels par du cannabis, et plus d’un tiers obtenaient l’autorisation d’un prestataire de soins de santé. Parmi les utilisateurs à des fins médicales, 13,6% satisfaisaient aux critères du TUC. Les maux les plus communs pour justifier l’utilisation du cannabis à des fins médicales étaient l’anxiété, les problèmes de sommeil, la dépression et la douleur. Quand les catégories liées à la santé mentale sont combinées, 78,2% des utilisateurs à des fins médicales s’en servent pour au moins une affection de santé mentale.
Conclusions:
L’utilisation du cannabis à des fins médicales a cours chez les étudiants universitaires. Aucun des maux énumérés par les utilisateurs à des fins médicales ne satisfait aux lignes directrices en matière de prescription des Médecins de famille canadiens, et la plupart ne sont pas des maux que les Académies nationales des sciences, de l’ingénierie et de la médecine considèrent présenter des preuves suffisantes pour une valeur thérapeutique. Les résultats soulèvent des préoccupations pour les prestataires de soins de santé qui autorisent ou conseillent les patients qui envisagent d’utiliser du cannabis à des fins médicales.
The number of registered medicinal cannabis users in Canada has more than tripled since 2016.1 The medicinal cannabis market has become increasingly competitive, with medicinal dispensaries promoting cannabis for an array of medical ailments ranging from mental illnesses to physical conditions.2 Although dispensaries promote cannabis as a panacea for numerous disorders, the scientific evidence supporting its efficacy is often overstated or insufficient, and use has been associated with adverse outcomes.3,4 Recently, the Canadian clinical practice guidelines5 and National Academies of Science, Engineering, and Medicine in the United States6 recommended limiting medicinal cannabis to a narrow subset of medical conditions, including palliative and neuropathic pain, chemotherapy-induced nausea and vomiting, and spasticity due to multiple sclerosis.
Although general authorization guidelines have been proposed, little is known about how medicinal cannabis use may differ among subpopulations, including emerging adults (18-25 years of age). Emerging adults have historically demonstrated higher estimates of cannabis use when compared to other age groups.7 Society’s changing beliefs about cannabis use and its legal status are having an impact on young people’s decision making, including declining perceptions that cannabis use is harmful.8 Recognizing cannabis as a valid treatment for illness management may be downplaying the potential risks associated with use.9 Despite cannabis representing a treatment for some conditions, there is an inherent risk with use among this age group given the potential impact of cannabinoids on the developing brain and potential increases in the risk for mental health conditions.10,11 To better understand cannabis use among emerging adults, the current study investigated medicinal use among a Canadian university sample, a group, by virtue of their age, is at an elevated risk for cannabis use.
Materials and Methods
In March 2018, a random sample of 4000 University of Calgary (Alberta, Canada) students were invited via email to participate in UCalgary’s Campus Experience with Cannabis, a 15- to 25-minute online survey. The current study represents a subset of the findings from the survey. A simple random sample method was employed, where each student included in the sampling frame had an equal opportunity of being included in the study. The sampling frame from which the sample was drawn was provided by the University of Calgary’s Registrar’s Office and included all graduate and undergraduate students older than 18 years enrolled in at least 1 class (including international students). Participants were provided with a written informed consent prior to starting the survey. A $10 honorarium was offered for participation. The study was approved by the University of Calgary’s Conjoint Health Research Ethics Board (REB18-0184). Following the protocol as described by Dillman and colleagues,12 a total of 4 reminders spaced 1 week apart were sent via email yielding a final sample of 2212 participants (55.3% response rate). Given the study’s exploratory objective, descriptive statistics were calculated using SPSS version 25 (SPSS, Inc., an IBM Company, Chicago, IL).
Measures
Recreational use
Recreational use was a composite variable consisting of 2 motives from the Marijuana Motives Measure13 (MMM). Participants who endorsed “never or almost never” to using cannabis to “get high and to have fun” were coded as nonrecreational users. Those who endorsed using cannabis at least “some of the time” to “get high or to have fun” were coded as recreational users.
Medicinal cannabis use
Participants were asked if they had ever used cannabis for medicinal purposes. If so, they were asked to report the frequency of their medicinal use (i.e., no use in the past 6 months, monthly or less, 2-4 times a month, 2-3 times a week, or 4 or more times a week). In addition, respondents were asked if they had been prescribed cannabis by a health care practitioner (yes/no), if they had used cannabis to replace a previously prescribed medication (yes/no), and what physical or mental health–related issues were they using cannabis for via an open-ended item.
Cannabis use disorder: Cannabis Use Disorder Identification Test–Revised
For those reporting cannabis use during the prior 6 months, criteria for cannabis use disorder (CUD) was assessed by the 8-item Cannabis Use Disorder Identification Test–Revised (CUDIT-R),14 where scores greater than 12 are indicative of CUD.
Results
Table 1 describes the sample’s demographics, lifetime cannabis use, and motives for use. More than half used cannabis at least once in their lifetime. Regarding motives, 56% used only recreationally, 18.1% used both medicinally and recreationally, 3% were medicinal only, and 23.2% did not endorse the criteria for either motive. In total, 21.1% of lifetime users reported medicinal cannabis use and 74.1% reported recreational use.
Table 1.
Demographics, Lifetime Cannabis Use, and Medicinal and Recreational Motives.
| Variable | No. (%) |
|---|---|
| Female | 1259 (57.1) |
| Undergraduate student | 1789 (81.2) |
| Living in residence | 159 (7.2) |
| Varsity athlete | 66 (3.0) |
| Lifetime cannabis use | 1143 (52.3) |
| Motives | |
| Recreational use only | 633 (56.0) |
| Both medicinal and recreational use | 206 (18.1) |
| Medicinal use only | 34 (3.0) |
| Neither motive endorsed | 263 (23.2) |
| Age, mean (SD), y | 23.2 (5.2) |
The percentages provided are for valid responses only as not all participants provided responses each time. When only lifetime medicinal users are considered, 85% endorsed both medicinal and recreational use.
In Table 2, medicinal cannabis users are described with respect to frequency of medicinal cannabis use, authorization of medicinal cannabis by a health care provider, replacement of traditional treatment with cannabis, and CUD.
Table 2.
Description of Lifetime Medicinal Cannabis Users (n = 240).
| Variable | No. (%) |
|---|---|
| Frequency of medicinal use | |
| Not used in past 6 months | 36 (15.0) |
| Monthly or less | 70 (29.2) |
| 2-4 times a month | 43 (17.9) |
| 2-3 times a week | 38 (15.8) |
| 4 or more times a week | 53 (22.1) |
| Authorized by health care providers | 85 (35.3) |
| Substitution of traditional treatment(s) with cannabis | 92 (38.2) |
| CUDIT-R >12 | 33 (13.6) |
CUDIT-R, Cannabis Use Disorder Identification Test–Revised.
The percentages provided are for valid responses only as not all participants provided responses each time.
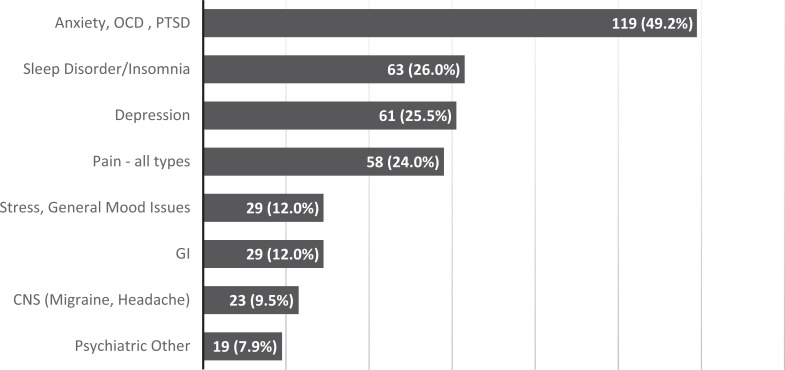
The majority of medicinal users used infrequently and more than a third (35%) reported that medicinal cannabis use was authorized by a health care professional. Nearly 40% had replaced traditional medication with cannabis to treat their ailment. Of the medicinal users, 13.6% met criteria for CUD in the past 6 months. The 4 most common ailments cited for medicinal cannabis use were anxiety (49.2%), sleep problems (26%), depression (25%), and pain (24%) (Figure 1). Of the medicinal users, 78.2% (n = 176) endorsed use for at least 1 mental health condition.
Figure 1.
Purported ailments (n = 225, reporting over 400 ailments). In total, 112 (49.8%) of participants reported using cannabis to treat more than 1 ailment. GI issues included menstrual symptoms, Crohn’s disease, irritable bowel disease, diabetes, and appetite. CNS included migraines, headaches, epilepsy, and brain damage. Psychiatric other included attention-deficit hyperactivity disorder, borderline personality disorder, and suicidal ideation. CNS, central nervous system; GI, gastrointestinal; OCD, obsessive-compulsive disorder; PTSD, posttraumatic stress disorder.
Discussion
Lifetime cannabis use for medicinal purposes is relatively common in this university sample (∼11%). Many students reported medicinal cannabis use to relieve anxiety or depression, and one-third replaced a traditional treatment with cannabis. These findings are concerning based on the US National Academies of Science, Engineering, and Medicine recommendation against cannabis use for mental health conditions. Cannabis use among individuals with depression has been associated with poorer outcomes,15 with evidence indicating more intense or disordered cannabis use preceding and even contributing to the onset of depressive symptomology.16 Cannabis use may also exacerbate anxiety and potentially induce panic attacks,3 as well as contribute to the onset and course of psychosis.17 The ailments reported by medicinal users in the sample do not match Canadian clinical practice guidelines, which limits medicinal cannabis use to treating palliative pain, spasticity, and chemotherapy-induced nausea.5
Approximately 35% of medicinal users in the survey reported authorization of cannabis by a health care provider. Although respondents were not asked to indicate the ailment for which cannabis was authorized, the ailments reported would suggest that professional authorization practices are inconsistent with evidence-based guidelines. The discrepancy between evidence and practice may reflect limited knowledge regarding the therapeutic value of medicinal cannabis use. Consistent with this position, Balneaves et al.18 and Ziemianski et al.19 found a need for further education and training on medicinal cannabis among prescribing health care professionals in Canada.
While the study did not address why medicinal users chose to use cannabis for their ailments, it is plausible that social norms, as well as current advertising and business marketing strategies, are influencing behaviours. There is notable similarity between the most frequent purported ailments in this study and in the top ailments touted by American cannabis dispensaries.2 Exposure to medicinal cannabis advertisement has also been found to be associated with greater cannabis use and negative health outcomes among adolescents.20 Marketing by medical cannabis dispensaries promoting cannabis as a panacea may also be influencing behaviours among university students.
This study showed that medicinal cannabis users are engaging in cannabis use for reasons beyond ailment management, with over 85% endorsing recreational motives. High rates of recreational use amongst this group appear to confirm clinicians’ suspicions that patients may be misrepresenting their motives when seeking medical authorization for cannabis.19 The risk of abuse is also concerning, as 13.6% of the sample met criteria for CUD. This is consistent with other studies that have found a high prevalence of CUD among medicinal cannabis users.21 The risk for cannabis dependence, combined with a sensitive period of brain development, may further predispose this age group to greater cannabis-related harm. Further investigations are needed to better describe the trajectory of health outcomes among university students who are medicinal cannabis users.
Limitations
The study has several limitations worth noting. Participants were not asked if they had been prescribed traditional medication for their purported ailments or what medication they had replaced. Thus, it is unknown what ailments were treated or what traditional treatments were replaced with cannabis. Not all university students check their emails, which may have limited participation, and respondents were unable to ask for clarification as they would in a laboratory setting.
Conclusions
The results of this study have specific implications for health care providers when considering authorization of medicinal cannabis. Physicians should caution against medicinal cannabis for treating conditions that are not evidence based, especially as it would relate to mental disorders, and should be alert to the diverse ailments and motives of those seeking medicinal cannabis. All patients requesting an authorization of medicinal cannabis should be screened for CUD. Physicians who are prescribing evidence-based treatments should caution against the use of medicinal cannabis until further research clarifies if these conditions could be worsened by either medicinal or recreational use.
Supplemental Material
Supplemental Material, Medicinal.Cannabis.Use.Among.Canadian.University.Students.2018.08.09 for Cannabis Use for Medicinal Purposes among Canadian University Students by Jacqueline M. Smith, Joel Mader, Andrew C. H. Szeto, Amelia M. Arria, Ken C. Winters and T. Chris R. Wilkes in The Canadian Journal of Psychiatry
Footnotes
Data Access: Data have been provided as a supplementary SPSS file (Medicinal.Cannabis.Use.Among.Canadian.University.Students.2018.08.09).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Support for this study was provided by the University of Calgary, Faculty of Nursing, and the National Institute on Drug Abuse (RO1DA14845).
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Health Canada, Government of Canada: Market Data. 2018. [cited 2018 Jul 31] www.canada.ca/en/health-canada/services/drugs-health-products/medical-use-marijuana/licensed-producers/market-data.html.
- 2. Cavazos-Rehg PA, Krauss MJ, Cahn E, et al. Marijuana promotion online: an investigation of dispensary practices [cited 2018 Jul 31]. Prev Sci. 2018;1–11. doi.org/10.1007/s11121-018-0889-2. [DOI] [PMC free article] [PubMed]
- 3. De Aquino JP, Sherif M, Radhakrishnan R, et al. The psychiatric consequences of cannabinoids [cited 2018 July 31]. Clin Ther. 2018;1–9. 2018;40(9): 1448–1456. [DOI] [PubMed] [Google Scholar]
- 4. Hall KP. Medicinal marijuana for treatment of chronic pain and other medical and psychiatric problems. JAMA. 2015;313(24):2474–2479. [DOI] [PubMed] [Google Scholar]
- 5. Allan MG, Ramji J, Perry D, et al. Simplified guideline for prescribing medical cannabinoids in primary care. Can Fam Physician. 2018;64(2):11–120. [PMC free article] [PubMed] [Google Scholar]
- 6. National Academies of Sciences, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington (DC): National Academies Press; 2017. [PubMed] [Google Scholar]
- 7. Substance Abuse and Mental Health Services Administration. 2017. Key substance use and mental health indicators in the United States: results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52) [cited 2018 Jul 31]. https://www.samhsa.gov/data/.
- 8. Sarvet AL, Wall MM, Keyes KM, et al. Recent rapid decrease in adolescents’ perception that marijuana is harmful, but no concurrent increase in use. Drug Alcohol Depend. 2018;186(1):68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wen H, Hockenberry JM, Druss BG. The effect of medicinal marijuana laws on marijuana-related attitude and perception among US adolescents and young adults [cited 2018 Jul 31]. Prev Sci. 2018;1–9. doi: 10.1007/s11121-018-0903-8 [DOI] [PubMed]
- 10. Volkow ND, Baler RD, Compton WM, et al. Adverse health effects of cannabis use. N Engl J Med. 2014;370(23):2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hall W, Lynskey M. Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction. 2016;111(10):1764–1773. [DOI] [PubMed] [Google Scholar]
- 12. Dillman DA, Smyth JD, Christian LM. Internet, Phone, Mail, and Mixed-Mode Surveys: The Tailored Design Method. Hoboken (NJ): John Wiley; 2014. [Google Scholar]
- 13. Simons J, Correia CJ, Carey KB, et al. Validating a five-factor marijuana motives measure: relations with use, problems, and alcohol motives. J Couns Psychol. 1998;45(3):265–273. [Google Scholar]
- 14. Adamson SJ, Kay-Lambkin FJ, Baker AL, et al. An improved brief measure of cannabis misuse: the Cannabis Use Disorders Identification Test–Revised (CUDIT-R). Drug Alcohol Depend. 2010;110(1-2):137–143. [DOI] [PubMed] [Google Scholar]
- 15. Bahorika AL, Leiowitz A, Sterling SA, et al. Patterns of marijuana use among psychiatry patients with depression and impact on recovery. J Affect Disord. 2017;213:168–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pacek LR, Martins SS, Crum RM. The bidirectional relationships between alcohol, cannabis, co-occurring alcohol and cannabis use disorders with major depressive disorder: results from a national sample. J Affective Disord. 2013;148(2-3):188–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Miller CL. Impact of marijuana on mental health In: Sabet KA, Winters KC, eds. Contemporary Health Issues on Marijuana. New York (NY): Oxford University Press; 2018. p. 121–163. [Google Scholar]
- 18. Balneaves LG, Alraja A, Ziemianski D, et al. A national needs assessment of Canadian nurse practitioners regarding cannabis for therapeutic purposes. Cannabis Cannabinoid Res. 2018;3(1):66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ziemianski D, Capler R, Tekanoff R, et al. Cannabis in medicine: a national educational needs assessment among Canadian physicians. BMC Med Educ. 2015;15:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. D’Amico EJ, Rodriquez A, Tucker JS, et al. Planting the seed for marijuana use: changes in exposure to medical marijuana advertising and subsequent adolescent marijuana use, cognitions and consequences over seven years. Drug Alcohol Depend. 2018;188(1):385–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Han B, Compton WM, Blanco C, et al. Trends in and correlates of medicinal marijuana use among adults in the United States. Drug Alcohol Depend. 2018;186:120–129. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Medicinal.Cannabis.Use.Among.Canadian.University.Students.2018.08.09 for Cannabis Use for Medicinal Purposes among Canadian University Students by Jacqueline M. Smith, Joel Mader, Andrew C. H. Szeto, Amelia M. Arria, Ken C. Winters and T. Chris R. Wilkes in The Canadian Journal of Psychiatry