Abstract
Randomized clinical trials are the preferred study design to address key research questions about the benefits or harms of interventions. However, randomized trials of oxygen therapy are difficult to conduct and have limitations. The purpose of this article is to offer our view on the potential use of patient registries in the field of home oxygen in COPD as an alternative to randomized trials by referring to the Swedish experience with a national registry for respiratory failure. Patient registries use observational study methods to collect uniform data (clinical and other) to evaluate specified outcomes for a population defined by a particular disease, condition, or exposure. As opposed to administrative databases, patient registries serve one or more predetermined scientific, clinical, or policy purposes. By systematically and prospectively compiling relevant data, patient registries may describe the natural history of a disease, determine effectiveness and cost-effectiveness, assess safety or harm, and measure quality of care. Registry-based randomized trials (ie, randomized trials within a clinical registry) combine the advantages of a prospective randomized trial with the strengths of a large-scale all-comers clinical registry. Challenges and issues in the design and implementation of patient registries include the representativeness of participants, data collection, quality assurance, ownership, and governance. Notwithstanding their limitations, patient registries represent valuable tools in the conduct of research in the area of home oxygen therapy.
Keywords: patient registry, home oxygen, COPD, evaluation
Introduction
Two landmark trials conducted in the late 1970s provided scientific evidence that long-term oxygen therapy (LTOT) may prolong life in patients with sCOPD) and severe resting daytime hypoxemia documented by direct arterial blood gas measurement.1,2 Thereafter, oxygen therapy became standard of care in COPD, and confirmatory trials would now be considered by many as unethical. New indications of oxygen therapy in COPD (such as nocturnal oxygen therapy in patients with isolated nocturnal oxygen desaturation, oxygen to relieve dyspnea, or ambulatory oxygen to correct exercise-induced desaturation) have since emerged, often without confirmation of effectiveness from randomized trials.3–5
Home oxygen therapy in COPD still offers a multitude of research opportunities.6 Suggestion has been made that multicenter clinical research networks should be established to perform such clinical trials.7 Although randomized clinical trials are the preferred study design when feasible to address some key research questions about the benefits or harms of interventions, there is increasing recognition that observational studies facilitated by registries are necessary to understand gaps in care, to evaluate the effects of interventions in real-world clinical and community settings, and to inform the design of hybrid effectiveness-implementation studies to accelerate the translation of guidelines into real-world settings.8 The objective of this commentary is to expand our view on the complementary roles of randomized trials and patient registries in evaluating outcomes of patients treated at home with oxygen.9
Current state of knowledge
Our review of home oxygen in COPD indicated that few randomized trials have been conducted, and the number of patients involved in these trials was small.9 For instance, the British Medical Research Council (BMRC) trial and the Nocturnal Oxygen Therapy Trial (NOTT) randomized a total of 290 patients.1,2 Although the utilization of LTOT is supported by the overall results of these two trials, numerous areas of uncertainty regarding its indications remain and represent important areas for further research. Both trials were conducted 40 years ago, in an era in which there were few medical therapies for COPD. The two trials evaluated the effects of LTOT in highly selected patients with COPD and few comorbidities, and in research conditions. Our understanding of the benefits and cost-effectiveness of home oxygen is therefore very limited.
For instance, subgroup analyses were conducted in the NOTT according to 16 different baseline characteristics and most lacked statistical power.2 No difference in mortality was seen among those with normocapnia, whereas the largest differences in mortality were noted in those with hypercapnia and respiratory acidosis at baseline. Patients enrolled in the BMRC trial were severely hypercapnic (mean pCO2: 54 mmHg). The benefit of LTOT in normocapnic patients is therefore unknown. Other subgroups of patients underrepresented in the two landmark trials include women who now constitute the majority of patients currently starting LTOT10,11 (as a total of only 58 women were randomized) and the very old (as mean age in the NOTT was 65, and the BMRC trial included only those aged <70).
Moreover, neither the BMRC trial nor the NOTT were submitted to a formal economic evaluation. Such analysis was conducted almost 10 years ago by Oba12 who estimated the incremental cost-effectiveness ratios for LTOT. This analysis was conducted from a third-party payer’s perspective. Accordingly, only direct costs were included. All costs were reported in 2007 US dollars. During 3- and 5-year horizons, the incremental cost-effectiveness ratios for LTOT were $23,807/quality-adjusted life year (QALY) and $16,124/QALY, respectively. These ratios fell below the cutoff that was then generally considered very cost-efficient (ie, $25,000/QALY). Although this analysis provided useful information, it was based only on modeling (rather than “real” data), and ignored indirect and intangible costs of LTOT. Only a few other economic analyses with limited scope have also been published.13,14
Limits of randomized trials of oxygen therapy
Randomized trials of oxygen therapy are difficult to conduct. Among the 20 published or ongoing trials that we referred to in our recent review of home oxygen in COPD,9 11 recruited <50 patients, three were stopped prematurely and one (the Long-Term Oxygen Treatment Trial)15 was redesigned after 7 months of recruitment and the randomization of only 34 patients. Why is that so?
Challenges in involving physicians and in recruiting participants in clinical trials are not unique to trials of home oxygen, and a body of literature has been devoted to this issue.16,17 Physicians-related barriers include, among others, time constraints and lack of support staff, whereas patient-related barriers include additional demands on participants and aversion to treatment choice by random allocation. Specific problems also arise in oxygen trials, however. Oxygen is part of general medical practice. Its perceived indications are numerous and, in several jurisdictions, the lack of evidence of efficacy does not translate into reimbursement constraints.18 Patients and clinicians may therefore decline participation in clinical trials if oxygen is readily available anyway. Clinicians themselves may be reluctant to allow their patients to be recruited in a placebo-controlled trial if clinical and personal equipoise (ie, the assumption that there is not one “better” intervention) does not exist. Long-term trials may be necessary to demonstrate benefits if survival or disease progression are the selected outcomes. During this extended period of time, patients’ and investigators’ interest may fade. Oxygen trials may compete with short-term protocols that are more attractive for patients seeking immediate benefits. Also, patients for whom oxygen therapy is considered have, by definition, severe COPD and are usually frail. This situation complicates their follow-up within the frame of clinical studies and increases the probability of withdrawal. Finally, the technology of providing oxygen at home is mature, and manufacturers have little incentive to participate in clinical trials. Hence, oxygen trials are more likely to be academic and operated from public funds, without business opportunity for investigators. We have faced all these problems in conducting the International Nocturnal Oxygen trial, a 4-year, multi-center, randomized, placebo-controlled trial of nocturnal oxygen therapy in patients with COPD (ClinicalTrials.gov ID. NCT01044628).19
Patient registry as an alternative
A patient registry is
an organized system that uses observational study methods to collect uniform data (clinical and other) to evaluate specified outcomes for a population defined by a particular disease, condition, or exposure, and that serves one or more predetermined scientific, clinical, or policy purposes.20
A registry database is a file derived from the registry.
Registries are not administrative databases
Registry databases must first be distinguished from administrative databases created by health authorities (often the payers of health care) by compiling claims data sets. Typically, administrative databases include patient demographics and other patient-level data about their utilization of health care resources. This information is usually limited to services that are billable. Administrative databases are not created to be used in clinical research and little attention is paid to the validity of its diagnoses. When administrative databases are exploited in research, data are used retrospectively.
We demonstrated that administrative databases from hospital records and billing claims notoriously lack validity for the diagnosis of COPD. In this study, the diagnosis of COPD was validated in 616 of 1,221 patients (predictive positive value of a diagnosis of COPD in the database: 50.4%; 95% confidence interval: 47.7–53.3).21 Accordingly, we warned against the utilization of such databases in clinical and epidemiological research if the purpose of using the database is to accrue a large cohort of patients with COPD, unless the validity of their diagnoses is demonstrated. Claiming that an administrative database “has been validated” is not sufficient since the validity of a database is diagnosis-specific.22 For instance, validity for the diagnosis of diabetes by no means implies validity for the diagnosis of COPD. In addition, validation studies should be regularly updated if the database is to be used in several occasions over time.
Patient registry as a research tool
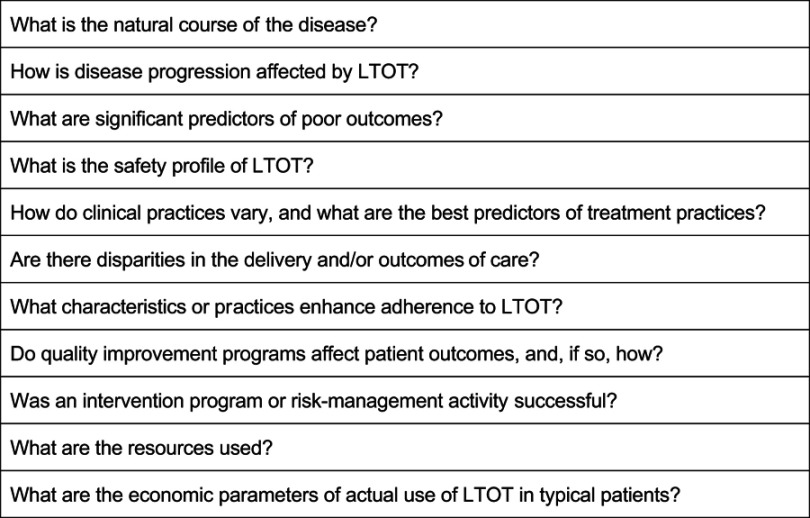
By systematically and prospectively compiling relevant data, patient registries may be used to describe the natural history of a disease, to determine effectiveness and/or cost-effectiveness, to assess safety or harm, and to measure quality of care.20 Patient registries are a powerful tool to evaluate patient outcomes when clinical trials are not practical or difficult to conduct, especially when very long-term outcomes are measured.23 Such is the case of clinical research on oxygen therapy. Successful national registries of patients on home oxygen are in place in Sweden24 and Denmark.25 Important pieces of information have emerged from these registries, including gender differences in the need of and survival with LTOT,10 and the prognosis of patients with alpha1-antitrypsine deficiency on long-term oxygen therapy.26 Other potential applications of patient registries in the area of home oxygen therapy include the assessment of clinical outcomes and their predictors, the study of adherence issues, the examination of health technologies, the determination of cost of illness and cost-effectiveness ratios, and the evaluation of clinical pathways and quality of care, to name a few. Examples of specific questions are presented in Figure 1.
Figure 1.
Examples of key questions on home oxygen in COPD to be addressed using patient registries.
Note: Adapted from Gliklich et al.20
Observational studies or randomized trials?
Up to recently, studies from patient registries have usually been observational (ie, cohort or case-control studies). This methodology lies below that of randomized trials in the hierarchy of research design and evidence.27 However, randomized trials themselves have limitations, even when they are well conducted. A major drawback of randomized trials in special populations is their limited generalizability (ie, external validity). For instance, the BMRC excluded patients with “systemic hypertension, proven coronary arterial disease and other life threatening diseases”,1 and the NOTT trial also excluded patients with other diseases that “might be expected to influence mortality, morbidity or compliance with therapy”.2 Even so, such patients who were excluded from both trials are now well represented among patients on home oxygen.
Another concern that is often raised regarding the use and interpretation of observational studies from patient registries, especially when they bear on clinical practice, is that they may systematically overestimate the magnitude of the effects of treatment as compared with those in randomized trials on the same topic. Empiric evidence suggests that in might not be the case if the observational study is well designed and conducted.28 Also, in some circumstances, observational design may be the only alternative when risks and harms are under scrutiny.
Registry-based randomized trials (ie, randomized trials within a clinical registry) have been suggested as a method of combining the advantages of a prospective randomized trial with the strengths of a large-scale all-comers clinical registry.29–31 This methodology involves the use of patient registries as a platform for patient recruitment and trial operationalization (patient inclusion, data collection, and follow-up).32 Routinely collected baseline information is retrieved from the registry. The additional work associated with inclusion of individual patients is limited to obtaining informed consent and randomization. Clinical end point parameters are obtained from continuous maintenance of the health registry. Such trials have the potential to improve external validity of results and may allow long-term follow-up. No significant difference was found between effect estimates from conventional and registry-based randomized controlled trials.33 It has even been suggested that researchers planning an RCT should always check whether existing registries can be used for data collection.29
An example of such a randomized trial in the field of home oxygen therapy is the REgistry-based Treatment Duration and Mortality in Long-term OXygen Therapy (REDOX) trial (ClinicalTrials.gov ID. NCT03441204), a multicenter, Phase IV, registry-based, randomized, controlled trial which is now recruiting. Patients starting LTOT are randomized between LTOT prescribed 24 h/day or 15 h/day using the Swedish Register for Respiratory Failure (Swedevox). Clinical follow-up and concurrent treatments are according to routine clinical practice. A sample size of 2,126 patients is targeted. The main endpoints of mortality, hospitalizations, and incident disease are assessed, with expected complete follow-up.
Practical issues
Who is in the registry?
A major issue, as in randomized trials, is the representativeness of participants and clinical practices under study in order to ensure the external validity of its content. National registries are particularly well suited for ensuring completeness, especially in jurisdictions where health care services (including home oxygen therapy) are covered through universal medical insurance plan such as in Sweden and Canada, making sampling unnecessary. In these settings, full account of a majority of patients may be taken, regardless of their clinical, social or economic status. For instance, in Sweden, completeness of patients starting LTOT has been stable at about 85% since 1987.24 Universality of health care services does not imply that patients are in the obligation to register in a registry, however. Depending on the jurisdiction, patients’ informed consent may be required.20 Quality and health services research restricted to patients who give consent may misrepresent outcomes.34
Data collection
In order to ensure comprehensiveness and validity, data must be collected in a systematic and timely manner. Data collection may be integrated into routine clinical workflow upon registration to respiratory home care programs.24 Mandatory prescription forms can be used to gather information regarding patients’ clinical characteristics including primary and secondary diagnoses, indication for home oxygen, smoking history, arterial blood gas results, oxygen prescription, and date of entry. Quality assurance is also a critical issue, and its requirements must be defined early during the creation of the registry.20
Clinical outcomes assessment implies repeated measurements and long-term follow-up. In patients on long-term oxygen, relevant outcomes include, among others, disease progression and vital status, quality of life, cost, harm, and adherence. Novel interventions and changes in clinical practices also need to be monitored. Quality of care represents another important outcome. A registry may be instrumental in monitor adherence to prescription guidelines – so that the right patients receive the right treatment35 – and costs. Routine collection of follow-up data is a major challenge of registries. Information on clinical outcomes may be collected prospectively through continued care, with the disadvantage of an increased burden on the clinical staff. In a registry of patients on home oxygen, vital status might be the easiest information to collect since, once a patient meets LTOT criteria and oxygen therapy is initiated, oxygen therapy is generally for life. Data linkage (a method of bringing information from different sources together about the same person to create a new, richer dataset) to supplement measurement of patient outcomes and clinical performance may be considered. However, data linkage has its own limitations36 by raising other methodological and ethical issues.37
Ownership and governance
A delicate issue is the ownership of patient registries and their governance. Ownership encompasses operational control of the registry data and publication rights.20 A pragmatic view would be that a registry belongs to those who fund it. Accordingly, health care providers, government agencies, research institutions, funding agencies and even insurers could claim ownership. Rules of governance must be set a priori to ensure that patient privacy, registry transparency and data quality are preserved. In this regard, executive, steering and data safety and monitoring committees that lead large randomized trials find their counterparts in patient registries.
Conclusion
The harms and benefits of home oxygen therapy remain largely unexplored in COPD and in other cardiopulmonary conditions (including interstitial lung diseases, cystic fibrosis, pulmonary arterial hypertension and chronic heart failure). Experience to date has demonstrated that clinical trials are difficult to conduct in this area. We now believe, as others, that
the focus should turn to what constitutes high-quality research and evidence for a particular purpose and how quickly and reliably the information can be obtained, and less on the label of the particular study design.23
Patient registries represent valuable tools in the conduct of research in the area of home oxygen therapy.
Disclosure
Professor Jerry A. Krishnan reports grants from the National Institutes of Health and Patient Centered Outcomes Research Institute during the conduct of the study. Dr Maltais reports grants and personal fees from Novartis and Boehringer Ingelheim, and grants from Sanofi, AstraZeneca and Grifols, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.Report of the Medical Research Council Working Party. Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Lancet. 1981;1(8222):681–686. [PubMed] [Google Scholar]
- 2.Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Ann Intern Med. 1980;93(3):391–398. [DOI] [PubMed] [Google Scholar]
- 3.Cranston JM, Crockett AJ, Moss JR, Alpers JH. Domiciliary oxygen for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;(4):CD001744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ekstrom M, Ahmadi Z, Bornefalk-Hermansson A, Abernethy A, Currow D. Oxygen for breathlessness in patients with chronic obstructive pulmonary disease who do not qualify for home oxygen therapy. Cochrane Database Syst Rev. 2016;11:CD006429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ameer F, Carson KV, Usmani ZA, Smith BJ. Ambulatory oxygen for people with chronic obstructive pulmonary disease who are not hypoxaemic at rest. Cochrane Database Syst Rev. 2014;(6):CD000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Croxton TL, Bailey WC. Long-term oxygen treatment in chronic obstructive pulmonary disease: recommendations for future research: an NHLBI workshop report. Am J Respir Crit Care Med. 2006;174(4):373–378. doi: 10.1164/rccm.200507-1161WS [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Croxton TL, Weinmann GG, Senior RM, Wise RA, Crapo JD, Buist AS. Clinical research in chronic obstructive pulmonary disease: needs and opportunities. Am J Respir Crit Care Med. 2003;167(8):1142–1149. doi: 10.1164/rccm.200207-756WS [DOI] [PubMed] [Google Scholar]
- 8.Gershon AS, Jafarzadeh SR, Wilson KC, Walkey AJ; Clinical Knowledge from Observational Studies. Everything you wanted to know but were afraid to ask. Am J Respir Crit Care Med. 2018;198(7):859–867. doi: 10.1164/rccm.201801-0118PP [DOI] [PubMed] [Google Scholar]
- 9.Lacasse Y, Tan AM, Maltais F, Krishnan JA. Home oxygen in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197(10):1254–1264. doi: 10.1164/rccm.201802-0382CI [DOI] [PubMed] [Google Scholar]
- 10.Franklin KA, Gustafson T, Ranstam J, Strom K. Survival and future need of long-term oxygen therapy for chronic obstructive pulmonary disease–gender differences. Respir Med. 2007;101(7):1506–1511. doi: 10.1016/j.rmed.2007.01.009 [DOI] [PubMed] [Google Scholar]
- 11.Nishi SP, Zhang W, Kuo YF, Sharma G. Oxygen therapy use in older adults with chronic obstructive pulmonary disease. PLoS One. 2015;10(3):e0120684. doi: 10.1371/journal.pone.0120684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oba Y. Cost-effectiveness of long-term oxygen therapy for chronic obstructive disease. Am J Manag Care. 2009;15(2):97–104. [PubMed] [Google Scholar]
- 13.Andersson A, Strom K, Brodin H, et al. Domiciliary liquid oxygen versus concentrator treatment in chronic hypoxaemia: a cost-utility analysis. Eur Respir J. 1998;12(6):1284–1289. [DOI] [PubMed] [Google Scholar]
- 14.Jodar-Sanchez F, Ortega F, Parra C, et al. Cost-utility analysis of a telehealth programme for patients with severe chronic obstructive pulmonary disease treated with long-term oxygen therapy. J Telemed Telecare. 2014;20(6):307–316. doi: 10.1177/1357633X14544421 [DOI] [PubMed] [Google Scholar]
- 15.Long-Term Oxygen Treatment Trial Research Group, Albert RK, Au DH, et al. A randomized trial of long-term oxygen for COPD with moderate desaturation. N Engl J Med. 2016;375(17):1617–1627. doi: 10.1056/NEJMoa1604344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaur G, Smyth RL, Williamson P. Developing a survey of barriers and facilitators to recruitment in randomized controlled trials. Trials. 2012;13:218. doi: 10.1186/1745-6215-13-218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Treweek S, Mitchell E, Pitkethly M, et al. Strategies to improve recruitment to randomised controlled trials. Cochrane Database Syst Rev. 2010;(1):MR000013. [DOI] [PubMed] [Google Scholar]
- 18.Lacasse Y, Bernard S, Maltais F. Eligibility for home oxygen programs and funding across Canada. Can Respir J. 2015;22(6):324–330. doi: 10.1155/2015/280604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lacasse Y, Bernard S, Series F, et al. Multi-center, randomized, placebo-controlled trial of nocturnal oxygen therapy in chronic obstructive pulmonary disease: a study protocol for the INOX trial. BMC Pulm Med. 2017;17(1):8. doi: 10.1186/s12890-017-0500-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gliklich R, Dreyer N, Leavy M, editors. Registries for Evaluating Patient Outcomes: A User’s Guide. 3rd ed. Rockville (MD): Agency for Healthcare Research and Quality; 2014. [PubMed] [Google Scholar]
- 21.Lacasse Y, Daigle JM, Martin S, Maltais F. Validity of chronic obstructive pulmonary disease diagnoses in a large administrative database. Can Respir J. 2012;19(2):e5–e9. doi: 10.1155/2012/260374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilchesky M, Tamblyn RM, Huang A. Validation of diagnostic codes within medical services claims. J Clin Epidemiol. 2004;57(2):131–141. doi: 10.1016/S0895-4356(03)00246-4 [DOI] [PubMed] [Google Scholar]
- 23.Dreyer NA, Garner S. Registries for robust evidence. JAMA. 2009;302(7):790–791. doi: 10.1001/jama.2009.1092 [DOI] [PubMed] [Google Scholar]
- 24.Ekstrom M, Ahmadi Z, Larsson H, et al. A nationwide structure for valid long-term oxygen therapy: 29-year prospective data in Sweden. Int J Chron Obstruct Pulmon Dis. 2017;12:3159–3169. doi: 10.2147/COPD.S140264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ringbaek TJ, Lange P. The impact of the Danish Oxygen Register on adherence to guidelines for long-term oxygen therapy in COPD patients. Respir Med. 2006;100(2):218–225. doi: 10.1016/j.rmed.2005.04.023 [DOI] [PubMed] [Google Scholar]
- 26.Ringbaek TJ, Seersholm N, Perch M, Iversen M, Lange P. Prognosis of patients with alpha1-antitrypsine deficiency on long-term oxygen therapy. Respir Med. 2014;108(8):1189–1194. doi: 10.1016/j.rmed.2014.05.001 [DOI] [PubMed] [Google Scholar]
- 27.Guyatt GH, Sackett DL, Cook DJ; Evidence-Based Medicine Working Group. Users’ guides to the medical literature. II. How to use an article about therapy or prevention. A. Are the results of the study valid? JAMA. 1993;270(21):2598–2601. [DOI] [PubMed] [Google Scholar]
- 28.Concato J, Shah N, Horwitz RI. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med. 2000;342(25):1887–1892. doi: 10.1056/NEJM200006223422507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mathes T, Buehn S, Prengel P, Pieper D. Registry-based randomized controlled trials merged the strength of randomized controlled trails and observational studies and give rise to more pragmatic trials. J Clin Epidemiol. 2018;93:120–127. doi: 10.1016/j.jclinepi.2017.09.017 [DOI] [PubMed] [Google Scholar]
- 30.Ekstrom M. What can we learn about breathlessness from population-based and administrative health data? Curr Opin Support Palliat Care. 2016;10(3):223–227. doi: 10.1097/SPC.0000000000000220 [DOI] [PubMed] [Google Scholar]
- 31.Lauer MS, D’Agostino RB Sr. The randomized registry trial–the next disruptive technology in clinical research? N Engl J Med. 2013;369(17):1579–1581. doi: 10.1056/NEJMp1310102 [DOI] [PubMed] [Google Scholar]
- 32.Li G, Sajobi TT, Menon BK, et al. Registry-based randomized controlled trials- what are the advantages, challenges, and areas for future research? J Clin Epidemiol. 2016;80:16–24. doi: 10.1016/j.jclinepi.2016.08.003 [DOI] [PubMed] [Google Scholar]
- 33.Mathes T, Klassen P, Pieper D. No difference were found between effect estimates from conventional and registry-based randomized controlled trials. J Clin Epidemiol. 2018:pii: S0895-4356(18)30401-3 Epub ahead of print. doi: 10.1016/j.jclinepi.2018.09.011 [DOI] [PubMed] [Google Scholar]
- 34.Woolf SH, Rothemich SF, Johnson RE, Marsland DW. Selection bias from requiring patients to give consent to examine data for health services research. Arch Fam Med. 2000;9(10):1111–1118. [DOI] [PubMed] [Google Scholar]
- 35.Guyatt GH, McKim DA, Austin P, et al. Appropriateness of domiciliary oxygen delivery. Chest. 2000;118(5):1303–1308. [DOI] [PubMed] [Google Scholar]
- 36.Bohensky MA, Jolley D, Sundararajan V, et al. Data linkage: a powerful research tool with potential problems. BMC Health Serv Res. 2010;10:346. doi: 10.1186/1472-6963-10-302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kelman CW, Bass AJ, Holman CD. Research use of linked health data–a best practice protocol. Aust N Z J Public Health. 2002;26(3):251–255. [DOI] [PubMed] [Google Scholar]