Abstract
Objective: This study aimed to investigate the anatomic configuration of the blood vessels that contribute to portal vein tumor thrombus (PVTT), a common complication of hepatocellular carcinoma, in VX2 rabbits.
Materials and methods: Peripheral blood mononuclear cells (MNCs) were isolated and labeled using superparamagnetic iron oxide particles in vitro. Twenty-four rabbits were injected with the VX2 tumor via the portal vein to establish the PVTT model. The rabbits (n=6/treatment group) were randomly assigned into four groups. Rabbits of groups A, B and C received an infusion of iron-labeled MNCs via the hepatic artery, the portal vein or the auricular vein, respectively, whereas rabbits of group D received an injection of normal saline via the auricular vein 7 days after the injection of VX2 tumors. MRI was performed, and the signal intensity (SI) of the PVTTs was measured on T2-weighted images (T2WIs) 1 day after the transfusion of iron-labeled cells.
Results: The SI of PVTTs, as measured on T2WIs, in rabbits of groups A, B, C and D was 241.400 (172.350, 364.825), 221.150 (203.775, 318.225), 590.200 (363.325, 728.875) and 568.050 (474.725, 705.150), respectively. Our data showed a significant decrease in the SI of PVTTs in rabbits of groups A and B compared with rabbits of groups C and D (group A vs group C, U=4.000, p=0.025; group A vs group D, U=2.000, p=0.010; group B vs group C, U=4.000, p=0.025; group B vs group D, U=1.000, p=0.006). There was no significant difference in the SI of PVTTs in rabbits of group A and B.
Conclusion: Our results indicated that the portal vein and the hepatic artery supplied blood flow to the PVTT in rabbits.
Keywords: portal vein tumor thrombus, magnetic resonance imaging, mononuclear cells
Background
Hepatocellular carcinoma (HCC) is characterized by the early formation of portal vein tumor thrombus (PVTT). PVTT is an important prognostic factor and predictor for HCC recurrence.1 The prognosis of patients diagnosed with hepatocellular carcinoma (HCC) remains extremely poor.2 The median survival time is generally less than 6 months for untreated HCC patients with PVTT.3 The hepatic artery, as opposed to the portal vein, supplies HCC, and intra-arterial chemotherapeutic treatment is based on this anatomic configuration. TACE is a standard locoregional treatment option widely used to fight unresectable HCC.4,5 Several studies reported that the infusion of chemotherapeutic agents, such as TACE, via the hepatic artery is effective in the treatment of patients diagnosed with HCC and accompanied by PVTT. However, the accumulation of Lipiodol in HCC patients with PVTT was different; it was found to be homogeneous, non-homogenous, mildly defective or poorly accumulated.6 In our review of the literature, we found almost no data on the intra-portal infusion of chemotherapeutic agents in HCC patients with PVTT. Furthermore, the vessels that supply blood to PVTTs are uncharacterized, although possible sources might be the hepatic artery, portal vein or other vessels surrounding the porta hepatis.
Endothelial progenitor cells (EPC), which are essential for tumor development, growth and metastasis, respond to chemokine gradients formed in ischemic or hypoxic tumorigenic tissues where they function in neovascularization.7 Emerging evidence suggests that peripheral blood contains a large number of mononuclear cells (MNCs) from which EPCs are derived.8,9 MNCs may have similar effects on tumor growth as mesenchymal stem cells (MSCs), which can home into various tumors as breast cancer, prostate cancer.10 Several studies reported that MNCs and EPCs can be labeled with superparamagnetic iron oxide (SPIO) particles without affecting the viability or function of these cells.8,9,11 In vivo magnetic resonance imaging (MRI) can then be used to track magnetically labeled MNCs and EPCs, including their incorporation into the neovasculature.11,12
In the present study, we measured the signal intensity (SI) of PVTTs in rabbits after intra-arterial or intra-portal transfusion of iron-labeled MNCs using MRI. Our results indicated that the low SI values directly corresponded to the poor overall quality of the transfused iron-labeled cells, suggesting that the hepatic artery and the portal vein supply blood to PVTTs. These results may provide new insights on how to improve intra-arterial and intra-portal chemotherapy for the treatment of PVTT.
Objective
This study aimed to investigate the anatomic configuration of the blood vessels that contribute to portal vein tumor thrombus (PVTT), a common complication of hepatocellular carcinoma, in VX2 rabbits.
Materials and methods
Study design
Our institutional animal care and use committee (Ethics committee of experimental animal welfare, Nanjing medical university) approved the study, and all procedures were performed under the guidelines prescribed by our university. A total of 40 adult New Zealand White male or female rabbits (Jingling Breeding Co., Nanjing, China) weighing 3.0–3.5 kg were used for this study. Twelve rabbits were used for collecting peripheral blood to isolate MNCs. Four rabbits were used as tumor carriers for the experimental rabbits, and 24 experimental rabbits received an injection of the VX2 tumor via the main portal vein. These experimental rabbits were then randomly assigned to four groups of six animals each. Rabbits of groups A, B and C received an infusion of iron-labeled MNCs via the hepatic artery, portal vein or auricular vein, respectively. Rabbits of group D received an injection of normal saline via the auricular vein 7 days after the injection of the VX2 tumor. There was no intra-sexual difference between these four groups. All animals underwent imaging in a 1.5-T clinical MRI scanner 1 day after cell infusion or saline injection.
Animal model
Anesthesia was induced by an intravenous injection of pentobarbital sodium (100 mg/kg; Reagent Chemicals Co., Shanghai, China). The VX2 tumor (obtained from Zhongda Hospital, Nanjing, China) was grown in the hind limb of donor rabbits. The tumors were approximately 2 cm in diameter 4 weeks later, at which time they were harvested and minced into smaller pieces approximately 0.2×1.5 cm. Following midline laparotomy, we cannulated a branch of the superior mesenteric vein by using an 18-gauge catheter (Terumo, Tokyo, Japan). We then introduced a percutaneous trans-hepatic cholangiography (PTC) cannula (Cook Inc., Bloomington, USA) into the portal trunk vein via a 0.014-in. wire (Terumo, Tokyo, Japan). Thereafter, we implanted the VX2 tumor via the main portal vein through the PTC cannula until the portal vein was totally occluded. Portography was conducted before and after the implantation. Subsequently, the superior mesenteric vein was closed with a ligature. Postoperatively, rabbits were subcutaneously given penicillin (25,000 IU/kg) once daily for 3 consecutive days. The model rabbits were kept for one week.
Iron-labeled MNCs
Poly-L-lysine (PLL)-conjugated SPIO particles were prepared as previously reported.11 In brief, Fe2+ was mixed with Fe3+ ions (PH =1.7), which was reacted at a pH of 9 for 30 mins. As the precipitant, Fe3O4 was collected, purified and oxidized by Fe(NO3)3 to obtain Fe2O3. To obtain PLL-capped Fe2O3 nanoparticles (PLL-SPIO particles), Fe2O3 was diluted with deionized water to a concentration of 8 g/l and then reacted with 1% PLL for 2 hrs.
MNCs were collected and labeled as previously reported.9 To isolate peripheral blood MNCs, 20 mL of peripheral blood was collected from a rabbit by cannulating an 18-gauge catheter into the central auricular artery. The blood was heparinized (100 IU/mL; heparin sodium, Qianhong Inc., Jiangsu, China), diluted to a 1:1 ratio with Histopaque 1077 (Sigma-Aldrich, St. Louis, MO, USA) in phosphate-buffered saline (PBS) and centrifuged in a density-gradient centrifuge at 400 g for 30 mins. The sedimented layer of peripheral blood MNCs was collected, washed twice with PBS and adjusted to a concentration of 5×105 cells/mL. After 12 hrs, the iron-labeled MNCs were washed thrice with PBS and adjusted to a concentration of 1×106 cells/mL for subsequent cell delivery. Rabbits were transfused with iron-labeled MNCs 7 days after the implantation of the VX2 tumor via the portal vein. MNCs were labeled and delivered within a time span of less than 2 hrs.
Access into the right common femoral artery was obtained via a surgical incision in rabbits of group A. A 2.7F catheter (Terumo, Tokyo, Japan) was introduced into the proper hepatic artery, and arteriography was performed. A 2-mL suspension containing 2×106 iron-labeled MNCs was slowly administered into the proper hepatic artery within a time span of 5 mins. Thereafter, the common femoral artery was ligated with absorbable sutures.
A 2.7F catheter was introduced into the portal vein trunk through a branch of the superior mesenteric vein after midline laparotomy and portography were performed in rabbits of group B. A 2-mL suspension containing 2×106 iron-labeled MNCs was slowly administered into the portal vein within a time span of 5 mins. Thereafter, the superior mesenteric vein was closed with a ligature.
A 2-mL suspension containing 2×106 iron-labeled MNCs was slowly administered into the auricular vein in rabbits of group C. A 2-mL saline injection was administered into the auricular vein in rabbits of group D.
MRI and data acquisition
All rabbits underwent imaging in a 1.5T clinical MRI scanner (Achieva 1.5T, Philips, Netherlands) 1 day after cell infusion or saline injection. Each rabbit was placed inside an extremity coil and covered with a blanket for warmth. The imaging protocol generated a T2-weighted image (T2WI) (matrix size, 288×288; slice thickness, 0.3 cm; slice gap, 0.03 cm; repetition/echo time, 6,716/100 ms; WFS (pix)/BW, 1.529/142.1 Hz) and a T1-weighted image (T1WI) (matrix size, 512×512; slice thickness, 0.3 cm; slice gap, 0.03 cm; repetition/echo time, 580/15 ms; WFS (pix)/BW, 1.895/114.6 Hz).
A computer with a Philips DICOM Viewer 3.0 SP2 was used to analyze the images. Two experienced MRI radiologists, X.M.Z. and Z.G., with no knowledge of the histopathological findings, evaluated the images. They determined the average SI of the PVTTs and measured the liver and the dorsal muscle on T2WIs. Any discrepancy between the findings was adjudicated by J.C. To determine the SI, the total area of each PVTT was outlined to generate the region of interest. To measure the SI of the liver and the dorsal muscle, but not the vessels, regions of interest were outlined as described for PVTTs.
Histopathological evaluation
Immediately after MRI examination, the livers of sacrificed animals were perfused via the heart with 4% paraformaldehyde for fixation and embedded in paraffin. The specimens were sliced into 6–10 μm in thickness for hematoxylin-eosin staining to identify tissue morphology and for Prussian blue staining to display iron particles. To evaluate the number of accumulated MNCs in PVTTs, representative sections stained with Prussian blue from rabbits of groups A, B and C were analyzed by a blinded investigator (J.Y.Z.). For each slide, five fields of view (magnification, ×200) were randomly selected and Prussian blue-stained cells were counted.
Statistical analysis
SPSS software (SPSS for Windows, version 11.0, 2001; SPSS, Chicago, IL, USA) was used for statistical analyses. All quantitative data obtained were presented as median and quartile ranges (25%, 75%). Pearson’s correlation test was used to determine the correlation between the SI of PVTTs, as measured on T2WIs, and the Prussian blue-stained cell count in rabbits of groups A and B. The SI between two groups was analyzed by testing for two independent samples (Mann–Whitney U). The differences were considered statistically significant at p-values less than 0.05.
Results
Animal model and MNCs
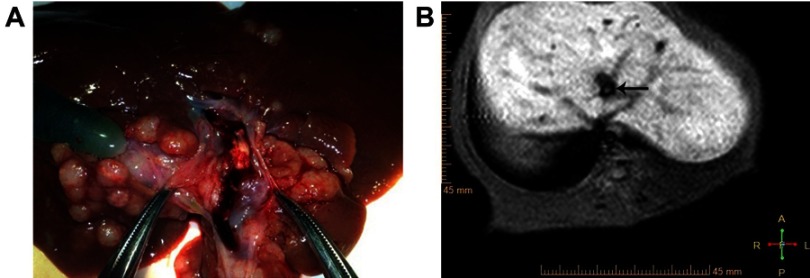
The implantation of the VX2 tumor via the portal vein was successful in all rabbits (Figure 1A). As shown by MRI, rabbits presented with PVTTs in the main portal vein (Figure 1B). The transfusion of iron-labeled MNCs was achieved via the hepatic artery, portal vein or auricular vein in rabbits of groups A, B and C, respectively.
Figure 1.
PVTT in VX2 rabbits. (A) Portal vein tumor thrombus successfully grown. (B) MRI showed equisignal in portal vein, which indicated PVTT production(arrow).
MRI
As observed on T1WIs and T2WIs, rabbits of groups A, B, C and D presented with PVTTs (Figure 2). There was a significant decrease in the SI in rabbits of groups A and B. The SI of PVTTs in rabbits of groups A, B, C and D was 241.400 (172.350, 364.825), 221.150 (203.775, 318.225), 590.200 (363.325, 728.875) and 568.050 (474.725, 705.150), respectively. The SI of PVTTs in rabbits of group A was significantly lower than that in rabbits of groups C and D (group A vs group C, U=4.000, p=0.025; group A vs group D, U=2.000, p=0.010). Furthermore, the SI of PVTTs in rabbits of group B was significantly lower than that in rabbits of groups C and D (group B vs group C, U=4.000, p=0.025; group B vs group D, U=1.000, p=0.006). There was no significant difference in the SI of PVTTs in rabbits of groups A and B, as well as in rabbits of groups C and D.
Figure 2.

PVTTs were observed in TW1s and TW2s in four groups. (A-B) showed PVTTs (arrow) in TW1s and TW2s of group A. (C-D) showed PVTTs (arrow) in TW1s and TW2s of group B. (E-F) showed PVTTs (arrow) in TW1s and TW2s of group C. (G-H) showed PVTTs (arrow) in TW1s and TW2s of group D. The SI of PVTTs in rabbits of groups A and B were significantly lower than that in rabbits of groups C and D in TW2s.
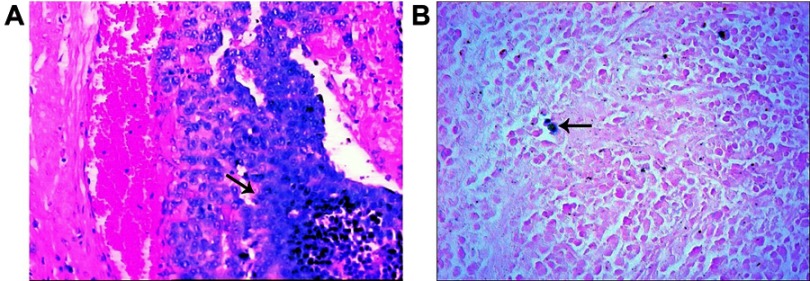
Histopathological findings
The VX2 tumors were identified by staining with hematoxylin-eosin (Figure 3A). The iron particles were identified by staining with Prussian blue in rabbits of groups A and B, which was indicative of successful delivery of iron-labeled MNCs (Figure 3B). The number of Prussian blue-positive cells derived from rabbits of groups A, B and C were 112.917 (71.667, 135.917), 119.583 (87.250, 125.375) and 1.750 (0.000, 22.333), respectively. The number of cells derived from rabbits of groups A and B was significantly higher than that isolated from rabbits of group C (group A vs group C, U=0.000, p=0.004; group B vs group C, U=0.000, p=0.004). There was no significant difference in the number of cells derived from rabbits of groups A and group B.
Figure 3.
Histopathological staining of PVTTs. (A) showed the tumor thrombus (arrow) in portal vein with HE staining. (B) showed iron particles (arrow) with Prussian blue staining.
Abbreviation: PVTT, Portal vein tumor thrombus.
Radiological–pathological analysis
The correlation coefficient between the SI of PVTTs, as determined from T2WIs, and the Prussian blue-stained cell count in groups A and B was −1.000 (p=0.000).
Discussion
Lyden et al reported that tumor angiogenesis and growth can be restored by transplanting circulatory EPCs in angiogenesis-defective Id1±Id3−/- mice, and the transplanted cells contributed to the creation of 90% of the neovessels.13 EPCs can be derived from peripheral blood, bone marrow and spleen MNCs.14 Matsuda reported that vascular endothelial growth factor-loaded poly captures EPCs from peripheral blood MNCs and induces their differentiation.15 Here, we successfully labeled MNCs with iron for subsequent in vivo tracking by MRI.
Cell labeling is essential for in vivo tracking by MRI. SPIO has been widely used as an MRI contrast agent because it generates an intense signal on T2WIs. Both EPCs and MNCs can be efficiently labeled with SPIO.8,9 Furthermore, Shapiro demonstrated that daughter cells at embryonic day 11.5 labeled with a particle, when injected into single cell-stage mouse embryos, could still be tracked even after many cell divisions.16 Other studies have demonstrated that the accumulation of magnetically labeled MNCs or EPCs could be detected by MRI after their systemic administration.11,12,14 In an MRI study, the contrast-to-noise ratio on T2WIs significantly decreased in the liver after injecting labeled mesenchymal stem cells, and the degree of the decrease in the SI correlated with the quantity of the labeled cells.17 Here, the SI of PVTTs was analyzed after administrating iron-labeled MNCs via the hepatic artery, portal vein or auricular vein. Although iron-labeled MNCs accumulated in PVTTs and participated in neovascularization, their transfusion led to a marked decrease in the SI. The decrease in the SI, which hinted at the overall poor quantity of the transfused iron-labeled cells, suggests that PVTTs received blood flow from the hepatic artery and the portal vein.
Increasing evidence indicates that trans-arterial chemoembolization, as well as intra-arterial and intra-portal chemotherapy, are effective in HCC patients with PVTTs.18–20 Intra-arterial and intra-portal chemotherapy for these indications requires a good understanding of the anatomic configuration of blood vessels and the direction of blood flow. For example, autopsies, surgeries and computed tomography studies have been used to understand the vasculature of the liver. However, it is virtually impossible to quantify the volume of blood that contributes to PVTT. Here, we used MRI to investigate the anatomic configuration of blood vessels contributing to PVTTs in rabbits. A significant decrease in the SI of PVTTs was observed on T2WIs after the intra-atrial and intra-portal transfusion of iron-labeled MNCs in rabbits of groups A and B. Furthermore, radiological–pathological analysis demonstrated a strong correlation between the decrease in the SI and the number of iron-labeled cells tumor was injected via the main portal vein, it is possible that the blood supply for PVTTs originated from the portal vein, as well as the hepatic artery. According to our quantitative data, however, it does not seem that one vessel type contritumor was injected via the main portal vein, it is possible that the blood supply for PVTTs originated from the portal vein, as well as the hepatic artery. According to our quantitative data, however, it does not seem that one vessel type contributed a higher proportion of blood than the other vessel type. Interestingly, there was no significant difference in the SI of PVTTs in rabbits of groups A and B. Taken collectively, our results may help in the understanding of the autonomic configuration of blood vessels that supply blood to PVTTs. Our results may also facilitate the administration of medications to treat PVTTs, as medications should be administered via the hepatic artery and the portal vein in patients receiving localized chemotherapy for PVTT.
The major strength of the present study was that the anatomic configuration of the blood vessels that contribute to PVTTs was defined. Our results provided in vivo insights into the blood supply originating from hepatic artery and portal vein and feeding into PVTTs. The major weakness of the present study, however, was that it failed to address the degrees of EPC differentiation from MNCs and incorporation into blood vessels. About group C, iron-labeled MNCs was administered into the auricular vein in rabbits. Because the MNCs have the potential of homing into tumor and injured vessel, after MRI examination, we did not analyze the number of MNCs trapped in the other oranges as lung, spleen. We will make further improvement in the following studies. Furthermore, the conclusions drawn from this study are limited to a mammalian model of experimental PVTT. Further research involving in vivo imaging methods, such as computerized tomography during hepatic arteriography and hepatic portography, are warranted to confirm the anatomic configuration of the blood vessels that contribute to PVTT in HCC patients.
In conclusion, we found that the hepatic artery and the portal vein supplied blood to PVTTs in rabbits. These results may help in the understanding of the anatomic configuration of vessels that supply blood to PVTTs. These results may also provide new insights on how to improve intra-arterial and intra-portal chemotherapy for the treatment of PVTT.
Acknowledgments
This work was supported by grants from the National Nature Science Foundation of China (grant no. 81271677), Talent 333 project in Jiangsu Province (grant no. BRA2015492) and Jiangsu Cancer Hospital Young Talents Plan (Jiangsu China).
Ethical approval
This study was approved by the Ethics Committee of Jiangsu Cancer Hospital and Cancer Hospital of Nanjing Medical University (NMU) (No. 2012-016).
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kamiyama T, Kakisaka T, Orimo T, Wakayama K. Hepatectomy for hepatocellular carcinoma with portal vein tumor thrombus. World J Hepatol. 2017;9(36):1296–1304. doi: 10.4254/wjh.v9.i36.1296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Park JW, Chen M, Colombo M, et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE study. Liver Int. 2015;35(9):2155–2166. doi: 10.1111/liv.12818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.European Association For The Study Of The Liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236. doi: 10.1016/j.jhep.2018.03.019 [DOI] [PubMed] [Google Scholar]
- 4.Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67(1):358–380. doi: 10.1002/hep.29086 [DOI] [PubMed] [Google Scholar]
- 5.Omata M, Cheng AL, Kokudo N, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017;11(4):317–370. doi: 10.1007/s12072-017-9799-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun J, Shi J, Huang B, et al. The degree of hepatic arterial blood supply of portal vein tumor thrombus in patients with hepatocellular carcinoma and its impact on overall survival after transarterial chemoembolization. Oncotarget. 2017;8(45):79816–79824. doi: 10.18632/oncotarget.19767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de la Puente P, Muz B, Azab F, Azab AK. Cell trafficking of endothelial progenitor cells in tumor progression. Clin Cancer Res. 2013;19(13):3360–3368. doi: 10.1158/1078-0432.CCR-13-0462 [DOI] [PubMed] [Google Scholar]
- 8.Richards JM, Shaw CA, Lang NN, et al. In vivo mononuclear cell tracking using superparamagnetic particles of iron oxide: feasibility and safety in humans. Circ Cardiovasc Imaging. 2012;5(4):509–517. doi: 10.1161/CIRCIMAGING.112.972596 [DOI] [PubMed] [Google Scholar]
- 9.Peng X, Li C, Bai Y, et al. Noninvasive evaluation of the migration effect of transplanted endothelial progenitor cells in ischemic muscle using a multimodal imaging agent. Int J Nanomedicine. 2018;13:1819–1829. doi: 10.2147/IJN.S152976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El-Said MM, Emile SH. Cellular therapy: A promising tool in the future of colorectal surgery. World J Gastroenterol. 2019;25(13):1560–1565. doi: 10.3748/wjg.v25.i13.1560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arbab AS, Pandit SD, Anderson SA, et al. Magnetic resonance imaging and confocal microscopy studies of magnetically labeled endothelial progenitor cells trafficking to sites of tumor angiogenesis. Stem Cells. 2006;24(3):671–678. doi: 10.1634/stemcells.2005-0017 [DOI] [PubMed] [Google Scholar]
- 12.Wang XY, Ju S, Li C, et al. Non-invasive imaging of endothelialprogenitor cells in tumor neovascularization using a novel dual-modalityparamagnetic/near-infrared fluorescence probe. PLoS One. 2012;7(11):e50575. doi: 10.1371/journal.pone.0050575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lyden D, Hattori K, Dias S, et al. Impaired recruitment of bone-marrow-derived endothelial and hematopoietic precursor cells blocks tumor angiogenesis and growth. Nat Med. 2001;7(11):1194–1201. doi: 10.1038/nm1101-1194 [DOI] [PubMed] [Google Scholar]
- 14.Chen J, Jia ZY, Ma ZL, et al. In vivo serial MR imaging of magnetically labeled endothelial progenitor cells homing to the endothelium injured artery in mice. PLoS One. 2011;6(6):e20790. doi: 10.1371/journal.pone.0020790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matsuda T, Kuwana M, Aomizu T, et al. Surface design for in situ capture of endothelial progenitor cells: VEGF-bound surface architecture and behaviors of cultured mononuclear cells. J Biomed Mater Res B Appl Biomater. 2013;101(1):50–60. doi: 10.1002/jbm.b.32812 [DOI] [PubMed] [Google Scholar]
- 16.Shapiro EM, Skrtic S, Sharer K, et al. MRI detection of single particles for cellular imaging. Proc Natl Acad Sci USA. 2004;101(30):10901–10906. doi: 10.1073/pnas.0403918101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ju S, Teng GJ, Lu H, et al. In vivo MR tracking of mesenchymal stem cells in rat liver after intrasplenic transplantation. Radiology. 2007;245(1):206–215. doi: 10.1148/radiol.2443061290 [DOI] [PubMed] [Google Scholar]
- 18.Sieghart W, Hucke F, Peck-Radosavljevic M. Transarterial chemoembolization: modalities, indication, and patient selection. J Hepatol. 2015;62(5):1187–1195. doi: 10.1016/j.jhep.2015.02.010 [DOI] [PubMed] [Google Scholar]
- 19.Chung GE, Lee JH, Kim HY, et al. Transarterial chemoembolization can be safely performed in patients with hepatocellular carcinoma invading the main portal vein and may improve the overall survival. Radiology. 2011;258(2):627–634. doi: 10.1148/radiol.10101058 [DOI] [PubMed] [Google Scholar]
- 20.Liang LJ, Hu WJ, Yin XY, et al. Adjuvant intraportal venous chemotherapy for patients with hepatocellular carcinoma and portal vein tumor thrombi following hepatectomy plus portal thrombectomy. World J Surg. 2008;32(4):627–631. doi: 10.1007/s00268-007-9364-0 [DOI] [PubMed] [Google Scholar]