Abstract
Background: Health literacy (HL) could influence self-care behaviors and further affect HbA1c values. Understanding the mechanism relationships between HL, self-care behaviors and HbA1c could provide the valuable knowledge for developing evidence-based interventions in diabetic patients. In this study, we hypothesized that HL and its subscales would be related to self-care behaviors and that HL would be indirectly related to glycemic control (HbA1c) via relations with self-care behaviors among diabetes patients.
Methods: This cross-sectional study was performed on 300 patients with type 2 diabetes referred to five educational hospitals affiliated to Shahid Beheshti University of Medical Sciences in 2018. The Persian version of Functional, Communicative, and Critical Health Literacy (FCCHL) questionnaire and the Summary of Diabetes Self-Care Activities (SDSCA) questionnaire were used. Also, recent HbA1c values were extracted from patients’ medical records. Structural equation modeling (SEM) was also used to investigate the relationships between the variables.
Results: The SEM results showed the direct standardized path of the total HL score, functional HL, communicative HL and critical HL on HbA1c were nonsignificant in the model with mediator. While the indirect effect of the total HL score (β = −0.24, P=0.042), functional HL (β = −0.15, P=0.01), communicative HL (β = −0.16, P=0.01) and critical HL (β = −0.22, P=0.03) on HbA1c through the mediation of self-care behaviors were significant.
Conclusion: The results of this study indicated that HL and particularly critical HL are significant factors in reducing HbA1c in patients with type 2 diabetes through the mediation of self-care behaviors.
Keywords: type 2 diabetes, health literacy, self-care, glycemic control
Background
Health literacy (HL) covers a set of skills that people need to effectively apply in health-care settings.1 HL has different dimensions, so Nutbeam has introduced a clear and tangible framework for this concept, which includes three levels:functional, communicative and critical.2 In fact, the functional HL is the most basic level including reading and writing skills which allows individuals to function effectively in everyday situations.2 The communicative HL is an advanced skill that allows individuals to extract information and their related meanings from multiple communication channels and put them into practice for changing conditions.2 Critical HL refers to more advanced skills that are needed to analyze information and use knowledge in order to apply more control on life events and situations.2,3 Over the past few decades, increasing attention has been paid to the concept of HL with an increasing emphasis on personal responsibility for maintaining and promoting health and self-management in chronic diseases,2,4,5 especially diabetes.6,7
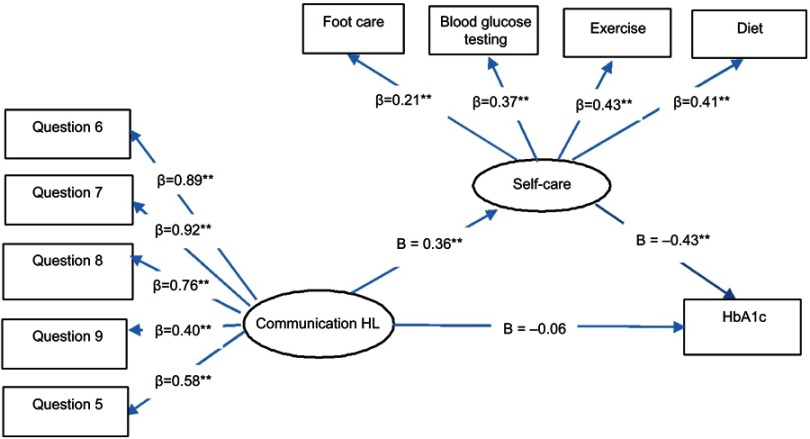
Figure 2.
Standardized parameter estimates of the final structural model 2. *P<0.05 **P<0.01.
Abbreviations: HL, health literacy; HbA1c, glycated hemoglobin.
Figure 3.
Standardized parameter estimates of the final structural model 3. *P<0.05 **P<0.01.
Abbreviations: HL, health literacy; HbA1c, glycated hemoglobin.
Type 2 diabetes mellitus is a common disease with high morbidity and mortality. The number of diabetes patients is increasing and is estimated that there will be 300 million diabetes people by 2025.8 The prevalence of diabetes in Iran is 3.0, 5.8, 10.8, and 14.0% in men and 3.0, 7.0, 14.0, and 19.4% in women aged 25–34, 35–44, 45–54, and 55–64 years, respectively.9
Achieving goals such as glycemic control which includes fasting blood glucose and glycosylated hemoglobin (HbA1c) is recommended to reduce mortality and economic costs associated with diabetes.10 Because of that, identifying the factors and pathways to the HbA1c values is crucial. Nevertheless, there are limited studies for understanding the pathways, or potential mechanisms, through which HL influences HbA1c. Powell et al reported that low levels of HL were associated with poor HbA1c and poor diabetes knowledge in patients with type 2 diabetes.11 Also, a systematic review study showed the relationship between HL and HbA1c.12 Some studies showed that a high level of HL had been associated with better HbA1c.13 In addition, other studies reported that HL had an indirect effect on HbA1c, and no direct relationship was found between them.14,15 In the study by Bains and Egedel , there was no relationship between HL and HbA1c.16 Whilemost studies have shown that several psychosocial factors, such as self-care behaviors, commonly influence the HbA1c values.14,17 Self-care is a process in which the patients use their knowledge and skills to carry out recommended behaviors.18 Therefore, not only patients should be able to obtain sufficient information about their disease and how to take care of themselves, but also they should be able to use their knowledge in different conditions and situations.18 Self-care behaviors among patients with diabetes include regularly monitoring blood glucose, adherence to a healthy and balanced diet, being physically active, compliance to drug therapy, and foot care.19 In the study of Gao et al, diabetes self-care had a direct effect on HbA1c.17 In the study of Jutterström et al, self-care education reduced the HbA1c values in diabetes patients.20
HL could influence self-care behaviors and further affect the HbA1c values. Understanding the mechanism of relationships between HL, self-care behaviors, and HbA1c could provide the valuable knowledge for developing evidence-based interventions in diabetes patients. Brega et al assessed a theoretical structure proposing that knowledge and behavior (diet, physical activity, and self-monitoring of blood glucose) mediate the relationship between HL and glycemic control. They showed that knowledge is the main mediator between HL and A1c because after including knowledge in the model, the behavior was no longer significant.21 The mediation effect of self-care in relationship between HL and HbA1c was assessed by Osborn et al.1 They showed that there is no direct relationship between HL and self-care or glycemic control. But, HL has an indirect effect on diabetes self-care and glycemic control through its association with social support. Also, Lee et al assessed the pathways of HL, self-efficacy, and self-care behaviors to glycemic control. HL relatively influenced glycemic control through self-efficacy and self-care behaviors in their study.15 But, to the best of our knowledge, no study has assessed the mediating role of self-care between HL subscales and glycemic control.
Based on the conceptualization of this framework, we hypothesized that among diabetes patients HL would be directly related to self-care behaviors and indirectly related to glycemic control via relation with self-care behaviors. Also, assessing HL beyond functional, communicative and critical literacy may help clarify how HL influences glycemic control through mediation of self-care behaviors in diabetes patients.
Methods
This cross-sectional study was performed on patients with type 2 diabetes referred to five educational hospitals affiliated to Shahid Beheshti University of Medical Sciences from May to September 2018. The inclusion criteria were ability to read and communicate. In addition, the patients were not included in the study if they had mental or cognitive disorders. Exclusion criteria included pregnancy and incomplete questionnaires. The patients were selected from each hospital by convenience sampling method. The majority of patients agreed to participate (94.2%). Finally, after exclusion of incomplete questionnaires, the sample included 300 patients with type 2 diabetes.
The anonymous self-administered questionnaires including demographic questionnaire, HL questionnaire, and self-care questionnaire were used to collect data. Patients completed all questionnaires at the same time. The demographic questionnaire consisted of age, sex, educational status, economic status, diabetes duration, side effects. A Persian version of the Functional Communicative and Critical Health Literacy scale (FCCHL) by Ishikawa22 was used to assess HL skills in patients with type 2 diabetes. This questionnaire consists of 14 questions with subscales of functional, communicative, and critical levels. The response to questions based on the 4-point Likert scale (never =1, rarely =2, sometimes =3, often =4) had been evaluated. At the functional, communicative and critical subscale, there are 5, 5 and 4 questions, respectively. The higher scores of this questionnaire shows higher HL. Cronbach’s alpha was 0.92 for total scale in our sample. Another questionnaire was a Persian version of the Summary of Diabetes Self-Care Activities (SDSCA) that was designed by Toobert et al.23 This questionnaire with 11-items evaluates the patients’ self-care over the past 7 days, covering the various aspects of self-care behaviors of patients with diabetes including diet (fourquestions), exercise (two questions), blood glucose test (twoquestions), foot care (two questions), and smoking (onequestion). Also, the higher scores of this questionnaire shows higher positive self-care behaviors. Cronbach’s alpha was 0.82 for total scale in our sample. The validity and reliability of Persian version of FCCHL24 and SDSCA25 questionnaires were assessed in Iranian studies. The recent HbA1c values were extracted from patients’ medical records for all patients who had completed the questionnaires.
Statistical analysis
In this study four hypotheses were tested using the structural equation modeling (SEM). In hypothesis 1, the role of mediating self-care between total HL score and HbA1c was assessed. In hypotheses 2–4, the role of mediating self-care between subscales of HL and HbA1c was assessed. In each model 1–4 (linked to hypotheses 1–4), the variables of HL or its subscales and self-care behaviors were considered as latent variables and HbA1c was considered as observed variable. Firstly, the correlations analysis between the variables was performed with the Pearson method. Then, a two-step procedure introduced by Anderson and Gerbing for analyzing the mediation effect was employed.26 In this procedure, in the first step, the measurement model of the latent variables was tested to show the extent to which each latent variable was represented by its indicators. In the second step, if the confirmatory measurement model in prior step is accepted, the structural model will be tested. The analysis was conducted in Mplus version 7. A model in both steps was considered a good fit if (1) chi-squared statistic divided by degree of freedom was less than 3;(2) the root mean square error of approximation (RMSEA) was less than 0.08; (3) comparative fit index (CFI);and (4) Tucker–Lewis index (TLI) was more than 0.9.27
Ethical statement
The study protocol was approved by the Ethics Review Committee of Shahid Beheshti University of Medical Sciences. All questionnaires were anonymous and patients were voluntary. All patients also signed a consent form.
Results
The mean age of diabetes patients was 58.70±14.69, of which 53.6% were women; 82.8% of the patients had less than high school education or had high school diploma and 17.2% had a university degree; 30.4% of the patients had low income, 61.6% had average income and 8% had high income. 30.4% of the patients had duration of diabetes for 5 years or less and 69.6% had for over 5 years. 33.2% of the patients did not report any side effects of diabetes, and 66.8% had at least one of the diabetes complications including retinopathy, nephropathy and neuropathy. 46% of the patients reported using ''other'' drugs, 50.4% using insulin and others both of them. In this study, the relationships between demographic variables and HL, subscales of HL, self-care, and HbA1c were investigated, and none of these variables had a significant relationship with demographic variables.
Descriptive statistics and correlation coefficients
The mean and standard deviation of total HL score, functional HL, communicative HL, critical HL, self-care and HbA1c as well as the correlation among them were presented in Table 1. The results showed that HL and its subscales were positively correlated with self-care. By contrast, HbA1c was negatively correlated with HL and its subscales and also self-care.
Table 1.
Descriptive statistics and correlations for all variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1 Total HL score | – | – | – | – | – | – |
| 2 Functional HL | 0.83** | – | – | – | – | – |
| 3 Communicative HL | 0.80** | – | – | – | – | – |
| 4 Critical HL | 0.69** | – | – | – | – | – |
| 5 Self-care | 0.28** | 0.16* | 0.21** | 0.32** | – | – |
| 6 HbA1c | −0.27** | −0.17* | −0.22** | −0.31** | −0.21** | – |
| Mean | 2.65 | 2.67 | 2.55 | 2.75 | 3.55 | 7.85 |
| SD | 0.77 | 1.25 | 0.83 | 0.82 | 1.12 | 1.97 |
Notes: *P<0.01; **P<0.001.
Abbreviations: HL, health literacy; HbA1c, glycated hemoglobin.
Measurement model
Confirmatory factor analysis (CFA) was tested for model 1–4 to assess whether the measurement model fits the sample data adequately or not. The initial test of the measurement model 1–4 revealed a satisfactory fit. All the factor loadings for the indicators on the latent variables were significant (P<0.001), except the smoking variable for self-care latent variable. Because of that, this variable was omitted from the measurement model nested in the structural equation model.
Structural model
The hypothesized models 1–4 were tested using SEM. For assessing the mediation effect of self-care in each model, first, the direct effect of HL and its subscales on HbA1c without mediator was tested. Then, in the model containing the self-care (mediator), a direct path from HL and its subscales to HbA1c was tested.
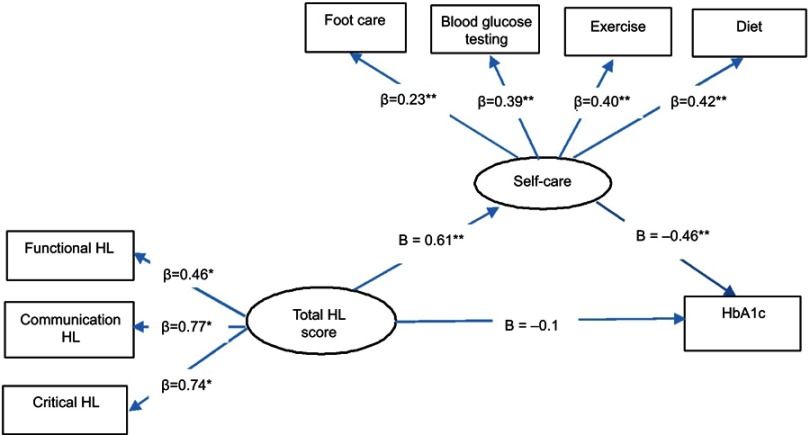
The results showed that the direct standardized path of total HL score on HbA1c without mediator (β = - 0.31,P<0.001) was significant. But the direct standardized path of total HL score on HbA1c with mediator (β = −0.10, P=0.47) was nonsignificant. Also, the indirect standardized effect of total HL score on HbA1c through the mediation of self-care was statistically significant (β = −0.24, P=0.042). The total effect of total HL score on HbA1c was statistically significant (β = −0.34, P<0.001) (Table 2). The results showed a good fit of the model 1 (chi-squared statistic divided by degree of freedom =2.66; RMSEA =0.04; CFI =0.97 and TLI =0.95).
Table 2.
Relationship between HL and its subscales with HbA1c mediated by self-care
| β | SEM (β) | P-value | |
|---|---|---|---|
| Total HL score (Model 1) | |||
| Direct effect | |||
| Total HL score → HbA1c | −0.1 | 0.14 | 0.47 |
| Total HL score → Self-care | 0.61 | 0.10 | <0.001 |
| Self-care → HbA1c | −0.39 | 0.16 | 0.01 |
| Indirect effect | |||
| Total HL score → HbA1c | −0.24 | 0.11 | 0.042 |
| Total effect | |||
| Total HL score → HbA1c | −0.34 | 0.68 | <0.001 |
| Functional HL (Model 2) | |||
| Direct effect | |||
| Functional HL → HbA1c | −0.02 | 0.08 | 0.82 |
| Functional HL → Self-care | 0.33 | 0.10 | 0.001 |
| Self-care → HbA1c | −0.46 | 0.10 | <0.001 |
| Indirect effect | |||
| Functional HL → HbA1c | −0.15 | 0.06 | 0.01 |
| Total effect | |||
| Functional HL → HbA1c | −0.17 | 0.06 | 0.006 |
| Communicative HL (Model 3) | |||
| Direct effect | |||
| Communicative HL → HbA1c | −0.06 | 0.08 | 0.46 |
| Communicative HL → Self-care | 0.36 | 0.10 | <0.001 |
| Self-care → HbA1c | −0.43 | 0.11 | <0.001 |
| Indirect effect | |||
| Communicative HL → HbA1c | −0.16 | 0.06 | 0.01 |
| Total effect | |||
| Communicative HL → HbA1c | −0.22 | 0.06 | <0.001 |
| Critical HL (Model 4) | |||
| Direct effect | |||
| Critical HL → HbA1c | −0.09 | 0.12 | 0.44 |
| Critical HL → Self-care | 0.59 | 0.09 | <0.001 |
| Self-care → HbA1c | −0.38 | 0.14 | 0.01 |
| Indirect effect | |||
| Critical HL → HbA1c | −0.22 | 0.10 | 0.03 |
| Total effect | |||
| Critical HL → HbA1c | −0.31 | 0.06 | <0.001 |
Abbreviations: SEM, structural equation modelling; HL, health literacy; HbA1c, glycated hemoglobin.
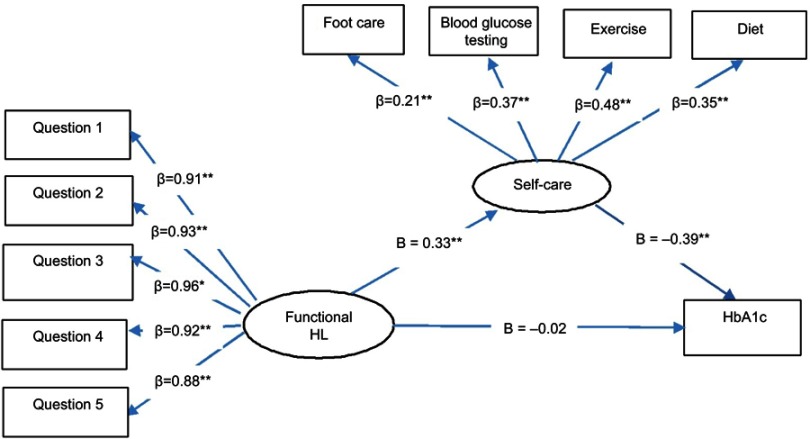
The direct standardized path of functional HL on HbA1c without mediator (β = –0.17, P=0.006) was significant. The results of Table 2 showed that the direct path of functional HL on HbA1c with mediator (β = –0.02, P=0.82) was nonsignificant. But the indirect effect of functional HL on HbA1c through the mediation of self-care (β = –0.15, P=0.01) and the total effect of functional HL on HbA1c (β = –0.17, P=0.006) were statistically significant. The fit indices of the model 2 were chi-squared statistic divided by degree of freedom =2.24; RMSEA =0.071; CFI =0.98 and TLI =0.97. Then, the hypothesized model 2 fitted the data well.
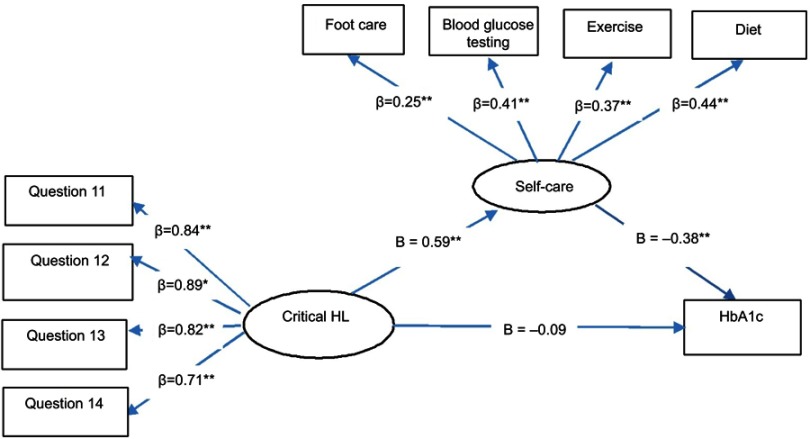
The direct standardized path of communicative HL on HbA1c without mediator (β = –0.22, P<0.001) was significant. Furthermore, the direct standardized path of critical HL on HbA1c without mediator (β = –0.31, P<0.001) was significant. But the direct effects of communicative HL (β = –0.06, P=0.46) and critical HL (β = –0.09, P=0.44) on HbA1c with mediator were nonsignificant. The indirect effects of communicative HL (β = –0.16, P=0.01) and critical HL (β = –0.22, P=0.03) on HbA1c were significant (Table 2). The third and fourth SEM showed a good fit of the model 3 (chi-squared statistic divided by degree of freedom =1.32; RMSEA =0.03; CFI =0.99 and TLI =0.98) and model 4 (chi-squared statistic divided by degree of freedom =2.74; RMSEA =0.08; CFI =0.92 and TLI =0.90).
Figures 1–4 show all of the observed variables significantly loaded on their latent variable in all models, supporting the measurement model of each latent variable. Furthermore, the standardized parameter estimates of the direct pathways between variables were shown.
Figure 1.
Standardized parameter estimates of the final structural model 1. *P<0.05, **P<0.01.
Abbreviations: HL, health literacy; HbA1c, glycated hemoglobin.
Figure 4.
Standardized parameter estimates of the final structural model 4. *P<0.05 **P<0.01.
Abbreviations: HL, health literacy; HbA1c, glycated hemoglobin.
Discussion
The results of our study showed that diabetes patients had moderate HL, with the best on critical HL, followed by functional and communicative HL. Our findings were consistent with findings of the study of Heijmans et al that patients in the Netherlands experienced their HL as quite good.7 Moreover, self-care of our patients was high indicating participants performed most of the self‐care tasks about 4 days a week and this was consistent with other Iranian studies for diabetes patients.28,29
In addition, the results showed that self-care is full mediation between HL and HbA1c, because this mediator accounts for the relationship between HL and HbA1c by reducing its relationship to nonsignificance. Hence, HL indirectly affects HbA1c through the mediation of self-care behaviors. In other words, HL has a crucial role for increasing self-care behaviors and glycemic control for diabetes patients. Osborn et al assessed the relationships between HL, diabetes self-care, and glycemic control in diabetes patients. They suggested that HL has an indirect effect on glycemic control through mediating of social support.1 Hence, HL has a major role for successful care in diabetes, because individuals with inadequate HL have problems with interactive communications. Hence, by increasing HL the complications of diabetes such as retinal damage and blindness could be controlled. Furthermore, other studies showed that low HL is linked to low use of preventive care,30,31 poor health status,32,33 and poor glycemic control.34,35 In this regard, nursing and health schools could help to improve HL by considering educating people in the community about health in chronic diseases such as diabetes. In addition, these findings offer significant insights concerning the design of interventions especially in low-income countries.
Based on our knowledge, the role of self-care mediation between subscales of functional, communicative, and critical HL and HbA1c was assessed in this study for the first time. The self-care had a full mediation role in relationship between functional, communicative, and critical HL and HbA1c, although the factor of critical HL was found to accountfor a more indirect effect on HbA1c, followed by communicative and functional HL. Heijmans et al examined the association between HL and self-management and found that communicative and critical HL play more of a role in successful self-management than functional HL.7 Hence, our findings were consistent with findings of the study of Heijmans et al that both critical and communicative skills play a more important role in successful glycemic control than functional skills. Therefore, for designing evidence-based interventions, critical and communicative HL should be considered more than functional HL in influencing glycemic control.
In the present study, there was no direct relationship between HL and its subscales and HbA1c in the model with the mediator. This finding was consistent with the conceptual framework of Paasche-Orlow and Wolf,36 Osborn et al1 and Bains et al,16 that HL did not have a direct effect on glycemic control.
In the present study, there were significant relationships between HL and its subscales and self-care. In the study by Lee et al, there was a significant indirect relationship between HL and self-care.15 In the study of Brega et al, significant relationships between HL and healthy food consumption, unhealthy food consumption and self-monitoring of blood glucose were reported.21 While Lai et al reported that self-management in diabetes was associated with critical and communicative HL, no association was reported with functional HL.5
Moreover, in the present study, there was a significant inverse correlation between self-care and the HbA1c variable such that, as self-care increasesthe HbA1c variable decreases. Hence, self-care is very important in managing diabetes. Toimprove self-care skills, patients need to enhance their knowledge and change their attitudes towards diabetes. In this regard, to strengthen the health-care system of the country, health promotion programs can focus more on self-care for patients; this goal can merely be achieved by collaboration of various organizations like the mass media that is considered one of the most significant health information sources for the majority of people.
There were limitations to our study that should be mentioned. First, using the self-report method as part of the data collection method could be a limitation of this research. However, using this method in such studies is inevitable and may lead to a bias for the “report of the researcher” by the audience. Therefore, anonymous questionnaires were used to minimize this bias. Second, we did not collect information on other variables that could explain the relationship between HL and HbA1c. Third, by the cross-sectional design, the causal conclusion was not possible; a longitudinal research is needed to investigate the effects of these constructs on changes in HL and HbA1c.
Conclusion
Our results confirmed that HL is directly associated with self-care and indirectly associated with HbA1c through the mediation of self-care. Hence, to improve the interaction between vulnerable patients and health systems, HL could be one of the main goals of optimizing care in diabetes.
Acknowledgments
The research team should like to thank Student Research Committee of Shahid Beheshti University of Medical Sciences for supporting this study. They would also like to thank to the study participants.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Osborn CY, Bains SS, Egede LE. Health literacy, diabetes self-care, and glycemic control in adults with type 2 diabetes. Diabetes Technol Ther. 2010;12:913–919. doi: 10.1089/dia.2010.0058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15:259–267. doi: 10.1093/heapro/15.3.259 [DOI] [Google Scholar]
- 3.Bailey SC, Brega AG, Crutchfield TM, et al. Update on health literacy and diabetes. Diabetes Educ. 2014;40:581–604. doi: 10.1177/0145721714540220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67:2072–2078. doi: 10.1016/j.socscimed.2008.09.050 [DOI] [PubMed] [Google Scholar]
- 5.Lai AY, Ishikawa H, Kiuchi T, Mooppil N, Griva K. Communicative and critical health literacy, and self-management behaviors in end-stage renal disease patients with diabetes on hemodialysis. Patient Educ Couns. 2013;91:221–227. doi: 10.1016/j.pec.2012.12.018 [DOI] [PubMed] [Google Scholar]
- 6.Kim S, Love F, Quistberg DA, Shea JA. Association of health literacy with self-management behavior in patients with diabetes. Diabetes Care. 2004;27:2980–2982. [DOI] [PubMed] [Google Scholar]
- 7.Heijmans M, Waverijn G, Rademakers J, van der Vaart R, Rijken M. Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management. Patient Educ Couns. 2015;98:41–48. doi: 10.1016/j.pec.2014.10.006 [DOI] [PubMed] [Google Scholar]
- 8.Amos AF, McCarty DJ, Zimmet P. The rising global burden of diabetes and its complications: estimates and projections to the year 2010. Diabetic Med. 1997;14:S7–S85. [PubMed] [Google Scholar]
- 9.Esteghamati A, Gouya MM, Abbasi M, et al. Prevalence of diabetes and impaired fasting glucose in the adult population of Iran: national survey of risk factors for non-communicable diseases of Iran. Diabetes Care. 2008;31:96–98. doi: 10.2337/dc07-0959 [DOI] [PubMed] [Google Scholar]
- 10.Association AD. Standards of medical care in diabetes—2012. Diabetes Care. 2012;35:S11–S63. doi: 10.2337/dc12-s011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Powell CK, Hill EG, Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ. 2007;33:144–151. doi: 10.1177/0145721706297452 [DOI] [PubMed] [Google Scholar]
- 12.Berkman ND, Sheridan SL, Donahue KE, et al. Health literacy interventions and outcomes: an updated systematic review. Evid Rep Technol Assess (Full Rep). 2011;199:941. [PMC free article] [PubMed] [Google Scholar]
- 13.Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006;121:245–254. doi: 10.1177/003335490612100305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Osborn CY, Cavanaugh K, Wallston KA, Rothman RL. Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun. 2010;15:146–158. doi: 10.1080/10810730.2010.499980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee Y-J, Shin S-J, Wang R-H, Lin K-D, Lee Y-L, Wang Y-H. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ Couns. 2016;99:287–294. doi: 10.1016/j.pec.2015.08.021 [DOI] [PubMed] [Google Scholar]
- 16.Bains SS, Egede LE. Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther. 2011;13:335–341. doi: 10.1089/dia.2010.0160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gao J, Wang J, Zheng P, et al. Effects of self-care, self-efficacy, social support on glycemic control in adults with type 2 diabetes. BMC Fam Pract. 2013;14:66. doi: 10.1186/1471-2296-14-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Breslow L. Self-Care Behavior. Encyclopedia of Public Health. MI: Gale Group Farmington Hills; 2002. [Google Scholar]
- 19.Tan MY, Magarey J. Self-care practices of Malaysian adults with diabetes and sub-optimal glycaemic control. Patient Educ Couns. 2008;72:252–267. doi: 10.1016/j.pec.2008.03.017 [DOI] [PubMed] [Google Scholar]
- 20.Jutterström L, Hörnsten Å, Sandström H, Stenlund H, Isaksson U. Nurse-led patient-centered self-management support improves HbA1c in patients with type 2 diabetes—A randomized study. Patient Educ Couns. 2016;99:1821–1829. doi: 10.1016/j.pec.2016.06.016 [DOI] [PubMed] [Google Scholar]
- 21.Brega AG, Ang A, Vega W, et al. Mechanisms underlying the relationship between health literacy and glycemic control in American Indians and Alaska natives. Patient Educ Couns. 2012;88:61–68. doi: 10.1016/j.pec.2012.03.008 [DOI] [PubMed] [Google Scholar]
- 22.Ishikawa H, Takeuchi T, Yano E. Measuring functional, communicative, and critical health literacy among diabetes patients. Diabetes Care. 2008;31:874–879. doi: 10.2337/dc07-1932 [DOI] [PubMed] [Google Scholar]
- 23.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–950. [DOI] [PubMed] [Google Scholar]
- 24.Reisi M, Mostafavi F, Javadzede H, Mahaki B, Sharifirad G, Tavassoli E. The functional, communicative, and critical health literacy (FCCHL) scales: cross-cultural adaptation and the psychometric properties of the Iranian version. Iran Red Crescent Med J. 2017;19:1–9. [Google Scholar]
- 25.Pourisharif H, Babapour J, Zamani R, Besharat MA, Mehryar AH, Rajab A. The effectiveness of motivational interviewing in improving health outcomes in adults with type 2 diabetes. Procedia Soc Behav Sci. 2010;5:1580–1584. doi: 10.1016/j.sbspro.2010.07.328 [DOI] [Google Scholar]
- 26.Fornell C, Yi Y. Assumptions of the two-step approach: reply to Anderson and Gerbing. Sociol Methods Res. 1992;20:334–339. doi: 10.1177/0049124192020003003 [DOI] [Google Scholar]
- 27.Wang J, Wang X. Structural Equation Modeling: Applications Using Mplus. West Sussex: John Wiley & Sons; 2012. [Google Scholar]
- 28.Shayeghian Z, Aguilar-Vafaie ME, Besharat MA, et al. Self-care activities and glycated haemoglobin in Iranian patients with type 2 diabetes: can coping styles and social support have a buffering role? Psychol Health. 2015;30:153–164. doi: 10.1080/08870446.2014.951651 [DOI] [PubMed] [Google Scholar]
- 29.Heidari S, Rezaei M, Sajadi M, Ajorpaz NM, Koenig HG. Religious practices and self-care in Iranian patients with type 2 diabetes. J Relig Health. 2017;56:683–696. doi: 10.1007/s10943-016-0320-x [DOI] [PubMed] [Google Scholar]
- 30.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among medicare enrollees in a managed care organization. Med Care. 2002;40:395–404. [DOI] [PubMed] [Google Scholar]
- 31.Howard DH, Sentell T, Gazmararian JA. Impact of health literacy on socioeconomic and racial differences in health in an elderly population. J Gen Intern Med. 2006;21:857–861. doi: 10.1111/j.1525-1497.2006.00530.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim SH. Health literacy and functional health status in Korean older adults. J Clin Nurs. 2009;18:2337–2343. doi: 10.1111/j.1365-2702.2008.02739.x [DOI] [PubMed] [Google Scholar]
- 33.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–1952. doi: 10.1001/archinte.165.17.1946 [DOI] [PubMed] [Google Scholar]
- 34.Tang YH, Pang SM, Chan MF, Yeung GS, Yeung VT. Health literacy, complication awareness, and diabetic control in patients with type 2 diabetes mellitus. J Adv Nurs. 2008;62:74–83. doi: 10.1111/j.1365-2648.2007.04526.x [DOI] [PubMed] [Google Scholar]
- 35.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. Jama. 2002;288:475–482. [DOI] [PubMed] [Google Scholar]
- 36.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31:S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19 [DOI] [PubMed] [Google Scholar]