Abstract
Background:
Theory-based tobacco use prevention programs in schools were implemented to evaluate the effectiveness of this peer-led intervention on tobacco use-related knowledge, attitude, normative beliefs, and intention to tobacco use of school children aged 14–17 years old.
Methods:
A school-based cluster randomized controlled intervention study was conducted among 1st, 2nd, and 3rd grade high school children in Sanandaj City, Iran. 4-h integrated tobacco use prevention program comprising of four structured modules was developed and delivered to the intervention group by trained peer educator. Outcome measures comprised changes in students’ smoking-related knowledge, attitude, normative beliefs, and intention to tobacco use from baseline to 6-month follow-up through validated anonymous questionnaire.
Results:
The present study showed an intervention effect on tobacco use-related knowledge, normative beliefs, and intention to tobacco use but not attitude. The results indicated that there was significant decrease in intention to tobacco use (P ≤ 0.013) observed after 6-month postintervention. The intervention module was also effective in improving smoking knowledge (P ≤ 0.001), normative beliefs with regard to perceived prevalence of cigarette smoking and water-pipe use among adults and adolescents (P ≤ 0.001) in intervention group 6-month postintervention.
Conclusions:
Participation in the peer-led education program to tobacco use prevention may have improvement in knowledge, normative beliefs, and intention to tobacco use. An implementation of the peer-led behavioral intervention components in the school setting may have a beneficial effect on public health by decreasing intention to tobacco use among nonsmoker adolescents.
Keywords: Cigarette smoking, high school children, intervention, peer-led intervention, tobacco use prevention, water-pipe use
Introduction
Smoking remains to be the single greatest preventable cause of mortality worldwide, being a major risk factor for a number of life-threatening diseases, including various cancers, cardiovascular diseases, and lung diseases.[1] Strategies to prevent uptake of adolescent tobacco use are still important to prioritize in public health. In Iran, prevalence of ever tobacco use among male and female adult aged 14–18 years old is 16.9% and 7.9%, respectively. Among this age range, 6.2% (8.97% of boys and 3.38% of girls) are current smokers.[2] Among adolescents in Iran, cigarette and water-pipe smoking are the most popular form of tobacco use.
Adolescent smoking is of particular concern due to the addictive nature of tobacco, the health risks associated with tobacco use, and the fact that it often acts as the gateway drug to future problem behaviors.[3,4] Early initiation and regular use of cigarettes are important predictors of substance use problems in young adulthood.[5] As the most adults begin smoking in their 10 years, schools have been used as appropriate setting for anti-smoking programs for teenagers.[6] As such, primary prevention efforts focusing on preventing initiation of tobacco use by young people have been recommended. Consequently, primary prevention in the school setting is considered to be one of the most proper strategies to prevent smoking.
Peer-led education in promoting health has become increasingly popular in school setting. Peer education has been proposed as a potentially effective method of undertaking smoking prevention work with adolescents. Several studies have shown that peer education can improve adolescent's knowledge and provide positive attitude and behavior.[7,8] The objectives of this study were to develop, implement, and evaluate the effectiveness of a peer-led behavioral intervention program among high school children that would improve knowledge, attitude, and normative beliefs relative to tobacco use and reduce intention to smoke among Iranian high school children.
Methods
Design and sample
This study, a cluster randomized intervention study, was conducted in male and female public high schools within the capital city of Kurdistan province, Iran. Eligible schools were those with minimum 2 classes in each grade. Four schools were randomly assigned by simple draw to the intervention group and four schools to the control group.
Out of 37 public high schools from two districts, two male and two female schools in each district were selected using simple random sampling. From the selected schools, in each district, one male and one female public high school were randomly assigned to intervention group that received peer education program and one male and one female public high school to control group that exposed to regular school program. All selected schools agreed to participate. All 1st, 2nd, and 3rd graders (14–17 year olds) in these schools were invited to participate.
The baseline data collection was conducted by trained assistants in December 2012 during a week before intervention program. The posttest took place in June 2013. Ethical approval and research clearance were obtained by ethics committee for research involving human subjects of UPM and Kurdistan state's general department of education.
Development of intervention
The peer-led behavioral intervention program module on tobacco use prevention was developed based on the result of focus group discussion (FGD) among 12 male and 10 female students. Questions for the FGD were semi-structured that included sociodemographic factors, smoking knowledge and opinion, smoking risk and protective factors, the most common reason for teenagers starting smoking, the prevalence of smoking among teens, and reasons for their estimation.
The development of final intervention module was based on literature review,[9] obtaining ideas from experts and findings from established FGD. It was simplified to the sociocultural settings of Iranians where emphasis was to encourage students not to smoke. The intervention was designed to improve harmful effects of smoking knowledge, increase negative attitude toward smoking, resist peer pressure, and increase ability to refuse smoking in different situations. The module consisted of four sessions of 4 h. The final content of the module was pretested. Two mock sessions were conducted to pilot test the intervention with the facilitators and group of students who were not involved in the actual study. It was a small trial in order to clarity of meaning, language, flow of contents, the time for presenting and suitability of the outcome measures.
Peer educators’ training
To transfer the module, two peer leaders in each intervention class were selected by the class teachers and school consolers from volunteer students based on their organization and oral expression ability, influence among students, and sense of responsibility. Then, peer leaders were attended 2 days off-school site training session (for male and female students separately) after obtaining their parent's permission. During 10-h exposure (5 h for each day), students were taught how to demonstration contained in the curriculum, how to do role play, teamwork, and other class activities. The trainers were the primary researchers and a team of external trainers who were experienced in substance abuse and adolescents’ health, led by health education specialists. The objectives of training were enhancing knowledge of harmful effects of smoking and the benefits of remaining “smoke free,” develop skills needed to promote smoking prevention among peers, and develop skills and practice intervening in everyday situations to encourage peers not to smoke. Four sessions were undertaken in each school during the 4-week period, at which the trainers offered support and monitored the peer supporters’ progress. All processes were conducted in a standard manner.
Description of the intervention
The intervention was made up of four sessions with each session lasting for about 1 h, implemented over a period of four consecutive weeks in a class room setting delivered by peer-led educators. The main objective of the intervention program was to educate the participants on the various tobacco-related products, harmful effects of tobacco use, and risk factors associated with smoking, improve self-esteem, develop personal skills such as assertive communication and refusal skills related to tobacco use, and equip them with the needed knowledge and skills to prevent from initiating tobacco use. Moreover, the intervention was aimed at changing the attitudes and social norms of the participants about smoking. The intervention was provided in the form of lecture note, case scenario, team work, role play, and group discussion. The respondents in control group were remained in the regular school curriculum that not contains any information regarding tobacco. During the trial, the control participants did not receive any smoking prevention education program but were tested at the beginning and the end of the study.
Outcome measures
A self-administered validated questionnaire was used in this study. It was administered at baseline and 6-month postintervention in class room in individual seats. To prevent social desirability and improve truthful responses, honesty was emphasized to the participants, and all questionnaires were anonymous, only 6-digit self-generated code was used to identify participants. The self-generated anonymous code was used to link pretest questionnaire with posttest evaluations while protecting the personal identification. The content of posttest was similar to the baseline questionnaire except that the questions on sociodemographics were omitted for the posttest in both the study and the control groups 6 months after intervention.
The questionnaire consisted of six sections, namely (a) demographic profile of the participants, (b) tobacco use-related knowledge, (c) tobacco use-related attitudes, (d) normative beliefs, (e) intention to tobacco use, and (f) smoking behavior in the past 30 days.
Smoking-related knowledge and health consequences of smoking were determined using thirteen questions that comprised from a combination of questions selected from the instruments in previous variety studies and modified to meet the objective of study.[10] It consisted of addictive substance in tobacco, health consequences of cigarette, and facts on water pipe. A score (0–13) representing evaluation of the student's smoking-related knowledge was then calculated.
Attitudes toward tobacco use were assessed using a 14-item scale. Most items were retrieved from Global Youth Tobacco Survey, EDDRA data bank, EU-Dap questionnaire (SDG). It consisted of perception of health, economy, and social consequences of tobacco use. Respondents was scored with values ranging from (1) strongly disagree to (5) strongly agree. This variable ranged from 14 to 70, with higher values representing a more negative attitude toward smoking.
Normative beliefs were measured through asking 4 questions on a 5-point scale ranging from all (1) to none (5) on which students had to estimate how many (a) “Adults in Iran” and (b) “Adolescents at their age” in Iran smoke cigarette and water pipe, separately.[11] Lower values represent that adolescents who believe the majority of people smoke cigarettes will tend to see smoking as normal activity.
A 4-point Likert-type scale was used to measure the intention to tobacco use (cigarettes and water pipe, separately) within next few months among nonsmokers. Responses were (1) very likely, (2) likely, (3) unlikely, and (4) very unlikely. This test produced a potential range of 2–8, where higher scores indicating less likely to intent to smoke within next few months. Outcome variables were compared at baseline and the effects of intervention on changes in outcome measures were determined after 6-month follow-up.
Statistical analysis
Data were analyzed using IBM SPSS Statistics version 21 (IBM Corp., Armonk, N.Y., USA). Descriptive statistics of frequencies, percentages, and means were used to describe the demographic profile of the participants as well as their smoking-related knowledge, attitudes toward smoking, normative beliefs, and intentions to smoke. The differences between the pre- and postintervention scores were established using paired t-test. The impact of the intervention on the outcomes was assessed using Generalized Estimating Equation with adjustment for baseline scores, smoking behavior and demographic factors and the use of robust standard errors to account for clustering of students within schools. For all the variables in the analysis, the alpha level at 0.05 was taken as the level of statistical significance.
Results
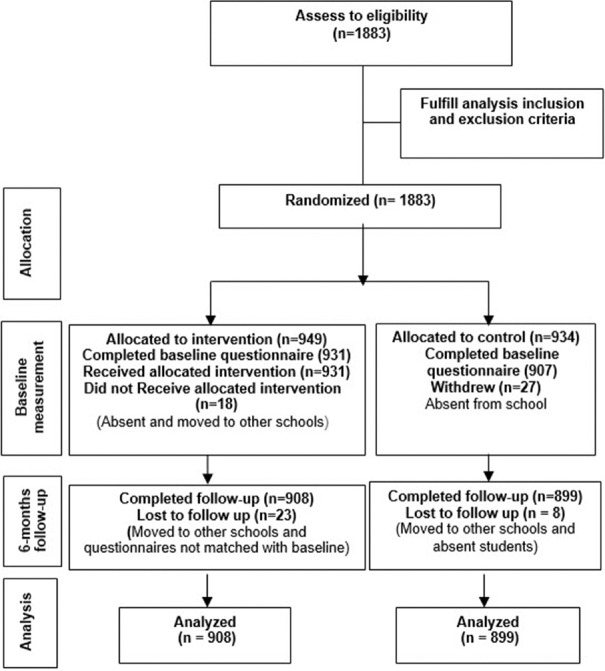
Consort flow diagram of the study is shown in Figure 1. A total of 1883 participants were enrolled in 8 selected schools, 949 participants were randomized to the intervention in four schools and 934 participants to the control group in four schools. During the baseline data collection, 931 (98.1%) and 907 (97.1%) participants turned out in the intervention and control group, respectively. Out of 1838 participants completed the questionnaire at baseline, 1807 respondents completed the questionnaire at 6 months post intervention giving up the response rate of 98.3%.
Figure 1.
Consort flow chart of intervention and control groups
Table 1 shows that the intervention and control groups did not differ with regard to baseline gender, age, living arrangement, father's education, mother's education, as well as average monthly pocket money.
Table 1.
Characteristics of the sample in intervention and control group at baseline
| Variable | Frequency (%) | Pa | |
|---|---|---|---|
| Intervention (n=908) | Control (n=899) | ||
| Gender | |||
| Male | 457 (50.3) | 452 (50.3) | 0.51 |
| Female | 451 (49.7) | 447 (49.7) | |
| Age (years) | |||
| Mean±SD | 15.05±0.79 | 15.13±0.85 | 0.06 |
| 95% CI | 15.00-15.11 | 15.07-15.18 | |
| Living arrangement | |||
| Both of parents | 831 (91.5) | 828 (92.1) | 0.08 |
| Mother/father only | 55 (6.1) | 35 (3.9) | |
| Grandparents/others | 22 (2.4) | 36 (4.0) | |
| Father’s education | |||
| No education | 110 (12.1) | 89 (9.9) | 0.18 |
| Primary level | 295 (32.5) | 278 (31.0) | |
| Middle level | 215 (23.7) | 200 (22.3) | |
| Secondary level | 160 (17.6) | 178 (19.9) | |
| College/university | 127 (14.0) | 151 (16.9) | |
| Mother’s education | |||
| No education | 303 (33.4) | 277 (30.9) | 0.10 |
| Primary level | 305 (33.7) | 317 (35.4) | |
| Middle level | 164 (18.1) | 137 (15.3) | |
| Secondary level | 85 (9.4) | 112 (12.5) | |
| College/university | 49 (5.4) | 53 (5.9) | |
| Pocket money (Rials/month) | |||
| <1,000,000 | 361 (42.2) | 303 (38.5) | 0.08 |
| 1,000,000-2,000,000 | 162 (18.9) | 159 (20.2) | |
| 2,000,001-3,000,000 | 135 (15.8) | 159 (20.2) | |
| ≥3,000,001 | 197 (23.0) | 167 (21.2) | |
aP value was calculated by Independent sample t-test, Chi-square or Fisher’s exact test between intervention and control groups. CI=Confidence interval, SD=Standard deviation
Table 2 compares the mean scores for smoking knowledge, attitude, normative beliefs, and intention to smoke and smoking behavior between the intervention and control groups at baseline. There was no significant difference in mean scores of smoking-related knowledge, attitude, normative belief, intention to tobacco use, and prevalence of smoking between the intervention and control groups at baseline.
Table 2.
Smoking-related knowledge, attitude, normative beliefs and intention and behavior between the intervention and control groups at baseline
| Outcome | Intervention | Control | Pa |
|---|---|---|---|
| Smoking-related knowledge (mean±SD) | 7.39±2.91 | 7.64±2.90 | 0.06 |
| Attitude toward smoking (mean±SD) | 56.59±7.11 | 56.90±7.28 | 0.38 |
| Normative beliefs (mean±SD) | 12.60±1.06 | 12.47±1.07 | 0.87 |
| Intention to tobacco use (mean±SD) | 7.05±1.35 | 6.99±1.30 | 0.08 |
| Past month smoking, n (%) | 60 (6.6) | 52 (5.8) | 0.26 |
aP value was calculated by independent sample t-test for knowledge, attitude, normative beliefs and intention, and the Fisher’s exact test of association for smoking behavior. SD=Standard deviation
Effect of the intervention on outcomes at 6-month follow-up
Effects of intervention programs on outcome measures at 6-month follow-up are presented in Table 3. The results for the test of the effectiveness of the intervention on each outcome were adjusted for school-specific covariates and the demographic variables of gender, age, living arrangement, father's education, mother's education, monthly pocket money, and smoking behavior. The results showed that there was a significant difference between intervention and control group on smoking-related knowledge (β ± standard error [SE] = 1.33 ± 0.13, P ≤ 0.001), normative beliefs (β ± SE = 0.69 ± 0.71, P ≤ 0.001), and intention to tobacco use (β ± SE = 0.17 ± 0.10, P = 0.013) after 6-month postintervention. The results indicated that was no significant difference between intervention and control group on attitude toward smoking after 6-month postintervention (β ± SE = 0.62 ± 2.84, P = 0.124).
Table 3.
Impact of the interventions on outcome measures, parameter estimates, and 95% confidence intervals from generalized estimating equation analyses
| Outcome measures | Main effect of intervention | |||
|---|---|---|---|---|
| Intervention | Control | β±SE | P | |
| Smoking-related knowledge (mean±SD) | ||||
| Baseline | 7.39±2.91 | 7.64±2.90 | 1.33±0.13 | <0.001* |
| Follow-up | 11.69±1.28 | 8.15±2.76 | ||
| Attitude toward smoking (mean±SD) | ||||
| Pretest | 56.59±7.11 | 56.90±7.28 | 0.62±2.87 | 0.124 |
| Posttest | 57.02±6.82 | 56.77±7.37 | ||
| Normative beliefs (mean±SD) | ||||
| Pretest | 12.60±1.06 | 12.47±1.07 | 0.69±0.71 | <0.001* |
| Posttest | 13.21±0.92 | 12.21±1.1 | ||
| Intention to tobacco use (mean±SD) | ||||
| Pretest | 7.05±1.35 | 6.49±1.30 | 0.17±0.10 | 0.013* |
| Posttest | 7.73±0.53 | 6.46±0.71 | ||
*Significant at P<0.05. SD=Standard deviation, SE=Standard error
Discussion
This study assessed the effectiveness of school-based intervention on tobacco use-related knowledge, attitude, normative beliefs, and intention to smoke. The intervention seems to have contributed to changes in the experimental students’ smoking-related knowledge. There was significant increase in knowledge score in the intervention group as compared to the control group. The reported increase in smoking related-knowledge in this study could be attributed to the inclusion of program activities related to the outcome. Similarly, a recent meta-analysis showed that 73% of 11 school-based smoking prevention programs resulted in significant improvement in participants’ knowledge about smoking.[12] This result is encouraging because according to Tobler et al.(2000), adolescents would refrain from smoking if they were provided with information about the harmful health effects of tobacco use.[13]
The intervention program did not significantly improve the anti-smoking attitudes of participants at 6-month follow-up in the intervention group compared to the control group. Conversely, desired positive changes in attitude were achieved in a study in Indonesia and another study in Taiwan.[14,15] The results of a study in Iran have found that stronger negative attitudes about tobacco were associated with lower to water pipe smoking.[16] In addition, the positive attitudes toward tobacco use and tobacco users were found to be related to an increased likelihood of tobacco use.[17,18]
At posttest, about 43% of the respondents in this study perceived that about half or more of their peers and 69% believed that about half or more of adults smoke cigarettes. Students of both groups showed about same level of normative belief score at baseline. At follow-up, compared with the control group, students in intervention group scored better in their estimation on prevalence of tobacco use among adults and peers. Therefore, the intervention program was effective on modify student's estimation of smoking prevalence in peer and adults. Teens typically overestimate how many of their peers are involved in substance abuse, which influences their own attitudes and behaviors. An investigation of early initiation of smoking among high school students revealed that high perceived prevalence of peer smoking predicted recent smoking. Subjective norm is a stronger predictor than the attitude to foresee the intention to refrain from water-pipe smoking among Iranian high school children.[19] Furthermore, perceived prevalence of smoking is associated with increased risk of smoking among adolescents.[20] However, the tendency for young people to overestimate the smoking prevalence of their peers suggests that associations made between perceived prevalence and smoking behavior should be treated carefully as they may be biased.
The findings of this study provide evidence that intervention programs significantly reduce nonsmoker students’ intention to smoke. The intervention group had a higher intention not to smoke than the control group. Many studies have demonstrated smoking intentions to be a strong predictor of future smoking behavior. This result was also supported by a systematic review.[21] They reported that school-based tobacco use prevention interventions are effective in reducing smoking initiation and intended smoking intentions in the short term. Similarly, the results of the study done by Joveyni et al. (2013) which determined the effect of health education programs using theory of planned behavior among Iranian male college students showed that there were significant differences between the mean score of intention to tobacco use in the experiment group compared with the control group after intervention.[22]
Limitations associated with the use of self-answered questionnaires need to be considered, which subjected the findings to self-report bias. Students may have given socially desirable answers, specifically regarding their smoking, especially among girls. Since sampling was done by schools (cluster sampling) in order to access students, certain disadvantages and limitations naturally occurred. Data from students associated with the same school are likely to be correlated because of exposure to the same social environment and sharing behaviors or opinions among students in the same school and therefore were not completely independent, which could have led to a decrease in the accuracy of the results. The fidelity of the intervention might have been compromised since only peer educators delivered the lessons.
Conclusions
The peer-led intervention programs highlight the positive impact on intention to tobacco use, smoking-related knowledge, correcting adolescents’ overestimates of tobacco use rates of adults and adolescents. A comparison of the pre- and posttest scores of the participants in intervention and control group reveals that there was significant decrease in the intention to tobacco use in the participants. This outcome could therefore be a protective factor in enabling them to overcome the temptation to smoke.
Based on the finding, this study has implications for both practice and further research. This study examined the outcomes at baseline and at 6-month follow-up, future studies will be stronger if utilize longer follow periods. It is important to assess long-term effects, identify delayed intervention effects that may not be observed within 6 months, and determine the sustainability of the intervention effects. Furthermore, on the basis of the findings of the present study, it can be recommended that long-term education program should be incorporated into the effective interventions to make students more sustainable.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelishadi R, Shahsanai A, Qorbani M, Esmaeil Motlagh M, Jari M, Ardalan G, et al. Tobacco use and influencing factors among Iranian children and adolescents at national and subnational levels, according to socioeconomic status: The Caspian-IV Study. Iran Red Crescent Med J. 2016;18:e21858. doi: 10.5812/ircmj.21858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Korhonen T, Levälahti E, Dick DM, Pulkkinen L, Rose RJ, Kaprio J, et al. Externalizing behaviors and cigarette smoking as predictors for use of illicit drugs: A longitudinal study among Finnish adolescent twins. Twin Res Hum Genet. 2010;13:550–8. doi: 10.1375/twin.13.6.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li H, Bu Q, Chen B, Shao X, Hu Z, Deng P, et al. Mechanisms of metabonomic for a gateway drug: Nicotine priming enhances behavioral response to cocaine with modification in energy metabolism and neurotransmitter level. PLoS One. 2014;9:e87040. doi: 10.1371/journal.pone.0087040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riala K, Hakko H, Isohanni M, Järvelin MR, Räsänen P. Teenage smoking and substance use as predictors of severe alcohol problems in late adolescence and in young adulthood. J Adolesc Health. 2004;35:245–54. doi: 10.1016/j.jadohealth.2003.08.016. [DOI] [PubMed] [Google Scholar]
- 6.Thomas RE, McLellan J, Perera R. School-based programmes for preventing smoking. Evid Based Child Health. 2013;8:1616–2040. doi: 10.1002/14651858.CD001293.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Campbell R, Starkey F, Holliday J, Audrey S, Bloor M, Parry-Langdon N, et al. An informal school-based peer-led intervention for smoking prevention in adolescence (ASSIST): A cluster randomised trial. Lancet. 2008;371:1595–602. doi: 10.1016/S0140-6736(08)60692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lotrean LM, Dijk F, Mesters I, Ionut C, De Vries H. Evaluation of a peer-led smoking prevention programme for Romanian adolescents. Health Educ Res. 2010;25:803–14. doi: 10.1093/her/cyq034. [DOI] [PubMed] [Google Scholar]
- 9.Whalen S, Splendorio D, Chiariello S. Tools for Teaching Health: Interactive Strategies to Promote Health Literacy and Life Skills in Adolescents and Young Adults. San Francisco: Jossey-Bass; 2007. pp. 1–31. [Google Scholar]
- 10.Faggiano F, Galanti MR, Bohrn K, Burkhart G, Vigna-Taglianti F, Cuomo L, et al. The effectiveness of a school-based substance abuse prevention program: EU-Dap cluster randomised controlled trial. Prev Med. 2008;47:537–43. doi: 10.1016/j.ypmed.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 11.Botvin GJ, Griffin KW, Diaz T, Ifill-Williams M. Drug abuse prevention among minority adolescents: Posttest and one-year follow-up of a school-based preventive intervention. Prev Sci. 2001;2:1–13. doi: 10.1023/a:1010025311161. [DOI] [PubMed] [Google Scholar]
- 12.Park E. School-based smoking prevention programs for adolescents in South Korea: A systematic review. Health Educ Res. 2006;21:407–15. doi: 10.1093/her/cyl038. [DOI] [PubMed] [Google Scholar]
- 13.Tobler NS, Roona MR, Ochshorn P, Marshall DG, Streke AV, Stackpole KM. School-based adolescent drug prevention programs: 1998 meta-analysis. J Prim Prev. 2000;20:275–336. [Google Scholar]
- 14.Tahlil T, Woodman RJ, Coveney J, Ward PR. The impact of education programs on smoking prevention: A randomized controlled trial among 11 to 14 year olds in Aceh, Indonesia. BMC Public Health. 2013;13:367. doi: 10.1186/1471-2458-13-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee PH, Wu DM, Lai HR, Chu NF. The impacts of a school-wide no smoking strategy and classroom-based smoking prevention curriculum on the smoking behavior of junior high school students. Addict Behav. 2007;32:2099–107. doi: 10.1016/j.addbeh.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 16.Karimy M, Niknami S, Heidarnia AR, Hajizadeh E, Shamsi M. Refusal self efficacy, self esteem, smoking refusal skills and water pipe (Hookah) smoking among Iranian male adolescents. Asian Pac J Cancer Prev. 2013;14:7283–8. doi: 10.7314/apjcp.2013.14.12.7283. [DOI] [PubMed] [Google Scholar]
- 17.Anjum Q, Ahmed F, Ashfaq T. Knowledge, attitude and perception of water pipe smoking (Shisha) among adolescents aged 14-19 years. J Pak Med Assoc. 2008;58:312–7. [PubMed] [Google Scholar]
- 18.Mohammadi M, Rampal L, Sidik SM, Ibrahim N, Rahman HA, Ghaleiha A. Prevalence and predictors of water pipe (Shisha) use among Iranian high school children. Malays J Med Health Sci. 2017;13:45–53. [Google Scholar]
- 19.Abedini S, MorowatiSharifabad M, Chaleshgar Kordasiabi M, Ghanbarnejad A. Predictors of non- hookah smoking among high-school students based on prototype/willingness model. Health Promot Perspect. 2014;4:46–53. doi: 10.5681/hpp.2014.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ellickson PL, Bird CE, Orlando M, Klein DJ, McCaffrey DF. Social context and adolescent health behavior: Does school-level smoking prevalence affect students’ subsequent smoking behavior? J Health Soc Behav. 2003;44:525–35. [PubMed] [Google Scholar]
- 21.Dobbins M, DeCorby K, Manske S, Goldblatt E. Effective practices for school-based tobacco use prevention. Prev Med. 2008;46:289–97. doi: 10.1016/j.ypmed.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 22.Joveyni H, Dehdari T, Gohari M. Water pipe smoking in the male college students: An education intervention using theory of planned behavior. J Res Health. 2013;3:497–503. [Google Scholar]