Abstract
Background:
Injury prevention neuromuscular training (NMT) programs reduce the risk for anterior cruciate ligament (ACL) injury. However, variation in program characteristics limits the potential to delineate the most effective practices to optimize injury risk reduction.
Purpose:
To evaluate the common and effective components included in ACL NMT programs and develop an efficient, user-friendly tool to assess the quality of ACL NMT programs.
Study Design:
Systematic review and meta-analysis.
Methods:
Study inclusion required (1) a prospective controlled trial study design, (2) an NMT intervention aimed to reduce incidence of ACL injury, (3) a comparison group, (4) ACL injury incidence, and (5) female participants. The following data were extracted: year of publication, study design, sample size and characteristics, and NMT characteristics including exercise type and number per session, volume, duration, training time, and implementer training. Analysis entailed both univariate subgroup and meta-regression techniques using random-effects models.
Results:
Eighteen studies were included in the meta-analyses, with a total of 27,231 participants, 347 sustaining an ACL injury. NMT reduced the risk for ACL injury from 1 in 54 to 1 in 111 (odds ratio [OR], 0.51; 95% CI, 0.37−0.69]). The overall mean training volume was 18.17 hours for the entire NMT (24.1 minutes per session, 2.51 times per week). Interventions targeting middle school or high school–aged athletes reduced injury risk (OR, 0.38; 95% CI, 0.24−0.60) to a greater degree than did interventions for college- or professional-aged athletes (OR, 0.65; 95% CI, 0.48−0.89). All interventions included some form of implementer training. Increased landing stabilization and lower body strength exercises during each session improved prophylactic benefits. A meta-regression model and simple checklist based on the aforementioned effective components (slope = −0.15, P = .0008; intercept = 0.04, P = .51) were developed to allow practitioners to evaluate the potential efficacy of their ACL NMT and optimize injury prevention effects.
Conclusion:
Considering the aggregated evidence, we recommend that ACL NMT programs target younger athletes and use trained implementers who incorporate lower body strength exercises (ie, Nordic hamstrings, lunges, and heel-calf raises) with a specific focus on landing stabilization (jump/hop and hold) throughout their sport seasons.
Clinical Relevance:
Clinicians, coaches, athletes, parents, and practitioners can use the developed checklist to gain insight into the quality of their current ACL NMT practices and can use the tool to optimize programming for future ACL NMT to reduce ACL injury risk.
Keywords: neuromuscular training, pediatric sports medicine, injury prevention, biomechanics, decision support
Knee injuries are the most common severe13 and season/ career-ending sport injury.72 The anterior cruciate ligament (ACL) sustains the majority of these traumatic knee injuries, and surgical reconstruction is the common treatment approach (ie, 80%).28 One ACL injury currently costs $38,000, which includes long-term costs; thus, the economic burden to society is substantial.42 Women’s basketball, soccer, gymnastics, and lacrosse are the highest risk sports for ACL injury.20,69 Women are approximately 3 times more likely than men to injure their ACL.20,58,62 ACL injuries often result in concomitant injury (meniscus 55%−65%, cartilage 16%−46%),32,77 which leads to a higher risk (4 times) for osteoarthritis,4,8,11,12,50 total knee replacement,68 and impaired knee-related quality of life at 5 to 25 years after injury.16 Risk for a second ACL injury is also substantial (ie, 10%), and if the athletes return to their preinjury sport, risk doubles (ie, 20%).5,38,75,76 The recovery time for ACL injury is approximately 1 year, and about 45% of athletes do not return to competitive sport.6,7,39 If athletes return to their respective sport, their performance is likely to decrease.30,39
Well-controlled neuromuscular training (NMT) for ACL injury prevention reduces the risk for such injury by roughly 50% in female athletes.46,61,66,67 Historically, NMT programs have included various modalities such as strength training, plyometrics, balance exercises, and stretching to manipulate muscle activation or imbalances. Numerous studies and simulations indicate that NMT is a cost-effective prevention strategy.36,41 However, NMT programs vary, thus warranting increased effort to determine the common and most effective components. In addition, to create useful best-practice guidelines, effective intervention components need to be explicitly documented, which has yet to be done through the use of robust quantitative and statistical methods.54 Thus, the goal of this study was to (1) determine the common and effective components of ACL NMT programs and (2) create an efficient, user-friendly tool to assess the quality of ACL NMT programs. This tool not only will provide transparent best-practice information regarding the most effective program components but also can be used as a feedback system to assess current programs or a decision support tool to develop effective ACL NMT programs in the future.
METHODS
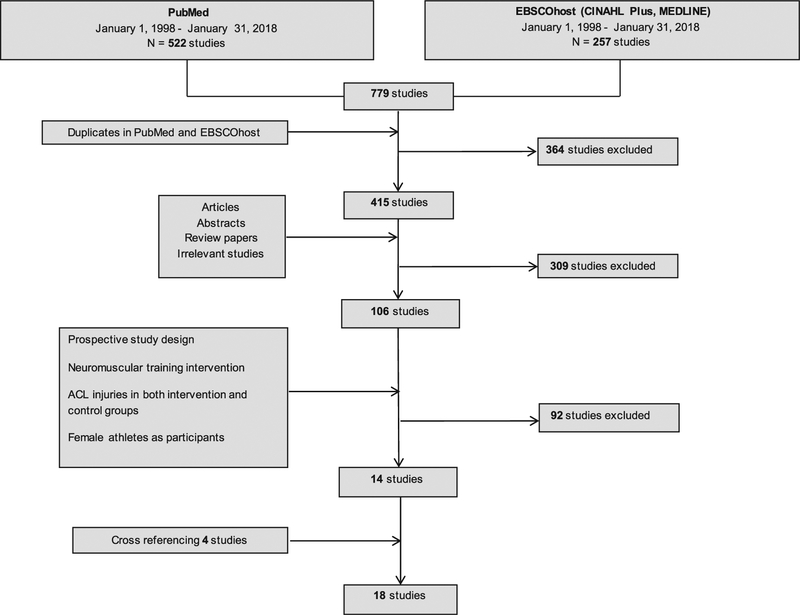
Search Methods for the Identification of Studies
A literature search was performed with PubMed and EBS-COhost (CINAHL Plus and MEDLINE), on January 31, 2018. The keyword search was performed with a combination of keywords related to ACL, knee, injury, prevention, neuromuscular, and training. Language was limited to English, and all participants were human. The following inclusion criteria were applied: (1) a prospective controlled trial study design was used, (2) an NMT intervention aimed to reduce ACL incidence was applied, (3) a comparison group was used, (4) the number of ACL injuries was reported, and (5) females were included as participants. Two authors (D.S. and E.J.P.) performed the literature search. Abstracts, posters, review papers, and irrelevant studies were excluded. When eligibility of certain studies was questionable, the 2 authors discussed and determined the status based on the 5 inclusion criteria. During the literature search, cross-referencing was performed when studies that met inclusion criteria cited other studies.
Data Extraction
The following information was extracted from each article identified for inclusion: year of publication, study design, sample size including number of ACL injuries, sample characteristics including age and sport, and NMT characteristics including exercise type and number per session, volume, duration, training time, and implementer training. The Physiotherapy Evidence Database (PEDro) scale was used to assess methodological quality and risk of bias. Data were independently extracted by 3 individuals (D.S., E.J.P., G.S.). Discrepancies between classifications or values were discussed and resolved between the extractors.
Statistical Analysis
The primary outcome of interest was ACL injury odds ratio (OR). To determine the most effective components of ACL NMT programs, both univariate subgroup and meta-regression techniques were used. Specifically, random-effects models (using restricted maximum likelihood estimators) were used to calculate the ORs and statistical parameters (95% CIs, regression slopes, and intercepts) for the various program characteristics.9,37 For univariate comparisons, only the exercises or components (eg, squat, calf raise, hip flexor stretch) that were included in at least 25% (k≥5) of the studies were included in the analysis in order to reduce biases associated with largely unequal sample sizes. Publication bias was assessed via regression tests for funnel plot asymmetry using standard error, sample size, and sample variance as predictors.15 All statistical calculations and analyses were performed by use of the metafor and meta packages with the statistical software environment R.
RESULTS
Overall Effects
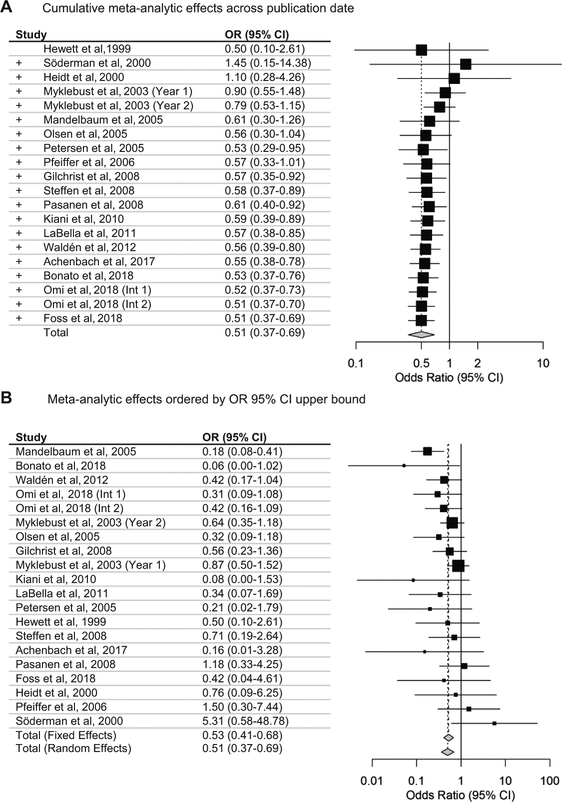
Eighteen studies were included in the analyses (Table 1 and Figure 1).‡‡ Because 2 studies had program changes after the first year/phase47,52 but reported injury outcomes for both years/phases, these studies were analyzed separately. Cumulative evidence gathered over time (from 1999 to the present) indicates that NMT has been an effective intervention to reduce ACL injury risk since approximately 2008 (Figure 2A). Specifically, Figure 2A shows how the accumulation of studies over time changes the effect estimate (eg, after each study is included, a new OR is calculated). As a whole, NMT reduced the risk for ACL injury from 1 in 54 to 1 in 111 (OR, 0.51; 95% CI, 0.37−0.69) (Figure 2B). Statistical heterogeneity (I2) for the random-effects model was 23.3% (Q19 = 24.81, P = .17). Because substantial heterogeneity was found in programming characteristics between studies (training exercises, target population, etc) and moderate statistical heterogeneity was noted, subgroup and meta-regression analyses were conducted. No significant publication bias or funnel plot asymmetry was found when standard error (Z = 0.92, P = .36), sample size (Z = −1.86, P = .06), and sample variance (Z = −1.07, P = .28) were used as predictors. Grouped ORs were similar between randomized trials (k = 11; OR, 0.54; 95% CI, 0.35−0.83) and nonrandomized trials (k = 9; OR, 0.46; 95% CI, 0.28−0.76). The average ± SD PEDro score across all studies was 5.45 ± 2.31 out of a possible score of 10. No significant meta-regression effects were found for the PEDro score on ACL injury risk (slope = −0.002; P = .98).
Table 1.
Individual Study Characteristics
| Lead Author (Year) | Study Design | Training: Noninjured/ Injured, n | Control: Noninjured/ Injured, n | Country: Level/Division | Participant Age, y | Sport Types | Total Training Time, ha | Total Training Sessionsa |
|---|---|---|---|---|---|---|---|---|
| Hewett (1999)24 | Prospective nonrandomized cohort | 364/2 | 458/5 | US: high school | Range 14–18 | Soccer, volleyball, and basketball | 13.4 | 18 |
| Söderman (2000)59 |
Prospective randomized controlled | 58/4 | 77/1 | Sweden: Divisions 2 and 3 | Mean 20.4 | Soccer | 22.5 | 108 |
| Heidt (2000)21 | Prospective randomized controlled | 41/1 | 250/8 | US: high school | Range 14–18 | Soccer | 21.8 | 30 |
| Myklebust (2003),47 year 1 |
Prospective nonrandomized observation-intervention | 832/23 | 913/29 | Norway: Divisions 1–3 | Range 21–22 | Handball | 13.8 | 55 |
| Myklebust (2003),47 year 2 |
Prospective nonrandomized observation-intervention | 833/17 | 913/29 | Norway: Divisions 1–3 | Range 21–22 | Handball | 13.8 | 55 |
| Mandelbaum (2005)40 |
Prospective nonrandomized cohort | 1879/6 | 3751/67 | US: Coast Soccer League (14- to 18- year-olds) | Range 14–18 | Soccer | 11.4 | 36 |
| Olsen (2005)51 | Prospective cluster randomized controlled | 805/3 | 769/9 | Norway: 16- to 17-y divisions | Range 16–17 | Handball | 13.5 | 45 |
| Petersen (2005)56 | Prospective matched cohort | 133/1 | 137/5 | Germany: semiprofessional and amateur | Mean ~19 | Handball | 9.8 | 59 |
| Pfeiffer (2006)57 | Prospective nonrandomized cohort | 574/3 | 859/3 | US: high school | Range 14–18 | Soccer, volleyball, and basketball | 10 | 30 |
| Gilchrist (2008)19 | Prospective cluster randomized controlled | 576/7 | 834/18 | US: college Division 1 | Mean 19.9 | Soccer | 11.4 | 36 |
| Steffen (2008)63 | Prospective block randomized controlled | 1073/4 | 947/5 | Norway: under 17 | Mean 15.4 | Soccer | 10 | 40 |
| Pasanen (2008)55 | Prospective cluster randomized controlled | 250/6 | 197/4 | Finland: top level | Mean 24 | Floorball | 12.4 | 42 |
| Kiani (2010)31 | Prospective cluster nonrandomized cohort | 777/0 | 724/5 | Sweden: various levels | Mean 15 | Soccer | 12.8 | 51 |
| LaBella (2011)34 | Prospective cluster randomized controlled | 735/2 | 749/6 | US: high school | Mean 16 | Soccer and basketball | 13.6 | 43 |
| Waldén (2012)74 | Prospective cluster randomized controlled | 2472/7 | 2071/14 | Sweden: under 14 to under 18 | Mean 14 | Soccer | 15 | 60 |
| Achenbach (2017)1 |
Prospective block randomized controlled |
98/0 | 76/2 | Germany: under 16 and under 18 | Range 13–18 | Handball | 13.9 | 56 |
| Bonato (2018)10 | Prospective cluster randomized controlled | 86/0 | 74/7 | Italy: Premier National League | Mean 20 | Basketball | 64 | 128 |
| Omi (2018),52 intervention 1 | Prospective nonrandomized observation-intervention | 268/6 | 309/16 | Japan: collegiate Division 2 | Mean 19.6 | Basketball | 34.3 | 103 |
| Omi (2018),52 intervention 2 | Prospective nonrandomized observation-intervention | 180/3 | 309/16 | Japan: collegiate Division 2 | Mean 19.6 | Basketball | 34.8 | 104 |
| Foss (2018)17 | Prospective cluster randomized controlled | 259/1 | 215/2 | US: middle and high school | Mean 14 | Soccer, volleyball, and basketball | 11.32 | 44 |
Training time and number of sessions are displayed according to protocol and not actual compliance.
Figure 1.
Flowchart of the literature review. ACL, anterior cruciate ligament.
Figure 2.
Odds of anterior cruciate ligament injury compared with control group. (A) Cumulative effects over time and (B) effects ordered by upper bound CI of the odds ratio (OR).
Training Duration and Timing
No significant meta-regression effects were found for total training duration on ACL injury risk (total training time estimate/slope = −0.02; P = .28). The overall mean training amount was 57 sessions totaling 18.17 hours (roughly 24 minutes per session, 2.5 times per week).§§ NMT interventions conducted only in the preseason did not reduce the risk for ACL injury (OR, 0.59; 95% CI, 0.16−2.15); however, only 2 studies were included in this estimate.21,24 NMT interventions conducted in-season only or both preseason and in-season reduced the risk for ACL injury (OR, 0.50; 95% CI, 0.36−0.70). Thus, continued exposure to neuromuscular training throughout the sport season seems to enhance prophylactic effects of NMT, but more preseason-only studies may help elucidate this finding.
Target Population
NMT interventions were effective for female basketball (OR, 0.33; 95% CI, 0.16−0.69), soccer (OR, 0.46; 95% CI, 0.24−0.88), and handball (OR, 0.66; 95% CI, 0.45−0.97) athletes, and interventions including various athletes were potentially effective (eg, soccer, basketball, and volleyball) (OR, 0.60; 95% CI, 0.25−1.44); however, only 4 small studies were included in the estimate for combined-sport investigations.17,24,34,57 Interventions targeting middle and high school–aged athletes (13−19 years old) reduced injury risk (OR, 0.38; 95% CI, 0.24−0.60) to a greater degree than did interventions for college- or professional-aged athletes (19−24 years old) (OR, 0.65; 95% CI, 0.48−0.89).
Neuromuscular Training Program Characteristics
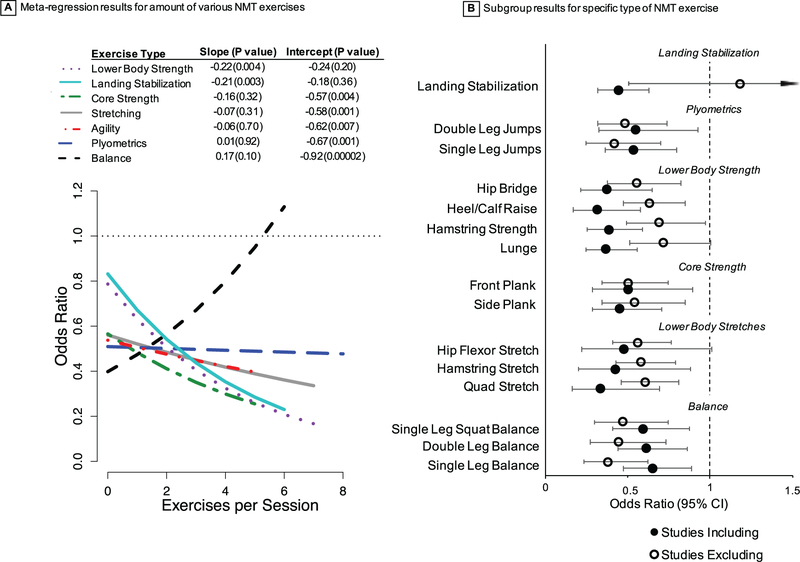
All interventions included some form of implementer training (eg, instructional workshop, video, or brochure) on proper program implementation (eg, exercise instruction and progression, feedback). All but 1 program59 focused on proper movement technique including knee control during landing and other dynamic movements. Programs including more landing stabilization and lower body strength exercises during each session were most effective (Figure 3). Programs including balance, core-strengthening, stretching, or agility exercises were no more effective than programs that did not incorporate these components (Figure 3). Specifically, programs that included more landing stabilization exercises (eg, drop landings, jump/hop and holds), hamstring strength (eg, Nordic hamstring), lunges, and heel-calf raises reduced the risk for ACL injury to a greater degree than did programs without these exercises.
Figure 3.
Exercise-based (A) meta-regression and (B) subgroup analyses. NMT, neuromuscular training.
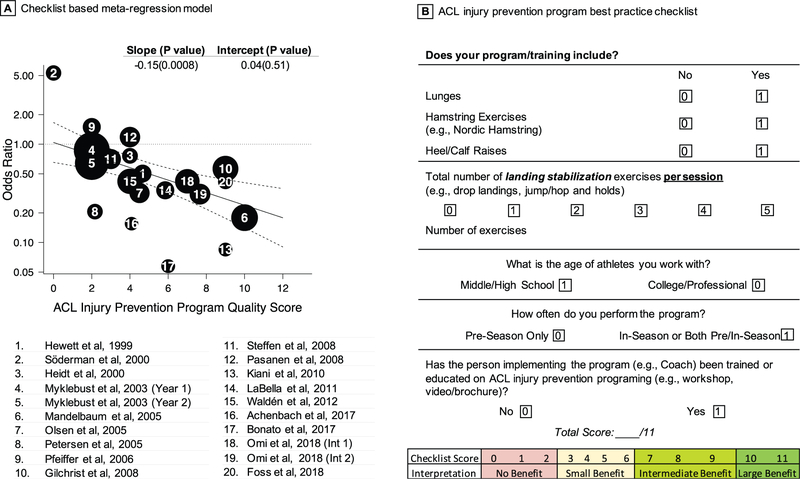
Best-Practice Model
A final additive meta-regression model was made and a simple checklist was created based on the aforementioned effective components and characteristics of ACL injury prevention programs (Figure 4). Sensitivity analysis was conducted by removing a potential outlier,59 and results or interpretations did not change. Because (1) each of the components displayed similar protective effects (eg, subgroup and meta-regression effect sizes), (2) the programs had multiple components, and (3) we wanted to create a simple, user-friendly tool for coaches and practitioners, a simple additive model was created by summing the inclusion of the various effective components. Scoring for this tool was as follows: all “yes” responses were considered 1 point; the numbers of landing stabilization exercises were counted as indicated (eg, if the program contained 3 landing stabilization exercises, the number of points was 3); middle or high school age was 1 point; college or professional age was 0 points; preseason only was 0 points; in-season or both preseason and in-season was 1 point; “no” for implementer training was 0 points; and “yes” for implementer training was 1 point. Thus, the maximum score was 11. As seen in Figure 4, a score of approximately 5 would result in the average meta-analytic effect of the combined interventions (eg, OR of approximately 0.5). It was determined that based on the CIs for the meta-regression model, a score of greater than 3 is likely to lead to protective effects. These findings were corroborated by qualitatively synthesizing the program components of the top 5 most effective programs based on 3 ranking systems: (1) 95% CI upper bound (Figure 2B), (2) OR, and (3) meta-regression checklist ranking. The majority of the top 5 programs included multiple landing stabilization exercises (forward and backward hop and hold, single-legged hop and hold, and vertical jump with landing stabilization), Nordic hamstrings, lunges, and heel-calf raises.
Figure 4.
Meta-regression based, best-practice checklist. (A) Regression model characteristics and (B) checklist. All dichotomous items are scored as 0 or 1, and continuous measures (landing stabilization exercises) are scored as indicated by the exact number. ACL, anterior cruciate ligament.
DISCUSSION
The goal of this investigation was to use robust quantitative analyses to determine the key components for optimizing ACL injury prevention programs. Through the development of a meta-analytic driven checklist, the current results provide specific guidelines for ACL injury prevention programming. Overall, the most effective ACL injury prevention programs included trained or informed personnel (eg, coaches, trainers), targeted younger athletes, exposed athletes to NMT throughout the sport season, and included lower body strengthening and landing stabilization exercises. Significant effectiveness was not found in programs including balance, core strengthening, stretching, or agility compared with NMT programs that did not incorporate these components. Including these other components may not be harmful but may be an ineffective use of time if ACL injury prevention is a primary goal. A potential important caveat is that these other components, such as balance training, have been shown to be effective for preventing ankle sprains73; thus, a more holistic perspective must be considered when designing overall sport injury prevention programs. In addition, proper exercise progression, especially for landing stabilization, was used throughout the majority of the ACL NMT programs.
Previous meta-analyses regarding ACL injury prevention have found consistently effective component results67,70; however, this analysis provides explicit characteristics for prevention programs that previous analyses lacked. The overall quality of the studies included in this analysis was moderate, based on PEDro scores; thus, more high-quality studies may help improve the strength of recommendations. Our results are also consistent with theoretical and empirical evidence on the mechanisms of action for these prevention programs/components as related to ACL injury mechanisms and risk factors. Specifically, stiff landings and improper alignment of the knee joint in the frontal plane, which are influenced by hip and trunk control, are likely to increase the risk for ACL injury.25,26,33,35 Thus, properly performed exercises that engage hip muscles (eg, gluteal muscles, hamstrings) and ACL agonist knee muscles (eg, calf and hamstrings), such as Nordic hamstrings, lunges, heel-calf raises, and landing stabilization exercises, should protect the ACL and limit hip internal rotation and adduction motions, which contribute to improper knee alignment. Landing stabilization exercises directly focus on optimizing muscle activation to ensure proper technique and alignment (landing softly and knee-over-toe positioning). Acute feedback interventions as well as some longer term training studies have shown muscular adaptations in response to NMT.23,44,45,71
Although between-study assessment of dosage effects seems to result in null or small effects, various within-study results of actual adherence to injury prevention have been found.60,65,74 Thus, adherence is key and should not be assumed or ignored. Despite the substantial evidence documenting the efficacy and societal benefit of prevention programs, ACL injury rates have not decreased.2,3,18,22 A primary reason is that athletes are not engaging in this prevention training. The use of ACL injury prevention through NMT by female high school teams is low nationally (13%−20%) and very low in rural areas (4%).29,48,64 Knowledge and comprehension of evidence-based prevention strategies have been documented to be the most important modifiable barriers to implementation.14,27,43,48,49,53 Thus, improving understanding of effective components of NMT should translate to greater implementation of NMT (see the online Video Supplement for a summary). Furthermore, the tool developed in this investigation will help coaches and practitioners to assess their current programs or design future NMT programs that optimize ACL injury prevention.
The checklist was developed based on descriptive meta-analytic findings and not randomized comparison trials; thus, results should be interpreted with caution. Future studies should directly compare program content (dosage, timing, exercises) and the associated injury prevention effects. However, because ACL injuries do not occur as frequently as one might think (eg, overall injury rate is approximately 1 in 80 athletes per season in these high-risk sports), large sample sizes (eg, > 8000) are needed to conduct a sufficiently powered randomized controlled or comparison trial. Given the amount of resources needed to conduct such a trial and considering the evidence found in this meta-analysis, it may be more appropriate to ensure that individuals are engaging in NMT (consisting of these best-practice components) rather than invest in additional large, randomized controlled trials. Ultimately, the goal of developing this tool is to ensure that athletes routinely engage in and adhere to evidence-based ACL injury prevention activities.
CONCLUSION
Various programmatic components of ACL NMT are associated with injury reduction. We recommend that ACL NMT programs target younger athletes and use trained implementers who incorporate lower body strength exercises (ie, Nordic hamstrings, lunges, and calf raises) and focus specifically on landing stabilization exercises (jump and hold, drop and land) throughout the sport season. Coaches, athletes, parents, and practitioners can use the developed checklist to gain insights into the quality of their current ACL NMT practices as well as to inform modification or development of future ACL NMT.
Supplementary Material
Acknowledgments
One or more of the authors has declared the following potential conflict of interest or source of funding: G.D.M. acknowledges funding support from National Institutes of Health/NIAMS Grant R21AR065068–01A1 and U01AR067997.
Footnotes
These numbers are based on the prescribed amount and not actual compliance. The average number of sessions per week typically varied for NMT interventions conducted in both preseason and in-season (fewer sessions per week during the season). Training session duration was substantially longer for the studies conducted during preseason only (eg, 75 minutes per session).
Investigation performed at Michigan State University, East Lansing, Michigan, USA
A Video Supplement for this article is available online.
REFERENCES
- 1.Achenbach L, Krutsch V, Weber J, et al. Neuromuscular exercises prevent severe knee injury in adolescent team handball players [published online October 20, 2017]. Knee Surg Sports Traumatol Arthrosc. doi: 10.1007/s00167-017-4758-5 [DOI] [PubMed] [Google Scholar]
- 2.Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in National Collegiate Athletic Association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33(4):524–531. [DOI] [PubMed] [Google Scholar]
- 3.Agel J, Rockwood T, Klossner D. Collegiate ACL injury rates across 15 sports: National Collegiate Athletic Association Injury Surveillance System data update (2004–2005 through 2012–2013). Clin J Sport Med. 2016;26(6):518–523. [DOI] [PubMed] [Google Scholar]
- 4.Ajuied A, Wong F, Smith C, et al. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2014;42(9):2242–2252. [DOI] [PubMed] [Google Scholar]
- 5.Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med. 2016;44(10):2492–2498. [DOI] [PubMed] [Google Scholar]
- 6.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. [DOI] [PubMed] [Google Scholar]
- 7.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538–543. [DOI] [PubMed] [Google Scholar]
- 8.Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049–1057. [DOI] [PubMed] [Google Scholar]
- 9.Berkey CS, Hoaglin DC, Mosteller F, Colditz GA. A random-effects regression model for meta-analysis. Stat Med. 1995;14(4):395–411. [DOI] [PubMed] [Google Scholar]
- 10.Bonato M, Benis R, La Torre A. Neuromuscular training reduces lower limb injuries in elite female basketball players: a cluster randomized controlled trial. Scand J Med Sci Sports. 2018;28(4):1451–1460. [DOI] [PubMed] [Google Scholar]
- 11.Caine DJ, Golightly YM. Osteoarthritis as an outcome of paediatric sport: an epidemiological perspective. Br J Sports Med. 2011;45(4): 298–303. [DOI] [PubMed] [Google Scholar]
- 12.Cinque ME, Dornan GJ, Chahla J, Moatshe G, LaPrade RF. High rates of osteoarthritis develop after anterior cruciate ligament surgery: an analysis of 4108 patients [published online September 1, 2017]. Am J Sports Med. doi: 10.1177/0363546517730072 [DOI] [PubMed] [Google Scholar]
- 13.Darrow CJ, Collins CL, Yard EE, Comstock RD. Epidemiology of severe injuries among United States high school athletes 2005–2007. Am J Sports Med. 2009;37(9):1798–1805. [DOI] [PubMed] [Google Scholar]
- 14.Donaldson A, Callaghan A, Bizzini M, Jowett A, Keyzer P, Nicholson M. A concept mapping approach to identifying the barriers to implementing an evidence-based sports injury prevention programme [published online January 20, 2018]. Inj Prev. doi: 10.1136/injuryprev-2017-042639 [DOI] [PubMed] [Google Scholar]
- 15.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Filbay SR, Culvenor AG, Ackerman IN, Russell TG, Crossley KM. Quality of life in anterior cruciate ligament-deficient individuals: a systematic review and meta-analysis. Br J Sports Med. 2015;49(16):1033–1041. [DOI] [PubMed] [Google Scholar]
- 17.Foss KDB, Thomas S, Khoury JC, Myer GD, Hewett TE. A school-based neuromuscular training program and sport-related injury incidence: a prospective randomized controlled clinical trial. J Athl Train. 2018;53(1):20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gage BE, McIlvain NM, Collins CL, Fields SK, Dawn Comstock R. Epidemiology of 6.6 million knee injuries presenting to United States emergency departments from 1999 through 2008. Acad Emerg Med. 2012;19(4):378–385. [DOI] [PubMed] [Google Scholar]
- 19.Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36(8):1476–1483. [DOI] [PubMed] [Google Scholar]
- 20.Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and meta-analysis. Am J Sports Med. 2016;44(10):2716–2723. [DOI] [PubMed] [Google Scholar]
- 21.Heidt RS, Sweeterman LM, Carlonas RL, Traub JA, Tekulve FX. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28(5):659–662. [DOI] [PubMed] [Google Scholar]
- 22.Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Incidence of anterior cruciate ligament reconstruction among adolescent females in the United States, 2002 through 2014. JAMA Pediatr. 2017;171(8):808–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hewett TE, Ford KR, Xu YY, Khoury J, Myer GD. Effectiveness of neuromuscular training based on the neuromuscular risk profile. Am J Sports Med. 2017;45(9):2142–2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. [DOI] [PubMed] [Google Scholar]
- 25.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. [DOI] [PubMed] [Google Scholar]
- 26.Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43(6):417–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iversen MD, Friden C. Pilot study of female high school basketball players’ anterior cruciate ligament injury knowledge, attitudes, and practices. Scand J Med Sci Sports. 2009;19(4):595–602. [DOI] [PubMed] [Google Scholar]
- 28.Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Joy EA, Taylor JR, Novak MA, Chen M, Fink BP, Porucznik CA. Factors influencing the implementation of anterior cruciate ligament injury prevention strategies by girls soccer coaches. J Strength Cond Res. 2013;27(8):2263–2269. [DOI] [PubMed] [Google Scholar]
- 30.Kester BS, Behery OA, Minhas SV, Hsu WK. Athletic performance and career longevity following anterior cruciate ligament reconstruction in the National Basketball Association. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3031–3037. [DOI] [PubMed] [Google Scholar]
- 31.Kiani A, Hellquist E, Ahlqvist K, Gedeborg R, Byberg L. Prevention of soccer-related knee injuries in teenaged girls. Arch Intern Med. 2010;170(1):43–49. [DOI] [PubMed] [Google Scholar]
- 32.Kilcoyne KG, Dickens JF, Haniuk E, Cameron KL, Owens BD. Epidemiology of meniscal injury associated with ACL tears in young athletes. Orthopedics. 2012;35(3):208–212. [DOI] [PubMed] [Google Scholar]
- 33.Kristianslund E, Faul O, Bahr R, Myklebust G, Krosshaug T. Sidestep cutting technique and knee abduction loading: implications for ACL prevention exercises. Br J Sports Med. 2014;48(9):779–783. [DOI] [PubMed] [Google Scholar]
- 34.LaBella CR, Huxford MR, Grissom J, Kim K-Y, Peng J, Christoffel KK. Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools. Arch Pediatr Adolesc Med. 2011;165(11):1033–1040. [DOI] [PubMed] [Google Scholar]
- 35.Leppänen M, Pasanen K, Kujala UM, et al. Stiff landings are associated with increased ACL injury risk in young female basketball and floorball players. Am J Sports Med. 2017;45(3):NP5–NP6. [DOI] [PubMed] [Google Scholar]
- 36.Lewis DA, Kirkbride B, Vertullo CJ, Gordon L, Comans TA. Comparison of four alternative national universal anterior cruciate ligament injury prevention programme implementation strategies to reduce secondary future medical costs. Br J Sports Med. 2018;52(4):277–282. [DOI] [PubMed] [Google Scholar]
- 37.Lipsey MW, Wilson DB. Practical Meta-analysis. Vol 49 Thousand Oaks, CA: Sage; 2001. http://rogeriofvieira.com/wp-content/uploads/2016/05/Wilson.pdf. Accessed May 8, 2017. [Google Scholar]
- 38.Magnussen RA, Meschbach NT, Kaeding CC, Wright RW, Spindler KP. ACL graft and contralateral ACL tear risk within ten years following reconstruction. JBJS Rev. 2015;3(1):e3. [DOI] [PubMed] [Google Scholar]
- 39.Mai HT, Alvarez AP, Freshman RD, et al. The NFL Orthopaedic Surgery Outcomes Database (NO-SOD): the effect of common orthopaedic procedures on football careers. Am J Sports Med. 2016;44(9):2255–2262. [DOI] [PubMed] [Google Scholar]
- 40.Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003–1010. [DOI] [PubMed] [Google Scholar]
- 41.Marshall DA, Lopatina E, Lacny S, Emery CA. Economic impact study: neuromuscular training reduces the burden of injuries and costs compared to standard warm-up in youth soccer. Br J Sports Med. 2016;50(22):1388–1393. [DOI] [PubMed] [Google Scholar]
- 42.Mather RC, Koenig L, Kocher MS, et al. Societal and economic impact of anterior cruciate ligament tears: J Bone Joint Surg Am. 2013;95(19):1751–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McKay CD, Steffen K, Romiti M, Finch CF, Emery CA. The effect of coach and player injury knowledge, attitudes and beliefs on adherence to the FIFA 111 programme in female youth soccer. Br J Sports Med. 2014;48(17):1281–1286. [DOI] [PubMed] [Google Scholar]
- 44.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34(3):445–455. [DOI] [PubMed] [Google Scholar]
- 45.Myer GD, Stroube BW, DiCesare CA, et al. Augmented feedback supports skill transfer and reduces high-risk injury landing mechanics: a double-blind, randomized controlled laboratory study. Am J Sports Med. 2013;41(3):669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Myer GD, Sugimoto D, Thomas S, Hewett TE. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis. Am J Sports Med. 2013;41(1):203–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Myklebust G, Engebretsen L, Braekken IH, Skjølberg A, Olsen O-E, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71–78. [DOI] [PubMed] [Google Scholar]
- 48.Norcross MF, Johnson ST, Bovbjerg VE, Koester MC, Hoffman MA. Factors influencing high school coaches’ adoption of injury prevention programs. J Sci Med Sport. 2016;19(4):299–304. [DOI] [PubMed] [Google Scholar]
- 49.O’Brien J, Finch CF. Injury prevention exercise programmes in professional youth soccer: understanding the perceptions of programme deliverers. BMJ Open Sport Exerc Med. 2016;2(1):e000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–1443. [DOI] [PubMed] [Google Scholar]
- 51.Olsen O-E, Mykelbust G, Engebretsen L, Holm I, Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ. 2005;330(7489):449–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Omi Y, Sugimoto D, Kuriyama S, et al. Effect of hip-focused injury prevention training for anterior cruciate ligament injury reduction in female basketball players: a 12-year prospective intervention study. Am J Sports Med. 2018;46(4):852–861. [DOI] [PubMed] [Google Scholar]
- 53.Orr B, Brown C, Hemsing J, et al. Female soccer knee injury: observed knowledge gaps in injury prevention among players/ parents/coaches and current evidence (the KNOW study). Scand J Med Sci Sports. 2013;23(3):271–280. [DOI] [PubMed] [Google Scholar]
- 54.Padua DA, DiStefano LJ, Hewett TE, et al. National Athletic Trainers’ Association position statement: prevention of anterior cruciate ligament injury. J Athl Train. 2018;53(1):5–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pasanen K, Parkkari J, Pasanen M, et al. Neuromuscular training and the risk of leg injuries in female floorball players: cluster randomised controlled study. Br J Sports Med. 2008;337:A295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2005;125(9):614–621. [DOI] [PubMed] [Google Scholar]
- 57.Pfeiffer RP, Shea KG, Roberts D, Grandstrand S, Bond L. Lack of effect of a knee ligament injury prevention program on the incidence of noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2006;88(8):1769–1774. [DOI] [PubMed] [Google Scholar]
- 58.Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury–reduction regimen. Arthroscopy. 2007;23(12):1320–1325. [DOI] [PubMed] [Google Scholar]
- 59.Söderman K, Werner S, Pietila T, Engström B, Alfredson H. Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study. Knee Surg Sports Traumatol Arthrosc. 2000;8(6):356–363. [DOI] [PubMed] [Google Scholar]
- 60.Soligard T, Myklebust G, Steffen K, et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. BMJ. 2008;337:A2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Soomro N, Sanders R, Hackett D, et al. The efficacy of injury prevention programs in adolescent team sports: a meta-analysis. Am J Sports Med. 2016;44(9):2415–2424. [DOI] [PubMed] [Google Scholar]
- 62.Stanley LE, Kerr ZY, Dompier TP, Padua DA. Sex differences in the incidence of anterior cruciate ligament, medial collateral ligament, and meniscal injuries in collegiate and high school sports 2009–2010 through 2013–2014. Am J Sports Med. 2016;44(6):1565–1572. [DOI] [PubMed] [Google Scholar]
- 63.Steffen K, Myklebust G, Olsen OE, Holme I, Bahr R. Preventing injuries in female youth football—a cluster-randomized controlled trial: injury prevention in youth football. Scand J Med Sci Sports. 2008;18(5):605–614. [DOI] [PubMed] [Google Scholar]
- 64.Sugimoto D, Mattacola CG, Bush HM, et al. Preventive neuromuscular training for young female athletes: comparison of coach and athlete compliance rates. J Athl Train. 2017;52(1):58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sugimoto D, Myer GD, Bush HM, Klugman MF, McKeon JMM, Hewett TE. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: a meta-analysis. J Athl Train. 2012;47(6):714–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sugimoto D, Myer GD, Foss KDB, Hewett TE. Specific exercise effects of preventive neuromuscular training intervention on anterior cruciate ligament injury risk reduction in young females: meta-analysis and subgroup analysis. Br J Sports Med. 2015;49(5):282–289. [DOI] [PubMed] [Google Scholar]
- 67.Sugimoto D, Myer GD, Barber Foss KD, Pepin MJ, Micheli LJ, Hewett TE. Critical components of neuromuscular training to reduce ACL injury risk in female athletes: meta-regression analysis. Br J Sports Med. 2016;50(20):1259–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Suter LG, Smith SR, Katz JN, et al. Projecting lifetime risk of symptomatic knee osteoarthritis and total knee replacement in individuals sustaining a complete anterior cruciate ligament tear in early adult-hood: ACL tears and risk of knee OA and TKR. Arthritis Care Res. 2017;69(2):201–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006–2010/2011. Med Sci Sports Exerc. 2013;45(3):462–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Taylor JB, Waxman JP, Richter SJ, Shultz SJ. Evaluation of the effectiveness of anterior cruciate ligament injury prevention programme training components: a systematic review and meta-analysis. Br J Sports Med. 2015;49(2):79–87. [DOI] [PubMed] [Google Scholar]
- 71.Thompson JA, Tran AA, Gatewood CT, et al. Biomechanical effects of an injury prevention program in preadolescent female soccer athletes. Am J Sports Med. 2017;45(2):294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tirabassi J, Brou L, Khodaee M, Lefort R, Fields SK, Comstock RD. Epidemiology of high school sports-related injuries resulting in medical disqualification 2005–2006 through 2013–2014 academic years. Am J Sports Med. 2016;44(11):2925–2932. [DOI] [PubMed] [Google Scholar]
- 73.Vriend I, Gouttebarge V, van Mechelen W, Verhagen EALM. Neuromuscular training is effective to prevent ankle sprains in a sporting population: a meta-analysis translating evidence into optimal prevention strategies. J ISAKOS Jt Disord Orthop Sports Med. 2016;1(4): 202–213. [Google Scholar]
- 74.Waldén M, Atroshi I, Magnusson H, Wagner P, Hägglund M. Prevention of acute knee injuries in adolescent female football players: cluster randomised controlled trial. BMJ. 2012;344:e3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction. J Bone Joint Surg Am. 2011;93(12):1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wyatt RWB, Inacio MCS, Liddle KD, Maletis GB. Prevalence and incidence of cartilage injuries and meniscus tears in patients who under-went both primary and revision anterior cruciate ligament reconstructions. Am J Sports Med. 2014;42(8):1841–1846. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.