Abstract
Background
In many studies on documentation, the data are self-reported, which makes it difficult to know the actual level of documentation by pharmacists in patients’ medical records. The literature assessing documentation by clinical pharmacists in health care centres is limited.
Objective
To assess the level of documentation in patients’ medical records by clinical pharmacists at one large urban hospital.
Methods
This retrospective observational study included all patients who were followed by a clinical pharmacist during their stay in the Centre hospitalier de l’Université de Montreal between July 1 and October 31, 2016. The primary outcome, the level of documentation in patients’ medical records, was categorized as minimal, sufficient, or extensive. The quality of notes and the impact of pharmacy students and residents on documentation were evaluated as secondary outcomes.
Results
A total of 779 patient charts from 4 inpatient units were included in the analysis. Of these, 131 (16.8%) were considered to have minimal documentation (at least 1 suggestion or verbal order without a note in the progress section), 432 (55.5%) had sufficient documentation (at least 1 note written during the patient’s hospitalization), and 81 (10.4%) had extensive documentation (appropriate number of notes in relation to duration of hospitalization). Medication reconciliation performed by pharmacists at the time of admission was documented in 696 (89.3%) of patients’ records. The presence of students or residents on a clinical unit was associated with a significant increase in the percentage of charts with at least 1 follow-up note (23.6% [120/508] with students/residents versus 12.5% [34/271] without students/residents; p < 0.001) and the mean number of followup notes (0.59 versus 0.23, respectively; p < 0.001) but had no effect on other variables. Of a total of 777 notes written by a pharmacist, the overall conformity with pre-established criteria was 56.8% (441/777), and conformity was 43.4% (139/320), 75.1% (272/362), and 31.6% (30/95) for admission, follow-up, and discharge notes, respectively.
Conclusions
Documentation by clinical pharmacists in patients’ medical records could be improved to achieve the stated goal of the American Society of Health-System Pharmacists and the Canadian Society of Hospital Pharmacists, that all significant clinical recommendations or interventions should be documented.
Keywords: documentation, pharmaceutical interventions, clinical pharmacist, patient chart
RÉSUMÉ
Contexte
Les données de bon nombre d’études portant sur la tenue des dossiers médicaux sont autodéclarées, ce qui fait qu’il est difficile de savoir exactement dans quelle mesure les pharmaciens consignent les informations dans les dossiers médicaux des patients. Il n’existe que peu d’études évaluant la tenue des dossiers par les pharmaciens cliniques dans les centres de soins de santé.
Objectif
Évaluer dans quelle mesure les pharmaciens cliniciens d’un important hôpital urbain consignent l’information dans les dossiers médicaux des patients.
Méthodes
La présente étude d’observation rétrospective englobait tous les patients ayant été suivis par un pharmacien clinicien pendant leur séjour au Centre hospitalier de l’Université de Montréal entre le 1er juillet et le 31 octobre 2016. Le principal paramètre d’évaluation, soit le degré de rigueur des inscriptions dans les dossiers médicaux des patients, entrait dans l’une des trois catégories suivantes : minimal, suffisant ou exhaustif. La qualité des notes et l’effet de la participation d’étudiants et de résidents en pharmacie à la tenue des dossiers ont servi de paramètres d’évaluation secondaires.
Résultats
L’analyse a porté sur 779 dossiers médicaux de patients provenant de quatre services hospitaliers. Les investigateurs ont considéré que 131 d’entre eux (16,8 %) appartenaient à la catégorie « minimal » (au moins une intervention consignée par écrit), 432 (55,5 %) se situaient dans la catégorie « suffisant » (au moins une note rédigée au cours de l’hospitalisation du patient) et 81 (10,4 %) se rangeaient dans la catégorie « exhaustif » (nombre adéquat de notes en fonction à la durée de l’hospitalisation). Les bilans comparatifs des médicaments établis par des pharmaciens au moment de l’admission ont été consignés dans 696 (89,3 %) dossiers médicaux de patients. On a associé la présence d’étudiants ou de résidents dans une unité clinique à une hausse significative du pourcentage de dossiers médicaux affichant au moins une note de suivi (23,6 % [120/508] avec des étudiants / résidents contre 12,5 % [34/271] sans étudiants / résidents; p < 0,001) et du nombre moyen de notes de suivi (respectivement 0,59 contre 0,23; p < 0,001), mais leur présence n’a été associée à aucun autre effet sur les autres variables. Le taux de conformité globale aux critères préétablis des 777 notes rédigées par un pharmacien était de 56,8 % (441/777) et le taux de conformité des notes d’admission, de suivi et de congé était respectivement de 43,4 % (139/320), 75,1 % (272/362) et 31,6 % (30/95).
Conclusions
La tenue des dossiers médicaux de patients par les pharmaciens cliniciens devrait s’améliorer pour qu’elle atteigne l’objectif établi par l’American Society of Health-System Pharmacists et la Société canadienne des pharmaciens d’hôpitaux, qui veut que toutes les recommandations et interventions cliniques d’importance soient consignées.
Mots clés: tenue des dossiers, interventions pharmaceutiques, pharmacien clinicien, dossiers médicaux de patients
INTRODUCTION
Over the past several decades, the practice of pharmacy has gradually shifted from drug dispensing to application of the concepts of clinical pharmacy and pharmaceutical care.1–3 By assuming patient care duties, pharmacists become responsible for documenting in the medical record their activities related to medication reconciliation, clinical problem-solving, therapeutic interventions, and patient education.3 The practice of documentation has been endorsed by many hospital pharmacist societies and pharmacy organizations worldwide and is included in their standards of practice, helping pharmacists to fulfill their professional obligations to ensure continuity of care and to be fully recognized as part of a multidisciplinary team.4–6 Over time, clinical pharmacists have used various documentation systems (such as SOAP [subjective, objective, assessment, plan], TITRS [title, introduction, text, recommendation, signature], and FARM [findings, assessment, recommendations/resolutions, management]) to determine what information should be included and how it should be communicated in the patient’s medical record.7
However, some studies have shown that pharmacists on inpatient units do not routinely complete documentation in patients’ medical records and that documentation varies among countries, hospitals, and clinical departments. Between 2005 and 2012, the American Society of Health-System Pharmacists (ASHP) conducted 3 surveys, in which 59.0% to 65.0% of respondents reported that their hospitals required pharmacists to document drug therapy recommendations and progress notes in the patient’s permanent medical record.8–10 In a questionnaire sent to pharmacists in a 900-bed teaching hospital in London, Ontario, 74% (29/39) of respondents reported that they did not write in the patient’s medical record.11 In a subsequent focus group, these pharmacists reported that they recognized the importance of documenting relevant issues but preferred to use oral communication or temporary adhesive notes instead.11 Similarly, in a cross-sectional descriptive study carried out at the Centre hospitalier universitaire Sainte-Justine in Montréal, Quebec, in 2014 and 2015, only 20% of the interventions performed by pharmacists were recorded in patients’ medical records.12 In the province of Quebec, the Ordre des pharmaciens du Québec evaluated the practice of health facility pharmacists since 2011 in relation to its standards of practice.13 This round of inspection showed a gap in the documentation of information, with only 50% of pharmacists documenting sufficiently in patients’ medical records.14 Like the clinical guidelines of the Canadian Society of Hospital Pharmacists (CSHP)4 and the ASHP,5 Quebec’s provincial standards of practice13 state that all significant clinical recommendations and interventions should be documented in the patient’s medical record, according to the pharmacist’s clinical judgment. Many published studies have detailed the clinical activities of hospital pharmacists, but they have provided little information about the level of documentation in the patient’s medical record.15,16 In addition, most studies present self-reported data on documentation, which makes it difficult to know the actual level of documentation by the pharmacists, who may be following several patients on a clinical unit.
Taken together, these results highlight the problem of lack of documentation by clinical pharmacists following patients on inpatient units in the hospital setting. Therefore, the objective of this study was to assess the quality and quantity of documentation about clinical interventions by pharmacists in patients’ medical records on 4 inpatient units at the Centre hospitalier de l’Université de Montréal (CHUM).
METHODS
Setting
The CHUM is a tertiary academic centre in Montréal, which moved to a new building, with 772 beds, in November 2017. At the time of this study, the CHUM was composed of 3 hospitals (Notre-Dame, Saint-Luc, and Hôtel Dieu), which together had more than 1500 beds. Pharmacy services are provided 24 h/day, with decentralization between the hours of 0800 and 2200. Between 3000 and 3500 medical prescriptions are validated each day. A total of 73 pharmacists (representing 68 full-time equivalents) contribute actively to teaching during the weekdays. On the inpatient units, there is no clinical position dedicated to a single pharmacist; rather each position rotates among 3 or 4 designated pharmacists. Each year, the department of pharmacy hosts 35 to 40 students and 7 pharmacy residents. These learners contribute to patient care and are present on the inpatient units for prespecified periods.
Various methods are used for communication among health care providers, including written notes in the paper medical records during the patient’s hospitalization and electronic charts for previous hospitalizations, which are easily accessible to the medical team. Also, pharmacists may use a parallel electronic documentation system within the pharmacy software, which is accessible only to pharmacy staff. Written information may be composed of SOAP notes in the medical section of a patient’s record and recommendations or verbal orders from doctors in the prescription section. At the time of the study, the hospital did not have a computerized physician order entry system.
Study Design
This multicentre retrospective study aimed to evaluate the documentation of interventions in patients’ medical records by clinical pharmacists between July 1 and October 31, 2016, in 4 inpatient units: hematology–oncology, solid organ transplantation, cardiology, and hepatology. Patients who had been followed by a clinical pharmacist during hospitalization were identified with the pharmacy department’s computer software, BDM Pharmacy (BDM IT Solutions Inc, Saskatoon, Saskatchewan). Patients whose electronic medical records were not available and those who were not followed by a clinical pharmacist were excluded from this study. Four pharmacy students (C.T., C.P.-W., M.-L.D., P.L.) collected the data from patients’ medical records held in the electronic clinical information system Oacis (Telus Health, Montréal, Quebec). The students were divided into pairs, with 10% of all data collected by each pair being double-checked by the other pair. The local independent ethics committee and independent institutional review board approved retrieval of data from patients’ medical records for the purposes of this study.
Outcomes
The primary outcome was the level of documentation in patients’ medical records by clinical pharmacists. A literature search of Google Scholar, PubMed, and Embase databases (with the keywords “documentation”, “pharmacist”, “impact”, “practice standards”, “notes”, and “hospital”) and a systematic review of the clinical guidelines published by various pharmacy professional and scientific societies (including ASHP, CSHP, and the American College of Clinical Pharmacy [ACCP]) yielded no defined criteria for adequate documentation and how to quantify it.
The authors of the present article (4 pharmacy students and 3 clinical pharmacists with 4, 6, and 10 years of experience, respectively) formed a committee to establish detailed criteria defining whether documentation in the patient’s medical record was minimal, sufficient, or extensive in relation to clinical practice standards. “Minimal” documentation was defined as at least 1 suggestion or verbal order recorded in the prescription section of the patient’s medical record, without any note in the progress section of the patient’s medical record. “Sufficient” documentation was defined as the presence of at least 1 note in the medical section of the patient’s medical record, regardless of the patient’s length of stay in hospital. “Extensive” documentation was defined as the presence of at least 1 admission, follow-up, or discharge note for hospital stays of up to 2 days; an admission note and a discharge note for hospital stays between 3 and 6 days; or an admission note, a follow-up note, and a discharge note for hospital stays of 7 days or longer. No discharge note was expected for any patient who died during the hospital stay, was transferred to another care unit or health facility, or was discharged on a weekend. These criteria were based on several studies that have demonstrated the benefits of a pharmacist’s medication management during transitions of care, in particular at hospital admission and discharge, on clinical outcomes such as medication discrepancies, adverse drug event–related hospital revisits, emergency department visits, and/or hospital readmissions.17,18
The secondary outcomes included the conformity of notes with pre-established criteria, the effect of the presence of pharmacy students and residents on the documentation of interventions, and the percentage of suggestions for modification of drug therapy in the prescription section of the patient’s medical record that were explained and detailed in the medical notes. Medication reconciliation electronically entered by the pharmacist into the pharmacy software was also collected.
The criteria for evaluating conformity of documentation were inspired by the CSHP guidelines.4 For all types of notes, the heading “pharmacy”, the date and time of the note, and the pharmacist’s signature were required. For admission notes, the pharmacist had to state the reason for consultation and had to mention medication reconciliation, the patient’s allergies and/or intolerances, the pharmacist’s analysis of pharmacotherapy, and an intervention plan. For follow-up notes, an analysis and a plan were required. For discharge notes, patient counselling and discharge medication reconciliation had to be described. To be considered in conformity, a note had to meet all of the criteria for the particular note type. The number of interventions by pharmacists documented in the prescription section, consisting of suggestions made by the pharmacist or the pharmacist’s transcription of verbal instructions from the medical team, was collected to understand the involvement of pharmacists in documentation in patients’ medical records, independent of written admission, follow-up, and discharge notes (as described above).
Statistical Analysis
Continuous variables are presented as means (with standard deviations) or medians (with interquartile ranges [IQRs]), whereas categorical variables are described as frequencies. The χ2 test (for proportions) and the Mann-Whitney U test (for differences between means) were used to analyze the distribution of categorical and continuous variables, respectively, with a significance level of 0.05. Statistical analysis was carried out with SPSS 24.0 software (IBM, Armonk, New York).
RESULTS
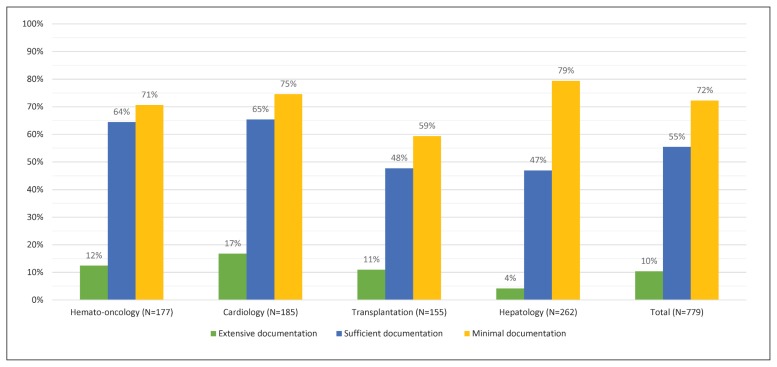
A total of 779 patients followed by a clinical pharmacist at the CHUM between July 1 and October 31, 2016, were selected for this study. One additional patient was excluded because the electronic record was not available. The duration of hospitalization was up to 2 days for 112 (14.4%) of the patients, between 3 and 6 days for 263 (33.8%), and 7 days or more for 404 (51.9%), with a median of 7 days. The numbers of patients’ medical records with minimal, sufficient, and extensive documentation were 131 (16.8%), 432 (55.5%) and 81 (10.4%), respectively (Table 1). These results are detailed according to clinical unit in Figure 1. Medication reconciliation done by pharmacists at the time of admission was documented in 696 (89.3%) of patients’ medical records.
Table 1.
Level of Documentation and Interventions Included in Patients’ Medical Records
| Characteristic | No. (%) of Records* (n = 779) |
|---|---|
| Level of documentation† | |
| Extensive | 81 (10.4) |
| Sufficient | 432 (55.5) |
| Minimal | 131 (16.8) |
|
| |
| Intervention documented in the prescription section | |
| Verbal orders | |
| Records with ≥ 1 verbal order | 142 (18.2) |
| No. of verbal orders per record (median and IQR) | 1 (1–2) |
| Suggestions | |
| Records with ≥ 1 suggestion | 369 (47.4) |
| No. of suggestions per record (median and IQR) | 1 (1–2) |
| Verbal orders and/or suggestions | |
| Records with ≥ 1 verbal order or suggestion (or both) | 426 (54.7) |
IQR = interquartile range.
Except where indicated otherwise.
Extensive documentation was defined as presence of ≥ 1 admission, follow-up, or discharge note for hospital stays ≤ 2 days; an admission note and a discharge note for hospital stays of 3–6 days; or an admission note, a follow-up note, and a discharge note for hospital stays ≥ 7 days. Sufficient documentation was defined as presence of ≥ 1 note in medical section of patient’s medical record, regardless of the patient’s length of stay in hospital. Minimal documentation was defined as ≥ 1 written intervention in patient’s medical record, such as a note in the medical section or a suggestion or verbal order in the prescription section.
Figure 1.
Level of documentation in patients’ medical records, by clinical unit.
Among the total of 777 notes written by pharmacists in the patients’ medical records, the overall conformity in relation to pre-established criteria was 56.8% (441/777), with conformity being higher for follow-up notes (75.1% [272/362]) than for admission notes (43.4% [139/320]) and discharge notes (31.6% [30/95]) (Table 2). The main effect on documentation of having pharmacy students or residents on the clinical unit was an increase in the number of patient records with at least 1 follow-up note (23.6% [120/508] with students/residents versus 12.5% [34/271] without students/residents; p < 0.001) and the mean number of follow-up notes (0.59 versus 0.23, respectively; p < 0.001) (Table 3). Although the presence of pharmacy students or residents was associated with a trend toward increased rate of sufficient documentation (57.7% [293/508] versus 51.3% [139/271]; p = 0.09), it did not affect the rates of extensive or minimal documentation. The principal topic of intervention in the followup notes was related to safety (44.5% [161/362]), efficacy (20.4% [74/362]), dose adjustment (13.8% [50/362]), compliance (5.5% [20/362]), drug interactions (3.6% [13/362]), access to medication (1.4% [5/362]), and other (10.8% [39/362]). When we analyzed the suggestions and verbal orders that clinical pharmacists wrote in the prescription section, we found that suggestions were combined with a note in the medical section (64.8% [239/369]) more often than were verbal orders (24.6% [35/142]).
Table 2.
Conformity of Admission, Follow-up, and Discharge Notes*
| Characteristic | No. (%) of Records |
|---|---|
| Admission notes | n = 320 |
| Title heading “Pharmacy” | 318 (99.4) |
| Date and time | 236 (73.8) |
| Pharmacist’s signature | 319 (99.7) |
| Reason for consultation | 305 (95.3) |
| Mention of medication reconciliation | 316 (98.8) |
| Patient’s allergies and/or intolerances | 242 (75.6) |
| Analysis of pharmacotherapy | 295 (92.2) |
| Plan of intervention | 258 (80.6) |
| Overall conformity | 139 (43.4) |
|
| |
| Follow-up notes† | n = 362 |
| Title heading “Pharmacy” | 361 (99.7) |
| Date and time | 309 (85.4) |
| Pharmacist’s signature | 360 (99.4) |
| Analysis of pharmacotherapy | 358 (98.9) |
| Plan of intervention | 315 (87.0) |
| Overall conformity | 272 (75.1) |
|
| |
| Discharge notes | n = 95 |
| Title heading “Pharmacy” | 95 (100) |
| Date and time | 68 (71.6) |
| Pharmacist’s signature | 94 (98.9) |
| Discharge medication reconciliation | 70 (73.7) |
| Mention of patient counselling | 80 (84.2) |
| Overall conformity | 30 (31.6) |
Conformity was assessed in relation to guidelines of the Canadian Society of Hospital Pharmacists.4
A patient’s medical record could have more than 1 follow-up note. The n value of 362 refers to the total number of follow-up notes assessed.
Table 3.
Effect of Students and Residents on Documentation
| Category; No. (%) of Records* | |||
|---|---|---|---|
|
|
|||
| Outcome | Student or Resident Present (n = 508) | No Students or Residents Present (n = 271) | p Value |
| Quality of documentation | |||
| Extensive | 50 (9.8) | 31 (11.4) | 0.49 |
| Sufficient | 293 (57.7) | 139 (51.3) | 0.09 |
| Minimal | 370 (72.8) | 193 (71.2) | 0.63 |
|
| |||
| Note type | |||
| Admission note | 215 (42.3) | 105 (38.7) | 0.36 |
| ≥ 1 follow-up note | 120 (23.6) | 34 (12.5) | < 0.001 |
| Mean no. of follow-up notes/PMR | 0.59 | 0.23 | < 0.001 |
| Mean no. of admission, follow-up, and discharge notes/PMR | 1.13 | 0.73 | 0.007 |
| Discharge note† | 61/436 (14.0) | 34/237 (14.3) | 0.91 |
NS = not significant, PMR = patient’s medical record.
Except where indicated otherwise.
In this row, the denominators (total number of patients’ medical records for which a discharge note was expected) are less than the total number in each category because a discharge note was not expected if the patient died, was transferred to another care unit or health establishment, or was discharged on a weekend.
DISCUSSION
To our knowledge, this is the first multicentre study to evaluate the level of documentation in patients’ medical records by clinical pharmacists using a method that did not involve self-reporting. With regard to the primary outcome, the level of documentation was minimal, sufficient, and extensive in 72.3%, 55.5%, and 10.4% of patients’ medical records, respectively. These results are similar to those in a study by Ballandras and others,12 who reported that 58.4% of patients’ medical records had at least 1 written note from a pharmacist resulting from a pharmaceutical intervention. The wide disparity between the proportions of records with extensive and sufficient documentation may be explained by several factors. For most of the records that did not meet the criteria for extensive documentation, the reason was lack of a discharge note (affecting 85.9% of eligible records [578/673]). Given the lack of a definition for “optimal” documentation in pharmacy organizations’ standards of practice, the interpretation varies among individual pharmacists, especially in our context, where 3 or 4 designated clinical pharmacists rotate through the same clinical area. For this reason, a committee (consisting of all the authors) developed the criteria for 3 levels of documentation by consensus. These criteria were based on previous studies that have demonstrated the benefits of pharmacists’ medication management during transitions of care and are compatible with clinical pharmacy practice in North America.17,18
The criteria for extensive documentation were based on the assumption that for a longer hospital length of stay, the pharmacist would have more time to see the patient and more occasions to document interventions in the patient’s medical records. We believe that efforts should be made to improve these results to achieve the standards of practice established by various pharmacy groups (e.g., ASHP, CSHP, ACCP).
The overall conformity of admission, follow-up, and discharge notes with pre-established criteria (based on CSHP guidelines4) was 43.4%, 75.1%, and 31.6%, respectively. In general, most of the records met most of the criteria, but often a single required element was missing, which meant that the note did not fulfill the criteria for conformity (Table 2). The study also aimed to evaluate the impact of pharmacy students and residents on the documentation of interventions in patients’ medical records. The involvement of these learners had a significant effect on the number of records with at least 1 follow-up note (23.6% versus 12.5%, p < 0.001) and the mean number of follow-up notes (0.59 versus 0.23, p < 0.001), which had a positive effect on the mean number notes per record (1.13 versus 0.73, p < 0.007). These results aligned with those reported in other studies, which have demonstrated that the educational activities of students and residents in health care establishments have a positive influence on patient care.19–21 The presence of pharmacy students and residents did not significantly affect the other variables. However, this study was not powered to assess a difference between the presence and absence of residents and students on the inpatient units. The calculation of a sample size was not possible because of the absence of data on documentation by pharmacy learners. Taken together, these results suggest that clinical pharmacists cannot actively follow more patients on the clinical unit, despite the presence of a student, probably because time must be spent in direct teaching activities.
As part of minimal documentation, nearly two-thirds of the suggestions and one-quarter of verbal orders in the prescription section were detailed or explained elsewhere in the patient’s medical records. These results were expected, because the existence of a verbal order implies that the pharmacist verbally explained the intervention to the medical team, and such orders reflect the important place of oral communication with the medical team.11 To promote a multidisciplinary approach and to help comprehension of their role and interventions, pharmacists should write a summary of any verbal discussion in the medical section of the patient’s record.11 In this study, the records of almost 30% of the patients contained no formal documentation by a pharmacist. This result was surprising, because the clinical pharmacists completed medication reconciliation at admission for 89.4% of patients across the 4 inpatient units. It is possible that some interventions were discussed verbally with the medical team, without documentation; in addition, the pharmacists may have chosen to not see some patients because they prioritized other patients.22
The overall documentation by pharmacists in patients’ medical records could be increased. In our centre, all medication reconciliations are done by pharmacists. With appropriate supervision, pharmacy technician–centred medication reconciliation programs have led to effective medication history-taking, documentation and communication of data, and enhanced pharmacotherapy safety.23,24 The clinical tasks of pharmacists in Canada and the United States have been expanding, which has made it more difficult for pharmacists to follow the same number of patients as in the past.25–27 Because the workload may be too great in inpatient units with rapid turnover of patients, such as hepatology, pharmacists may not have the time to write multiple notes in patients’ medical records. Clinical pharmacists could prioritize their patients, because high-risk patients should benefit the most from their interventions.22,28 To our knowledge, there is little information available on methods to classify high-risk patients on a clinical unit with already highly demanding medication needs, such as oncology or solid organ transplantation. As described above, pharmacists often document their interventions in the pharmacy software, without recording the information in patients’ medical records. To increase productivity and enhance documentation, pharmacists could print electronic documentation from the pharmacy software and include it in the patient’s medical record.29,30 Another way to increase efficiency and achieve better conformity of documentation would be to use preprinted forms.31 Also, improving communication among doctors, pharmacists, and unit coordinators could help pharmacists to know when a patient will be discharged. Doing so could help to increase the number of discharge notes, thereby increasing the proportion of records with extensive documentation. Finally, as pharmacy practice is continuously changing and improving, it will be important to develop educational presentations and documents to raise pharmacists’ and students’ awareness regarding practice standards for documentation.32
This study had both strengths and limitations. Collection of the data by 2 pairs of students may have introduced observation bias. To limit such bias, 10% of all records were double-checked and corrected, if appropriate, by the other team of students. The patients’ medical records were handwritten and although the observers were vigilant, some data may have been missed (e.g., if pharmacists did not identify themselves adequately in the record or if the quality of the handwriting was poor). However, the large number of records analyzed (with exclusion of only 1 record) may have compensated for these limitations. Another limitation was the absence of testing for interindividual variability between clinical pharmacists. However, the goal of the study was not to identify differences among pharmacists, but rather to determine tendencies and trends, in order to ameliorate the practice of a group of pharmacists.
This study examined an issue that is very poorly investigated and reported in the literature. Comparing the results of this study with results of similar analyses in other health care centres would be of interest. We believe that the results of this study can be generalized to other North American centres. A strength of the study was its focus on the actual number of patients being followed by pharmacists on weekdays, rather than total admissions to an inpatient unit, whether or not the patients were being followed by a pharmacist. A retrospective study was an appropriate design for this study, because it limited the observation bias that might have been introduced with a prospective study.
CONCLUSION
This study assessed the level of documentation of clinical interventions in patients’ medical records by pharmacists on 4 inpatient units at the CHUM. Despite the increased availability and use of advanced technology, objective data supporting clinical functions can be difficult to quantify. This study highlights variability in the level of documentation. The guidelines of the ASHP and the CSHP state that all significant clinical recommendations and interventions should be documented; however, these guidelines do not indicate the minimal documentation rates recommended or how often documentation should be done during a patient’s hospitalization. With the constant evolution of pharmacy practice, further studies are needed to evaluate documentation by pharmacists in health care establishments. Such studies could help in establishing comprehensive guidelines to ensure that pharmacists document information and interventions in patients’ medical records.
Footnotes
Competing interests: Jean-Philippe Adam has received honoraria and consulting fees from Apobiologix, Novartis, Amgen, Abbvie, Janssen, and Teva, for activities unrelated to the study reported here. No other competing interests were declared.
Funding: None received.
References
- 1.American College of Clinical Pharmacy. The definition of clinical pharmacy. Pharmacotherapy. 2008;28(6):816–7. doi: 10.1592/phco.28.6.816. [DOI] [PubMed] [Google Scholar]
- 2.Hepler CD. Clinical pharmacy, pharmaceutical care, and the quality of drug therapy. Pharmacotherapy. 2004;24(11):1491–8. doi: 10.1592/phco.24.16.1491.50950. [DOI] [PubMed] [Google Scholar]
- 3.American College of Clinical Pharmacy. Burke JM, Miller WA, Spencer AP, Crank CW, Adkins L, Bertch KE, et al. Clinical pharmacist competencies. Pharmacotherapy. 2008;28(6):806–15. doi: 10.1592/phco.28.6.806. [DOI] [PubMed] [Google Scholar]
- 4.Documentation of pharmacists’ activities in the health record: guidelines. Ottawa (ON): Canadian Society of Hospital Pharmacists; 2013. Available from: https://www.cshp.ca/guidelines. [Google Scholar]
- 5.American Society of Health-System Pharmacists. ASHP guidelines on documenting pharmaceutical care in patient medical records. Am J Health Syst Pharm. 2003;60(7):705–7. doi: 10.1093/ajhp/60.7.705. [DOI] [PubMed] [Google Scholar]
- 6.SHPA Committee of Specialty Practice in Clinical Pharmacy. SHPA standards of practice for clinical pharmacy. J Pharm Pract Res. 2011;41(Suppl) [Google Scholar]
- 7.Zierler-Brown S, Brown TR, Chen D, Blackburn RW. Clinical documentation for patient care: models, concepts, and liability considerations for pharmacists. Am J Health Syst Pharm. 2007;64(17):1851–8. doi: 10.2146/ajhp060682. [DOI] [PubMed] [Google Scholar]
- 8.Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: monitoring and patient education—2006. Am J Health Syst Pharm. 2007;64(5):507–20. doi: 10.2146/ajhp060669. [DOI] [PubMed] [Google Scholar]
- 9.Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: monitoring and patient education—2009. Am J Health Syst Pharm. 2010;67(7):542–58. doi: 10.2146/ajhp090596. [DOI] [PubMed] [Google Scholar]
- 10.Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: monitoring and patient education—2012. Am J Health Syst Pharm. 2013;70(9):787–803. doi: 10.2146/ajhp120777. [DOI] [PubMed] [Google Scholar]
- 11.Pullinger W, Franklin BD. Pharmacists’ documentation in patients’ hospital health records: issues and educational implications. Int J Pharm Pract. 2010;18(2):108–15. doi: 10.1211/ijpp.18.02.0006. [DOI] [PubMed] [Google Scholar]
- 12.Ballandras C, Lebel D, Atkinson S, et al. Inscription des interventions pharmaceutiques au dossier de santé des patients. J Pharm Clin. 2016;35(1):29–34. [Google Scholar]
- 13.Standards de pratique. Montréal (QC): Ordre des pharmaciens du Québec; 2016. [cited 2018 Oct 30]. Available from: http://www.opq.org/doc/media/290_38_fr-ca_0_standards_pratique_vf.pdf. [Google Scholar]
- 14.Programme de surveillance de l’exercice professionnel des pharmaciens: où en sommes nous? L'interaction [Ordre des pharmaciens du Québec] 2017;6(2):11–16. Available from: www.myvirtualpaper.com/doc/odp/iinteraction-v6n2/2016112301/ #15 [cited 2018 Oct 30] [Google Scholar]
- 15.Condren ME, Haase MR, Luedtke SA, Gaylor AS. Clinical activities of an academic pediatric pharmacy team. Ann Pharmacother. 2004;38(4):574–8. doi: 10.1345/aph.1D384. [DOI] [PubMed] [Google Scholar]
- 16.Lada P, Delgado G., Jr Documentation of pharmacists’ interventions in an emergency department and associated cost avoidance. Am J Health Syst Pharm. 2007;64(1):63–8. doi: 10.2146/ajhp050213. [DOI] [PubMed] [Google Scholar]
- 17.Mekonnen AB, McLachlan AJ, Brien JA. Effectiveness of pharmacist-led medication reconciliation programmes on clinical outcomes at hospital transitions: a systematic review and meta-analysis. BMJ Open. 2016;6(2):e010003. doi: 10.1136/bmjopen-2015-010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mekonnen AB, McLachlan AJ, Brien JA. Pharmacy-led medication reconciliation programmes at hospital transitions: a systematic review and meta-analysis. J Clin Pharm Ther. 2016;41(2):128–44. doi: 10.1111/jcpt.12364. [DOI] [PubMed] [Google Scholar]
- 19.Taylor CT, Church CO, Byrd DC. Documentation of clinical interventions by pharmacy faculty, residents, and students. Ann Pharmacother. 2000;34(7):843–7. doi: 10.1345/aph.19310. [DOI] [PubMed] [Google Scholar]
- 20.Andrus MR, Stevenson TL, Eiland LS. Documentation of clinical interventions by pharmacy students and recent pharmacy graduates. Am J Health Syst Pharm. 2016;73(23):1916–8. doi: 10.2146/ajhp160281. [DOI] [PubMed] [Google Scholar]
- 21.Divall MV, Zikaras B, Copeland D, Gonyeau M. School-wide clinical intervention system to document pharmacy students’ impact on patient care. Am J Pharm Educ. 2010;74(1):14. doi: 10.5688/aj740114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jokanovic N, Wang KN, Dooley MJ, Laic S, Tan EC, Kirkpatrick CM, et al. Prioritizing interventions to manage polypharmacy in Australian aged care facilities. Res Social Adm Pharm. 2017;13(3):564–74. doi: 10.1016/j.sapharm.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 23.Sen S, Siemianowski L, Murphy M, McAllister SC. Implementation of a pharmacy technician-centered medication reconciliation program at an urban teaching medical center. Am J Health Syst Pharm. 2014;71(1):51–6. doi: 10.2146/ajhp130073. [DOI] [PubMed] [Google Scholar]
- 24.Irwin AN, Ham Y, Gerrity TM. Expanded roles for pharmacy technicians in the medication reconciliation process: a qualitative review. Hosp Pharm. 2017;52(1):44–53. doi: 10.1310/hpj5201-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freeman C, Cottrell WN, Kyle G, Williams I, Nissen L. Integrating a pharmacist into the general practice environment: opinions of pharmacist’s, general practitioner’s, health care consumer’s, and practice manager’s. BMC Health Serv Res. 2012;12:229. doi: 10.1186/1472-6963-12-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guirguis LM, Hughes CA, Makowsky MJ, Sadowski CA, Schindel TJ, Yuksel N. Survey of pharmacist prescribing practices in Alberta. Am J Health Syst Pharm. 2017;74(2):62–9. doi: 10.2146/ajhp150349. [DOI] [PubMed] [Google Scholar]
- 27.Heck T, Gunther M, Bresee L, Mysak T, Mcmillan C, Koshman S. Independent prescribing by hospital pharmacists: patterns and practices in a Canadian province. Am J Health Syst Pharm. 2015;72(24):2166–75. doi: 10.2146/ajhp150080. [DOI] [PubMed] [Google Scholar]
- 28.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–9. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 29.Nurgat ZA, Al-Jazairi AS, Abu-Shraie N, Al-Jedai A. Documenting clinical pharmacist intervention before and after the introduction of a web-based tool. Int J Clin Pharm. 2011;33(2):200–7. doi: 10.1007/s11096-010-9466-x. [DOI] [PubMed] [Google Scholar]
- 30.Zimmerman CR, Smolarek RT, Stevenson JG. A computerized system to improve documentation and reporting of pharmacists’ clinical interventions, cost savings, and workload activities. Pharmacotherapy. 1995;15(2):220–7. [PubMed] [Google Scholar]
- 31.Robinson SM, Harrison BD, Lambert MA. Effect of a preprinted form on the management of acute asthma in an accident and emergency department. J Accid Emerg Med. 1996;13(2):93–7. doi: 10.1136/emj.13.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rector KB, Veverka A, Evans SK. Improving pharmacist documentation of clinical interventions through focused education. Am J Health Syst Pharm. 2014;71(15):1303–10. doi: 10.2146/ajhp130670. [DOI] [PubMed] [Google Scholar]