Abstract
Background: Horner’s Syndrome is defined by myosis, enophthalmos, lack of sweating and eyelid ptosis, as well as vascular dilatation of one half of the face, caused by damage of the ipsilateral cervical sympathetic chain. It is known that Horner’s syndrome is an unusual complication of thyroidectomy and selective lateral neck dissection. Its exact pathophysiology is not totally explained and its treatment remains conservative. Case presentation: A 27-year-old man developed one-sided partial eyelid ptosis, enophthalmos and myosis two hours after a total thyroid gland excision and a selective lateral neck dissection for papillary carcinoma. A clinical diagnosis of Horner’s syndrome was formed. He was treated conservatively and presented with an incomplete recovery at a 2-month follow up. Conclusions: The present case report underlines the adjacent anatomical correlation between the thyroid gland, the celluloadipose tissue and the cervical sympathetic trunk throughout thyroidectomy and selective lateral neck dissection. Every surgeon should be familiar with the potential complications in order to preoperatively counsel patients, as well as avoid them during the surgical procedure.
Keywords: Horner’s syndrome , cervical sympathetic chain damage, thyroidectomy, selective lateral neck dissection
Background
It has been previously observed that Horner’s syndrome (HS) [1] is characterized by vascular dilatation, myosis, enophthalmos, eyelid ptosis and lack of sweating.
Also one half of the face, following impairment of the ipsilateral cervical sympathetic trunk.
HS following thyroid cancer and surgical intervention is an uncommon complication.
The adjacent relation between the thyroid gland, the internal jugular vein and the cervical sympathetic trunk, renders the latter an insecure structure during neck dissection [2].
We present a case of HS arising from sympathetic chain involvement after a total thyroidectomy and a selective lateral neck dissection (SLND) including levels II, III, IV, V, VI for papillary carcinoma.
No difficulties or unexpected findings came up during the surgical procedure.
Case Presentation
A 27-year-old man was presented to our surgical department due to an ultrasonographic examination which revealed a moderate-sized multinodular goiter and lymph nodes on the right side of the neck (level IV), all of which showed ultrasonographic characteristics that highly indicated malignancy. (Fig.1,2,3)
Figure 1.

B-mode US shows a solid nodule measuring 16x12x10mm in the upper right lobe of the thyroid with peripheral and central calcifications
Figure 2.
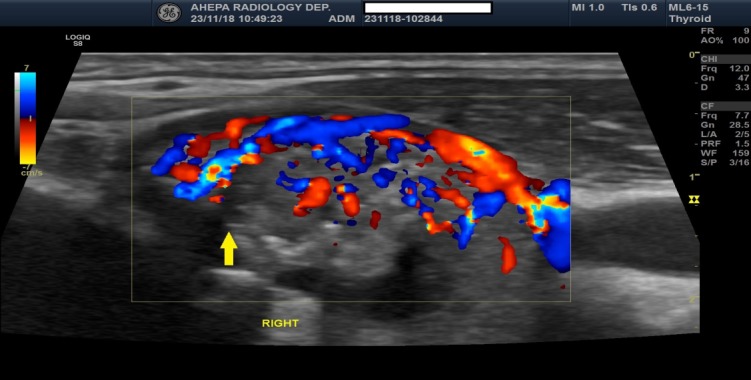
Color Doppler US shows the right thyroid lobe with a hypervascular solid nodule with a secondary blood supply
Figure 3.

B-mode US shows a neck lymph node measuring 10mm with central fusion in level IV of the neck
A Fine Needle Aspiration Biopsy (FNAB) was undertaken and was found positive for papillary carcinoma (Bethesda VI).
The patient’s personal, familial and surgical history was clear, while his social history included rare alcohol consumption and was negative for any tobacco or drug use. General physical examination and routine blood tests were within normal limits.
The patient underwent a total thyroidectomy and a selective lateral neck dissection including levels II, III, IV, V, VI.
Both recurrent laryngeal nerves were identified with the use of intraoperative neurostimulation and preserved. The parathyroid glands were conserved bilaterally according to the basic technique. No difficulties or strange findings came up during the surgical procedure (Fig.4).
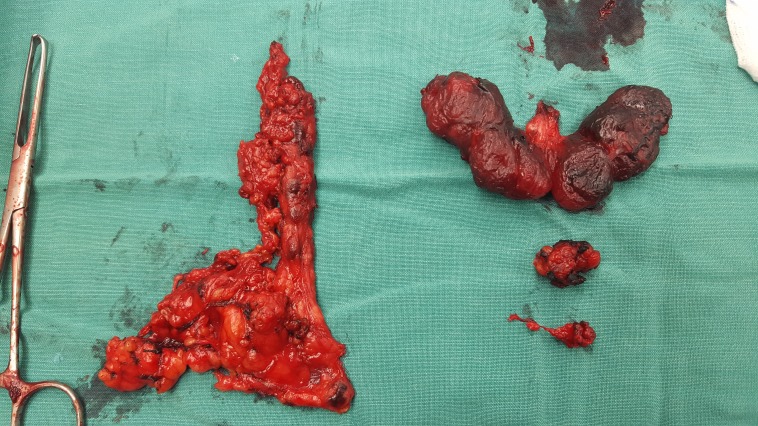
Figure 4.
Surgical specimen after surgery
Two hours after the surgery the patient presented partial eyelid ptosis, mild enophthalmos and myosis on the right side of his face. Neither anhidrosis nor vascular dilatation were noticed on the unilateral face (Fig.5).
Figure 5.
Two hours after surgery the patient was detected to have right-sided partial
A clinical diagnosis of HS was made. The patient was treated conservatively and by the time he was dismissed from the clinic, on postoperative day 3, he showed minor improvement in the ptosis.
The histopathological examination confirmed the original diagnosis of thyroid papillary carcinoma (Fig.6 and 7) and cervical lymph node metastasis in 6 out of the 43 lymph nodes that had been removed (Fig.8). The papillary carcinoma cells were found immunopositive for Galactine 3 (Fig.9), as well as for CK 19 (Fig.10), and negative for CD 56 (Fig.11).
Figure 6.
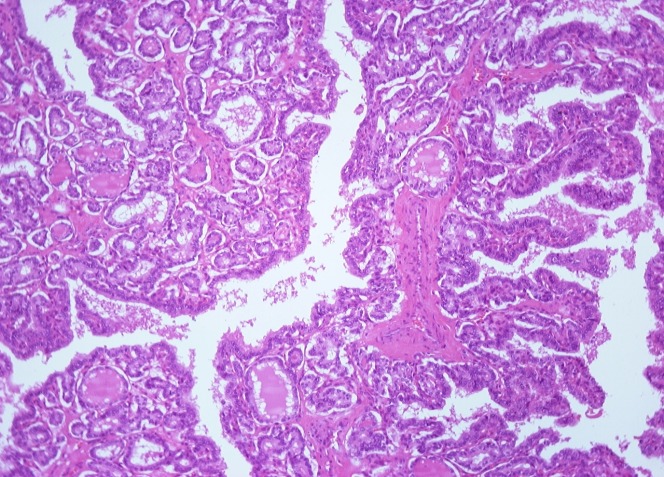
Conventional Papillary Thyroid Carcinoma. The papillae are composed of a central fibrovascular stalk covered by a neoplastic epithelial lining. The nuclei of the neoplastic cells show changes in size and shape, irregularities of the membrane and often overlapping (x100 HE)
Figure 7.
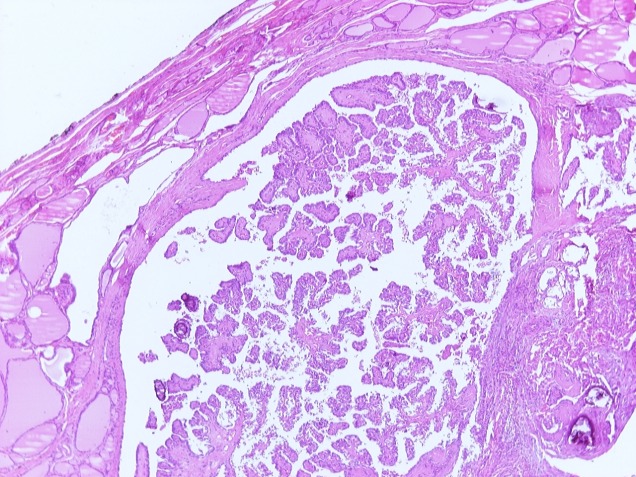
Conventional Papillary Thyroid Carcinoma. The papillae are composed of a central fibrovascular stalk covered by a neoplastic epithelial lining. The nuclei of the neoplastic cells show changes in size and shape, irregularities of the membrane and often overlapping (x40 HE)
Figure 8.
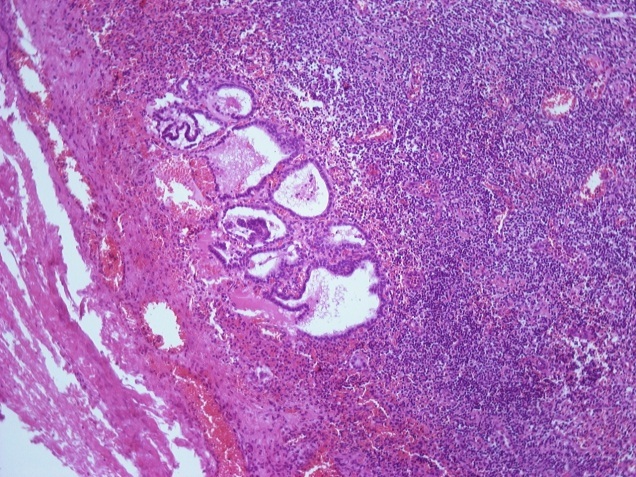
A metastasis from the PTC is present in this lymph node (x100 HE)
Figure 9.
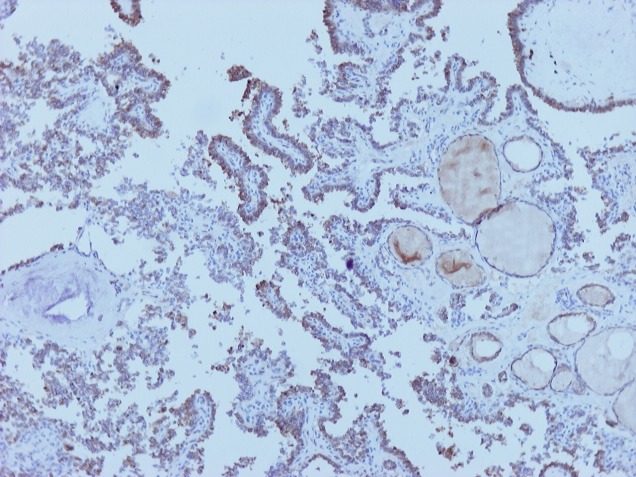
PTC cells are immunoactive for GAL 3 (x100 HE)
Figure 10.
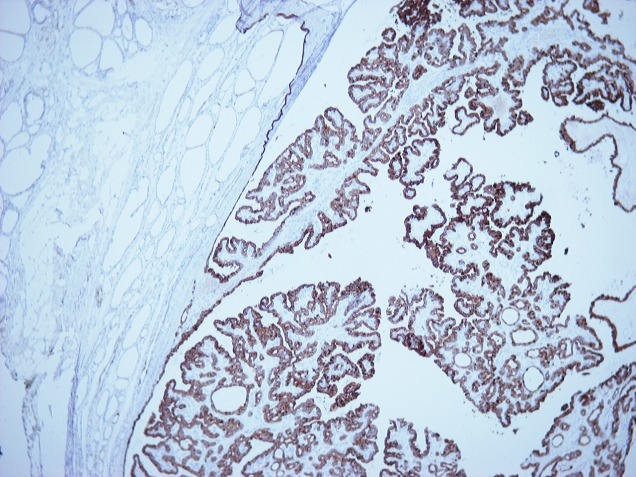
PTC cells are negative for CD 56 (x100 HE)
Figure 11.
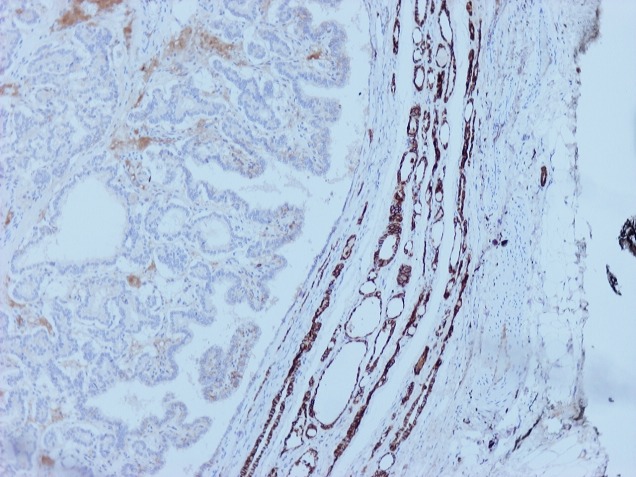
PTC cells are immunoactive for CK 19 (x40 HE)
At the moment, and at-2 months after surgery the patient’s symptoms have shown a slight improvement, with signs of HS however still present.
Discussions
HS develops with myosis, enophthalmos, eyelid ptosis, with or without anhidrosis and vascular dilatation of the ipsilateral part of the face, following an injury of the cervical sympathetic trunk [3].
The anatomy describes the sympathetic trunk which lies deeply posteriorly and medial to the carotid artery [4].
The probable causes of HS following thyroidectomy and selective lateral neck dissection, include direct damage of the stellate ganglion, strain of the sympathetic trunk during lateral retraction, ischemia-caused neural impairment, postoperative hematoma compressing the cervical sympathetic chain and finally damage of the communication between the cervical sympathetic trunk and the recurrent laryngeal nerve [3].
In 2004, Harding et al. stated that the possibility of postoperative HS rises with more expanded surgery, such as lateral lymph node dissection [5].
There is no uniformal pattern in the onset of Horner`s Syndrome after the surgery.
The majority of cases however seems to appear between the second and the fourth postoperative day [6,7,8].
The patient of the present case report had a very early onset of HS, only two hours after surgery, and was treated conservatively.
Conclusion
It is known that Horner’s syndrome-is an injury to the cervical sympathetic chain following thyroid surgical interventions, is quite an unusual complication of thyroidectomy.
Therefore surgeons operating the thyroid gland should always take cautions since that it is a vulnerable structure and should be familiar with the related complications.
There can be significant cosmetic concerns for the patients and therefore it is important to counsel patients preoperatively.
Conflict of Interest
None to declare.
Ethics Statement
Written informed consent has been provided by the patient to have the case details and any accompanying images published.
Investigational Review Board approval was acquired for the publication of the present case report from the investigational review board of the 3rd Surgery Department of “AHEPA” University Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece. Although it was not required.
References
- 1.Rai W, Olcese V, Elsheikh B, Stino AM. Horner's Syndrome as Initial Manifestation of Possible Brachial Plexopathy Neurolymphomatosis. Frontiers in neurology. 2019;10:4–4. doi: 10.3389/fneur.2019.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaha AR. Complications of neck dissection for thyroid cancer. Annals of surgical oncology. 2008;15(2):397–399. doi: 10.1245/s10434-007-9724-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cozzaglio L, Coladonato M, Doci R, Travaglini P, Vizzotto L, Osio M, Gennari L. Horner's syndrome as a complication of thyroidectomy: report of a case. Surgery today. 2008;38(12):1114–1116. doi: 10.1007/s00595-007-3741-z. [DOI] [PubMed] [Google Scholar]
- 4.Prim MP, De Diego JI, Verdaguer JM, Sastre N, Rabanal I. Neurological complications following functional neck dissection. European archives of oto-rhino-laryngology: official journal of the European Federation of Oto-Rhino-Laryngological Societies. 2006;263(5):473–476. doi: 10.1007/s00405-005-1028-9. [DOI] [PubMed] [Google Scholar]
- 5.Harding JL, Sywak MS, Sidhu S, Delbridge LW. Horner's syndrome in association with thyroid and parathyroid disease. ANZ journal of surgery. 2004;74(6):442–445. doi: 10.1111/j.1445-1433.2004.03030.x. [DOI] [PubMed] [Google Scholar]
- 6.Seneviratne SA, Kumara DS, Drahaman AM. Horner's syndrome: an unusual complication of thyroidectomy: a case report. Journal of medical case reports. 2016;10(1):300–300. doi: 10.1186/s13256-016-1072-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Italiano D, Cammaroto S, Cedro C, Bramanti P, Ferlazzo E. Horner syndrome following thyroidectomy. Neurological sciences: official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2011;32(3):531–531. doi: 10.1007/s10072-010-0451-x. [DOI] [PubMed] [Google Scholar]
- 8.Solomon P, Irish J, Gullane P. Horner's syndrome following a thyroidectomy. The Journal of otolaryngology. 1993;22(6):454–456. [PubMed] [Google Scholar]