Abstract
Background
The effect of maxillary implant overdentures on masticatory ability in edentulous patients with complaints regarding their conventional maxillary dentures is unknown.
Purpose
To assess the change in objective masticatory ability (mixing ability index, MAI), patient reported masticatory ability (questionnaire), and patient satisfaction (GSS) after maxillary implant overdenture treatment with either solitary attachments or bars.
Materials and Methods
Two groups randomly received four‐implant maxillary overdentures on either solitary attachments (group I, n = 25) or bars (group II, n = 25). The MAI, questionnaire, and GSS were scored before (T0) and 12 months (T12) after treatment.
Results
After treatment, both groups had significantly better MAI outcomes, better questionnaire scores and better GSS. Post‐treatment questionnaire scores and GSS were significantly better for group II. Before treatment a strong, positive correlation between the MAI and the questionnaire was found for all participants who had had full conventional dentures combined (group I, n = 17; group II, n = 3).
Conclusion
Mixing ability was the same for all the participants treated with maxillary implant overdentures on either solitary attachments or bars. Patient reported masticatory ability and satisfaction was better for participants treated with maxillary implant overdentures on bars. There was a correlation between MAI and patient reported masticatory ability in participants with full conventional dentures.
Keywords: dentures, humans, mastication, overdentures, prospective studies, quality of life
1. INTRODUCTION
When patients are provided with conventional dentures, improvements are reported with regard to aesthetics, comfort, and speech, but the improvement in masticatory ability is often unsatisfactory and patient satisfaction is thereby often rather low.1 A common way to try to improve masticatory ability and patient's satisfaction is to place implants to retain a mandibular2, 3 and/or maxillary4, 5, 6, 7 denture. It has been shown that patients treated with mandibular implant overdentures can chew better,8, 9 need fewer chewing cycles,10 and can eat hard food better11 than patients with conventional dentures. Also masticatory ability and bite force are improved by implant overdenture treatment, but neither of them work at the same level as individuals with natural dentitions.12 However, no studies have assessed the masticatory ability of both maxillary and mandibular implant overdentures yet.1, 8, 10, 11, 13
A variety of methods are used to measure masticatory ability and the degree of breakdown can be measured using real test foods (peanuts, carrots, etc)8, 14, 15 or artificial materials (eg, Optosil and Optocal).16, 17, 18, 19 The consistency of the latter two materials is more standardized than that of real test foods. Studies have shown that patients with a compromised oral function are not always able to fragment the real or artificial test food; their maximum bite force can be below the force needed to break the test food particles. Other methods to assess masticatory ability include the evaluation of: mandibular border movements during chewing and chewing patterns;20 swallowing threshold;2 jaw muscle activity and maximum bite force;10 blood plasma levels of homocysteine, vitamin B12, vitamin B6, albumin, serum folate, and C‐reactive protein concentrations; questionnaires to rate the difficulty associated with chewing foods of various textures;1 body mass index;13, 21 and two‐colored gum mixing ability tests.11, 13 Of all these tests, the two‐colored wax mixing ability test is much better at discriminating between people with compromised masticatory ability.22 Therefore, this test was chosen for the current study.
As mentioned above, no studies have assessed the masticatory ability of both maxillary and mandibular implant overdentures.1, 8, 10, 11, 13 Therefore, the aim of our study was to assess the objective masticatory ability (mixing ability test), the participants' reported (subjective questionnaire) masticatory ability as well as the participants' satisfaction (general satisfaction score) with the provided maxillary implant overdentures 1 year after placement. These parameters were assessed for two groups of participants from an randomized controlled trial (RCT) about the treatment outcome of maxillary implant overdentures on a bar attachment system or a solitary attachment system (Locator; Zest Anchors Inc, Escondido, California).
2. MATERIALS AND METHODS
2.1. Patient population
Between January 2013 and January 2016, a total of 50 consecutive patients were approached and included in this RCT with parallel design at the Department of Oral and Maxillofacial Surgery (University Medical Center Groningen, The Netherlands [UMCG]). All the patients were referred to the UMCG because of persistent complaints regarding their conventional maxillary dentures. The participants in our trial had to have been edentulous in the maxilla for at least 1 year and they had to have sufficient bone volume to place the implants. All the participants received a written explanation of the study and written informed consent was obtained from each patient after a further explanation in person of the clinical trial. The study was approved by the Medical Ethical Committee of the UMCG (ABR NL43293.042.13) and was registered in the Netherlands National Trial Register (NTR3813). The participants were randomly divided into two groups by the means of sealed envelopes. Group I: participants receiving maxillary implant overdentures on a solitary attachment system (n = 25) (Figure 1A); Group II: participants receiving maxillary implant overdentures on a bar attachment system (n = 25) (Figure 1). G.C.B. generated the random allocation sequence, enrolled participants and assigned participants to interventions.
Figure 1.

A, Intraoral view of patient with locators. B, Intraoral view of a patient with bars. C, View of intaglio surface of maxillary overdenture with chromium alloy structure, denture caps, and nylon males. D, View of intaglio surface of maxillary overdenture with chromium alloy structure and gold retentive clips
2.2. Selection bias
The random sequence was generated by printing 50 cards (25 with “locator” and 25 with “bar”). The cards were put in opaque, sealed envelopes. The envelopes were shuffled and numbered sequentially. The allocation sequence was concealed until after the prosthodontist made the individual impression. At that moment in time G.C.B. opened the envelop to assign the participant to either group I or II.
2.3. Performance bias
For this study, it was not possible to blind participants and personnel. It is not likely, however, that the outcome is influenced by lack of blinding.
2.4. Detection bias
Blinding was not possible for the outcome assessors. There is no doubt, however, about the outcomes, because they are derived from a validated analyzing technique for the MAI and the answers of a questionnaire.
2.5. Surgical and prosthetic procedures
All the surgical procedures were performed by one oral and maxillofacial surgeon (GMR) at the UMCG. The prosthetic procedures were accomplished by one prosthodontist (HJAM). Manufacturing of the superstructure was done by a single experienced dental laboratory. All participants received four dental implants (NobelActive Narrow Platform [Nobel Biocare USA, LLC, Yorba Linda, California]) in the maxillary anterior region (group I and II). Participants who were fully edentulous before treatment had two mandibular implants (NobelReplace Select TC [Nobel Biocare USA, LLC, Yorba Linda, California]) placed simultaneously as the ones in the maxilla (17 participants in group I and three participants in group II). The implants in the maxilla were placed according to a two‐stage surgical protocol.
After a 3‐month osseointegration period, second stage surgery was performed and healing abutments were placed and the prosthetic procedures were initiated. A bilateral balanced occlusion concept was followed. The final superstructure consisted of a solitary attachment system (Locator; Zest Anchors Inc, Escondido, California) (group I) (Figures 1C and 2A) or a milled titanium egg‐shaped bar23, 24, 25 with distal extensions (max. 8 mm long), screw‐retained to abutments (custom made by Maxillofacial Dental Laboratory G. van Dijk, Groningen, The Netherlands, milling company: ES Healthcare NV, Hasselt, Belgium) (group II) (Figures 1D and 2B), and an implant overdenture with, respectively, Locator male self‐aligns and pivots (group I) or a cobalt chromium reinforcement structure and gold retentive clips (Cendres +Métaux, Biel/Bienne, Switzerland)26 (group II). Regarding the solitary attachments, the nylon male elements are available in different color‐coded designs with different retention forces (blue 6.7 N [light], pink 13.4 N [medium], clear 22.3 N [strong]). In the present study, all participants were initially provided with pink inserts (13.4 N; medium force), providing possibilities for strengthening or loosening the retention force. The maxillary implant overdentures were designed with full coverage of the alveolar process, but without palatal coverage. The superstructures of the maxillary and mandibular implant overdentures placed in participants without any implants before treatment were the same whereby both implant overdentures had either a bar attachment system or solitary attachments.
Figure 2.
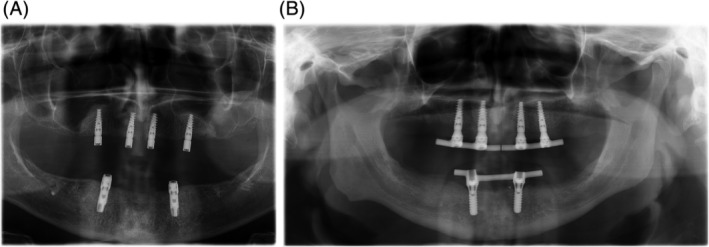
A, Panoramic radiograph of a patient with locators. B, Panoramic radiograph of a patient with bars
2.6. Outcome measures
The primary outcome measure of this analysis was masticatory ability by means of the mixing ability test. The secondary outcomes were self‐reported masticatory ability (for details of the tests see below) and patient satisfaction according to their general satisfaction score. All the parameters were scored before treatment and 12 months after placement of the implant overdenture. All the measurements were done by one researcher (GCB) not involved in the treatment of the participants.
2.7. Mixing ability test
The mixing ability test22, 27 measures how well a subject mixes a tablet (diameter 20 mm), which consists of a red and a blue wax layer (3 mm each), after 20 chewing strokes. The wax tablets were offered to the participants at room temperature (20°C). The chewed wax was rinsed, dried, and stored. To measure the amount of mixing, the chewed wax was brought up to a temperature of 28°C and placed between two sheets of stiff and clear foil. The sandwich of foil and wax was pressed between two thick brass plates to a thickness of 2.0 mm. Then, both sides of the wax were optically scanned using a high‐quality scanner (Epson V750, Long Beach, California). The images of the wax were processed using Adobe Photoshop, CS3 extended (Adobe, San Jose, California). The spread of the color intensities in the combined image of both sides is the measure of mixing. If the wax tablet has not been chewed, one side is red and the other is blue, and the spread of the intensities of both colors is maximal. Chewing the tablet mixes the colors, whereupon first intermediate intensities appear and the more the tablet is chewed, the more the spread of the intensities decreases. So, a high spread intensity of, for example, 30 is caused by the red and blue layers of the wax tablet being badly mixed, which means a low mixing performance. This spread is referred to as the mixing ability index (MAI).
2.8. Masticatory ability questionnaire
All the participants were asked to complete a masticatory ability questionnaire.4, 28, 29 In this questionnaire, participants have to rate their opinion about their ability to chew nine different food items on a 3‐point rating scale (0 = good, 1 = moderate, 2 = bad). The items were grouped into three categories: (1) “soft food” (boiled vegetables and potatoes, crustless bread, minced meat); (2) “tough food” (crusty bread, steak, Gouda cheese); (3) “hard food” (apple, carrot, peanuts). The category total score and each item's total score were reported. The maximum score was 18 points.
2.9. Patient satisfaction
Patient satisfaction with the maxillary implant overdenture was measured with a general satisfaction score ranging from 0 to 10, with 0 representing a bad outcome and 10 a good outcome.4, 8, 29, 30
2.10. Data analysis
Intergroup differences with regard to the scores of the mixing ability test (continuous data) were analyzed using the Student's t‐test. Intragroup differences for the scores of the mixing ability test before and 1 year after treatment were analyzed with paired sample t‐tests.
The results of each group's masticatory ability questionnaires and general satisfaction scores (ordinal data) were analyzed with a Wilcoxon Matched Pairs Signed Ranks test. Intergroup differences were analyzed by applying the independent samples Mann‐Whitney U test.
Spearman's correlation was used to determine the relationship between the total score of the masticatory ability questionnaire and the MAI outcome. A P‐value of less than 0.05 was considered statistically significant. All analyses were performed with the SPSS 23.0 software (SPSS, Inc, Chicago, Illinois).
3. RESULTS
Fifty participants with a mean age of 62.4 ± 7.3 years (range 37.5‐75.0 years) were initially included in this study. Twenty five were placed in group I and 25 in group II (both groups 13 male/12 female participants, mean age group I 60.1 ± 8.6 years (range 37.5‐75.0 years), mean age group II 63.8 ± 5.4 years (range 53.0‐72.6 years). Then, two participants deceased before the 1‐year follow‐up and one patient was lost to follow‐up (moved without leaving an address). Consequently, 47 participants were available for the 1‐year evaluation: 23 participants in group I and 24 participants in group II.
Pairwise deletion was used for missing data and intergroup comparisons. Listwise deletion was used for missing data and intragroup comparisons. The reasons for missing data were not related to treatment or the outcome measures. Missing data was balanced in numbers and with similar reasons across the intervention groups.
Three participants in group I lost one implant during the osseointegration phase (96.9% survival). Two participants in group II lost one implant during the osseointegration phase (98.0% survival). We decided to continue and used the remaining three implants for the construction of the superstructure. One patient in group I requested to replace the lost implant after 3 months of functioning with the implant overdenture on three implants.
All participants were initially provided with pink inserts. Four participants requested strengthening of the retention force immediately after placement of the overdenture. Three participants received two pink and two clear inserts and one participant received two clear and two green inserts. There were no statistically significant differences between these patients and patients that did not request strengthening of the retention force with regard to MAI outcomes, questionnaire outcomes, or general satisfaction scores.
3.1. Objective mixing ability test
Both groups had significantly better post‐treatment than pretreatment MAI outcomes (Table 1). There was no significant difference in the amount of improvement between the groups (Table 1). Also, there was no significant difference in pre‐ and post‐MAI outcomes between the groups (Table 2).
Table 1.
Mean and standard deviation (± SD) of the outcomes of the mixing ability index (MAI) and median and interquartile range (Q1 − Q3) of the total score and the scores of the three items of the masticatory performance questionnaire (MPQ); and of the general satisfaction score (GSS) before (T0) and after treatment (T12); difference in score between T0 and T12; and comparative analyses
| Group I | Group II | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| T0, n = 25 | T0, n = 25 | Group I | Group II | ||||||
| T12, n = 23 | T12, n = 24 | Difference in score between | Difference in score between | ||||||
| T0 | T12 | P‐value | T0 | T12 | P‐value | T0 − T12 | T0 − T12 | P‐value | |
| MAI | 20.5(±3.4) | 18.0(±1.7) | 0.001** , a | 20.2(±3.5) | 17.8(±2.6) | 0.001** , a | 2.6(±3.4) | 2.5(±3.4) | 0.917a |
| Total score MPQ | 8 (4‐14) | 4 (2‐7) | 0.001**, b | 9 (8‐12) | 0 (0‐3) | 0.000***, b | 4 (1‐9) | 8 (6‐10) | 0.025* , b |
| Soft food | 1 (0‐5) | 0 (0‐1) | 0.003** , b | 2 (1‐3) | 0 (0‐0) | 0.000*** , b | 1 (0‐4) | 2 (1‐3) | 0.385b |
| Tough food | 1 (1‐4) | 0 (0‐1) | 0.003** , b | 2 (1‐3) | 0 (0‐0) | 0.000*** , b | 1 (0‐4) | 2 (1‐2) | 0.344b |
| Hard food | 6 (4‐6) | 3 (2‐6) | 0.007** , b | 5 (5‐6) | 0 (0‐2) | 0.000*** , b | 1 (0‐4) | 5 (3‐6) | 0.002** , b |
| GSS | 4 (1‐6) | 8 (7‐9) | 0.000*** , b | 4 (2‐6) | 9 (8‐10) | 0.000*** , b | 4 (2‐6) | 5 (4‐7) | 0.340b |
Paired samples t‐test.
Wilcoxon matched pairs signed ranks test.
*P < 0.05, **P < 0.01, ***P < 0.001.
Table 2.
Mean and standard deviation (± SD) of the outcomes of the mixing ability index (MAI) and median and interquartile range (Q1 − Q3) of the total score the scores of the three items of the masticatory performance questionnaire (MPQ); and of the general satisfaction score (GSS) before (T0) and after treatment (T12). A comparative intergroup analysis
| Group I | Group II | Comparative analysis | |
|---|---|---|---|
| T0, n = 25 | T0, n = 25 | ||
| T12, n = 23 | T12, n = 24 | ||
| MAI − T0 | 20.5(±3.4) | 20.2(±3.5) | 0.779a |
| Total score MPQ − T0 | 8 (4‐14) | 9 (8‐12) | 0.783b |
| Soft food − T0 | 1 (0‐5) | 2 (1‐3) | 0.933b |
| Tough food − T0 | 1 (1‐4) | 2 (1‐3) | 0.792b |
| Hard food − T0 | 6 (4‐6) | 5 (5‐6) | 0.822b |
| GSS − T0 | 4 (1‐6) | 4 (2‐6) | 0.607b |
| MAI − T12 | 18.0(±1.7) | 17.8(±2.6) | 0.628a |
| Total score MPQ − T12 | 4 (2‐7) | 0 (0‐3) | 0.001** , b |
| Soft food − T12 | 0 (0‐1) | 0 (0‐0) | 0.043*, b |
| Tough food − T12 | 0 (0‐1) | 0 (0‐0) | 0.016* , b |
| Hard food − T12 | 3 (2‐6) | 0 (0‐2) | 0.000*** , b |
| GSS − T12 | 8 (7‐9) | 9 (8‐10) | 0.041* , b |
Independent t‐test.
Mann‐Whitney U test.
*P < 0.05, **P < 0.01, ***P < 0.001.
3.2. Patient reported questionnaire
Both groups had significantly better post‐treatment scores on the masticatory ability questionnaires compared to the pretreatment ones; both groups' ability to chew soft, tough, and hard foods had improved significantly (Table 1). However, there was a significant difference between the groups in the amount of improvement at the scores on the masticatory ability questionnaires and the ability to chew hard foods, in favor of group II (Table 1).
There was no significant difference between both groups' total scores on the pretreatment masticatory ability questionnaires. There was a significant difference between the groups' post‐treatment total scores and their ability to chew hard, tough, and soft foods in favor of group II (Table 2).
3.3. General satisfaction score
Both groups had a significantly better general satisfaction post‐treatment than pretreatment score (Table 1). There was no significant difference in the amount of improvement between the groups (Table 1).
The inter group pretreatment general satisfaction scores were not significantly different. The inter group post‐treatment general satisfaction scores were significantly different, in favor of group II (Table 2).
3.4. Relation between patient reported (subjective) and objective masticatory ability
A Spearman's correlation was run to determine the relationship between the MAI outcome and the masticatory ability questionnaires' total score.
The pretreatment data (group I and II) demonstrated a statistically significant weak, positive monotonic correlation between the MAI outcome and the total score of the masticatory ability questionnaires (r s = 0.39, n = 50, P [one‐tailed] 0.002).
The groups were combined and then split into participants with and participants without mandibular implant overdentures. The pretreatment results of the participants with full conventional dentures gave a statistically significant, strong, positive monotonic correlation between the MAI outcome and the total score of the masticatory ability questionnaire (r s = 0.59, n = 20, P [one‐tailed] 0.001). The pretreatment results of the participants with mandibular implant overdentures gave no statistically significant correlation between the MAI outcome and the total score of the masticatory ability questionnaire (r s = 0.18, n = 30, P [one‐tailed] 0.163).
There was no statistically significant post‐treatment correlation between the MAI outcome and the total score of the masticatory ability questionnaire (r s = 0.12, n = 47, P [one‐tailed] 0.227).
3.5. Participants with or without mandibular implant overdentures before treatment
The scores of participant with or without mandibular implant overdentures before treatment did not differ with regard to MAI, pretreatment masticatory ability questionnaires, and GSS. As expected, at baseline there was a significant difference in in the patients' ability to chew hard foods in favor of patients with mandibular implant overdentures (Table 3).
Table 3.
For participants with full conventional dentures (CD) or mandibular implant overdentures (MIOD) before treatment. Mean and standard deviation (± SD) of the outcomes of the mixing ability index (MAI) and median and interquartile range (Q1 − Q3) of the total score the scores of the three items of the masticatory performance questionnaire (MPQ); and of the general satisfaction score (GSS) before (T0) and after treatment (T12). A comparative intergroup analysis
| CD | MIOD | Comparative analysis | |
|---|---|---|---|
| T0, n = 20 | T0, n = 30 | ||
| T12, n = 19 | T12, n = 28 | ||
| MAI − T0 | 21.1(±3.9) | 19.9(±3.1) | 0.214a |
| Total score MPQ − T0 | 10 (7‐16) | 9 (6‐12) | 0.549b |
| Soft food − T0 | 2 (1‐6) | 2 (1‐3) | 0.857b |
| Tough food − T0 | 2 (1‐5) | 2 (1‐3) | 0.618b |
| Hard food − T0 | 6 (4‐6) | 6 (4‐6) | 0.248b |
| GSS − T0 | 4 (1‐6) | 4 (2‐6) | 0.526b |
| MAI − T12 | 18.4(±1.7) | 17.6(±2.5) | 0.326a |
| Total score MPQ − T12 | 2 (3‐8) | 0 (0‐4) | 0.057, b |
| Soft food − T12 | 0 (0‐0) | 0 (0‐0) | 0.118b |
| Tough food − T12 | 0 (0‐0) | 0 (0‐1) | 0.525, b |
| Hard food − T12 | 2 (0‐3) | 0 (0‐3) | 0.035* , b |
| GSS − T12 | 9 (7‐9) | 9 (8‐9) | 0.437, b |
Independent t‐test.
Mann‐Whitney U test.
*P < 0.05, **P < 0.01, ***P < 0.001.
4. DISCUSSION
Wearing maxillary overdentures on four implants results in an improvement in objective masticatory ability, patient reported (subjective) masticatory ability, and patient satisfaction 1 year after placement. There is a difference between maxillary implant overdentures with a bar attachment system or with a solitary attachment system with regard to the patient reported masticatory ability and general satisfaction score in favor of the bar attachment system. There is no difference with regard to the objective masticatory ability.
As mentioned, the objective masticatory ability (mixing ability test) improved after treatment in both groups. This means that participants with maxillary implant overdentures can mix better than participants without maxillary implant overdentures, regardless of the type of attachment system. The participants of both groups also reported personally an improvement in masticatory ability after treatment, which means that both the participants' objective and subjective results show that they can chew better.
The effect of maxillary implant overdenture treatment on mastication was studied by De Albuquerque Junior.31 In contrast to our findings, they found no differences in masticatory ability between a conventional maxillary denture and a maxillary overdenture on implants. This observed difference in masticatory ability between their and our study might be due to the fact that Albuquerque Junior et al randomly selected participants from a population wearing full conventional dentures (mandibular and maxillary). Latter participants first received mandibular fixed prosthesis. Chances are, that a big part of these participants did not have any problems with masticatory ability due to a bad functioning maxillary conventional denture before treatment. They found that scores on the masticatory ability questionnaire did improve when the mandibular fixed prosthesis was introduced, but no further after introduction of the maxillary overdenture. Our participants were all referred to the department due to problems with the retention or stability of the maxillary conventional denture, so they did have severe problems before treatment, therefore, for this group, improvements could still be accomplished after treatment.
In the present study, there is no significant difference between group I and II in the post‐treatment results for objective masticatory ability (Table 2). This is in line with other literature comparing bar attachments or solitary attachment systems for mandibular implant overdentures.10, 32 However, the participants' intergroup post‐treatment subjective results for masticatory ability are significantly different. Participants in group I felt an improvement in mastication, but this improvement is smaller than the improvement in group II (Table 1). Post‐treatment three of the participants in group II reported problems with chewing soft or tough foods (highest score 2, maximum score 6) whereas nine participants in group I reported a problem with chewing soft foods and 10 participants with chewing tough foods (highest score 6, maximum score 6). Resulting in significantly different post‐treatment scores on the masticatory ability questionnaires and with the biggest difference seen for the ability to chew hard foods. The masticatory ability questionnaire is.
It must be noticed that all patient in group I not only had a solitary attachment system for the maxillary overdenture on four implants, but also for the mandibular overdenture on two implants. It has been reported that the stability of a mandibular implant overdenture with a bar attachment system is better than that with a solitary attachment system.33 The design of the pivoting Locator male allows a resilient connection. The retentive nylon Locator male remains in contact with the abutment socket while its titanium denture cap has a full range of rotational movement over the male. When using two implants this results in a nonrigid connection, when using more than two implants (like in the maxilla) the denture cap will have no possibility to move over the male anymore. The smaller improvement in group I for the ability to chew hard foods, might be due to the design of the mandibular implant overdenture.
Another explanation for the greater improvement of the ability to chew hard foods in group II participants might be that a number of these participants are in fact denture wearers with slight maxillary denture problems before but whose problems have shifted from the mandibular to the maxillary denture since mandibular overdenture treatment. Those who were fully edentulous at the start, by contrast, may have had more serious maxillary problems, leading to the indication for implant‐overdenture treatment for the mandible and maxilla simultaneously. The over‐representation of fully edentulous participants with possibly more severe maxillary denture problems in group I could be an explanation for the differences found. Because improvements are more easily reached for the participants with slight maxillary denture problems than for participants with severe denture problems.
The participants are very satisfied with the maxillary implant overdenture treatment as represented by the general satisfaction score (median of 8 and 9 on a 10 point scale). The score is comparable to earlier reported studies on maxillary implant overdentures.5 There is a difference in general satisfaction between a maxillary implant overdenture on solitary attachments or a bar attachment system. Post‐treatment, the GSS for the bar attachment system is slightly higher than the GSS for the solitary attachment. Additionally, the amount of improvement does not differ between the groups. Showing that the evidence for additional value of a maxillary implant overdenture on bars compared to a solitary attachment system to achieve a higher GSS is not very strong. This is supported by the conclusion of a previous study on splinted and unsplinted maxillary overdentures.7 In that study, no differences with regard to patient satisfaction were found between splinted and unsplinted maxillary overdenturese. The reported GSS in our study for the bar overdenture is comparable to those of others.6, 31 Also the scores for the locator overdenture are similar to those of others.7
There is a statistically significant positive monotonic correlation between the subjective and objective results for masticatory ability. This correlation is weak for the total group, but is strong when comparing the pretreatment results of the participants with complete conventional dentures (without any implants). No statistically significant correlation can be found anymore after the treatment, indicating that the worse the masticatory ability the better the correlation between the MAI and the masticatory ability questionnaire. This finding is in line with an earlier published study.34
An explanation for the lack in correlation in the group with better MAI scores could be that the mixing ability test was developed for measuring differences in masticatory ability for groups of participants with compromised oral functions,22 and is less suitable for participants with better masticatory ability.35 The same applies to the masticatory ability questionnaire; this questionnaire might not discriminate enough between participants with better masticatory ability, as seen by the relatively low post‐treatment scores.
Another factor contributing to the correlation between objective and subjective masticatory ability could be that the lower maximum bite force due to pain is the main contributor to the bad reports of masticatory ability by complete denture wearers and not due to their impaired mixing ability.36 It has been found that a higher bite force results in better chewing efficiency.37, 38 However this statement mainly refers to methods that evaluate masticatory ability with brittle test foods, which are usually hard.39
Participants with impaired masticatory ability often cannot chew hard foods at all. The method with a softer wax tablet makes the association between masticatory ability and maximum bite force less coherent, but it is certainly more representative of the type of food denture wearers eat.13
4.1. Limitations
A limitation of the current study are the outcome measures applied. As there is no generally used chewing ability questionnaire, a custom made chewing ability questionnaire was used. Even though this questionnaire has been used in earlier research4, 28, 29 it is not a widely used questionnaire limiting comparability with other studies.
The general satisfaction score was expressed as a numerical rating scale. A numerical rating scale is in itself a good way of measuring. However, as a visual analogue scale (VAS) is more widely applied,6, 7, 31 in future as a routine a VAS should be added to more specific, custom made, questionnaires to ease comparison between studies. Another option would be to use a validated questionnaire such as the oral health impact profile40 to measure general satisfaction.
A second limitation of our study is the skewed distribution between group I and II participants with regard to the presence of patients with mandibular overdentures before treatment. We did not randomize on this matter. In hindsight, it would have been better to use a more balanced method of allocation of participants to the two treatments, taking possible factors of importance to the outcome such as status of the mandible (conventional denture vs implant‐retained overdenture) into account. Another option to prevent this bias would have been to provide all participants with mandibular overdentures first and provide them with the maxillary overdenture later.
The third limitation is the fact that the participants all had a sufficient amount of bone to place implants circumventing the need of bone augmentations before implant placement. Meaning that our results might not be applicable for patients with severe resorption of the alveolar ridge.
5. CONCLUSION
Maxillary implant overdentures improve mixing ability, patient reported masticatory ability, and patient satisfaction. Regarding patient reported masticatory ability and patient satisfaction, a post‐treatment difference is seen between maxillary implant overdentures with solitary attachments or a bar attachment system, in favor of the bar attachment system. There is a correlation between objective outcomes and subjective reports from participants with full conventional dentures.
CONFLICT OF INTEREST
The authors declare that there are no conflicts of interest.
Boven GC, Speksnijder CM, Meijer HJA, Vissink A, Raghoebar GM. Masticatory ability improves after maxillary implant overdenture treatment: A randomized controlled trial with 1‐year follow‐up. Clin Implant Dent Relat Res. 2019;21:369–376. 10.1111/cid.12721
REFERENCES
- 1. Awad MA, Morais JA, Wollin S, Khalil A, Gray‐Donald K, Feine JS. Implant overdentures and nutrition a randomized controlled trial. J Dent Res. 2012;91(1):39‐46. [DOI] [PubMed] [Google Scholar]
- 2. Garrett NR, Kapur KK, Hamada MO, et al. A randomized clinical trial comparing the efficacy of mandibular implant‐supported overdentures and conventional dentures in diabetic patients. Part II. Comparisons of masticatory performance. J Prosthet Dent. 1998;79(6):632‐640. [DOI] [PubMed] [Google Scholar]
- 3. Sun X, Zhai JJ, Liao J, Teng MH, Tian A, Liang X. Masticatory efficiency and oral health‐related quality of life with implant‐retained mandibular overdentures. Saudi Med J. 2014;35(10):1195‐1202. [PMC free article] [PubMed] [Google Scholar]
- 4. Slot W, Raghoebar GM, Cune MS, Vissink A, Meijer HJA. Maxillary overdentures supported by four or six implants in the anterior region: 5‐year results from a randomized controlled trial. J Clin Periodontol. 2013;43(12):1180‐1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Boven GC, Raghoebar GM, Vissink A, Meijer HJA. Improving masticatory performance, bite force, nutritional state and patient's satisfaction with implant overdentures: a systematic review of the literature. J Oral Rehabil. 2015;42(3):220‐233. [DOI] [PubMed] [Google Scholar]
- 6. Kronstrom M, Widbom C, Soderfeldt B. Patient evaluation after treatment with maxillary implant‐supported overdentures. Clin Implant Dent Relat Res. 2006;8(1):39‐43. [DOI] [PubMed] [Google Scholar]
- 7. Al‐Zubeidi MI, Alsabeeha NHM, Thomson WM, Payne AGT. Patient satisfaction with maxillary 3‐implant overdentures using different attachment systems opposing mandibular 2‐implant overdentures. Clin Implant Dent Relat Res. 2012;14(suppl 1):11‐19. [DOI] [PubMed] [Google Scholar]
- 8. Pera P, Bassi F, Schierano G, Appendino P, Preti G. Implant anchored complete mandibular denture: evaluation of masticatory efficiency, oral function and degree of satisfaction. J Oral Rehabil. 1998;25(6):462‐467. [DOI] [PubMed] [Google Scholar]
- 9. Kapur KK, Garrett NR, Hamada MO, et al. Randomized clinical trial comparing the efficacy of mandibular implant‐supported overdentures and conventional dentures in diabetic patients. Part III: Comparisons of patient satisfaction. J Prosthet Dent. 1999;82(4):416‐427. [DOI] [PubMed] [Google Scholar]
- 10. Van Der Bilt A, Burgers M, Van Kampen FMC, Cune MS. Mandibular implant‐supported overdentures and oral function. Clin Oral Implants Res. 2010;21(11):1209‐1213. [DOI] [PubMed] [Google Scholar]
- 11. Bakke M, Holm B, Gotfredsen K. Masticatory function and patient satisfaction with implant‐supported mandibular overdentures: a prospective 5‐year study. Int J Prosthodont. 2002;15(6):575‐581. [PubMed] [Google Scholar]
- 12. Fontijn‐Tekamp FA, Slagter AP, van der Bilt A, et al. Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res. 2000;79(7):1519‐1524. [DOI] [PubMed] [Google Scholar]
- 13. Müller F, Duvernay E, Loup A, Vazquez L, FR H, Schimmel M. Implant‐supported mandibular overdentures in very old adults: a randomized controlled trial. J Dent Res. 2013;92(suppl 12):154S‐160S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Manly RS, Braley LC. Masticatory performance and efficiency. J Dent Res. 1950;29(4):448‐462. [DOI] [PubMed] [Google Scholar]
- 15. Lucas PW, Luke DA. Methods for analysing the breakdown of food in human mastication. Arch Oral Biol. 1983;28(9):813‐819. [DOI] [PubMed] [Google Scholar]
- 16. Edlund J, Lamm CJ. Masticatory efficiency. J Oral Rehabil. 1980;7(2):123‐130. [DOI] [PubMed] [Google Scholar]
- 17. Olthoff LW, Van Der Bilt A, Bosman F, Kleizen HH. Distribution of particle sizes in food comminuted by human mastication. Arch Oral Biol. 1984;29(11):899‐903. [DOI] [PubMed] [Google Scholar]
- 18. Slagter AP, Olthoff LW, Steen WHA, Bosman F. Comminution of food by complete‐denture wearers. J Dent Res. 1992;71(2):380‐386. [DOI] [PubMed] [Google Scholar]
- 19. Slagter AP, Bosman F, Bilt A. Comminution of two artificial test food by dentate and endentulous subjects. J Oral Rehabil. 1993;20:159‐176. [DOI] [PubMed] [Google Scholar]
- 20. Benzing U, Weber H, Simonis a, Engel E. Changes in chewing patterns after implantation in the edentulous mandible. Int J Oral Maxillofac Implants. 1997;9(2):207‐213. [PubMed] [Google Scholar]
- 21. Khoo HD, Chai J, Chow TW. Prosthetic outcome, patient complaints, and nutritional effects on elderly patients with magnet‐retained, implant‐supported overdentures–a 1‐year report. Int J Oral Maxillofac Implants. 2013;28(5):1278‐1285. [DOI] [PubMed] [Google Scholar]
- 22. Speksnijder CM, Abbink JH, Van Der Glas HW, Janssen NG, Van Der Bilt A. Mixing ability test compared with a comminution test in persons with normal and compromised masticatory performance. Eur J Oral Sci. 2009;117(5):580‐586. [DOI] [PubMed] [Google Scholar]
- 23. Dolder E. Bar‐joint prosthesis of mandibula. Schweiz Monatsschr Zahnheilkd. 1953;63(4):339‐376. [PubMed] [Google Scholar]
- 24. Dolder E. Prosthesis with anchorage bar. Rev Fr Odontostomatol. 1967;14(10):1658‐1668. [PubMed] [Google Scholar]
- 25. Dolder E. The prosthesis with a bar. Odontoiatr Prat. 1970;5(4):291‐297. [PubMed] [Google Scholar]
- 26. Slot W, Raghoebar GM, Van Dijk G, Meijer HJA. Attachment of clips in a bar‐retained maxillary implant overdenture: a clinical report. J Prosthet Dent. 2012;107(6):353‐357. [DOI] [PubMed] [Google Scholar]
- 27. van der Bilt A, Speksnijder CM, de Liz Pocztaruk R, Abbink JH. Digital image processing versus visual assessment of chewed two‐colour wax in mixing ability tests. J Oral Rehabil. 2012;39(1):11‐17. [DOI] [PubMed] [Google Scholar]
- 28. Stellingsma K, Slagter AP, Stegenga B, Raghoebar GM, Meijer HJA. Masticatory function in patients with an extremely resorbed mandible restored with mandibular implant‐retained overdentures: comparison of three types of treatment protocols. J Oral Rehabil. 2005;32(6):403‐410. [DOI] [PubMed] [Google Scholar]
- 29. Slot W, Raghoebar GM, Vissink A, Meijer HJA. A comparison between 4 and 6 implants in the maxillary posterior region to support an overdenture; 1‐year results from a randomized controlled trial. Clin Oral Implants Res. 2014;25(5):560‐566. [DOI] [PubMed] [Google Scholar]
- 30. Guljé F, Raghoebar GM, Ter Meulen J‐WP, Vissink A, Meijer HJA. Mandibular overdentures supported by 6‐mm dental implants: a 1‐year prospective cohort study. Clin Implant Dent Relat Res. 2012;14(s1):e59‐e66. [DOI] [PubMed] [Google Scholar]
- 31. de Albuquerque Júnior RF, Lund JP, Tang L, et al. Within‐subject comparison of maxillary long‐bar implant‐retained prostheses with and without palatal coverage: patient‐based outcomes. Clin Oral Implants Res. 2000;11(6):555‐565. [DOI] [PubMed] [Google Scholar]
- 32. Elsyad MA, Hegazy SAF, Hammouda NI, Al‐Tonbary GY, Habib AA. Chewing efficiency and electromyographic activity of masseter muscle with three designs of implant‐supported mandibular overdentures. A cross‐over study. Clin Oral Implants Res. 2014;25(6):742‐748. [DOI] [PubMed] [Google Scholar]
- 33. Timmerman R, Stoker GT, Wismeijer D, Oosterveld P, Vermeeren JIJF, van Waas MAJ. An eight‐year follow‐up to a randomized clinical trial of participant satisfaction with three types of mandibular implant‐retained overdentures. J Dent Res. 2004;83(8):630‐633. [DOI] [PubMed] [Google Scholar]
- 34. Cardoso RG, de Melo LA, Barbosa GAS, et al. Impact of mandibular conventional denture and overdenture on quality of life and masticatory efficiency. Braz Oral Res. 2016;30(1):1‐7. [DOI] [PubMed] [Google Scholar]
- 35. Van Der Bilt A, Mojet J, Tekamp FA, Abbink JH. Comparing masticatory performance and mixing ability. J Oral Rehabil. 2010;37(2):79‐84. [DOI] [PubMed] [Google Scholar]
- 36. Fontijn‐Tekamp FA, Slagter AP, van't Hof MA, Kalk W, Jansen JA. Pain and instability during biting with mandibular implant‐retained overdentures. Clin Oral Implants Res. 2001;12(1):46‐51. [DOI] [PubMed] [Google Scholar]
- 37. Schimmel M, Voegeli G, Duvernay E, Leemann B, Müller F. Oral tactile sensitivity and masticatory performance are impaired in stroke patients. J Oral Rehabil. 2017;44(3):163‐171. [DOI] [PubMed] [Google Scholar]
- 38. Ikebe K, Matsuda KI, Kagawa R, et al. Association of masticatory performance with age, gender, number of teeth, occlusal force and salivary flow in Japanese older adults: is ageing a risk factor for masticatory dysfunction? Arch Oral Biol. 2011;56(10):991‐996. [DOI] [PubMed] [Google Scholar]
- 39. Sugiura T, Fueki K, Igarashi Y. Comparisons between a mixing ability test and masticatory performance tests using a brittle or an elastic test food. J Oral Rehabil. 2009;36(3):159‐167. [DOI] [PubMed] [Google Scholar]
- 40. Slade GD. Derivation and validation of a short‐form oral health impact profile. Community Dent Oral Epidemiol. 1997;25(4):284‐290. [DOI] [PubMed] [Google Scholar]


