Abstract
Background: Epithelial cytokines, including IL-33 and Thymic stromal lymphopoietin (TSLP), have attracted interest because of their roles in chronic allergic inflammation-related conditions such as asthma. Mast cells are one of the major targets of IL-33, to which they respond by secreting cytokines. Most studies performed thus far have investigated the acute effects of IL-33 on mast cells. In the current study, we investigated how acute vs. prolonged exposure of mast cells to IL-33 and TSLP affects mediator synthesis and IgE-mediated activation.
Methods: Human lung mast cells (HLMCs), cord blood-derived mast cells (CBMCs), and the ROSA mast cell line were used for this study. Receptor expression and the levels of mediators were measured after treatment with IL-33 and/or TSLP.
Results: IL-33 induced the release of cytokines. Prolonged exposure to IL-33 increased while TSLP reduced intracellular levels of tryptase. Acute IL-33 treatment strongly potentiated IgE-mediated activation. In contrast, 4 days of exposure to IL-33 decreased IgE-mediated activation, an effect that was accompanied by a reduction in FcεRI expression.
Conclusion: We show that IL-33 plays dual roles in mast cells, in which its acute effects include cytokine release and the potentiation of IgE-mediated degranulation, whereas prolonged exposure to IL-33 reduces IgE-mediated activation. We conclude that mast cells act quickly in response to the alarmin IL-33 to initiate an acute inflammatory response, whereas extended exposure to IL-33 during prolonged inflammation reduces IgE-mediated responses. This negative feedback effect suggests the presence of a novel regulatory pathway that modulates IgE-mediated human mast cell responses.
Keywords: FcεRI, IgE, IL-33, mast cells, TSLP
Introduction
Compelling evidence suggests that epithelial cell-derived cytokines, such as thymic stromal lymphopoietin (TSLP), and interleukin (IL) 33 (IL-33), are strongly involved in the initiation and/or perpetuation of allergy and chronic inflammatory lung diseases such as asthma (1–3). Data have accumulated over the years from extensive investigations performed in experimental models, both in vivo and in vitro, as well as from genome wide association studies (4) and clinical trials (5). Both TSLP and IL-33 are released from epithelial cells in response to pathogens, environmental pollutants and allergens, or, in the case of IL-33, as a result of cell damage. Cells that respond to TSLP and IL-33 include T-lymphocytes, type 2 innate lymphoid cells, eosinophils, neutrophils, basophils and mast cells, many of which are often associated with type 2 immune responses, such as allergies (6, 7).
Mast cells are normally located just beneath epithelial cells, and in asthma, they are also found within the intraepithelial cell layer, and they are therefore capable of rapidly responding to TSLP and IL-33 released from epithelial cells (8). In contrast to allergen-induced cross-linkage of the IgE receptor, neither TSLP nor IL-33 causes acute mast cell exocytosis, i.e., the release of histamine, proteases, and other mediators stored in the granules. Instead, Th2 cytokines are prominently induced in response to TSLP and IL-33 (9–11). Interestingly, IL-33 is the sole alarmin that is released from damaged cells that can immediately activate mast cells to induce an inflammatory response and recruit granulocytes (12, 13). Whether mast cells also synthesize lipid mediators, such as prostaglandins and leukotrienes, in response to TSLP and IL-33 is less clear and might depend on species differences and/or the type of mast cell (10–12, 14–17). Although it does not induce mast cell degranulation on its own, IL-33 increases the synthesis and therefore the amount of pre-stored granule mediators (18, 19) and augments IgE-mediated mast cell activation (15, 20, 21), and it can therefore potentially aggravate an allergic reaction.
Most of the pioneering experimental studies that have analyzed the effects of TSLP and IL-33 on mast cell degranulation and cytokine production have explored the acute treatment of mast cells, i.e., a timescale of minutes to a few hours (22). Those results can probably be accurately transferred to an acute inflammatory situation in which mast cells should respond to “danger,” such as trauma. However, during prolonged chronic inflammation, such as asthma, the expression of IL-33 is increased in both epithelial cells and airway smooth muscle cells (23, 24), two compartments of the asthmatic lung that are associated with increased mast cell numbers (25–27). We therefore asked how human mast cell functions are affected by acute and prolonged exposure to IL-33 and/or TSLP. The expression profiles of receptors for IL-33 and TSLP were analyzed in human lung mast cells (HLMCs), primary developed mast cells, and mast cell lines. The effects of acute or prolonged exposure to IL-33 and/or TSLP on mediators, receptors, and IgE-mediated activation were analyzed. Our results reveal that IL-33 increases the FcεRI-mediated response when cells are concomitantly exposed to IL-33 and an antigen, whereas prolonged exposure to IL-33 inhibits FcεRI expression and thereby diminishes IgE-mediated mast cell degranulation. IL-33 may therefore play a significant role in the regulation of mast cell reactivity in IgE-associated chronic inflammation.
Methods
Cell Culture and in vitro Stimulations
The human mast cell line ROSAWT KIT (28) was cultured in IMDM supplemented with 10% fetal calf serum, 2 mM L-glutamine, 100 μg/mL streptomycin, 100 IU/mL penicillin, and 80 ng/mL murine stem cell factor (SCF). Cord blood -derived mast cells (CBMCs) were cultured as previously described (29). Single cell suspensions obtained from human lung tissue, for the analysis of HLMCs, were obtained as previously described (30) and maintained in RPMI 1640 medium (Sigma Aldrich) supplemented with 10% fetal calf serum, 100 ng/ml hSCF, 0.01 M HEPES, 0.5x non-essential amino acids, 2 mM L-glutamine, 100 units/ml penicillin, 0.1 mg/ml streptomycin, and 48 μM β-mercaptoethanol (Sigma Aldrich). The access to human lung tissue and number of cells obtained was limited therefore these cells were only used for selected experiments, primary CBMC and in some cases the cell-line ROSA cells was used as substitutes. Cells were stimulated with 10 ng/ml TSLP and/or 10 ng/ml IL-33 (Peprotech, Rocky Hill, NJ, USA). The cytokine concentration was chosen based on published data (10, 11, 17). The acute response was analyzed after either 1 h (degranulation and lipid mediator response that occur within 15 min after mast cell activation) or 24 h (cytokine release that occurs later after transcription, translation and secretion) of stimulation and the prolonged response after 4 days with daily addition of the cytokines without media change. To measure the levels of FcεRI receptor (in ROSA cells and CBMCs) and the amount of degranulation induced by FcεRI crosslinking (CBMCs), 10 ng/ml IL-4 (Peprotech) was added 4 days prior (unless otherwise stated) and 1 μg/ml human IgE (Calbiochem, Minneapolis, MN, USA) was added 1 day prior to crosslinking [plasma concentration of IgE in healthy individual is <1 μg/ml, in atopic individuals this is elevated and a plasma concentration above 0.5 μg/ml is predictive of allergy (31)]. After removal of unbound IgE by washing, cells were cross-linked with various concentrations of anti-IgE antibody (Sigma), and calcium ionophore A23187 (2 μM, Sigma) was used as a positive control for activation. In some experiments (indicated in the figure legends) performed to measure lipid mediators, the cells were pretreated with 10 ng/ml IL-4 and 5 ng/ml IL-3 for 4 days.
Measurement of Mediator Release
Released histamine was measured using a histamine release test kit according to the manufacturer's instructions (RefLab, Copenhagen, Denmark). Briefly, this test is based on the adsorption of histamine to glass fiber-coated microtiter plates. The glass fibers bind histamine with high affinity and selectivity. The plates were sent to RefLab, and histamine was detected fluorometrically (OPA-method) by HISTAREADER™ 501-1. PGD2 was measured using a Prostaglandin D2-MOX ELISA kit (Caymen Chemical, Ann Arbor, MI. USA), and the levels of IL-1β, IL-5, MCP-1, MIP-1α, GM-CSF, and TNF were analyzed with Luminex (BioRad, Hercules, CA, USA).
Flow Cytometry
The following antibodies were used: ST2-FITC (clone B4E6, MD Bioproducts, Zürich, Switzerland), IL7R-PE (clone A019D5, Biolegend, San Diego, CA, USA), TSLP-R-PE (clone 1B4, Biolegend), FcεRIα-PE (clone AER-37 (CRA-1), Biolegend), CD63-Pe-Cy7 (Clone H5C6, BD Biosciences, San Jose, CA, USA), tryptase (clone G3, Millipore, Burlington, MA, USA) conjugated in-house with an Alexa Fluor 647 Monoclonal antibody labeling kit (Invitrogen), chymase (clone B7, Millipore) conjugated in-house with a PE Conjugation Kit (Abcam, Cambridge, UK) or CPA3 (clone CA5, a kind gift from Andrew Walls, Southampton, UK) conjugated in-house with an Alexa Fluor™ 488 Antibody Labeling Kit (Thermo Fisher Scientific, Waltham, MA, USA). Human lung cells were stained with BD Horizon™ Fixable Viability Stain 450 (BD Biosciences) and CD45-V500 (Clone HI30, BD Biosciences), CD14- APC-Cy7 (Clone M5E2, Biolegend), and CD117-APC (clone 104D2, BD Biosciences) antibodies; and mast cells were gated as live, CD45+, CD14low CD117high. For intracellular staining, cells were fixed with 4% PFA and permeabilized using PBS-S buffer (0.1% saponin in PBS with 0.01 M HEPES). Unspecific binding was blocked using blocking buffer (PBS-S with 5% dry milk and 2% FCS). The cells were analyzed using a BD FACSCanto system (BD, Franklin Lakes, NJ, USA), and FlowJo software (FlowJo LLC, Ashland, OR, USA) was used for flow cytometry data analysis.
Quantitative PCR
RNA was extracted using an RNeasy Plus Mini Kit (Qiagen, Hilden, Germany), cDNA was prepared using an iScript cDNA synthesis kit (Bio-Rad), and qPCR was performed using iTaq Universal SYBR Green Supermix (Biorad) on a CFX96 Real-time system (Biorad). The following primers were used: GAPDH (5′- CCACATCGCTCAGACACCAT-3′ and 5′-GGCAACAATATCCACTTTACCAGAG-3′), FcεRIα (5′-CGCGTGAGAAGTACTGGCTA-3′ and 5′-TGTGACCTGCTGCTGAGTTG-3′), FcεRIβ (5′-TGCAGTAAGAGGAAATCCACCA-3′ and 5′-TGTGTTACCCCCAGGAACTC-3′), and FcεRIγ (5′-CCAGCAGTGGTCTTGCTCTT-3′ and 5′-AGGCCCGTGTAAACACCATC-3′). The results were calculated using the ΔΔCT method, and CT values were normalized to the housekeeping gene GAPDH and related to the unstimulated control.
Statistical Analysis
Data are shown as the mean ± the standard error of the mean (SEM). Statistical analyses were performed with GraphPad Prism software version 7.0b. D'Agostino and Pearson normality test or when n was smaller than eight Shapiro-Wilk normality test was performed. For normally distributed data Student's t-test was performed when comparing two groups, and when more than two groups were compared, one- or two-way ANOVA with Bonferroni's post hoc test was performed. For data that did not pass the normality test, Mann-Whitney or Wilcoxon test (paired data) was performed when comparing two groups, and when comparing more than two groups Kruskal-Wallis with Dunn's multiple comparisons test was performed (*, P < 0.05; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001).
Results
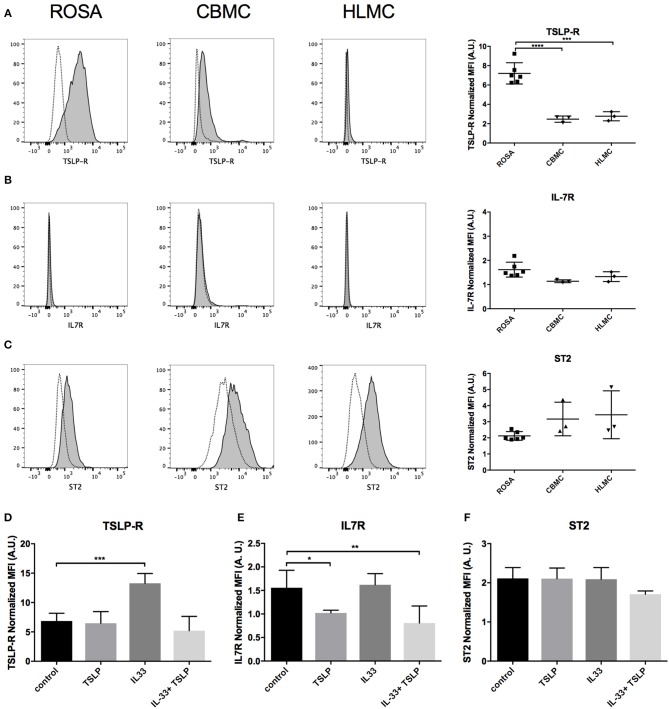
Expression of Receptors for IL-33 and TSLP on Mast Cells
The surface expression levels of different receptors for IL-33 (ST2) and TSLP (TSLP-R and IL7R) were analyzed in mast cell line ROSA and primary CBMCs and HLMCs by flow cytometry. The surface expression level of TSLP-R was higher in ROSA cells than in the primary CBMCs and HLMCs (Figure 1A). IL7R staining was very low in all cells analyzed (Figure 1B) but all cells had detectable levels of the IL-33 receptor ST2 (Figure 1C). When the mast cells were treated for 4 days with IL-33, the surface expression level of TSLP-R increased, and this effect was counteracted by TSLP, possibly via the internalization of the receptor (Figure 1D). The addition of TSLP also reduced surface staining for IL7R (Figure 1E). To confirm that TSLP induced the internalization of the receptor we also stained fixed and permeabilized cells, staining both surface, and intracellular TSLP-R and in this case the TSLP-R was equally induced in the IL-33 and the IL-33 plus TSLP group (Supplementary Figure 1). None of the cytokines had any significant effect on ST2 receptor expression (Figure 1F).
Figure 1.
Expression of receptors for IL-33 (ST2) and TSLP (TSLP-R/IL7R) on various human mast cells. Surface expression of TSLP-R (A), IL7R (B), and ST2 (C) on ROSA (A–F), CBMC (A–C), and HLMCs (A–C) was measured by flow cytometry. Representative histograms in which dotted lines represent the respective isotype controls are shown for different cell lines to the left, and quantification of the data is shown to the right (A–C). Mast cells were treated with 10 ng/ml IL-33, TSLP or a combination or both repeatedly for 4 days; thereafter, surface expression of TSLP-R (D), IL7R (E), and ST2 (F) was measured by flow cytometry. The median fluorescent intensity (MFI) of the receptors was normalized to the respective isotype control. Data shown were pooled from three independent experiments, n = 3–6.
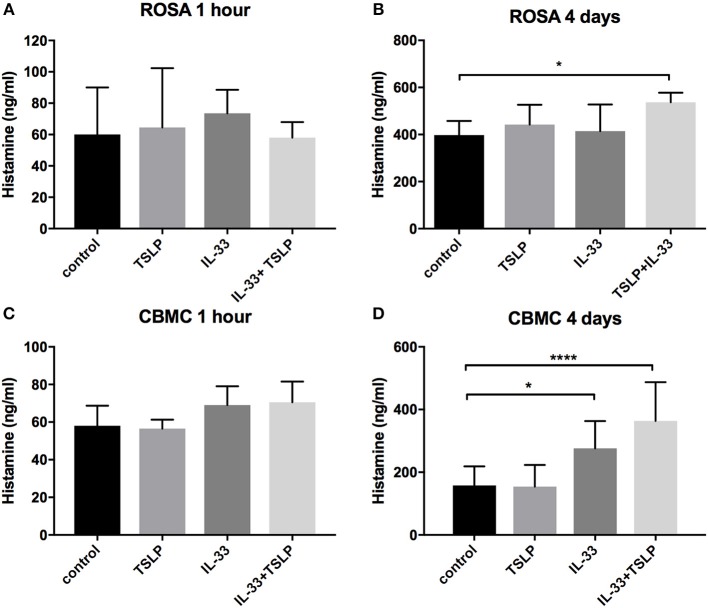
Degranulation After Prolonged Exposure to IL-33 and TSLP
It has been reported that neither IL-33 nor TSLP causes mast cell degranulation (9–11, 20, 32), and our results confirm this finding because no histamine was released after 1 h of stimulation (Figures 2A,C); however, after 4 days of stimulation, IL-33 caused a small but significant increase in the release of histamine in CBMCs (Figure 2D), and the combined addition of IL-33 and TSLP induced histamine release in ROSA cells (Figure 2B).
Figure 2.
Histamine release induced by prolonged exposure to IL-33. ROSA cells (A,B) or CBMCs (C,D) were treated with 10 ng/ml IL-33, TSLP or a combination of both for 1 h (A,C) or treated repeatedly (every day) for 4 days (B,D). Thereafter, supernatants were collected, and histamine was measured. Data shown were pooled from 3 to 5 independent experiments, n = 6–10.
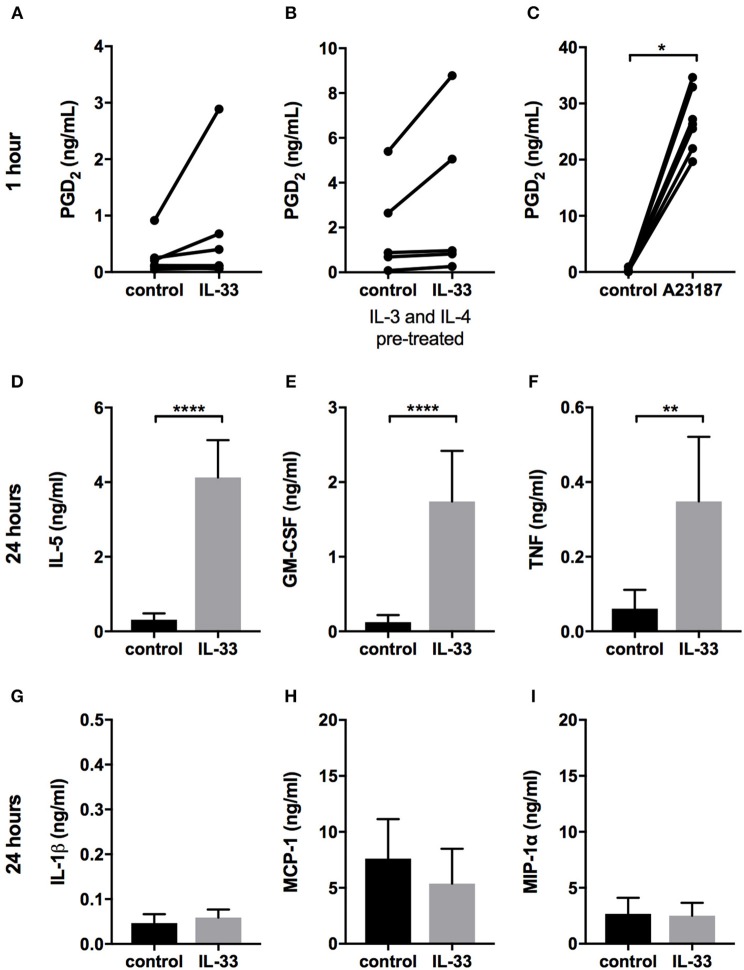
Prostaglandin D2 and Cytokine Release Induced by IL-33
The results of reports regarding whether IL-33 induces the release of lipid mediators in mast cells have been inconsistent (10, 12, 14–17). We observed considerable variation in the basal levels of PGD2 released from different CBMC cultures: in some, there appeared to be an increase following IL-33 stimulation, whereas there was no change in others. Collectively, our results indicated there was no significant increase overall (Figure 3A). Pretreating the cells with IL-4 and IL-3 for 4 days increased the amount of PGD2 released but did not increase the number of CBMC cultures that responded to IL-33 (Figure 3B). Increasing the IL-33 concentration from 10 to 100 ng/ml did not increase the number of CBMC cultures that responded either (data not shown). TSLP did not induce any PGD2 release (data not shown). All cultures treated with calcium ionophore A23187 (used as a positive control) exhibited a substantial increase in the amount of PGD2 released following this treatment (Figure 3C). There was no detectable release of cysteine leukotrienes in response to IL-33 or TSLP (data not shown). Mast cells can store some cytokines in their granules and release them directly upon degranulation, but activation can also induce de-novo synthesis of cytokines (33). Since we did not detect any degranulation by IL-33 (Figures 2A,C) we measured cytokine release after 24 h to detect de-novo synthesized cytokines. IL-33 caused a significant increase in the cytokines IL-5, GM-CSF and TNF (Figures 3D–F) but did not affect the amount of IL-1β, MCP-1 (CCL2), and MIP-1α (CCL3) released (Figures 3G–I).
Figure 3.
Prostaglandin D2 and cytokine release in response to IL-33. CBMCs were treated for 1 h (A–C) or 24 h (D–I) with 10 ng/ml IL-33 or 2 μM A23187, and supernatants were collected. PGD2 (A–C) was measured using ELISA, and cytokines were measured using Luminex assays (D–I). The CBMCs shown in (B) were pretreated with 10 ng/ml IL-4 and 5 ng/ml IL-3 for 4 days. Data shown were pooled from 5 to 9 independent experiments, n = 5–9.
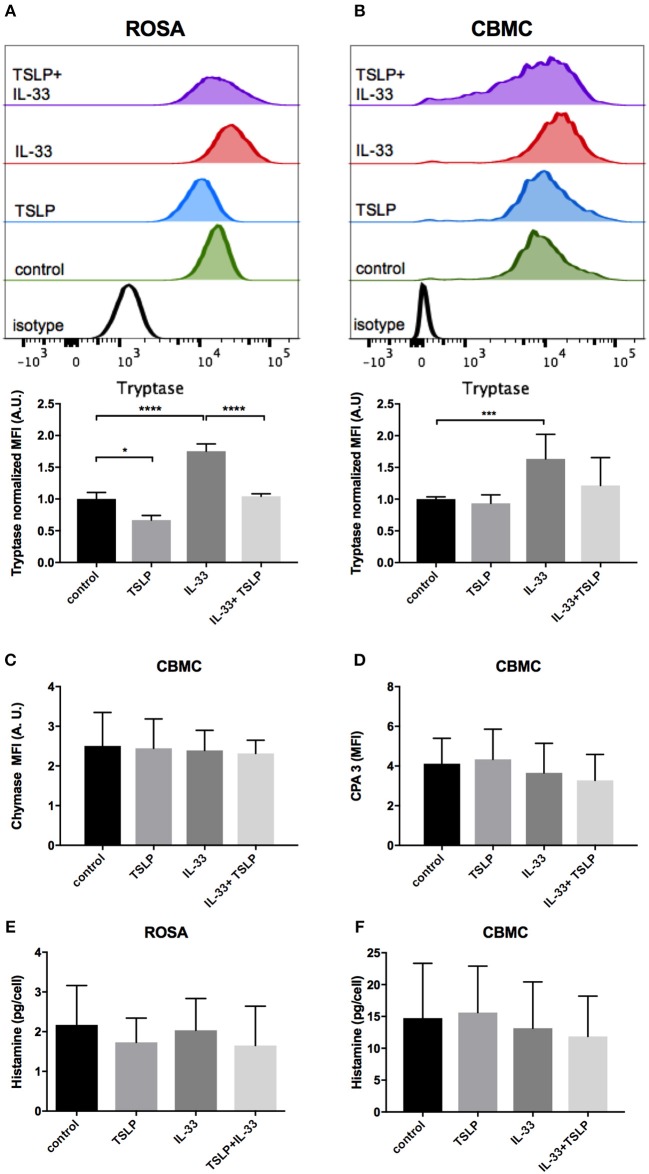
Effects on Mediator Storage by IL-33 and TSLP
Next, we investigated whether the storage of mast cell mediators would be affected by 4 days of exposure to IL-33 and TSLP. Intracellular tryptase was increased by IL-33 but decreased by TSLP in ROSA cells (Figure 4A). IL-33 also increased tryptase storage in CBMCs, while TSLP alone had no effect in these mast cells (Figure 4B). Neither IL-33 nor TSLP had any effect on the intracellular storage of the mast cell proteases chymase and CPA3 in CBMCs (Figures 4C,D). Chymase was not detectable and CPA3 was very low in ROSA cells, and the addition of IL-33 and/or TLSP did not affect the levels (data not shown). Nor did IL-33 and/or TLSP affect the storage of intracellular histamine (Figures 4E,F).
Figure 4.
Changes in mediator storage after 4 days of treatment with IL-33 and TSLP. ROSA cells (A,E) or CBMCs (B–D,F) were repeatedly treated every day for 4 days with 10 ng/ml IL-33, TSLP or a combination of both; thereafter, the levels of the proteases tryptase (A,B), chymase (C), and CPA3 (D) were measured by intracellular flow cytometry staining, and total histamine content (E,F) was measured by a histamine release test kit. The MFI of protease expression was normalized to the respective isotype control. (A) a representative of three independent experiments, n = 3. Data shown were pooled from 5 (B), 2 (C,D), 3 (E), and 6 (F) independent experiments, n = 4–12.
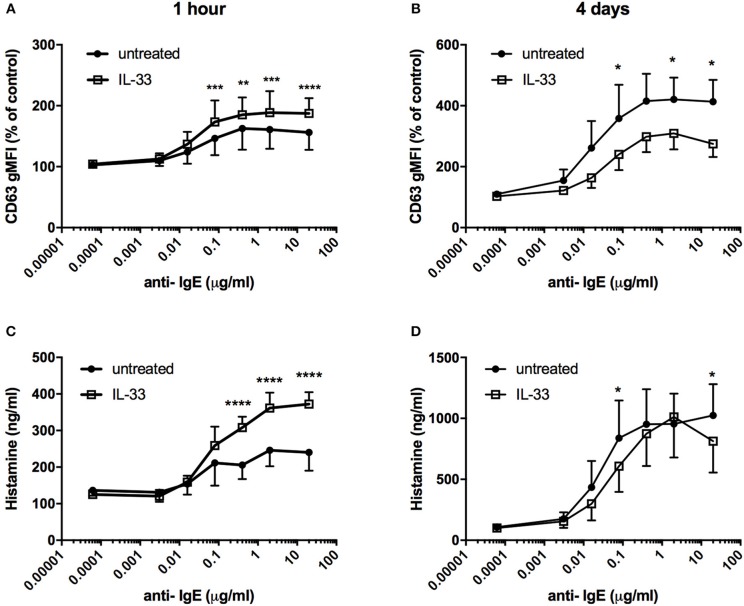
Effects on IgE-Mediated Degranulation by IL-33
It has previously been demonstrated that IL-33 potentiates IgE-mediated degranulation (15, 19–21). Pretreatment with IL-33 for 1 h prior to FcεRI crosslinking increased both surface CD63 expression and histamine release (Figures 5A,C). In contrast, when CBMCs were repeatedly treated with IL-33 for 4 days, IgE-mediated degranulation was significantly decreased, with reduced induction of CD63 surface expression and histamine release compared to the untreated group (Figures 5B,D). Pretreatment with TSLP for 4 days had no effect on IgE-mediated degranulation (data not shown).
Figure 5.
Effect of IL-33 on mast cell degranulation by FcεRI crosslinking. CBMCs were treated with 10 ng/ml IL-33 for 1 h (A,C) or repeatedly every day for 4 days (B,D); thereafter, they were stimulated various concentrations of anti-IgE. Degranulation was measured by the detection of surface CD63 with flow cytometry (A,B) or as histamine release (C,D). Data shown were pooled from 3 independent experiments, n = 3.
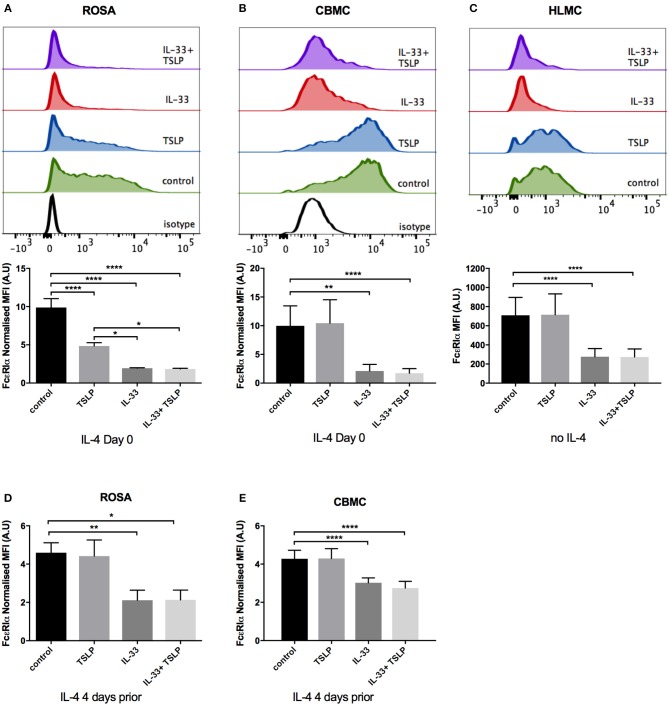
FcεRI Surface Receptor Expression Is Decreased by 4 Days of IL-33 Treatment
To further investigate a possible mechanism that could underlie the observed decrease in degranulation, we next investigated the effect of IL-33 and TSLP on surface expression of the FcεRI receptor. We found that 4 days of treatment with IL-33 caused a dramatic decrease in the surface expression of the FcεRI receptor in ROSA cells, CBMCs, and HLMCs (Figures 6A–C). In ROSA cells, TSLP also caused a significant drop in FcεRI surface staining (Figure 6A). Since human mast cells grown in culture express very low levels of FcεRI, we added IL-4 to upregulate the receptor in ROSA cells and CBMCs (Figures 6A,B). To investigate whether IL-33 reduces receptor expression simply by blocking IL-4-mediated receptor upregulation, IL-4 was added 4 days prior to a media change, and IL-33 and TSLP addition. Also, in this experiment, IL-33 downregulated the FcεRI receptor, indicating that a blockade of IL-4-mediated upregulation is not the mechanism that reduces FcεRI receptor surface expression. However, the reduction of FcεRI by TSLP was absent in this case, indicating that TSLP is blocking the IL-4 mediated upregulation (Figures 6D,E). In addition, we exposed ROSA cells to IL-33 and TSLP without the addition of IL-4 and although the receptor expression is low in this case, IL-33 caused a reduction (Supplementary Figure 2). HLMC that are extracted from human lung tissue have a natural high FcεRI expression therefore IL-4 was not added to these cells and IL-33 caused a decrease also in these cells (Figure 6C). Altogether, these data indicate that the downregulation of FcεRI by IL-33 is independent of IL-4.
Figure 6.
Decrease in FcεRI surface expression by IL-33. ROSA cells (A,D), CBMCs (B,E), or HLMCs (C) were repeatedly treated every day for 4 days with 10 ng/ml IL-33, TSLP or a combination of both. In addition, IL-4 was added on day 0 (A,B) or 4 days prior to the addition of IL-33 and TSLP (D,E) to upregulate the FcεRI receptor. IL-4 was not added to HLMCs (C). Surface FcεRIα receptor expression was measured by flow cytometry; representative histograms are shown in (A–C) and quantification of the expression is shown below. The MFI of FcεRI was normalized to that of the isotype control. Data shown were pooled from 3 to 5 independent experiments, n = 6–10.
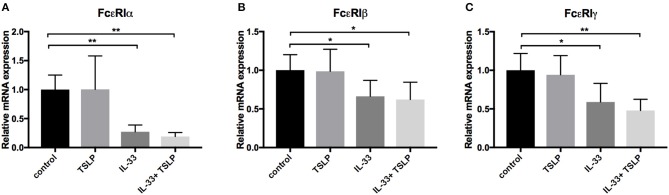
IL-33 Decreases the Expression of FcεRI
The FcεRI receptor consists of four chains, including one α-, one β- and two γ-chains, which are regulated at both the protein and mRNA levels (34). We therefore next investigated whether IL-33 affects the mRNA expression of the different subunits of this receptor. We found that 4 days of treatment with IL-33 significantly reduced the levels of all subunits, indicating that the relevant regulatory mechanism occurs at the mRNA level (Figures 7A–C).
Figure 7.
Decrease in mRNA expression of the FcεRI receptor by IL-33. CBMCs were repeatedly treated every day for 4 days with 10 ng/ml IL-33, TSLP or a combination of both. In addition, IL-4 was added on day 0. The mRNA expression level of the different subunits of the FcεRI receptor were quantified using qPCR (A–C). Expression was normalized to that of the housekeeping gene GAPDH and thereafter to the unstimulated control. Data shown were pooled from six independent experiments, n = 6.
Discussion
Compelling evidence indicates that IL-33 acts as an alarmin to activate mast cells in an acute manner, resulting in the release of pro-inflammatory mediators (22). In the present study, we demonstrate an opposite effect of IL-33 by which prolonged exposure to IL-33, down-regulates the high-affinity IgE receptor and reduces the allergic response (Figures 5, 6). Thus, IL-33 appears to have divergent functions on mast cells, including an acute effect by which it induces the release of cytokines (Figure 3) and consequentially acute inflammation and a dampening effect observed in cells exposed to IL-33 for a longer period, such as during chronic inflammation (2).
We also investigated the surface expression of receptors for IL-33 and TSLP, including ST2, TSLP-R and IL7R, in the mast cell line ROSA as well as primary CBMCs and HLMCs. Similar to previously published reports, we found that all of these cells expressed the ST2 receptor (Figure 1C) (10, 11, 14, 35); however, contrary to Kaur et al. (35), we did not observe any increase in the surface expression of ST2 after IL-33 treatment (Figure 1F), possibly because we exposed the cells to IL-33 for different periods of time (24 h vs. 4 days). TSLP-R surface staining was stronger in the mast cell lines than in primary mast cells (Figure 1A), and the ROSA mast cells were the only cells that responded to TSLP, with no response observed in the primary cells (Figures 4A,B, 6A–E). However, exposure to IL-33 upregulated TSLP-R surface expression (Figure 1D), and in some cases, we also observed that TSLP affected primary cells when added in combination with IL-33 (Figure 2D), possibly because of the upregulation of its receptor. IL7R surface staining was very low in all cells, but when cells were treated with TSLP, it was even lower, suggesting that although it is expressed at very low levels, it is still functional and internalized upon ligand binding (Figure 1E).
Several studies have previously demonstrated that IL-33 induces the release of cytokines from mast cells (10–12, 14, 15, 20, 21, 32, 36). Studies have also shown that IL-33 induces the release of lipid mediators (12, 14, 16, 17), while other studies have reported no lipid mediator release in response to IL-33 (10, 11, 15). We also observed that IL-33 induced the release of cytokines (Figures 3D–I); however, there was high donor to donor variation in PGD2 release, resulting in no significant change overall (Figures 3A,B). The reason for this variation between donors remains unresolved, and further studies are needed to determine why some patients do not release PGD2 in response to IL-33.
IL-33 has been proposed to be important for the maturation of mast cells because it increases storage of the mast cell proteases tryptase and CPA3 as well as the amine serotonin (10, 16, 18, 19). In our experiments, 4 days of exposure to IL-33 also increased, whereas TSLP decreased, the intracellular level of tryptase. These findings are in contrast to the results presented by Lai et al. who found that storage of tryptase was increased by TSLP (16). This difference could be because we used mature CBMCs (more than 8 weeks in culture), while they added TSLP when the cultures of cord blood cells were begun in order to develop them into mast cells. They also cultured the cells in the presence of TSLP for 3 weeks, while we did so for only 4 days. Interestingly, this was the only experiment in our study in which IL-33 and TSLP exerted opposing effects. We did not observe any change in chymase and CPA3 expression after 4 days of stimulation, in agreement with the results presented in Lai et al. (16). However, they reported that CPA3 expression was increased after 3 weeks of treatment. Human mast cells do not contain as much serotonin as is contained in mouse mast cells, but they store more histamine (37). We therefore investigated whether the storage of histamine was affected by IL-33 and TSLP, but we observed no change after 4 days of treatment (Figures 4E,F).
Previous studies have shown that neither IL-33 nor TSLP alone induces acute mast cell degranulation (21, 38, 39), and this finding was also confirmed in this study (Figures 2A,C). However, 4 days of exposure to IL-33 induced partial exocytosis and histamine release (Figures 2B,D). Similar to previous studies (21, 39), we found that 1 h of pretreatment with IL-33 strongly potentiated the mast cell degranulation induced by crosslinkage of the IgE- receptor (Figures 5A,C). In contrast, 4 days of exposure to IL-33 had the opposite effect, with the treated cells exhibiting less degranulation than was observed in the untreated group (Figures 5B,D). Jung et al. also showed that prolonged exposure to IL-33 induced a hyporesponsive phenotype in mast cells. They investigated the cause of this hyporesponsiveness in mouse mast cells and observed that while there was no difference in FcεRI receptor expression, but Hck expression was decreased (40). We did not observe any change in Hck expression (data not shown) in human mast cells, but FcεRI surface receptor expression dropped dramatically in both human ROSA cells and primary CBMCs as well as in primary mast cells isolated from human lungs (Figures 6A–C). FcεRI expression can be regulated at both the mRNA and protein level (34); IL-33 mediated the downregulation of FcεRI by decreasing the mRNA expression levels of the different subunits (Figures 7A–C). Since IL-33 activates mast cells to release various cytokines it is not clear if the observed long-term effect of IL-33 is a direct effect or if it is a secondary consequence of the mediators that are released by IL-33 activation. This warrants further investigation to clarify.
Mast cells are very potent pro-inflammatory cells, and the systemic activation of mast cells can lead to anaphylaxis and potentially death. Mast cell activation must therefore be tightly regulated (41). IL-33 is a potent pro-inflammatory cytokine, and it is clear that acute exposure to IL-33 activates mast cells and increases their responsiveness to antigens. This is a potentially dangerous situation, and we therefore suggest that after prolonged exposure to IL-33, mast cells down-regulate the FcεRI receptor in a negative feedback loop to prevent damage caused by excessive mast cell activation.
Ethics Statement
The local ethics committee approved the experiments involving human subjects, i.e., the collection of lung tissue from patients undergoing lobectomies, and all patients provided informed consent. In accordance with Swedish legislation, ethics approval was not needed for the anonymous collection of cord blood because the samples cannot be traced to a specific person.
Author Contributions
ER involved in conception and designed of study, performed experiments, analyzed data, and wrote manuscript. GN involved in conception and design of study and wrote manuscript. AG, CC, MatE, and MarE planned and performed experiments. JS provided clinical samples. MA provided reagents. All authors contributed to manuscript writing.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This manuscript has been released as a Pre-Print at bioRxiv (42). We thank SOBI, Stockholm, Sweden, for generously gifting SCF and Andrew Walls for generously gifting the CPA3 antibody. This study was supported by grants from the Swedish Research Council; the Heart-Lung Foundation; the Ollie and Elof Ericssons foundation; the Ellen, Walter and Lennart Hesselman's foundation; Tore Nilssons Foundation; the Lars Hiertas memory fund; the Konsul Th C Berghs Foundation; the Tornspiran Foundation; the O. E. and Edla Johanssons Foundation; the Swedish Society for Medical Research; The ChAMP (Centre for Allergy Research Highlights Asthma Markers of Phenotype) consortium funded by the Swedish Foundation for Strategic Research; the AstraZeneca and Science for Life Laboratory Joint Research Collaboration; and the Karolinska Institutet.
ChAMP collaborators: Ann-Charlotte Orre, Mamdoh Al-Ameri, Mikael Adner, and Sven-Erik Dahlén.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2019.01361/full#supplementary-material
References
- 1.Ohno T, Morita H, Arae K, Matsumoto K, Nakae S. Interleukin-33 in allergy. Allergy. (2012) 67:1203–14. 10.1111/all.12004 [DOI] [PubMed] [Google Scholar]
- 2.Makrinioti H, Toussaint M, Jackson DJ, Walton RP, Johnston SL. Role of interleukin 33 in respiratory allergy and asthma. Lancet Respir Med. (2014) 2:226–37. 10.1016/S2213-2600(13)70261-3 [DOI] [PubMed] [Google Scholar]
- 3.Mitchell PD, O'byrne PM. Epithelial-derived cytokines in asthma. Chest. (2017) 151:1338–44. 10.1016/j.chest.2016.10.042 [DOI] [PubMed] [Google Scholar]
- 4.Vicente CT, Revez JA, Ferreira MAR. Lessons from ten years of genome-wide association studies of asthma. Clin Transl Immunol. (2017) 6:e165. 10.1038/cti.2017.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corren J, Parnes JR, Wang L, Mo M, Roseti SL, Griffiths JM, et al. Tezepelumab in adults with uncontrolled asthma. N Engl J Med. (2017) 377:936–46. 10.1056/NEJMoa1704064 [DOI] [PubMed] [Google Scholar]
- 6.Liew FY, Girard JP, Turnquist HR. Interleukin-33 in health and disease. Nat Rev Immunol. (2016) 16:676–89. 10.1038/nri.2016.95 [DOI] [PubMed] [Google Scholar]
- 7.Griesenauer B, Paczesny S. The ST2/IL-33 axis in immune cells during inflammatory diseases. Front Immunol. (2017) 8:475. 10.3389/fimmu.2017.00475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Erjefalt JS. Mast cells in human airways: the culprit? Eur Respir Rev. (2014) 23:299–307. 10.1183/09059180.00005014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allakhverdi Z, Comeau MR, Jessup HK, Yoon BR, Brewer A, Chartier S, et al. Thymic stromal lymphopoietin is released by human epithelial cells in response to microbes, trauma, or inflammation and potently activates mast cells. J Exp Med. (2007a) 204:253–8. 10.1084/jem.20062211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allakhverdi Z, Smith DE, Comeau MR, Delespesse G. Cutting edge: The ST2 ligand IL-33 potently activates and drives maturation of human mast cells. J Immunol. (2007b) 179:2051–4. 10.4049/jimmunol.179.4.2051 [DOI] [PubMed] [Google Scholar]
- 11.Iikura M, Suto H, Kajiwara N, Oboki K, Ohno T, Okayama Y, et al. IL-33 can promote survival, adhesion and cytokine production in human mast cells. Lab Invest. (2007) 87:971–8. 10.1038/labinvest.3700663 [DOI] [PubMed] [Google Scholar]
- 12.Enoksson M, Lyberg K, Moller-Westerberg C, Fallon PG, Nilsson G, Lunderius-Andersson C. Mast cells as sensors of cell injury through IL-33 recognition. J Immunol. (2011b) 186:2523–8. 10.4049/jimmunol.1003383 [DOI] [PubMed] [Google Scholar]
- 13.Enoksson M, Moller-Westerberg C, Wicher G, Fallon PG, Forsberg-Nilsson K, Lunderius-Andersson C, et al. Intraperitoneal influx of neutrophils in response to IL-33 is mast cell dependent. Blood. (2013) 121:530–6. 10.1182/blood-2012-05-434209 [DOI] [PubMed] [Google Scholar]
- 14.Moulin D, Donze O, Talabot-Ayer D, Mezin F, Palmer G, Gabay C. Interleukin (IL)-33 induces the release of pro-inflammatory mediators by mast cells. Cytokine. (2007) 40:216–25. 10.1016/j.cyto.2007.09.013 [DOI] [PubMed] [Google Scholar]
- 15.Silver MR, Margulis A, Wood N, Goldman SJ, Kasaian M, Chaudhary D. IL-33 synergizes with IgE-dependent and IgE-independent agents to promote mast cell and basophil activation. Inflamm Res. (2010) 59:207–18. 10.1007/s00011-009-0088-5 [DOI] [PubMed] [Google Scholar]
- 16.Lai Y, Altemeier WA, Vandree J, Piliponsky AM, Johnson B, Appel CL, et al. Increased density of intraepithelial mast cells in patients with exercise-induced bronchoconstriction regulated through epithelially derived thymic stromal lymphopoietin and IL-33. J Allergy Clin Immunol. (2014) 133:1448–55. 10.1016/j.jaci.2013.08.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buchheit KM, Cahill KN, Katz HR, Murphy KC, Feng C, Lee-Sarwar K, et al. Thymic stromal lymphopoietin controls prostaglandin D2 generation in patients with aspirin-exacerbated respiratory disease. J Allergy Clin Immunol. (2016) 137:1566–76 e1565. 10.1016/j.jaci.2015.12.777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaieda S, Shin K, Nigrovic PA, Seki K, Lee RT, Stevens RL, et al. Synovial fibroblasts promote the expression and granule accumulation of tryptase via interleukin-33 and its receptor ST-2 (IL1RL1). J Biol Chem. (2010) 285:21478–86. 10.1074/jbc.M110.114991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sjoberg LC, Gregory JA, Dahlen SE, Nilsson GP, Adner M. Interleukin-33 exacerbates allergic bronchoconstriction in the mice via activation of mast cells. Allergy. (2015) 70:514–21. 10.1111/all.12590 [DOI] [PubMed] [Google Scholar]
- 20.Andrade MV, Iwaki S, Ropert C, Gazzinelli RT, Cunha-Melo JR, Beaven MA. Amplification of cytokine production through synergistic activation of NFAT and AP-1 following stimulation of mast cells with antigen and IL-33. Eur J Immunol. (2011) 41:760–72. 10.1002/eji.201040718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joulia R, L'faqihi FE, Valitutti S, Espinosa E. IL-33 fine tunes mast cell degranulation and chemokine production at the single-cell level. J Allergy Clin Immunol. (2017) 140:497–509 e410. 10.1016/j.jaci.2016.09.049 [DOI] [PubMed] [Google Scholar]
- 22.Saluja R, Zoltowska A, Ketelaar ME, Nilsson G. IL-33 and thymic stromal lymphopoietin in mast cell functions. Eur J Pharmacol. (2016) 778:68–76. 10.1016/j.ejphar.2015.04.047 [DOI] [PubMed] [Google Scholar]
- 23.Prefontaine D, Lajoie-Kadoch S, Foley S, Audusseau S, Olivenstein R, Halayko AJ, et al. Increased expression of IL-33 in severe asthma: evidence of expression by airway smooth muscle cells. J Immunol. (2009) 183:5094–103. 10.4049/jimmunol.0802387 [DOI] [PubMed] [Google Scholar]
- 24.Prefontaine D, Nadigel J, Chouiali F, Audusseau S, Semlali A, Chakir J, et al. Increased IL-33 expression by epithelial cells in bronchial asthma. J Allergy Clin Immunol. (2010) 125:752–4. 10.1016/j.jaci.2009.12.935 [DOI] [PubMed] [Google Scholar]
- 25.Brightling CE, Bradding P, Symon FA, Holgate ST, Wardlaw AJ, Pavord ID. Mast-cell infiltration of airway smooth muscle in asthma. N Eng J Med. (2002) 346:1699–705. 10.1056/NEJMoa012705 [DOI] [PubMed] [Google Scholar]
- 26.Balzar S, Fajt ML, Comhair SA, Erzurum SC, Bleecker E, Busse WW, et al. Mast cell phenotype, location, and activation in severe asthma: data from the severe asthma research program. Am J Respir Crit Care Med. (2011) 183:299–309. 10.1164/rccm.201002-0295OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.James A, Gyllfors P, Henriksson E, Dahlén S, Adner M, Nilsson G, et al. Corticosteroid treatment selectively decreases mast cells in the smooth muscle and epithelium of asthmatic bronchi. Allergy. (2012) 67:958–61. 10.1111/j.1398-9995.2012.02836.x [DOI] [PubMed] [Google Scholar]
- 28.Saleh R, Wedeh G, Herrmann H, Bibi S, Cerny-Reiterer S, Sadovnik I, et al. A new human mast cell line expressing a functional IgE receptor converts to tumorigenic growth by KIT D816V transfection. Blood. (2014) 124:111–20. 10.1182/blood-2013-10-534685 [DOI] [PubMed] [Google Scholar]
- 29.Enoksson M, Ejendal KF, Mcalpine S, Nilsson G, Lunderius-Andersson C. Human cord blood-derived mast cells are activated by the Nod1 agonist M-TriDAP to release pro-inflammatory cytokines and chemokines. J Innate Immun. (2011a) 3:142–9. 10.1159/000321933 [DOI] [PubMed] [Google Scholar]
- 30.Ravindran A, Ronnberg E, Dahlin JS, Mazzurana L, Safholm J, Orre AC, et al. An optimized protocol for the isolation and functional analysis of human lung mast cells. Front Immunol. (2018) 9:2193. 10.3389/fimmu.2018.02193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amarasekera M. Immunoglobulin E in health and disease. Asia Pac Allergy. (2011) 1:12–5. 10.5415/apallergy.2011.1.1.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ho LH, Ohno T, Oboki K, Kajiwara N, Suto H, Iikura M, et al. IL-33 induces IL-13 production by mouse mast cells independently of IgE-FcepsilonRI signals. J Leukoc Biol. (2007) 82:1481–90. 10.1189/jlb.0407200 [DOI] [PubMed] [Google Scholar]
- 33.Zhang Y, Ramos BF, Jakschik BA. Neutrophil recruitment by tumor necrosis factor from mast cells in immune complex peritonitis. Science. (1992) 258:1957–9. 10.1126/science.1470922 [DOI] [PubMed] [Google Scholar]
- 34.Kraft S, Kinet JP. New developments in FcepsilonRI regulation, function and inhibition. Nat Rev Immunol. (2007) 7:365–78. 10.1038/nri2072 [DOI] [PubMed] [Google Scholar]
- 35.Kaur D, Gomez E, Doe C, Berair R, Woodman L, Saunders R, et al. IL-33 drives airway hyper-responsiveness through IL-13-mediated mast cell: airway smooth muscle crosstalk. Allergy. (2015) 70:556–67. 10.1111/all.12593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bandara G, Beaven MA, Olivera A, Gilfillan AM, Metcalfe DD. Activated mast cells synthesize and release soluble ST2-a decoy receptor for IL-33. Eur J Immunol. (2015) 45:3034–44. 10.1002/eji.201545501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kushnir-Sukhov NM, Brown JM, Wu Y, Kirshenbaum A, Metcalfe DD. Human mast cells are capable of serotonin synthesis and release. J Allergy Clin Immunol. (2007) 119:498–9. 10.1016/j.jaci.2006.09.003 [DOI] [PubMed] [Google Scholar]
- 38.Fux M, Pecaric-Petkovic T, Odermatt A, Hausmann OV, Lorentz A, Bischoff SC, et al. IL-33 is a mediator rather than a trigger of the acute allergic response in humans. Allergy. (2014) 69:216–22. 10.1111/all.12309 [DOI] [PubMed] [Google Scholar]
- 39.Cop N, Ebo DG, Bridts CH, Elst J, Hagendorens MM, Mertens C, et al. Influence of IL-6, IL-33, and TNF-alpha on human mast cell activation: lessons from single cell analysis by flow cytometry. Cytometry B Clin Cytom. (2017) 94:405–11. 10.1002/cyto.b.21547 [DOI] [PubMed] [Google Scholar]
- 40.Jung MY, Smrz D, Desai A, Bandara G, Ito T, Iwaki S, et al. IL-33 induces a hyporesponsive phenotype in human and mouse mast cells. J Immunol. (2013) 190:531–8. 10.4049/jimmunol.1201576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Halova I, Ronnberg E, Draberova L, Vliagoftis H, Nilsson GP, Draber P. Changing the threshold-Signals and mechanisms of mast cell priming. Immunol Rev. (2018) 282:73–86. 10.1111/imr.12625 [DOI] [PubMed] [Google Scholar]
- 42.Rönnberg E, Ghaib A, Ceriol C, Enoksson E, Arock M, Säfholm J, et al. Divergent effects of acute and prolonged interleukin 33 exposure on mast cell IgE-mediated functions. bioRxiv. (2018). 10.1101/463950 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.