Abstract
This study uses administrative claims from an insurance database to examine adoption of digital breast tomosynthesis for cancer screening and describe regional patterns and sociodemographic characteristics associated with its use.
Although digital mammography has been widely used for breast cancer screening for more than a decade, it has imperfect sensitivity and specificity. A newer technology, digital breast tomosynthesis (DBT), may have a lower recall rate and a higher cancer detection rate than 2-dimensional mammography, although most studies of DBT were retrospective and did not evaluate long-term health outcomes.1 The use of DBT has some important trade-offs compared with 2-dimensional mammography, including higher costs and higher radiation dose with some machines.2 Although the US Preventive Services Task Force and the American Cancer Society have not specifically endorsed DBT for routine breast cancer screening, citing insufficient evidence, the American College of Radiology supports its use.3,4 Our objectives were to describe adoption of DBT for breast cancer screening in a large privately insured population, characterize regional patterns of adoption, and identify regional-level characteristics associated with that adoption.
Methods
This was a longitudinal study evaluating regional changes in DBT use for breast cancer screening. Our primary data source was the Blue Cross Blue Shield (BCBS) Axis, a database of BCBS plan claims. We included women aged 40 to 74 years who underwent screening mammography between January 1, 2015, and December 31, 2017. We defined screening mammography using a validated algorithm, and we identified DBT by its Current Procedural Terminology code.5 We defined regions according to hospital referral region (HRR) boundaries. To assess generalizability of our findings to other payer populations, we compared HRR-level DBT use in the BCBS population with HRR-level use in fee-for-service Medicare beneficiaries from January 1, 2015, through December 31, 2016, using data from publicly available Medicare Provider Utilization and Payment files. For this source, we defined DBT use as the ratio of DBT screening claims to 2-dimensional screening mammography claims within an HRR. This study was not considered human subjects research because we used a previously collected, limited data set. Therefore, the study was deemed exempt from the need for institutional review board approval by the Human Investigation Committee of Yale School of Medicine in New Haven, Connecticut.
To identify regional patterns of DBT adoption over time, we used group-based trajectory modeling.6 We implemented the model with a zero-inflated Poisson distribution using the crimCV package available in R and assessed goodness of fit using the Bayesian information criterion. We also used 2015 data from the US Census Bureau’s American Community Survey and 2010 data from the US Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance Survey to evaluate baseline area-level characteristics associated with patterns of DBT adoption. Analyses were performed in Stata (version 14.0; StataCorp) and RStudio (version 0.99.896; RStudio Inc). A 2-sided P < .05 was considered statistically significant.
Results
Our study included 9 673 583 breast cancer screening examinations performed over 3 years. Overall, DBT use increased substantially from 12.9% of screening examinations in early 2015 to 43.2% in late 2017. In early 2015, DBT was the predominant mode of breast cancer screening (ie, used in >50% of screening examinations) in 4.6% of HRRs. By the end of 2017, DBT had become the predominant mode of screening in 41.8% of HRRs. We found that HRR-level use in the BCBS population was strongly correlated with HRR-level use in the Medicare population (r in 2015 = 0.85; P < .001; r in 2016 = 0.70; P < .001).
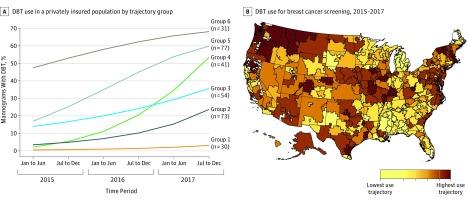
We identified 6 typical trajectories of DBT adoption (Figure, A). Mapping of the trajectories revealed clear geographic patterns. Hospital referral regions in the Southeast tended to have slower growth and lower overall rates of DBT use than HRRs in other regions; HRRs in the Northeast and Northwest tended to have more rapid growth and higher rates of use at study end (Figure, B).
Figure. Patterns of Digital Breast Tomosynthesis (DBT) Adoption.
A, Digital breast tomosynthesis use for breast cancer screening in a privately insured population by trajectory group. Hospital referral regions (HRRs) were categorized into 6 groups on the basis of similar trends in adoption of DBT identified by group-based trajectory analysis. N indicates the number of HRRs within each trajectory group. B, Digital breast tomosynthesis use by HRRs. Map shading indicates the trajectory of DBT use in each HRR, ordered according to use at the end of 2017; white areas are excluded from HRR boundaries.
Trajectory of DBT use was also associated with regional sociodemographic characteristics (Table). Digital breast tomosynthesis was adopted more quickly in areas of the country with higher median household incomes (mean [SD] was $45 254 [$8873] in group 1 and $53 835 [$11 667] in group 6; P for trend across groups, <.001) and greater educational attainment (mean [SD] percentage of population with a college education or more was 23.2% [7.1%] in group 1 and 27.5% [8.2%] in group 6; P for trend across groups, <.001). Trajectory groups with greater DBT adoption also had a larger percentage of white residents (mean [SD] percentage ranged from 70.5% [14.5%] in group 1 to 82.2% [7.8%] in group 6; P for trend across groups, .01) and smaller black populations (mean [SD] percentage ranged from 18.6% [14.5%] in group 1 to 5.3% [5.2%] in group 6; P for trend across groups, <.001).
Table. Baseline Regional Demographic Characteristics and DBT Use by Trajectory Groupa.
| Characteristic | DBT Use Trajectory Groupb | P Valuec | P Value for Test for Trendd | |||||
|---|---|---|---|---|---|---|---|---|
| 1 (n = 30 [9.8%]) | 2 (n = 73 [23.9%]) | 3 (n = 54 [17.6%]) | 4 (n = 41 [13.4%]) | 5 (n = 77 [25.2%]) | 6 (n = 31 [10.1%]) | |||
| Race/ethnicity, % | ||||||||
| White | 70.5 (14.5) | 75.8 (13.1) | 74.6 (13.4) | 80.4 (12.6) | 75.0 (13.0) | 82.2 (7.8) | .001 | .008 |
| Black | 18.6 (14.5) | 11.6 (10.7) | 9.6 (7.6) | 8.2 (10.6) | 11.5 (11.4) | 5.3 (5.2) | <.001 | <.001 |
| Other | 10.9 (11.1) | 12.6 (9.8) | 15.8 (12.5) | 11.4 (7.2) | 13.5 (7.5) | 12.5 (6.5) | .01 | .02 |
| College degree or higher, % | 23.2 (7.1) | 25.2 (7.0) | 28.7 (6.8) | 25.9 (8.0) | 29.1 (7.3) | 27.5 (8.2) | <.001 | <.001 |
| Median household income, $ | 45 254 (8873) | 49 436 (10 782) | 55 059 (11 426) | 49 796 (8728) | 57 198 (12 752) | 53 835 (11 667) | <.001 | <.001 |
| Metro, %e | 69.0 (34.0) | 80.7 (22.0) | 89.5 (12.9) | 79.7 (19.2) | 82.6 (23.1) | 76.5 (20.3) | .01 | .99 |
| Screened with mammography per HRR, median (IQR), % | 69.6 (67.7-71.9) | 69.0 (66.3-71.5) | 69.4 (65.8-72.7) | 70.7 (67.9-73.6) | 71.3 (68.0-73.9) | 69.6 (66.7-71.3) | .04 | .17 |
Abbreviations: DBT, digital breast tomosynthesis; HRR, hospital referral region; IQR, interquartile range.
All data on HRR characteristics are from the US Census Bureau’s American Community Survey, except data on population-level screening mammography use, which came from the Behavioral Risk Factor Surveillance Survey.
Numbers in the trajectory group column headings represent the number (percentage) of HRRs in each group. Data are presented as mean (SD) unless noted otherwise.
Evaluated using the Kruskal-Wallis test for group differences.
Evaluated using a nonparametric test for trend across trajectory groups.
Defined according to the US Department of Agriculture Rural-Urban Continuum Codes (https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx).
Discussion
We found that in a large privately insured population, DBT was rapidly adopted into practice and became the predominant mode of screening in more than 40% of HRRs around the country. Although our use of BCBS data limits generalizability to other payer populations, patterns of use were similar to those among Medicare beneficiaries, suggesting that our results are not completely specific to the BCBS population.
We also observed wide regional variations in patterns of DBT adoption, with more rapid uptake in areas of the country with greater socioeconomic resources, including higher income and educational attainment. Whether this variation in DBT use affects health outcomes will ultimately depend on DBT’s long-term effectiveness at reducing morbidity and mortality from breast cancer.
References
- 1.Melnikow J, Fenton JJ, Miglioretti D, Whitlock EP, Weyrich MS. Screening for Breast Cancer With Digital Breast Tomosynthesis. Rockville, MD: Agency for Healthcare Research and Quality; 2016. AHRQ publication 14-05201-EF-2. [PubMed] [Google Scholar]
- 2.Richman IB, Gross CP. New breast cancer screening technologies in older women—is it time to pump the brakes? JAMA Intern Med. 2019;179(3):289-290. doi: 10.1001/jamainternmed.2018.7767 [DOI] [PubMed] [Google Scholar]
- 3.Siu AL; US Preventive Services Task Force . Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement [published correction appears in Ann Intern Med. 2016;164(6):448]. Ann Intern Med. 2016;164(4):279-296. doi: 10.7326/M15-2886 [DOI] [PubMed] [Google Scholar]
- 4.Oeffinger KC, Fontham ET, Etzioni R, et al. ; American Cancer Society . Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599-1614. doi: 10.1001/jama.2015.12783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith-Bindman R, Quale C, Chu PW, Rosenberg R, Kerlikowske K. Can Medicare billing claims data be used to assess mammography utilization among women ages 65 and older? Med Care. 2006;44(5):463-470. doi: 10.1097/01.mlr.0000207436.07513.79 [DOI] [PubMed] [Google Scholar]
- 6.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109-138. doi: 10.1146/annurev.clinpsy.121208.131413 [DOI] [PubMed] [Google Scholar]