Abstract
In Lake Zone, Tanzania, low contraceptive prevalence, closely spaced births, and child stunting are common. Synergies exist between postpartum family planning (PPFP) and maternal, infant, and young child nutrition (MIYCN), yet health services are often provided in silos. This qualitative formative research study aimed to identify barriers and facilitating factors for optimal nutrition and PPFP practices in Mara and Kagera, Tanzania. Results informed the program design of an integrated nutrition and family planning (FP) implementation approach. The study involved in‐depth interviews with mothers of infants under 1 year (n = 24), grandmothers (n = 12), health providers (n = 6), and traditional birth attendants (n = 12), and 14 focus group discussions with community health workers, fathers, and community leaders. Findings reveal that breastfeeding initiation was often delayed, and prelacteal feeding was common. Respondents linked insufficient breast milk to inadequate maternal nutrition—in terms of the quality of the diet and small quantities of food consumed by mothers. Breast milk insufficiency was addressed through early introduction of foods and liquids. Mothers believed that breastfeeding prevents pregnancy, regardless of the frequency or duration of breastfeeding, yet were generally not aware of the lactational amenorrhea method (LAM) of FP. Joint decision‐making on FP was viewed as important, and women often discussed it with their partner. Future programming should address misconceptions about return to fecundity1 knowledge gaps and concerns about FP methods including LAM; and perceptions regarding insufficient breast milk and early introduction of foods which are impediments to optimal MIYCN and FP practices.
Keywords: breastfeeding, complementary feeding, family planning, infant feeding, lactational amenorrhea method, programme design
Key messages.
Women's early return to work as well as perceived insufficient breast milk, thought to be caused by inadequate maternal nutrition, led to early introduction of foods and liquids prior to 6 months of age.
Misconceptions regarding return to fecundity are common: Although mothers see a link between breastfeeding and fecundity, most are not aware of nor use LAM for postpartum family planning.
Although return to sexual activity varied, PPFP knowledge and use were low, due to concerns about side effects, partner opposition, and waiting for menses to return.
Multilayered interventions should improve integrated service delivery of MIYCN and PPFP; promote community and family support for exclusive breastfeeding alongside LAM and maternal nutrition during lactation; and incorporate cues to action for timely PPFP uptake, LAM transition, and introduction of complementary foods.
1. INTRODUCTION
Intervals of 24 months or less between childbirth and a woman's next pregnancy place children at greater risk of stunting, underweight, and premature death. Global guidelines recommend that women postpone any subsequent pregnancy for at least 2 years after the birth of a child (World Health Organization, 2007). Global data from a 52‐country analysis of Demographic and Health Surveys (DHS) revealed that children conceived less than 24 months after the birth of the next oldest sibling were 1.3–2.3 times more likely to die within the first year of life (Rutstein, 2008). In addition, children conceived 12 to 17 months after their next oldest sibling are 25 percent more likely to be stunted or underweight in comparison with children conceived 36 to 47 months apart (Rutstein, 2008). Moreover, birth intervals of less than 18 months place infants at significantly higher odds of early mortality and small for gestational age (Kozuki et al., 2013).
In Tanzania, DHS data reveal that a high total fertility rate (5.2) combined with substantial unmet need for family planning (FP; 22%) and low modern contraceptive use (32% among currently married women) go hand‐in‐hand with short interpregnancy intervals, inadequate infant and young child feeding practices, and moderate to high levels of stunting (Ministry of Health, Community Development, Gender, Elderly and Children et al, 2016). A reanalysis of the 2010 Tanzania DHS revealed that forty‐seven percent of non‐first births in Tanzania occurred at interpregnancy intervals of less than 24 months and 61% of women who had given birth in the last 2 years had an unmet need for FP (Maternal and Child Health Integrated Program & Maternal and Child Survival Program, 2015).
Suboptimal infant and young child feeding practices pose a challenge, as exclusive breastfeeding (EBF) declines markedly as infants approach 6 months of age. Only about one quarter of Tanzanian infants aged 4–5 months are exclusively breastfed, according to the 2015–2016 Tanzania DHS (Ministry of Health, Community Development, Gender, Elderly and Children, 2016). Efforts to improve EBF can dovetail with improving FP use in the postpartum period. The lactational amenorrhea method (LAM) is a natural contraceptive method that is 98.5% efficacious in protecting against pregnancy up to the first 6 months of life (Labbok et al., 1997). Although LAM provides an opportunity for breastfeeding women to use FP, use of LAM remains very low among married women in Tanzania, at 0.5% (Ministry of Health, Community Development, Gender, Elderly and Children, 2016).
LAM requires that three criteria are met: the woman exclusively breastfeeds, her menses have not resumed, and her infant is less than 6 months (Georgetown University, Institute for Reproductive Health, & Jhpiego, 2009). Menses are a complicated indicator of return to fecundity; in that, it signals anticipated ovulation or even that ovulation has already occurred depending on duration of time since childbirth (Gray et al., 1990). This is especially the case when breastfeeding is only partial, which plays a role in earlier return to fecundity (Eslami, Gray, Apelo, & Ramos, 1990). Prelacteal feeding and early introduction of first foods and liquids prior to the recommended 6 months of age and perceived insufficiency of breast milk can impede EBF and LAM use, according to DHS data from several countries including Tanzania and recent implementation science research (National Bureau of Statistics & ICF Macro, 2011; Kavle et al., 2015).
Despite challenges to EBF and LAM use, several synergies exist between postpartum family planning (PPFP) and maternal, infant, and young child (health and) nutrition (MIYCN), which may be strengthened through integration during routine health contacts (World Health Organization, 2013), yet few studies have explored these linkages. Integrating MIYCN and PPFP during routine health services reinforces information about the importance of maternal nutrition during lactation as well as EBF during the first 6 months, and transition to another modern method of FP before LAM criteria are no longer met, with the commencement of complementary feeding at 6 months of age. These health services, however, are often provided in silos, and missed opportunities exist for integration.
The aim of this formative research study was to examine gaps and opportunities to strengthen integrated service delivery of MIYCN and PPFP in order to inform programme design of an integrated nutrition and FP implementation approach, via the following objectives:
Examine barriers and facilitating factors for breastfeeding initiation, timely introduction of complementary foods, and PPFP use from the perspectives of mothers, family members, and health providers;
Gain an understanding of perceptions around links between breastfeeding, return to fecundity, and timing of introduction of complementary foods among Tanzanian mothers;
Assess sociocultural, household decision‐making, and service delivery triggers for PPFP use and timely complementary feeding at 6 months among Tanzanian mothers and fathers.
2. MATERIALS AND METHODS
2.1. Study sites
The Maternal and Child Survival Program (MCSP), the United States Agency for International Development (USAID)'s global flagship project on maternal, newborn, and child health, conducted this study. MCSP provided technical assistance to the government of Tanzania to improve the delivery of reproductive, maternal, newborn, and child health and nutrition interventions in Mara and Kagera, Lake Zone, Tanzania. Mara is a rural region, with an estimated population of 1.74 million people. Cassava and sweet potatoes are the main food crops, along with rice, sorghum, maize, finger millet, groundnuts, and other legumes. Kagera has a population of 2.45 million and is an agricultural rural region that produces mainly coffee, banana, sweet potatoes, cassava, beans, maize, and sorghum. Mara and Kagera are also both situated on Lake Victoria, and fish is a main food source. In the Lake Zone, over one third of children under 5 years of age are stunted, and in Kagera region, nearly half of children are stunted. The Lake Zone also has a comparatively low modern contraceptive prevalence rate (23.4% compared with the national contraceptive prevalence of 32%, DHS 2015–2016).
Six districts, where MCSP supports the government of Tanzania to strengthen health services, were selected for the study: Musoma DC, Tarime, and Rorya in Mara region and Ngara, Muleba, and Misenyi in Kagera region. These sites were selected to be representative of the range of cultural groups in this region of Tanzania. The health facilities included in the study were within MCSP project areas and had high client loads. Prior to study implementation, health providers received training in PPFP counselling and basic emergency obstetric and newborn care over the period of July 2014–August 2015. The health facilities also had MCSP‐trained community health workers (CHWs) working in the facility catchment areas. These CHWs also received training on provision of interpersonal communication and referrals for reproductive, maternal, newborn, and child health (including basic information about FP and infant feeding) in 2014, prior to study implementation.
2.2. Study design
Conceptualization of the study was framed around an adapted version of the World Health Organization (WHO) framework on child stunting (Figure 1; adapted from Stewart, Iannotti, Dewey, Michaelsen, & Onyango, 2013; Kavle et al., 2015).
Figure 1.
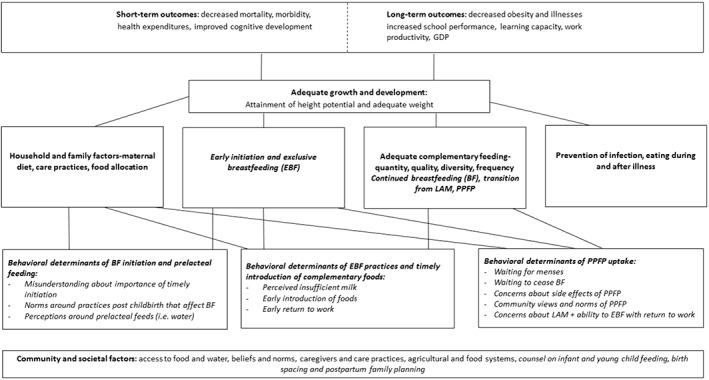
Conceptual framework for maternal, infant, and young child nutrition (MIYCN) and postpartum family planning (PPFP) adapted from World Health Organization framework on childhood stunting (Stewart et al., 2013). Concepts that are italicized represent the variables for which results are presented in this paper. (adapted from Stewart et al., 2013; Kavle et al., 2015)
In collaboration with local researchers, in‐depth interview (IDI) and focus group discussion (FGD) guides were piloted in communities in Mara and Kagera and adapted to the local cultural context. All IDI and FGD guides and oral consent forms were translated and administered in Kiswahili.
IDIs were conducted with mothers of infants less than 1 year (n = 24), grandmothers (n = 12), health providers (n = 6), and traditional birth attendants (TBAs; n = 12), and a total of 14 FGDs (with 15–29 participants) were held with community health workers, fathers, and community leaders. Sample IDI and FGD guides are included as supporting files. The study was conducted in a manner that was in compliance with consolidated criteria for reporting qualitative research (Tong, Sainsbury, & Craig, 2007).
Data collectors were trained to screen the participants to confirm that they met the eligibility criteria. Consent forms were read in the local language for all study participants. This study received ethical approval from National Institute for Medical Research Institutional Review Board (IRB) in Tanzania and the Johns Hopkins Bloomberg School of Public Health IRB in the United States.
2.3. Data collection
Fieldwork took place during December 2015–January 2016. A series of three consecutive IDIs were conducted with mothers of children up to 1 year of age over the course of 3 days in order to gain an understanding of MIYCN and PPFP practices. The consecutive interview approach was selected to build trust and rapport between respondents and interviewers and allow content to be covered in shorter visits of approximately 45 min to 1 hr per session, so as not to overburden the respondents. More culturally sensitive topics, such as resumption of sexual activity, were broached during the third visit. IDIs with mothers, grandmothers, and TBAs were conducted in their homes, whereas IDIs with health care providers were conducted at the health facility in a room with privacy. FGDs were conducted in rooms that offered privacy, organized by village leaders.
2.4. Topics covered
FGDs and IDIs covered the following topics: knowledge and perceptions related to PPFP and MIYCN (including return to fecundity and pregnancy risk after delivery); factors influencing adherence to provider counselling on MIYCN and PPFP; postpartum contraceptive use and MIYCN practices; motivators and barriers to birth spacing or limiting; and care‐seeking patterns for FP, maternal, newborn, and child health services and immunization. Other topics covered include service provider counselling practices (including beliefs/biases) and service delivery processes.
2.5. Analyses
Data collectors audio recorded the IDIs and FGDs. Recordings were transcribed verbatim in Swahili, and local interpreters translated transcripts from Kiswahili into English, which were checked against Swahili (V. M.,E. A., J. M., E. M., H. Y., J. S., M. P., and S. K.). A team of local researchers and MCSP staff jointly reviewed translated interviews, and a 1 week preliminary analysis workshop was held to identify dominant themes drawing from the adapted WHO framework (Figure 1). The categories under which dominant themes were explored included current MIYCN practices (including breastfeeding, complementary feeding, timing of initiation of breastfeeding, prelacteal feeding, and timing of introduction of complementary foods and liquids); knowledge and use of LAM; PPFP use; and return to fecundity, as well as gender norms, couple communication, and household decision‐making.
Findings from these preliminary analyses were used to develop a coding structure, which guided the analyses. Qualitative analyses of transcripts were conducted using hand coding as well as NVIVO v11, an analytic programme (J. N., V. M., J. M., E. A., C. C., J. N., and M. D.; QSR International Pty Ltd., 2012). The coding process allowed for the identification of additional themes emergent from interviews. After coding was completed by the local team, two researchers (J. A. K., C. C.) examined a subset of transcripts to verify the themes and confirm any additional emerging concepts.
3. RESULTS
We present respondent characteristics (Table 1), followed by two illustrative individual experiences with breastfeeding and PPFP uptake (Table 2). We then present study results aligned with the research objectives: (a) behavioural determinants of each of the categories highlighted in the adapted WHO framework (Figure 1)—breastfeeding initiation and prelacteal feeding, EBF and timely introduction of complementary foods, and PPFP uptake; (b) perceptions regarding links between MIYCN and PPFP; and (c) triggers for PPFP uptake related to household decision‐making and provision of health services.
Table 1.
Characteristics of study participants, mothers of infants <1 year, Mara and Kagera, Tanzania
| Age of mother (years) | |||
|---|---|---|---|
| Kagera | Mara | Total | |
| 15–17 | 4 | 1 | 5 |
| 18–23 | 6 | 7 | 13 |
| 24–29 | 0 | 2 | 2 |
| 30+ | 2 | 2 | 4 |
| 24 | |||
| Age of child (months) | |||
| Kagera | Mara | Total | |
| 0–3.99 months | 5 | 4 | 9 |
| 4–6.99 months | 1 | 2 | 3 |
| 7–9.99 months | 4 | 5 | 9 |
| 10–12 months | 2 | 1 | 3 |
| 24 | |||
| Educational level of mothers | |||
| Kagera | Mara | ||
| Some primary school | 2 | 3 | 5 |
| Completed primary school | 7 | 7 | 14 |
| Some secondary school | 3 | 2 | 5 |
Table 2.
Profiles of two women's experiences with maternal, infant, and young child nutrition and family planning practices
| Profile 1 | Profile 2 |
|---|---|
| Mother is 18 years old, works as a farmer, and has a 4 month old infant as well as a 22 month old. She lives with her husband and their children, mother and father in law, and three brothers‐in‐law and their wives and children. Her husband's responsibility is providing food, taking the infant to the hospital for care, and finding money to purchase clothing. She feeds her child only breast milk, because she feels he is still small, she is building a bond with him, and she wants him to grow healthy and strong. She and her husband agreed together that she would feed the child only breast milk for the first 6 months. She had breastfed the older infant for a much shorter time and felt she wanted things to happen differently this time. She breastfeeds him anytime he wakes or cries, and she doesn't have concerns about the quantity of her breast milk. She is motivated to eat well so she can have enough energy to breastfeed. She plans to continue breastfeeding him until he is 2 years old. For herself, she eats stiff porridge with vegetables or sauce, maize, meat, fish, rice, and beans. Just 1 week ago, she started using a contraceptive implant, which she opted for due to the close spacing of her previous pregnancies. The decision to use a family planning method was made together with her husband, although she says her husband was ultimately the one to make the decision. Decisions about infant feeding were made by her husband, mother‐in‐law, and father‐in‐law. | Mother is 18 years old. She has a 3 month old infant who is her only child. She lives with her grandmother, mother, and three siblings. She does not have a close relationship with the father of her child. She works in a shop during the day, but has not yet returned to work since she gave birth. Fourteen hours after the baby was born, she fed him lemonade and then initiated breastfeeding. During the first month, she gave him lemonade because his stomach was filled with gas and her mother advised that the lemonade would reduce the gas. At 2 months, she began feeding the baby tea, which she felt minimized his crying (she also mentioned the nurse advised introducing tea to help motivate breastfeeding). At 3 months, she felt that he was not being sufficiently filled because he was crying frequently, so her mother advised her to initiate porridge. She also feeds him cow's milk once during the day and at night, and she has noticed that that results in him sleeping well. She has noticed that her own breast milk is “very light…like water.” She is not currently using a family planning method but plans to after her son stops breastfeeding. She says the decision to use FP is hers, but she is influenced somewhat by her mother. Regarding her grandmother's influence, she “becomes so upset saying it's too bad because God gave you the ability to have children but you don't want to have them.” She said she would like to receive more information about family planning but has not yet sought out this information at the health facility. She also said she has not received much advice about infant nutrition. Decisions about feeding her child are influenced by her father and mother, “for instance when there is no milk they provide money to buy some more milk or they ask me if some more milk is needed.” |
3.1. Respondent characteristics
The study reached all intended respondent groups (see Table 1), with a total of 150 respondents, including 24 mothers, 12 grandmothers, 46 fathers, 6 service providers, 24 community health workers, 26 community leaders, and 12 TBAs. Characteristics of mothers of infants under age one, as our primary respondent group, are outlined in Table 1. The mean age of mothers was 22 in both Kagera (range: 17–32 years) and Mara (range: 15–31 years). Most mothers worked as farmers or small business operators. The majority of mothers had completed primary education. Health providers ranged in years of working at facilities from 1 to 9 years. Half of grandmothers (n = 6) had never attended school and most worked as farmers.
Two profiles of women's individual experiences with PPFP and MIYCN are included in Table 2, to provide greater illustration of beliefs, perceptions, and practices around FP and nutrition, which include (a) a mother who generally demonstrated optimal MIYCN and FP practices and (b) a mother who experienced substantial gaps in MIYCN and PPFP practices.
3.1.1. Behavioural determinants of breastfeeding initiation and prelacteal feeding
Early initiation of breastfeeding varies and may be delayed for some women
Most mothers and health providers expressed the desire to put the newborn to the breast “immediately” after birth, however the understanding of “immediate” varied. Some mothers started to breastfeed within the first hour after birth, whereas others delayed initiation of breastfeeding to 2 hr or even up to 3 days. Delayed initiation was most commonly attributed to the common practice of bathing, resting, and/or eating food (“taking porridge”), prior to commencing breastfeeding, prioritization of postdelivery cultural practices (i.e., bathing of mother), or challenges with breast milk supply. Mothers generally did not recognize the importance of early initiation of breastfeeding nor had the understanding that delayed initiation can interfere with the child's ability to establish EBF, as illustrated in the following quote:
…I breastfed 3 hours after giving birth…nobody told me to breastfeed her. (Mother, 18 years; child, 9 months; Mara region)
TBAs also spoke of assisting mothers in bathing and preparing porridge for them so that they were able to produce milk before they gave the child to the mother for breastfeeding. The process would take more than an hour before the mother was “ready” to breastfeed her baby, as one mother relayed:
After delivery you need to start with taking a bath and take porridge, then that is when the child can breastfeed. (Mother, 17 years; child, 12 months; Kagera region)
Many infants are fed prelacteal feeds and initiation of breastfeeding is delayed
Some mothers fed their infants prelacteal feeds, namely water, prior to when their breast milk “came down” and until the infant “learns to suckle” or to avoid “starving the child.” Mothers saw infants' cries as a telltale sign of thirst or hunger and thought that providing water prior to breastfeeding could help satisfy the child's needs. At times, water was sweetened or salt was added to give the child “strength to be able to suck.” For example, one mother indicated:
I mixed salt and sugar with boiled water so that the child was not hungry. Traditionally, they say that a child should not be hungry before it knows how to suck. I gave birth in the morning and started breastfeeding in the evening. (Mother, 22 years; child, 2 months; Mara region)
Some mothers waited for their milk to come down, whereas others began breastfeeding despite reporting not having breast milk, as relayed by one mother:
…first day I gave the child water … the second day tea because I did not have breast milk, though she was breastfeeding, but there was no milk until I returned home.”(Mother, 32 years; child, 10 months; Mara region)
3.1.2. Behavioural determinants of EBF practices and timely introduction of complementary foods/liquids
A key barrier to EBF is the perception that the quantity and quality of the breast milk is not sufficient nourishment for infants in the first 6 months of life
Many mothers, fathers, and grandmothers expressed the view that women do not have enough breast milk to satisfy the child's hunger, indicated by the child's cries, the breast “feeling empty” and/or the inability “to squeeze out much milk from the breast.” As discussed by one mother:
There was a time I felt like [the baby] was not being filled only on breastmilk…In the first month when she was breastfeeding…she used to cry. In this second month when I initiated porridge even when she cries it's not so much. (Mother, 28 years; child, 2 months; Mara region)
The consistency of breast milk was seen to be indicative of breast milk quality. “Light milk” was “watery,” “not good for the child's growth,” and linked to “food of poor quality.” “Heavy milk” was thought to be more nutritious and satisfying for the infant, as he/she did not cry immediately after being breastfed. Crying, according to the mothers, indicated “not enough” breast milk or that the breast milk was “too light” to make the child full. As relayed by a TBA:
…if you have heavy milk, the child grows strong; but if your milk is light, the baby suffers as well…weight gain becomes poor and the baby's skin will not be soft. (TBA, Mara region)
Maternal consumption of “enough” and “appropriate” foods is perceived to stimulate breast milk production
Primary factors cited for causing insufficient breast milk, by mothers, fathers, community leaders, and CHWs, were that women are either not eating enough food or not consuming the “appropriate types of food” to stimulate breast milk production. It is believed that a breastfeeding mother needs to consume “good” hot foods and drinks such as porridge, soup, or tea to stimulate milk production. Consumption of “dry or roasted foods” that are not “hot” were seen to negatively affect breast milk production, as relayed by a mother in the following quote:
Breastmilk will not be enough and the child would be crying while breast feeding…[if] the mother does not have enough milk…she eats dry food, not getting porridge or soup to drink…[then] what should she do to increase breast milk?…she should drink porridge…she should put a lot of sauce in her foods and not roasted or dry foods; she should also have soup to drink. (Mother, 17 years; child, 5 months old; Kagera region)
Mothers often believed that eating nutritious foods, which were not affordable or not locally available, could improve the quality of their milk. To increase breast milk production and quality, some mothers took traditional herbs in tandem with trying to improve their own food intake. A few mothers believed that nothing can be done to improve the quality of breast milk, because this was due to “genetic” reasons. Some mothers also expressed concerns that the “more the baby breastfeeds, the less milk there is.”
Women relayed that they often consumed small amounts of food and cited sometimes skipping meals, if food was not available. Some mothers indicated that they only consumed one meal per day. This was illustrated in the quote below:
Most of them [mothers] experience poor nutrition. A mother starts a day with no food not even porridge or any leftovers—depending on what she had the previous night—that way breastmilk will not be sufficient. (Mother, 32 years, child, 1 week old; Kagera region).
Mothers often introduce foods and liquids early, prior to 6 months of age, to address perceived insufficient breast milk
Mothers frequently introduce foods, as early as 3 to 4 months of age, to address breast milk insufficiency, marked by cries of hunger by infants, as relayed often by mothers “he would cry so very much while breastfeeding that…my mother advised me to initiate porridge.” A watery porridge was often introduced first, as the watery consistency was seen to be good for the child's stomach as “new” food.
Other “soft” foods introduced early included soft‐cooked beans, ugali (a stiff dough prepared with cornmeal, cassava flour, and sorghum or millet), potatoes, banana, fish, and cooked rice.
Most mothers reported returning to work within 1 month of giving birth, which can affect their ability to maintain EBF. Mothers working outside the household, who farm, are more likely to introduce foods early while continuing to breastfeed. Mothers typically work in the fields between four to six hours at a time. Some mothers leave infants under the care of other household members, whereas other mothers brought their infants with them to the field. A concern was expressed by a mother in Mara who believed that working out in the sun negatively affected her breast milk:
…when a mother comes back from performing heavy work or having walked in the sun, you should not breastfeed the child because such situations disturb breastmilk form, and it becomes lighter. (Mother, 22 years; child, 2 months; Mara region)
Mothers, especially adolescents, who reported working around the home, would continue with their domestic chores between breastfeeding sessions. In Kagera, it was noted that mothers work much closer to home and are able to breastfeed more often compared with mothers in Mara region, who travel farther to work as farms are outside the village residential areas. For example, one mother in Kagera describes how she feeds her child while farming:
Who takes care of the baby when you are on the farm? [An older child in the household] carries him. How about feeding him?… He has not started eating so she calls me to come and breastfeed. Because I do not work [far] from home, it is easy. When the child cries, they will call me to come back and breastfeed him. (Mother, 17 years; child, 5 months; Kagera region)
3.1.3. Perceived links between breastfeeding, LAM, return to fecundity, and timely introduction of complementary foods/liquids
Mothers recognized a relationship between breastfeeding and birth spacing, but gaps in understanding exist and use of LAM is low
Mothers expressed a belief that women are protected from pregnancy for as long as they are breastfeeding, regardless of the frequency or duration of breastfeeding. Breastfeeding for a long period over time (in months) was linked to delay of menses. However, women also discussed that some women's menses returned even while they were still breastfeeding. Some women said that they had heard that breastfeeding helps birth spacing, but they did not trust the method because other women breastfeed and do not see their menses but still get pregnant.
Although some mothers, fathers, and grandmothers had heard of using breastfeeding for birth spacing, knowledge of “LAM” as a FP method was low across respondent groups. One father in Mara noted:
I once heard that when a woman is breastfeeding, she does not get her menstruation period. It only starts when she stops breastfeeding, so it can be used as a method of family planning. (FGD, fathers, Mara region)
Several respondents, including fathers and health providers expressed concerns about whether LAM is a method that mothers can actually adhere to. Some men in the FGDs also doubted the effectiveness of LAM as a FP method. On the other hand, some fathers expressed positive views about using breastfeeding for birth spacing, especially due to the fact that it is a safe method with no side effects in comparison with other FP methods. A father in Mara expressed:
…I think this is a good method [LAM] because it does not have side effects compared with shots and implants. A mother will be in good health, more if she is using breastfeeding as a method of family planning. (FGD, fathers, Mara region)
Knowledge about LAM among the CHWs and health service providers was mixed, with some demonstrating a better understanding of the method and others demonstrating poor understanding and/or distrust of the method.
None of the mothers with children less than 6 months of age reported that they were using LAM as an FP method. In addition, health service providers do not proactively discuss LAM as a postpartum contraceptive option, as they often do not consider it to be an effective method.
This method [LAM] is not preferred by many. That is the reason we advise mothers to use other methods…It is a method that is not well known in the community, and we are not very sure women will be able to follow it properly. That is why we are advising them to use other methods of family planning. (Health service provider, Kagera region)
3.1.4. Behavioural determinants of PPFP
Postpartum return to sexual activity linked to perceived timing of recovery from childbirth and fear of infidelity
Resumption of sex after childbirth varied across respondents, ranging from 1 month to 1 year after childbirth. Timing was often linked to when the woman has stopped bleeding or recovered after childbirth. Early resumption of sex was mainly attributed to lack of patience among men or fear among women that they will lose their husbands to other women if they delay resuming sex, as illustrated here:
It's difficult for men to wait for two or three months. He tells you according to traditions here, he cannot wait otherwise he will have extra‐marital affairs. (Mother, 28 years; child, 2 months, Mara region)
Postpartum contraceptive use among mothers is low
Women clearly want to avoid pregnancy, especially in the first year postpartum. Women's concern during that year was mainly focused on the welfare of the new baby and a desire to rest after childbirth.
I have not started using family planning; I am still discussing with my husband…I expect to start using this month because I have seen it is important, as I am tired of giving birth and I have enough children. (Mother, 28 years; child, 2 months; Mara region)
However, overall use of contraceptives by respondents was low. Of the 12 mothers interviewed who had children under the age of 6 months, only two reported that they were using contraceptives (implant and injectables [Depo‐Provera]). Many women relied more on breastfeeding for protection against pregnancy, which they believed was effective as verified by the lack of the return of their menstrual periods (or “menses”). Although as mentioned previously, they were not actively following LAM criteria, and frequency and duration of breastfeeding were suboptimal. The main reasons for not using contraceptives were not having seen their menstrual periods or that the child was still breastfeeding.
Use of FP beyond 6 months after delivery was also low. Only two out of 12 mothers with children above the age of 6 months reported using a modern FP method. These two mothers had children aged 9 and 10 months and were using Depo‐Provera (injectable contraceptives). Both women reported discussing their intention to use FP with their husbands.
Women often wait for menses return to initiate postpartum contraceptive use
The return of menses is taken as the first sign of the return to fecundity and signals to mothers that it is time to start using a FP method. Mothers explained that once a woman sees her menses, she should either abstain from sexual activity or think of using an FP method. For example, one mother expressed:
What will motivate you to start using a family planning method in the near future?…until I see my periods, and I can only go when I see my periods. (Mother, 25 years; child, 1 month; Mara region)
Resuming menses as a sign of return to fecundity was also shared by fathers and CHWs. Some mothers reported that health providers required that a woman see her menses before initiating FP.
I was told at the health facility I should wait until I resume my periods to start using family planning. (Mother, 31 years; child, 1 year; Kagera region)
Other factors affecting PPFP uptake include waiting to stop breastfeeding, concerns about side effects, and partner opposition.
Women believed that they are protected from a subsequent pregnancy because they are breastfeeding, regardless of the frequency and duration of breastfeeding, as one woman relayed:
I have not started using any family planning, but I expect to do that once I have stopped breastfeeding my son…and when are you planning to stop?…when he is 1 year and 2 months. (Mother, 18 years; child, 3 months; Mara region)
Another challenge preventing women from initiating use of a modern contraceptive method was concerns about side effects. This concern was raised by mothers as well as fathers and grandmothers.
The side effects that are related to family planning makes most mothers to give up on it, for instance [implants] might get dislodged and go as far as to the back of the head…and make other people to be admitted in hospitals for operation. Intrauterine devices make the intestine to coil around it, contraceptive pills makes women to have menstruation period for a long time. (Grandmother, Mara region)
Fathers mentioned concerns about irregular bleeding (heavy bleeding and absence of bleeding), cancer, and loss of sexual desire due to FP, as well as cost‐related concerns, as discussed by fathers:
Women who are using family planning have poor health. For instance, using the intrauterine device harms a mother's health, and still you have to spend 70,000 shillings [approximately $30 USD] to remove it. It has reached a point that family planning does not help, but rather brings some problems to us. (FGD, fathers, Mara region)
Another obstacle to FP uptake among postpartum women is their husband's opposition, often linked to their fear of side effects or desire to have more children, as indicated below:
Many men refuse to allow their wives to use family planning, so they have to hide that they go to the health facility to get an injection or pills without the husband knowing because the husbands want them to continue having children. Many men do not have adequate knowledge, and some of them refuse completely. (FGD, CHWs, Kagera region).
Furthermore, using contraception was linked to the belief that a woman was not being faithful to her husband: she decided to use FP to become “free.” A woman “being free” was defined as a woman not having the responsibility to take care of children, especially when FP methods are linked to infertility, and hence, she has time to engage in sexual relations with other men.
3.1.5. Sociocultural, household decision‐making around nutrition and PPFP, and service delivery triggers for PPFP
Mothers primarily make decisions regarding which foods and when to feed children, whereas fathers strongly influence decisions on PPFP.
Mothers reported that the father's role was mainly to ensure that money was available for the family to buy food, provide suggestions on foods to eat (i.e., ugali and fish), yet fathers rarely feed the children.
For FP, fathers indicated that it is important to discuss FP as a couple; however, it is husbands that have a significant role in deciding whether or not their wives use a FP method, in large part due to their responsibility to provide for the family. For example, several fathers noted:
We discuss, together with my wife on using family planning, if you just take her for family planning, she would ask you ‘How about you?’ (FGD, fathers, Mara region)
A father is a decision maker on family planning matter because he also provides for the family; if family planning decisions are left on women, they will bring children the father cannot handle (FGD, fathers, Mara region)
Discussions with partners about FP use or intention to use FP were not universal. A little over half of mothers interviewed reported discussing FP with their partners. When couples did discuss these topics, the discussions took place during the pregnancy period and also after delivery. It was reported that partners would discuss FP use based on the desire to space/limit the number of children. As noted above, fear of side effects was reported as an obstacle to men agreeing to discuss FP use.
Some mothers mentioned that they had received information about FP and infant feeding through community health workers and at the hospital or health center. However, others indicated that they had not received any information on these topics from a health worker. For many mothers, FP and infant and young child feeding had not been raised during routine maternal and child health visits at the health facility.
4. DISCUSSION
In this study, we sought to explore perceptions and beliefs that shape breastfeeding and complementary feeding practices, LAM, and PPFP. We provide considerations for rollout of integrated nutrition and FP interventions, within the context of health programming. Our findings reveal that the timing of initiation of breastfeeding was often delayed for several hours or days and prelacteal feeding was common. Although families understand the importance of breastfeeding, mothers had difficulty maintaining EBF due to working the fields and perceptions of insufficient breast milk were linked to inadequate maternal nutrition—in terms of the quality and the small quantities of foods consumed by mothers. Breast milk insufficiency was often addressed through early introduction of foods and liquids at 3–4 months of age. At the same time, mothers held the common belief that breastfeeding is protective against pregnancy, regardless of the frequency or duration of breastfeeding. These data also reveal a disconnection between the concept of “breastfeeding for birth spacing” and knowledge of LAM as a FP method among all participants. A distrust of LAM as an FP method was reported by study participants, as health providers rarely counsel mothers and families on LAM among other methods; PPFP use is low, yet mothers often reported return to sexual activity within the first several months postpartum. Joint decision‐making on FP was cited as important, and the majority of mothers indicated they discussed it with their partner.
Our findings are consistent with studies in Bangladesh and Kenya, which have also identified barriers to PPFP uptake related to misconceptions around return to fecundity, pregnancy risk, and the role of breastfeeding (Cooper et al., 2014; Cooper et al., 2017; Kouyaté et al., 2015). A study conducted in Morogoro, Tanzania, similarly identified concerns about side effects as a critical reason for nonuse of contraceptives (Chebet et al., 2015). Inadequate social support, perceived inadequate maternal nutrition, perceptions of insufficient breast milk, and difficulty breastfeeding while working outside the home have been highlighted as key barriers to EBF (Dulli & Randrianasolo, 2015; Kavle, LaCroix, Dau, & Engmann, 2017; Matsuyama, Karama, Tanaka, & Kaneko, 2013). Consumption of foods perceived to be nutritious is associated with sufficient milk production, good quality of “heavy” milk, and health of the child and energy levels of the mother in studies in Egypt and DRC (Kavle et al., 2018; Maternal and Child Survival Program, 2018).
Although LAM is a natural contraceptive method that is 98.5% efficacious in protecting against pregnancy when the three conditions for use are met, LAM is often overlooked and not incorporated in country health programmes, including in this region of Tanzania (Labbok et al., 1997). If women are counselled about the three criteria for LAM use, many women do not adequately adhere to them, and/or do not transition from LAM to another modern method before they are at risk of pregnancy (Türk, Terzioğlu, & Eroğlu, 2010; Kouyaté et al., 2015). A recent multicountry DHS analysis found that approximately 75% of women who reported using LAM actually did not meet the three LAM criteria (Fabic & Choi, 2013).
Globally, effective communication regarding return to fecundity, pregnancy risk after delivery, LAM, and the importance of timely transition has proven difficult. Breastfeeding problems and challenges, many of which are unaddressed and underestimated in the first 6 months of age, continue to affect exclusivity of breastfeeding and compromise using LAM as a FP method (Kavle et al., 2017).
Programmes that have promoted LAM along with infant and young child feeding messages have demonstrated increases in EBF rates and continued use of FP at 1 year postpartum (Ahmed et al., 2015; Bongiovanni, Samam'h, Al'Sarabi, Masri, & Zehner, 2005). A study in Kenya also demonstrated the feasibility of integrating MIYCN and FP services at health centres and dispensaries as well as through community level activities including home visits by community health workers (Cooper et al., 2017).
This study's unique contribution is that it explored perceptions and experiences with infant and young child nutrition and PPFP in an integrated way, which facilitates the design of programme strategies to reduce missed opportunities for both interventions during the first year postpartum.
4.1. Strengths and limitations
The study collected in‐depth qualitative data from a total of 150 mothers, fathers, grandmothers, health providers, community health workers, and influential community members, and attained saturation with regard to the breadth of beliefs and perceptions on topics present in this paper. One limitation was respondents were only those with infants under 1 year of age, so data on continued breastfeeding until 2 years was limited, and complementary feeding practices only included timely introduction of foods. Therefore, we did not have information about practices during the 1‐ to 2‐year period, which remains critical for optimal infant health and spacing of pregnancies. Given the number of consecutive IDIs, it is possible that some information may not have been conveyed in translation from Swahili to English. Multiple expert Swahili researchers reviewed the recordings and translations to minimize any data loss. Collection of in‐depth dietary information through 24‐hr recall or food frequency for maternal nutrition during breastfeeding and complementary feeding data would have strengthened and aided in supporting our findings. This would have allowed for further elaboration on dietary diversity, meal frequency, and quantities of foods consumed by young children.
4.2. Programmatic implications
Study findings provide valuable insights to inform the development of activities to improve MIYCN and PPFP practices in Tanzania's Lake Zone. Specific nutrition and FP integration opportunities are identified in alignment with the Circle of Care Model (Health Communication Capacity Collaborative, 2017), which illustrates entry points for facilitating social and behaviour change within the context of service delivery: before, during, and after services (see an adapted version of the model in Figure 2). We selected this model to guide reflections on implications for future programming due to the interface between social and behaviour change and service delivery efforts, which allow for identification of entry points for future conjoined programming to address barriers to MIYCN and PPFP identified in this study.
Figure 2.
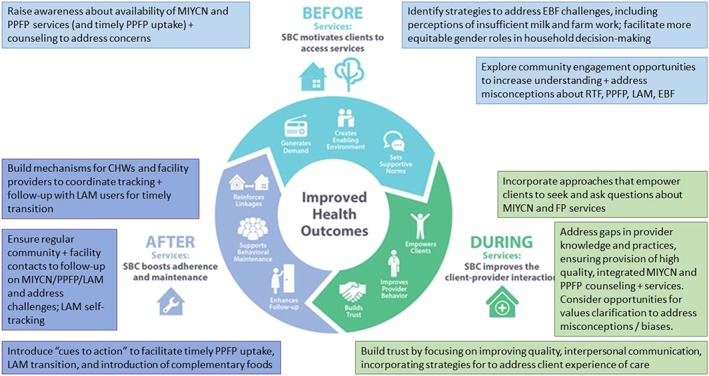
Maternal, infant, and young child nutrition (MIYCN) + family planning (FP) program opportunities across the circle of care (adapted from HC3)
4.2.1. Before services
Findings from this study indicate a need for efforts to increase understanding among mothers and fathers about maternal nutrition during lactation, importance of early and EBF, return to fecundity, and PPFP options including LAM (about which knowledge is currently very low). Creating an enabling environment will require providing support for early initiation of breastfeeding and maintaining EBF for the full 6 months at the community level. Specifically, programmes should engage fathers and key family members regarding solutions that allow women to delay return to work, address perceptions around breastfeeding challenges (i.e., perceptions around breast milk sufficiency) that impede EBF, and address concerns surrounding FP use (i.e., side effects and partner opposition) and planning for appropriate family size.
Community support for early initiation and EBF is needed to improve breastfeeding rates and ensure that LAM is a viable contraceptive option.
4.2.2. During services
Our study showed that gaps exist in the information and counselling provided during health service contacts. Program approaches should look for opportunities to encourage mothers and families to seek MIYCN, PPFP, and other health services while at the health facility. Efforts are needed to address gaps in provider knowledge, to address misconceptions and build support for LAM as a contraceptive option, and to ensure that high quality counselling on MIYCN and PPFP (including other PPFP options if LAM is not desired or feasible) is provided during health contacts from pregnancy through the first year postpartum and beyond. LAM presents a unique opportunity to link conversations about breastfeeding and timely introduction of complementary foods with return to fecundity and importance of timely contraceptive uptake at 6 months postpartum (Kavle et al., 2018).
This study demonstrates that training alone will not facilitate sustained changes in health worker practices (as health workers had been trained in PPFP prior to the study, yet gaps remained). A provider behaviour change lens to strengthen service integration at health contacts from pregnancy to the months following childbirth will serve to improve service delivery at both facility and community levels. This will entail on‐site training on integrated MIYCN and PPFP, paired with mentoring, and routine supportive supervision to improve integrated counselling for MIYCN and PPFP, screening for FP needs, ensuring provision of quality FP, screening for nutritional needs, and linking up to services.
4.2.3. After services
Following receipt of FP and MIYCN services at the health facility, linkages between health facility providers and community health workers can facilitate follow‐up. Active monitoring and support at the community level can provide support to maintain EBF, address any breastfeeding problems that may arise, discuss LAM, as well as initiation and continued use of FP for at least 2 years (Kavle et al., 2018). Women using LAM have an especially critical need for follow‐up to ensure that they adhere to the LAM criteria and transition to another FP method by 6 months postpartum, while at the same time, introducing complementary foods at 6 months of age (Kavle et al., 2018). Opportunities to enable women to self‐track their own LAM use along with “cues to action” to facilitate timely transition to another contraceptive method and introduction of complementary foods are worth exploring in future programming.
4.3. Next steps for implementation
Findings from this formative research study are being used in the development of a set of interventions that MCSP will implement in collaboration with the government, to promote optimal MIYCN and FP practices in Mara and Kagera regions. The integrated programmatic approach will include activities at facility, household, and community levels in line with recommendations above, with documentation of implementation results in a separate forthcoming publication.
5. CONCLUSION
This study identified barriers and facilitating factors for infant feeding and postpartum FP practices, such as misconceptions around insufficient breast milk, lack of knowledge and use of LAM, return to fecundity and concerns about FP methods, and alongside pressure to return to work early after childbirth. These gaps should be addressed using innovative, sustainable approaches in service delivery that incorporate provider behaviour change, culturally tailored counselling strategies, cues to action, and opportunities to strengthen client and family agency in decision making for PPFP and nutrition.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest. While USAID provided reviews of the content in this article, authors had intellectual freedom to incorporate feedback, as needed.
CONTRIBUTIONS
CMC and JAK led research study conceptualization. CMC, JAK, AP, MD, and RL contributed to development of data collection tools. JN led the data collection, with oversight from MD and RLJN led the analyses, and CMC, JAK, MD, RL, and LM contributed to the analysis of data and interpretation of results. CMC and JAK led the writing of the paper, and JN, MD, RL, LM, and AP contributed to writing of the paper. All authors agreed for submission of the manuscript for publication.
FUNDING
This article is made possible by the generous support of the American people through the United States Agency for International Development (USAID) under the terms of the Cooperative Agreement AID‐OAA‐A‐14‐00028. The contents are the responsibility of the Maternal and Child Survival Program and do not necessarily reflect the views of USAID or the United States Government.
Supporting information
Data S1. Supporting information
Data S2. Supporting information
ACKNOWLEDGEMENTS
We would like to acknowledge the contributions of Elizabeth Sasser, Chrisostom Lipingu, and John George from MCSP/Jhpiego; Sarah Straubinger and Allison Gottwalt from MCSP/PATH; and Violet Mbilima and Judith Meta from the University of Dar es Salaam. Finally, we appreciate the contributions of the Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) and regional offices in guiding and facilitating this study.
Cooper CM, Kavle JA, Nyoni J, et al. Perspectives on maternal, infant, and young child nutrition and family planning: Considerations for rollout of integrated services in Mara and Kagera, Tanzania. Matern Child Nutr. 2019;15(S1):e12735 10.1111/mcn.12735
Return to fecundity refers here to a woman's ability to become pregnant after childbirth
Footnotes
Defined as menstrual bleeding.
PPFP refers to the start and use of a modern contraceptive method during the first year after childbirth. Source: World Health Organization, 2013.
REFERENCES
- Ahmed, S. , Ahmed, S. , McKaig, C. , Begum, N. , Mungia, J. , Norton, M. , & Baqui, A. H. (2015). The effect of integrating family planning with a maternal and newborn health program on postpartum contraceptive use and optimal birth spacing in rural Bangladesh. Studies in Family Planning, 46(3), 297–312. 10.1111/j.1728-4465.2015.00031.x [DOI] [PubMed] [Google Scholar]
- Bongiovanni, A. , Samam'h, M. A. , Al'Sarabi, R. H. , Masri, S. D. , & Zehner, E. R. (2005). Promoting the lactational amenorrhea method (LAM) in Jordan increases modern contraceptive use in the extended postpartum period. Washington, DC: LINKAGES Project & Academy for Educational Development. [Google Scholar]
- Chebet, J. J. , McMahon, S. A. , Greenspan, J. A. , Mosha, I. H. , Callaghan‐Koru, J. A. , Killewo, J. , … Winch, P. J. (2015). Every method seems to have its problems—Perspectives on side effects of hormonal contraceptives in Morogoro Region, Tanzania. BMC Women's Health, 15(1), 97 10.1186/s12905-015-0255-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, C. M. , Ahmed, S. , Winch, P. J. , Pfitzer, A. , McKaig, C. , & Baqui, A. H. (2014). Findings from the use of a narrative story and leaflet to influence shifts along the behavior change continuum toward postpartum contraceptive uptake in Sylhet District Bangladesh. Patient Education and Counseling, 97(3), 376–382. 10.1016/j.pec.2014.09.007 [DOI] [PubMed] [Google Scholar]
- Cooper, C. M. , Ogutu, A. , Matiri, E. , Tappis, H. , Mackenzie, D. , Pfitzer, A. , & Galloway, R. (2017). Maximizing opportunities: Family planning and maternal, infant, and young child nutrition integration in Bondo Sub‐County, Kenya. Maternal & Child Health Journal, 21(10), 1880–1889. 10.1007/s10995-017-2341-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulli, L. , & Randrianasolo, B.S. (2015). Formative research to improve the promotion of the Lactational Amenorrhea Method (LAM) and exclusive breastfeeding (EBF) in the MAHEFA USAID/Madagascar Program, Ambilobe District, DIANA Region. Washington, DC: FHI 360/FANTA.
- Eslami, S. S. , Gray, R. H. , Apelo, R. , & Ramos, R. (1990). The reliability of menses to indicate the return of ovulation in breastfeeding women in Manila The Philippines. Studies in Family Planning, 21(5), 243–250. 10.2307/1966504 [DOI] [PubMed] [Google Scholar]
- Fabic, M. S. , & Choi, Y. (2013). Assessing the quality of data regarding use of the lactational amenorrhea method. Studies in Family Planning, 44(2), 205–221. 10.1111/j.1728-4465.2013.00353.x [DOI] [PubMed] [Google Scholar]
- Georgetown University, Institute for Reproductive Health, & Jhpiego (2009). Lactational amenorrhea method (LAM): A learning resource package for family planning service providers and trainers. Washington, DC: Georgetown University. [Google Scholar]
- Gray, R. H. , Campbell, O. M. , Apelo, R. , Eslami, S. S. , Zacur, H. , Ramos, R. M. , … Labbok, M. H. (1990). Risk of ovulation during lactation. The Lancet, 335(8680), 25–29. 10.1016/0140-6736(90)90147-W [DOI] [PubMed] [Google Scholar]
- Health Communication Capacity Collaborative [HC3] (2017). The Circle of Care Model: Social and behavior change along the service delivery continuum. Baltimore, MD: HC3. [Google Scholar]
- Kavle, J. A. , LaCroix, E. , Dau, H. , & Engmann, C. (2017). Addressing barriers to exclusive breast‐feeding in low‐ and middle‐income countries: A systematic review and programmatic implications. Public Health Nutrition, 20(17), 3120–3134. 10.1017/S1368980017002531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavle, J. A. , Mehanna, S. , Khan, G. , Hassan, M. , Saleh, G. , & Engmann, C. (2018). Program considerations for integration of nutrition and family planning: Beliefs around maternal diet and breastfeeding within the context of the nutrition transition in Egypt. Maternal & Child Nutrition, 14(1). 10.1111/mcn.12469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavle, J. A. , Mehanna, S. , Saleh, G. , Fouad, M. A. , Ramzy, M. , Hamed, D. , … Galloway, R. (2015). Exploring why junk foods are ‘essential’ foods and how culturally tailored recommendations improved feeding in Egyptian children. Maternal & Child Nutrition, 11(3), 346–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouyaté, R. A. , Ahmed, S. , Haver, J. , McKaig, C. , Akter, N. , Nash‐Mercado, A. , & Baqui, A. (2015). Transition from the lactational amenorrhea method to other modern family planning methods in rural Bangladesh: Barrier analysis and implications for behavior change communication program intervention design. Evaluation and Program Planning, 50, 10–17. 10.1016/j.evalprogplan.2014.11.008 [DOI] [PubMed] [Google Scholar]
- Kozuki, N. , Lee, A. C. , Silveira, M. F. , Victora, C. G. , Adair, L. , Humphrey, J. , … Katz, J. (2013). The associations of birth intervals with small‐for‐gestational‐age, preterm, and neonatal and infant mortality: A meta‐analysis. BMC Public Health, 13(3), S3 10.1186/1471-2458-13-S3-S3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labbok, M. H. , Hight‐Laukaran, V. , Peterson, A. E. , Fletcher, V. , Von Hertzen, H. , & Van Look, P. F. (1997). Multicenter study of the lactational amenorrhea method (LAM): I. Efficacy, duration, and implications for clinical application. Contraception, 55(6), 327–336. 10.1016/S0010-7824(97)00040-1 [DOI] [PubMed] [Google Scholar]
- Maternal and Child Health Integrated Program & Maternal and Child Survival Program (2015). Family planning needs during the first two years postpartum in Tanzania. Washington, DC: MCHIP & MCSP. [Google Scholar]
- Matsuyama, A. , Karama, M. , Tanaka, J. , & Kaneko, S. (2013). Perceptions of caregivers about health and nutritional problems and feeding practices of infants: A qualitative study on exclusive breast‐feeding in Kwale Kenya. BMC Public Health, 13(1), 525 10.1186/1471-2458-13-525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maternal and Child Survival Program (2018). Integration of preventive and curative aspects of nutrition into integrated community case management (iCCM) in the Democratic Republic of Congo: Study report. Washington, DC: MCSP. [Google Scholar]
- Ministry of Health [MoH] (Zanzibar), National Bureau of Statistics [NBS] (Tanzania), Office of the Chief Government Stat [OCGS] (Tanzania), & ICF (2016). Tanzania Demographic and Health Survey and Malaria Indicator Survey (TDHS‐MIS) 2015–16. Dar es Salaam, Tanzania & Rockville, MD: MoHCDGEC, MoH, NBS, OCGS, & ICF. [Google Scholar]
- Ministry of Health, Community Development, Gender, Elderly and Children (Tanzania) (2016). The national road map strategic plan to improve reproductive, maternal, newborn, child & adolescent health in Tanzania (2016–2020): One plan II. Dar es Salaam. Tanzania: MoHCDGEC. [Google Scholar]
- NBS (Tanzania), & ICF Macro (2011). Tanzania Demographic and Health Survey 2010. Dar es Salaam, Tanzania: NBS & ICF Macro. [Google Scholar]
- QSR International Pty Ltd . (2012). NVivo qualitative data analysis software. Version 11.
- Rutstein, S. O. (2008). Further evidence of the effects of preceding birth intervals on neonatal, infant, and under‐five‐years mortality and nutritional status in developing countries: Evidence from the Demographic and Health Surveys. Calverton, MD: MEASURE DHS. [DOI] [PubMed] [Google Scholar]
- Stewart, C. P. , Iannotti, L. , Dewey, K. G. , Michaelsen, K. F. , & Onyango, A. W. (2013). Contextualising complementary feeding in a broader framework for stunting prevention. Maternal and Child Nutrition, 9(Suppl 2), 27–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Türk, R. , Terzioğlu, F. , & Eroğlu, K. (2010). The use of lactational amenorrhea as a method of family planning in eastern Turkey and influential factors. The Journal of Midwifery & Women's Health, 55(1), e1–e7. 10.1016/j.jmwh.2009.02.015 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2013). Programming strategies for postpartum family planning. Geneva: WHO. [Google Scholar]
- World Health Organization (2007). Report of a WHO technical consultation on birth spacing: Geneva, Switzerland, 13–15 June 2005. Geneva: WHO. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting information
Data S2. Supporting information


