Abstract
The aim of this cross‐sectional study was to assess differences in caries experience according to socio‐economic status (SES) in a health‐care system with full coverage of dental costs for children up to the age of 18 yr. In 2011 and 2014, by performing hurdle negative binomial models, we obtained data on 3,022 children and young adults aged 5, 8, 11, 14, 17, 20, and 23 yr, living in four cities in the Netherlands. At all ages between 5 and 23 yr, the percentages of children with caries‐free dentitions were lower and mean caries experience were higher in low‐SES than in high‐SES participants. In 5‐yr‐old children with dmft > 0, mean caries experience was 3.6 in those with low SES and 2.3 in those with high SES. In 23‐yr‐old participants, these estimates were 6.8 and 4.4, respectively (P < 0.05). Low‐SES children have a greater risk of more caries experience than high‐SES children. Thus, in a system with full free paediatric dental coverage, socio‐economic inequality in caries experience still exists. Dental health professionals, well‐child care doctors and nurses, general practitioners, and elementary school teachers should collaborate to promote oral health at the community level, with specific targeting of low‐SES families. We further need policy measures to curtail, at community level, the increasing availability and consumption of highly processed, carbohydrate‐rich foods, with particular attention for low‐SES families.
Keywords: access to care, caries experience, dental care, public health dentistry, youths
Disparities in child health according to socio‐economic status (SES) are often reported. Youths in high‐SES families generally experience better health than youths in low‐SES families 1. Children and young adolescents experiencing socio‐economic disadvantages encounter a wide range of health risk factors and adverse outcomes in adulthood 2, including increased risks of injury, asthma, and elevated blood pressure, as well as involvement in risky health behaviours, such as smoking and physical inactivity 2, 3.
Dental caries experience is reportedly a strong indicator of socio‐economic inequality in both children and adults 4, 5, 6, 7, 8, 9, 10, 11. It is the most common paediatric disease 12. Among 5‐ to 17‐yr‐old individuals in the USA, dental caries is over five times more common than asthma and seven times more common than hay fever 13. The term ‘dental caries’ refers to decay on any surface of a tooth 14. It is characterized by a continuum of disease states, ranging from subclinical lesions to cavitated lesions that extend into dentine or even into the pulp. If left untreated, caries may lead to pain, discomfort, infections, or tooth loss. Dental caries, and poor oral health in general, has a major impact on children's overall health, growth, and development. It not only affects the ability to chew and eat properly but can also result in lost school hours and affect a child's overall wellness and self‐esteem 15, 16.
Prevention of caries in children requires adequate oral hygiene and a healthy diet with limited cariogenic foods, as well as starting young with dental check‐ups and regular dental visits. Risk factors, on the other hand, include brushing teeth less than two times a day, frequent consumption of cariogenic foods, skipping breakfast, and lower parental educational level and income 12, 17, 18, 19, 20. Low‐SES individuals have been found to be more likely to have inadequate preventive oral‐health behaviour 21, 22.
Availability of full financial coverage for costs of dental care may also affect whether children receive dental care and the occurrence of dental caries 23. However, other factors may contribute, such as low parental oral health literacy and limited parental language proficiency 23, 24. Moreover, care‐related barriers may add to this (e.g. inadequate preventive services, care that is not culturally well adapted, and services that do not fully take into account low levels of oral health literacy) 23, 24.
In the Netherlands, dental care for youth is included in the mandatory health insurance and is free of charge for children up to 18 yr of age. Research in this setting can clarify to which degree factors other than the costs of dental care contribute to socio‐economic differences in caries experience. The research question for this study was therefore: In a health‐care system with full coverage of dental costs for children up to the age of 18 yr, does a socio‐economic difference in caries experience exist, based on SES? Our hypothesis was that between socio‐economic groups in children up to 18 yr of age, all of whom have free access to dental services, no differences in oral health would exist.
Material and methods
Study population
During the study period from March 2011 through October 2011 and April 2014 through November 2014, children and young adults aged 5–23 yr who were living in four medium‐sized cities in the Netherlands were eligible to participate. These four cities (Gouda, Alphen aan den Rijn, Breda, and Den Bosch) are typical of the Dutch population regarding age, gender, ethnicity, and marital status 25. Random samples were drawn from the municipal population records of each city and stratified according to age, to reach similar numbers per city per age category. Sample sizes were determined based on the potential to detect relative differences of 30% in mean caries experience, from earlier estimates from 2005 to 2009, at an alpha of 0.05 with a power of 80%. This led to a required sample size of about 450 children per age category 26, 27.
In total, 13,961 children and young adults aged 5–23 yr (and their parents) received invitations to participate, including information about the purpose of the study. Trained interviewers personally attempted to contact individuals who had not responded, to emphasize the importance of the study. If the initial contact attempt failed, the interviewer made a maximum of three additional attempts. Individuals who refused to participate were asked to fill out a non‐response questionnaire with questions about gender, SES, and oral health behaviour. Of the 13,961 children and young adults and their parents invited to take part in the study, 3,022 (23%) participated.
Ethics statement
The Central Committee on Research Involving Human Subjects concluded that no ethical considerations were involved, as the clinical proceedings were harmless and the questions not sensitive in nature. The study met all the requirements of the Personal Data Protection Act (number m1383077 for 2011 and number m1556571 for 2014).
Procedure and measures
Data were gathered via clinical oral examinations and a questionnaire. The questionnaire was completed by a parent for the 5‐, 8‐, and 11‐yr‐old children and by the 14‐, 17‐, 20‐, and 23‐yr‐old subjects themselves. In this study, SES was operationalized as the highest level of education completed by the mother of the children aged 5, 8, and 11 yr or by the adolescent/young adult (ages 14, 17, 20, and 23 yr). A total of 10 or fewer years of education was coded as low SES, whereas a total of more than 10 yr of education was coded as high SES. This decision was in accordance with the International Standard Classification for Education 2011 28.
The total score of the decayed, missing, and restored teeth (DMFT) index was used to indicate level of caries experience 29. The DMFT score represents caries experience in permanent teeth, whereas the dmft score represents that in deciduous teeth. Caries‐free dentitions are defined in our paper as those with dmft = 0 or DMFT = 0. Caries experience was observed during a clinical oral examination that comprised visual inspection of the teeth with documentation of caries lesions and any subsequent treatment (i.e. restoration or extraction). Participants in urgent need of treatment were advised to visit their dental professional.
Clinical examinations were performed by four dentists in a mobile oral health facility. During the clinical assessment, both permanent and deciduous teeth were evaluated, depending on the age of the participant. For children aged 5 yr, only caries in deciduous teeth was included. For children aged 8 yr, caries in both deciduous and permanent teeth was included. For children aged 11 yr or older, permanent teeth were evaluated, with the exclusion of wisdom teeth.
To assess the quality of the clinical examinations, we determined the inter‐examiner agreement for 304 participants in 2011 and 137 participants in 2014. We calculated overall Pearson correlations and intraclass correlations between the two examiners, and mean outcomes of each examiner for dmft and DMFT. The intraclass correlation coefficients were 0.92 and 0.95, respectively. Differences between the two examiners in mean caries experience were clinically negligible (i.e. at most 0.2 dmft and DMFT).
Data analysis
First, we calculated descriptive statistics for gender, SES, ethnicity, toothbrushing frequency, and dental attendance for the 5‐, 8‐, 11‐, 14‐, 17‐, 20‐, and 23‐yr‐old participants in the sample. Second, we assessed mean caries experience for low‐SES and high‐SES children. We used Student's t‐tests or Mann–Whitney U‐tests to assess statistical significance, depending on the frequency distribution. Crosstabs and chi‐square tests were used for categorical variables. Third, we assessed differences in caries experience according to SES and age, using hurdle modelling. Hurdle models have the advantage of estimating two separate parameters to accommodate many zero counts: one estimate for the dichotomization of zero vs. non‐zero (i.e. caries‐free or not); and one estimate for caries experience in cases of not‐caries‐free. As the count part had a negative binomial distribution, we used a negative binomial hurdle model 30. Hurdle analyses yield ORs for the probability of having any caries and, in the case of those with caries, rate ratios comparing the greater caries experience of low‐SES groups with that of high‐SES groups 30. We made one hurdle model for caries experience in the deciduous teeth and another for caries experience in the permanent teeth. Models were adjusted for age and age‐squared because the relationship between age and caries experience for the count part was not linear. We performed bivariate analyses using spss, version 22.0 (IBM, Armonk, NY, USA), and negative binomial hurdle models in R version 3.3.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Table 1 shows the characteristics of the participants. Of all participants, 46% were male and 39% had a low SES.
Table 1.
Characteristics of participants according to age category
| Variable | Age category (yr) | ||||||
|---|---|---|---|---|---|---|---|
| 5 | 8 | 11 | 14 | 17 | 20 | 23 | |
| n | |||||||
| 302 | 363 | 453 | 619 | 434 | 438 | 413 | |
| Characteristics | |||||||
| Male gender | 54.9 | 54.0 | 49.8 | 46.5 | 43.3 | 39.3 | 35.7 |
| Low socio‐economic status | 40.3 | 38.8 | 40.8 | 41.0 | 38.8 | 34.7 | 36.9 |
| Mother with Dutch ethnicity | 83.1 | 87.8 | 88.9 | 85.0 | 82.4 | 85.3 | 83.7 |
| Oral health behaviour | |||||||
| Toothbrushing twice daily | 73.9 | 85.4 | 82.1 | 80.6 | 71.3 | 73.3 | 72.6 |
| Dental check‐up every 6 months | 78.2 | 87.1 | 89.7 | 84.0 | 82.9 | 67.1 | 65.6 |
Values are given as %.
Table 2 shows caries experience in deciduous and permanent teeth and mean caries experience according to age and SES. For all age groups, except 11‐yr‐old children, the percentage of subjects with caries‐free teeth was lower for those with low SES than for those with high SES (P < 0.05). We observed mean dmft (or DMFT) scores to be higher in low‐SES children than in high‐SES children.
Table 2.
Percentages of Dutch children and young adults with caries experience in deciduous or permanent teeth, and mean caries experience (SD) of them, according to age and SES (2011–2014)
| Variable | Age category (yrs) and tooth type | |||||||
|---|---|---|---|---|---|---|---|---|
| 5a | 8* | 11 | 14 | 17 | 20 | 23 | ||
| n | ||||||||
| 295 | 363 | 448 | 619 | 420 | 438 | 401 | ||
| dmft > 0 or DMFT > 0 (%) | ||||||||
| Low SES | 42.9** | 56.7** | 25.5** | 21.3 | 53.5** | 66.9** | 75.0** | 89.2** |
| High SES | 29.5 | 48.6 | 13.5 | 18.9 | 38.1 | 52.9 | 70.3 | 77.9 |
| Mean caries experience (SD) when dmft > 0 or DMFT > 0 | ||||||||
| Low SES | 3.6 (2.6)** | 4.3 (2.6)** | 1.7 (0.8) | 2.0 (1.2) | 3.3 (2.8)** | 4.1 (3.6) | 5.4 (4.3)** | 6.8 (5.4)** |
| High SES | 2.3 (1.7) | 3.1 (2.1) | 1.8 (0.9) | 1.7 (1.1) | 2.3 (1.6) | 3.3 (2.6) | 4.4 (3.9) | 4.4 (3.2) |
aIn this age group, caries experience in the 20 deciduous teeth only.
*In this age group, caries experience in deciduous and permanent teeth as present.
**Statistically significant different from high SES group (P < 0.05).
Table 3 shows ORs and rate ratios (RRs) for the association of SES and age with caries experience in children aged 5 and 8 yr and children aged 14 yr and older. Children with low‐SES had higher odds of dmft > 0 or DMFT > 0 than children with high SES. Low‐SES children with dmft > 0 or DMFT > 0 had (on average) more caries experience than did children with high SES, teens, and young adults. The odds of dfmt > 0 or DFMT > 0 increased with age. The same held for the mean number of caries experiences. Older children had higher odds of dmft > 0 or DMFT > 0 than did younger children. Older children with dmft > 0 or DMFT > 0 had more caries experience than did younger children. We found no statistically significant interaction of SES with age.
Table 3.
Association of socio‐economic status (SES) and age with caries experience in deciduous and permanent teeth of children (5 and 8 yr of age) and young adults (14 yr of age and older): findings of Hurdle models
| Variable | Deciduous teeth | Permanent teeth† | ||
|---|---|---|---|---|
| OR for dmft > 0 (95% CI) | RR for caries experience (95% CI) | OR for DMFT > 0 (95% CI) | RR for caries experience (95% CI) | |
| SES (Low vs. High) | 1.66 (1.13–2.14)** | 1.55 (1.32–2.08)*** | 1.75 (1.41–2.16)*** | 1.47 (1.29–1.68)*** |
| Centred age (per yr) | 1.15 (1.14–1.51)*** | 1.31 (1.02–1.29)* | 1.22 (1.18–1.27)*** | 1.11 (1.08–1.15)*** |
| Centred age2 † | 1.00 (0.98–1.01) | 0.99 (0.98–1.00)* | ||
| Centred age × SES | 0.93 (0.74–1.14) | 0.92 (0.79–1.09) | 0.99 (0.93–1.06) | 1.01 (0.97–1.04) |
Age squared was significant, meaning that the association between age and caries experience for the count part was not lineair. Therefore age‐squared was used in the count model for a better fit.
*P < 0.05, **P < 0.01, ***P < 0.001.
†We included a quadratic term for centred age to achieve a better fit of the data with the model. RR, rate ratio.
Discussion
At all ages between 5 and 23 yr, children with low SES were less likely to have caries‐free teeth and had, on average, more caries experiences. The absolute difference in caries experience between those with low SES and those with high SES was greatest among 23‐yr‐old subjects. Children with low SES and older children had higher odds for dmft > 0 or DMFT > 0 than children with high SES and younger children. Also, when having caries, children with low SES and older children had, on average, more caries experiences than did children with high SES and younger children, respectively.
We found a difference in caries experience, according to SES, in a health‐care system with full coverage of dental costs for children up to the age of 18 yr. Epidemiological research in the Netherlands reported dental check‐up rates of around 95% for children with low SES and high SES from ages 4 to 16 yr 31. Moreover, in our sample, we also found that most participants in all age groups visited dental professionals yearly. Nevertheless, socio‐economic differences in caries experience existed, which may be explained in several ways: by client‐related factors; by professional‐related factors; or by the organization of care.
With respect to client‐related factors, children from low‐SES groups have been shown to have a greater risk of unfavourable preventive oral health behaviour than their high‐SES counterparts, resulting in the gradient found in caries experience 21, 22, 32, 33, 34. Low‐SES households consume larger quantities of highly processed carbohydrate‐rich foods (because such foods are inexpensive) than do high‐SES households 35. There is a lack of regulation in the production, availability, and pricing of junk food and sugar‐sweetened beverages. Another client‐related factor is that parents with low SES may have lower oral health literacy than parents with high SES and consequently have limited potential to teach their children how to perform optimal dental care. In the matter of professional‐related factors, not all dental professionals may have the skills to promote oral health behaviour effectively among parents with low SES, or to solve the challenges associated with lower levels of oral health literacy 36, 37. Concerning factors related to the organization of care, clear guidelines for oral health promotion and prevention are not yet available. Without guidelines, dental professionals may be insufficiently informed about the recommendations to train parents how to keep their childrens’ teeth healthy and children to keep their own teeth healthy, and the methods to achieve this.
Our findings of differences in caries experience between participants with low SES and high SES are in line with those of studies completed in Switzerland, Brazil, Denmark, Australia, Los Angeles County (USA), Norway, and southern China 4, 5, 6, 7, 8, 10, 11, 38. These findings indicate the socio‐economic inequality in oral health in children in multiple countries, despite different dental‐coverage systems.
In a Dutch system with full dental coverage, we found inequalities in caries experience according to SES in participants from the ages of 5 yr through 23 yr. In Denmark, socio‐economic inequality was still found to exist in dental health, even though almost all children and adolescents attended a free public dental service 6. Moreover, according to darmawikarta et al. 39, among urban Canadian children who had been to a dentist, those in low‐income families were more likely to have dental caries. Findings from a study conducted in North Carolina showed that low‐income children with extended dental coverage had less dental caries experience than children in Medicaid 40. These findings indicate that although free dental services are important for children, socio‐economic differences in caries experience may persist nonetheless (Fig. 1).
Figure 1.
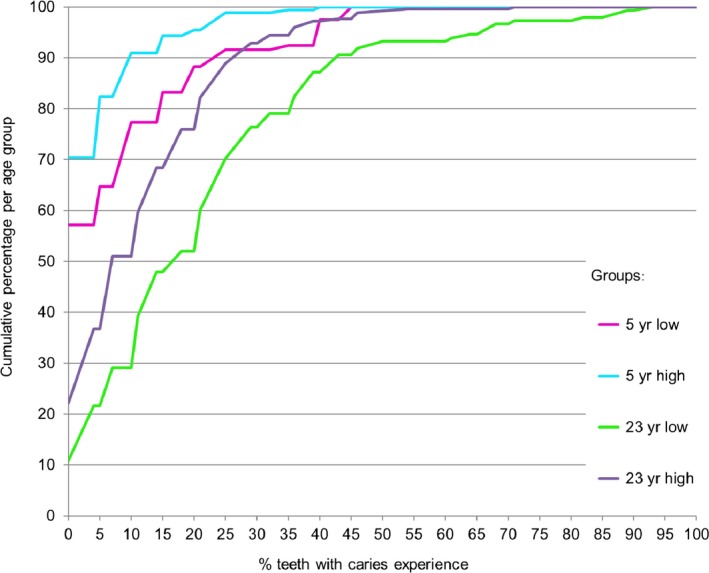
Cumulative frequency distribution of the percentage of teeth with caries. One‐hundred percent teeth with caries experience is equivalent to 20 teeth with caries experience for age 5 yr, and 28 teeth with caries experience for age 23 yr.
The findings of this study should be considered in light of its strengths and limitations. The strengths include the large sample of children and young adults shown to be representative of the Dutch population of 5‐ to 23‐yr‐old subjects with respect to background variables 26, 41. Moreover, the dental examinations were carried out by trained professionals with satisfactory interexaminer agreement. There are also some limitations. Given the low response rate of 23%, selection bias may have affected our findings. In our study, the inclusion of participants stopped when the required number was reached, slightly increasing non‐response rates but less likely causing bias. Non‐response analyses indicated why people were unwilling to participate. The most frequent reasons were lack of interest, lack of time, and anxiety, with (in particular) the last item in this list potentially resulting in bias. Moreover, selection bias is less likely as the demographic characteristics of the sample were very similar to those of the general population. A second limitation may be that we assessed SES only according to educational level and not by using other measures, such as income or occupation. Asking about educational level has the advantage of a high response, particularly in contrast to asking about income; moreover, in the Netherlands, educational level has been found to be the most sensitive indicator of SES 42.
Our finding, of large absolute differences according to SES in all age groups in a country with a system of full dental coverage, suggests a need for additional preventive efforts. The disease of dental caries is preventable 43. One way to prevent it is to change unfavourable oral health behaviours, such as toothbrushing less than twice daily and frequent consumption of cariogenic food and drinks. Interventions to reach children to prevent caries experience may include enhancing oral health literacy, as well as improving parental knowledge, skills, and self‐efficacy in relation to preventive oral health behaviour, both early in life and thereafter.
In this study, differences in mean caries experience between children with low SES and high SES were already present in 5‐yr‐old participants, despite full dental coverage. One could hypothesize that children receive preventive dental care too late. To minimize socio‐economic differences, community‐based interventions aimed at improving the oral health of children and young adults should start early in life – as early as the age of 6 months when the first tooth erupts 44, 45. To reach all children, better integration of preventive dental care in well‐child care, paediatric primary care, and elementary school programmes could improve caries prevention.
Another challenge to decrease the socio‐economic gap is the growing problem of a higher intake of highly processed foods with added sugars in low‐SES households, mainly because these low‐quality foods are more affordable 35. The cariogenic and obesogenic environment is especially a problem in areas of high deprivation. Better regulation policies for production, pricing, and provision of highly processed foods with fermentable carbohydrates are needed. Furthermore, dental health professionals, well‐child care doctors and nurses, and general practitioners should collaborate at community level to motivate parents to favour healthy food choices. Such community‐level interventions are, for instance, integrated preventive dental care performed by dental hygienists at well‐child clinics or routine referral of children to a dental clinic by a well‐child clinic paediatrician. Both interventions are now researched for (cost‐)effectiveness in the Netherlands. Dental professionals participating in these interventions follow the Non‐Operative Caries Treatment Program while caring for children's teeth 46, 47.
In conclusion, low SES is associated with a lower prevalence of caries‐free teeth and more caries experience at the ages of 5–23 yr, even in a system with full dental coverage. The presence of additional socio‐economic differences indicate that factors other than access contribute to these differences. Low‐SES children may be at a higher risk of unfavourable preventive oral health behaviour than their high‐SES counterparts. Dental professionals may not have the skills to promote oral health behaviour effectively, often with challenges for lower levels of oral health literacy. Furthermore, there is a dearth of clear guidelines for preventive dental care in children. Community‐based interventions to decrease the socio‐economic differences and to improve oral health may include enhancing oral health literacy and improving parental knowledge, skills, and self‐efficacy in relation to preventive oral‐health behaviour. Better collaboration between paediatric primary care, elementary schools, and preventive dental care may help motivate parents to brush their child's teeth twice a day, to let their child drink water, and to limit their child's consumption of highly processed carbohydrate‐rich foods. Moreover, we need policy measures to curtail, at community level, the increasing availability and consumption of highly processed, carbohydrate‐rich foods, which particularly affects low‐SES families. Further research is needed on the effectiveness of such interventions and on the degree to which they reach low‐SES children. This may reduce child dental morbidity in a major way.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgements
We wish to thank Dr. Paula van Dommelen for her contribution to the statistical analyses, Ineke van Kempen for her skilled assistance during the data collection and Dr. Erik Vermaire for his useful suggestions.
Verlinden DA, Reijneveld SA, Lanting CI, van Wouwe JP, Schuller AA. Socio‐economic inequality in oral health in childhood to young adulthood, despite full dental coverage. Eur J Oral Sci 2019; 127: 248–253. © 2019 Eur J Oral Sci
References
- 1. Cheng TL, Emmanuel MA, Levy DJ, Jenkins RR. Child health disparities: what can a clinician do? Pediatrics 2015; 136: 961–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Poulton R, Caspi A, Milne BJ, Thomson WM, Taylor A, Sears MR, Moffitt TE. Association between children's experience of socioeconomic disadvantage and adult health: a life course study. Lancet 2002; 360: 1640–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen E, Matthews KA, Boyce WT. Socioeconomic differences in children's health: how and why do these relationships change with age? Psychol Bull 2002; 128: 295–329. [DOI] [PubMed] [Google Scholar]
- 4. Baggio S, Abarca M, Bodenmann P, Gehri M, Madrid C. Early childhood caries in Switzerland: a marker of social inequalities. BMC Oral Health 2015; 15: 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Baldani MH, Mendes YBE, Lawder JAC, De Lara API, Rodrigues MMAS, Antunes JLF. Inequalities in dental services utilization among Brazilian low‐income children: the role of individual determinants. J Public Health Dent 2011; 71: 46–53. [DOI] [PubMed] [Google Scholar]
- 6. Christensen LB, Twetman S, Sundby A. Oral health in children and adolescents with different socio‐cultural and socio‐economic backgrounds. Acta Odontol Scand 2010; 68: 34–42. [DOI] [PubMed] [Google Scholar]
- 7. Kilpatrick NM, Neumann A, Lucas N, Chapman J, Nicholson JM. Oral health inequalities in a national sample of Australian children aged 2‐3 and 6‐7 years. Aust Dent J 2012; 57: 38–44. [DOI] [PubMed] [Google Scholar]
- 8. Mulligan R, Seirawan H, Faust S, Barzaga C. Dental caries in underprivileged children of Los Angeles. J Health Care Poor Underserved 2011; 22: 648–662. [DOI] [PubMed] [Google Scholar]
- 9. Schwendicke F, Dӧrfer CE, Schlattmann P, Foster Page L, Thomson WM, Paris S. Socioeconomic inequality and caries: a systematic review and meta‐analysis. J Dental Res 2015; 94: 10–18. [DOI] [PubMed] [Google Scholar]
- 10. Wigen TI, Wang NJ. Caries and background factors in Norwegian and immigrant 5‐year‐old children. Commun Dent Epidemiol 2010; 38: 19–28. [DOI] [PubMed] [Google Scholar]
- 11. Zhou Y, Lin HC, Lo ECM, Wong MCM. Risk indicators for early childhood caries in 2‐year‐old children in southern China. Aust Dent J 2011; 56: 33–39. [DOI] [PubMed] [Google Scholar]
- 12. Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century—the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 2003; 31: 3–23. [DOI] [PubMed] [Google Scholar]
- 13. Szilagyi PG. Oral health in children: a pediatric health priority. Acad Pediatr 2009; 9: 372–373. [DOI] [PubMed] [Google Scholar]
- 14. Innes NPT, Frencken JE, Bjørndal L, Maltz M, Manton D, Ricketts SD, Van Landuyt K, Banerjee A, Campus G, Doméjean S, Fontana M, Leal S, Lo E, Machiulskiene V, Schulte A, Splieth C, Zandona A, Schwendicke F. Managing carious lesions: consensus recommendations on terminology. Adv Dent Res 2016; 28: 49–57. [DOI] [PubMed] [Google Scholar]
- 15. Jackson SL, Vann WF Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children's school attendance and performance. Am J Public Health 2011; 101: 1900–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yost J, Li Y. Promoting oral health from birth through childhood: prevention of early childhood caries. MCN Am J Matern Child Nurs 2008; 33: 17–23. [DOI] [PubMed] [Google Scholar]
- 17. Dusseldorp E, Kamphuis M, Schuller AA. Impact of lifestyle factors on caries experience in three different age groups: 9, 15, and 21‐year olds. Community Dent Oral Epidemiol 2015; 43: 9–16. [DOI] [PubMed] [Google Scholar]
- 18. Marinho VCC, Higgins JPT, Logan S, Sheiham A. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2003; 1: CD002278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Petersen PE. Sociobehavioural risk factors in dental caries ‐ international perspectives. Community Dent Oral Epidemiol 2005; 33: 274–279. [DOI] [PubMed] [Google Scholar]
- 20. Mejáre I, Axelsson S, Dahlén G, Espelid I, Norlund A, Tranaeus S, Twetman S. Caries risk assessment. A systematic review. Acta Odontol Scand 2014; 72: 81–91. [DOI] [PubMed] [Google Scholar]
- 21. Bast LS, Nordahl H, Christensen LB, Holstein BE. Tooth brushing among 11‐ to 15‐year‐olds in Denmark: combined effect of social class and migrant status. Community Dent Health 2015; 32: 51–55. [PubMed] [Google Scholar]
- 22. Holstein BE, Bast LS, Brixval CS, Damsgaard MT. Trends in social inequality in tooth brushing among adolescents: 1991‐2014. Caries Res 2015; 49: 595–599. [DOI] [PubMed] [Google Scholar]
- 23. Isong I, Dantas L, Gerard M, Kuhlthau K. Oral health disparities and unmet dental needs among preschool children in Chelsea, MA: exploring mechanisms, defining solutions. J Oral Hyg Health 2014; 2: 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Geboers B, Reijneveld SA, Koot JAR, De Winter AF. Moving towards a comprehensive approach for health literacy interventions: the development of a health literacy intervention model. Int J Environ Res Public Health 2018; 15: 1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Central Bureau For Statistics . Demographic data per city (2014) Statistics Netherlands, StatLine. http://statline.cbs.nl/Statweb/publication/?DM=SLNL&PA=70072ned&D1=0-2,21-27,3341,88&D2=0,72,154,269,329&D3=16,19&HDR=T&STB=G1,G2&VW=T. Accessed 17 September 2018.
- 26. Schuller AA, Van Dommelen P, Poorterman JHG. Trends in oral health in young people in the Netherlands over the past 20 years: a study in a changing context. Community Dent Oral Epidemiol 2014a; 42: 178–184. [DOI] [PubMed] [Google Scholar]
- 27. Schuller AA, Van Buuren S. Estimation of caries experience by multiple imputation and direct standardization. Caries Res 2014b; 48: 91–95. [DOI] [PubMed] [Google Scholar]
- 28. UNESCO . International Standard Classification of Education ISCED 2011. Montreal: UNESCO Institute for Statistics, 2012. [Google Scholar]
- 29. Klein H, Palmer CE, Knutson JW. Studies on dental caries. 1. Dental status and dental needs of elementary schoolchildren. Public Health Rep 1938; 53: 751–765. [Google Scholar]
- 30. Hofstetter H, Dusseldorp E, Zeileis A, Schuller AA. Modeling Caries experience: advantages of the use of the Hurdle model. Caries Res 2016; 50: 517–526. [DOI] [PubMed] [Google Scholar]
- 31. Central Bureau For Statistics . The use of dental services. Statistics Netherlands, StatLine.http://statline.cbs.nl/Statweb/publication/?DM=SLNL&PA=83005ned&D1=67-69&D2=0-6&D3=0&D4=2-3&HDR=G2,G3,T&STB=G1&VW=T. Accessed 17 September 2018.
- 32. Do LG, Ha DH, Spencer AJ. Factors attributable for the prevalence of dental caries in Queensland children. Community Dent Oral Epidemiol 2015; 43: 397–405. [DOI] [PubMed] [Google Scholar]
- 33. Duijster D, De Jong‐Lenters M, De Ruiter C, Thijssen J, Van Loveren C, Verrips E. Parental and family‐related influences on dental caries in children of Dutch, Moroccan and Turkish origin. Community Dent Oral Epidemiol 2015; 43: 152–162. [DOI] [PubMed] [Google Scholar]
- 34. Levin KA, Currie C. Adolescent toothbrushing and the home environment: sociodemographic factors, family relationships, and mealtime routines and disorganization. Community Dent Oral Epidemiol 2010; 38: 10–18. [DOI] [PubMed] [Google Scholar]
- 35. Otero G, Pechlaner G, Gürcan EC, Liberman G. The neoliberal diet and inequality in the United States. Soc Sci Med 2015; 142: 47–55. [DOI] [PubMed] [Google Scholar]
- 36. Horowitz AM, Kleinman DV. Oral health literacy: a pathway to reducing oral health disparities in Maryland. J Public Health Dent 2012; 72: 26–30. [DOI] [PubMed] [Google Scholar]
- 37. Macek MD, Atchison K, Chen H, Wells W, Haynes D, Parker RM, Azzo S. Oral health conceptual knowledge and its relationships with oral health outcomes: findings from a Multi‐site Health Literacy Study. Community Dent Oral Epidemiol 2017; 45: 323–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Capurro DA, Iafolla T, Kingman A, Chattopadhyay A, Garcia I. Trends in income‐related inequality in untreated caries among children in the United States: findings from NHANES I, NHANES III, and NHANES 1999‐2004. Community Dent Oral Epidemiol 2015; 43: 500–510. [DOI] [PubMed] [Google Scholar]
- 39. Darmawikarta D, Chen Y, Carsley S, Birken CS, Parkin PC, Schroth RJ, Maguire JL, The Target Kids! Collaboration . Factors associated with dental care utilization in early childhood. Pediatrics 2014; 133: 1594–1600. [DOI] [PubMed] [Google Scholar]
- 40. Brickhouse TH, Rozier RG, Slade GD. Effects of enrollment in Medicaid versus the State Children's health insurance program on kindergarten children's untreated dental caries. Am J Public Health 2008; 98: 876–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kalsbeek H, Poorterman JH, Eijkman MA, Verrips GH. Dental care for young people insured by health insurance fund 1. Prevalence and treatment of dental caries between 1987 and 1999. Ned Tijdschr Tandheelkd 2002; 109: 250–254. [PubMed] [Google Scholar]
- 42. Vart P, Gansevoort RT, Coresh J, Reijneveld SA, Bültmann U. Socioeconomic measures and CKD in the United States and the Netherlands. Clin J Am Soc Nephrol 2013; 8: 1685–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Featherstone JD. The continuum of dental caries – evidence for a dynamic disease process. J Dent Res 2004; 83: 39–42. [DOI] [PubMed] [Google Scholar]
- 44. Chen E, Martin AD, Matthews KA. Trajectories of socioeconomic status across children's lifetimes predict health. Pediatrics 2007; 120: 297–303. [DOI] [PubMed] [Google Scholar]
- 45. Lioret S, Betoko A, Forhan A, Charles MA, Heude B, De Lauzon‐Geuillain B, Eden Mother‐Child Cohort Study Group . Dietary patterns track from infancy to preschool age: cross‐sectional and longitudinal perspectives. J Nutr 2015; 145: 775–782. [DOI] [PubMed] [Google Scholar]
- 46. Ekstrand KR, Christiansen MEC. Outcomes of a non‐operative caries treatment programme for children and adolescents. Caries Res 2005; 39: 455–467. [DOI] [PubMed] [Google Scholar]
- 47. Vermaire JH, Poorterman JHG, van Herwijnen L, van Loveren C. A three‐year randomized controlled trial in 6‐year‐old children on caries‐preventive strategies in a general dental practice in the Netherlands. Caries Res 2014; 48: 524–533. [DOI] [PubMed] [Google Scholar]


