Abstract
In Mozambique, about two thirds of children 6–59 months of age are affected by vitamin A deficiency and anaemia. The objective of this case study is to provide programme considerations for planning, implementing, monitoring, and evaluating vitamin A and iron deficiency interventions within the context of lessons learned to date for vitamin A supplementation, micronutrient powders (MNPs), and food‐based strategies. For 15 years, the Mozambique Ministry of Health implemented twice‐yearly vitamin A supplementation through both campaigns and routine health services. Yet coverage in 2017 (55%) was not much higher than in 2003 (44%). Reaching every district/reaching every child, a strategy adapted from the field of immunization, was used to achieve equitable coverage of vitamin A and for microplanning of outreach services in health facilities, with support from the Maternal and Child Survival Program. In Mozambique, a free or subsidized distribution model for MNPs has been rolled out, yet integration of MNPs into infant and young child feeding programming (i.e., cooking demonstrations) is needed to reinforce “the who, what, and why” of MNPs through culturally sensitive behaviour change communication. Food‐based strategies to promote dietary diversity, such as through complementary feeding recipes, are also critical. To harmonize efforts, the Mozambique government should consider the development of a national strategy for the prevention and control of micronutrient malnutrition, with clear monitoring and evaluation targets. Ongoing monitoring of the prevalence of micronutrient deficiencies and coverage of implemented micronutrient interventions is needed to make evidence‐based decisions to drive nutrition–health programming.
Keywords: complementary feeding, iron, micronutrient deficiencies, micronutrient supplementation, Mozambique, vitamin A
Key messages.
In Mozambique, the success of micronutrient programming to address vitamin A and iron deficiency will be largely determined by the rollout of existing guidelines; implementation of demand generation activities, particularly through community health actors; and adequate planning and forecasting of resources and supplies to meet needs in an equitable manner.
Ongoing monitoring of the prevalence of micronutrient deficiencies and the coverage of micronutrient interventions is needed in the face of multiple interventions implemented concurrently to address vitamin A and iron deficiency for the same target groups.
To ensure coordinated, harmonized, and cost‐effective efforts, the Mozambique government should consider the development of a cohesive national strategy for the prevention and control of micronutrient malnutrition.
1. BACKGROUND
Nearly 70% of Mozambicans reside in rural areas and are dependent on agriculture for subsistence, with nearly half of the country's population suffering from absolute poverty (National Institute of Statistics [INE; Mozambique], 2017; Ministry of Agriculture and Food Security [Mozambique], 2016; Ministry of Economy and Finance [Mozambique], 2016). Chronic food insecurity affects one quarter of households and stems from limited food production and access due to a prolonged civil war (1977–1992), political strife, and an economic recession (2015; Carrilho, Abbas, Júnior, Chidassicua, & Mosca, 2016; Technical Secretariat for Food Security and Nutrition [SETSAN; Mozambique], 2013; Ministry of Agriculture and Food Security [Mozambique], 2014; African Development Bank Group, 2018). In Mozambique, the prevalence of stunting or chronic malnutrition is 43% for children less than 5 years of age (Ministry of Health [MISAU], INE, & ICF International [ICFI], 2013). The Mozambican diet is largely characterized by low amounts of animal source proteins, fresh fruits and vegetables, and dairy products, as cassava, maize, sorghum, millet, and rice are staple foods (FAO, 2011). Thus, micronutrient deficiency rates are feared to be high. Evidence of these deficiencies from the most recent national survey (2002) determined that low concentration of serum retinol affects 69% of children 6–59 months (MISAU, 2006). Rates of child anaemia have remained high at 63.8%, affecting primarily children 6–23 months in poorer households (MISAU, INE, & ICFI, 2015). Although these two indicators are also influenced by infection, it is likely that low intake of micronutrients is a main cause of nutrient deficiency and anaemia.
2. OBJECTIVE
The objective of this case study is to provide programme considerations for planning, implementing, monitoring, and evaluating vitamin A and iron deficiency interventions targeting children under 5 within the context of complementary multisectoral interventions and lessons learned to date.
3. METHODS
The information presented in this case study was drawn from published and unpublished government documents and programme reports from Mozambique and from global literature. In addition, health information system data, evaluation reports from international non‐governmental organizations, and expert consultations are presented.
4. NORMS, POLICIES, AND STRATEGIES TO REDUCE MICRONUTRIENT DEFICIENCIES WITHIN INTEGRATED HEALTH PROGRAMMING IN MOZAMBIQUE
For the past two decades, addressing micronutrient deficiencies has been one of the top priorities of public health programmes targeting women of reproductive age and children under 5 in Mozambique. Micronutrient interventions are integrated in key guidance documents for maternal and child health programmes, including the Integrated Plan for the Achievement of the Millennium Development Goals 4 & 5 2009–2012 (and subsequently extended to 2017; MISAU, 2009); the Guidelines for Integrated Management of Childhood Illnesses (MISAU, 2014); and the Well‐Child/At‐Risk Child Clinical Norms (MISAU, 2011). The Ministry of Health (MOH) Nutrition Department developed a Guide for Health Professionals on Supplementation with Micronutrients in Mozambique (Ministry of Health [MISAU] (Mozambique), 2005) and the Basic Nutrition Package (MISAU, 2007), which delineate guidelines for the implementation of vitamin A and iron‐folic acid supplementation, deworming, and promotion of micronutrient‐rich foods. Furthermore, the Health Sector Strategic Plan 2014–2019 integrates essential nutrition actions for implementation through the health sector, including interventions to address micronutrient deficiencies.
In 2010, recognizing the high child stunting rates and its effect on the country's economic development, the Government of Mozambique developed the Multisectoral Action Plan for the Reduction of Chronic Malnutrition 2011–2014 (2020; Plano de Acção Multisectorial para a Redução da Desnutrição Crónica [PAMRDC]), to reduce the prevalence of chronic malnutrition to 20% by 2020 (Government of the Republic of Mozambique, 2010). As delineated in the PAMRDC, micronutrient delivery interventions were introduced in the country through point‐of‐use food fortification (micronutrient powders) or industrial food fortification (including wheat and maize flour with iron and vegetable oil and sugar with vitamin A).
5. CURRENT PROGRESS AND CHALLENGES IN MICRONUTRIENT REDUCTION EFFORTS
5.1. Vitamin A supplementation
In 1999, high dose vitamin A supplementation (VAS) was employed as a short‐ to medium‐term strategy to reduce vitamin A deficiency among children 6–59 months of age in Mozambique (Aguayo, Khan, Ismael, & Meershoek, 2005). The delivery model for VAS has undergone several iterations over the past 19 years, with the purpose of reducing cost but keeping the good coverage of national campaigns (defined as 95% or above). Two rounds of VAS campaigns were estimated to cost US$8 million per year in 2015, 2.5% of the current overall annual health budget (United Nations Children's Fund [UNICEF], 2017). Vitamin A supplements were initially delivered through campaigns as the sole platform and later oscillated between routine services and campaigns for 13 years (see Figure 1).
Figure 1.
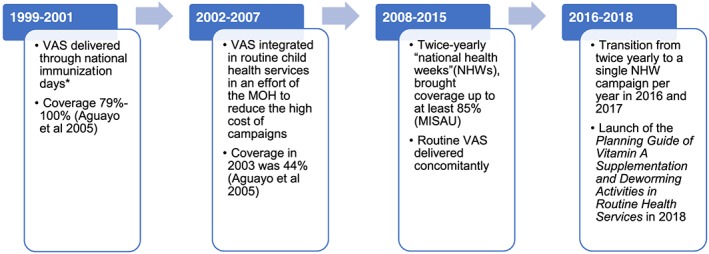
Delivery model of vitamin A supplementation (VAS) in Mozambique, 1999–2018 (source: Aguayo et al., 2005). MOH: Ministry of Health, *National immunization days were polio eradication campaigns
Given the priority to strengthen integrated health programming, national health week campaigns are viewed to detract from routine systems. Investment in an integrated package of schedulable, population‐based preventative health services for all children has the potential to be more sustainable in the long term. Lack of certainty about funding for national health weeks in light of decreasing external funds due to political strife has increased the urgency to make a transition from campaigns to strengthened routine VAS services integrated in efficient primary healthcare delivery platforms.
The Maternal and Child Survival Program (MCSP) is a global, U.S. Agency for International Development funded programme, with a focus on supporting reproductive, maternal, newborn, and child health interventions to prevent maternal and child mortality, in 25 low‐ and middle‐income priority countries (MCSP, 2018). In Mozambique, MCSP has worked to scale up preventative and curative nutrition interventions at the facility and community level for the past 3 years, in Nampula and Sofala provinces. MCSP supported the MOH in the implementation of the transition from VAS campaigns to routine child health services in 2016. This allowed MCSP a unique opportunity to support both campaign modalities (one round in 2017) and routine modalities, through all its distribution channels as well as to work with the MOH to shape new guides, plans, implementation, and monitoring and evaluation tools to strengthen VAS routine distribution channels, taking into account field experience. In total, MCSP, with MOH, reached 2,972,138 children 6–59 months of age with nutrition interventions at health facility and community levels (i.e., behaviour change communication activities, supplementation with vitamin A and micronutrient powders (MNPs), nutrition screening and referral, and treatment of acute malnutrition), and 2,190,319 were reached with at least one dose of vitamin A from October 2016 to June 2018.
Currently, routine VAS integrated in child health services is the main platform the national health system uses for delivery and includes varied distribution channels, all of which are supported by MCSP given its integrated nature that extends along the continuum of care. Fixed‐site (i.e., health facility) distribution is integrated with routine well‐child visits (i.e., growth monitoring and promotion and immunization services). Mobile‐site distribution occurs via integrated health facility teams, “mobile brigades,” which deliver VAS, deworming, immunization, family planning, and other interventions to the community—especially to hard‐to‐reach populations). Community health workers (CHWs), such as polyvalent elemental agents (Agente Polivante Elementar, who are the government healthcare system's paid CHWs) and community health activists (who are non‐governmental organizations‐implemented projects' CHWs, who are unpaid), also deliver vitamin A supplements to children in a radius of 8 to 25 km of the health facility, in addition to the integrated management of childhood illnesses, acute malnutrition screening, and deworming.
Despite Mozambique's 15 years of experience in implementing VAS in routine health services, the coverage in 2017 (55%) was not much higher than that in 2003 (44%; see Table 1 for coverage trends over the last 3 years). To address some of the challenges to routine VAS (see Box 1), UNICEF, Hellen Keller International, and MCSP provided technical assistance to the MOH to develop a Planning Guide of Vitamin A Supplementation and Deworming Activities in Routine Health Services (MISAU, 2017b). The guide is focused on generating demand for routine VAS, for which the MOH developed a separate social and behaviour change communication (SBCC) plan (MISAU & Helen Keller International Mozambique, 2018), and implementing outreach services targeting hard‐to‐reach populations (~60% of the total population), using the MOH Reaching Every District and Community (RED/REC) Guide.
Table 1.
Annual vitamin A coverage through routine child health services versus national health weeks 2015–2017
Box 1 Major factors contributing to low coverage of vitamin A supplementation in routine child health services.
1. Insufficient demand for vitamin A—Caregivers do not seek preventive health services once child completes vaccination schedule at 9 months of age
2. Low capacity to adequately register, aggregate, report, and analyse routine vitamin A data from all delivery platforms
3. Localized stock‐outs of supplements due to the use of nationwide coefficients to forecast needs per district and lack of microplanning for requisition of vitamin A at service provider level
4. Missed opportunities for vitamin A supplementation during at‐risk child and sick‐child visits at the health facility
5. Large vitamin A supplementation campaigns may demotivate health workers to provide vitamin A during routine services
6. Low‐quality microplanning and lack of means to operationalize outreach activities for hard‐to‐reach children
The reaching every district (RED) (and later reaching every child [REC]) strategy was designed to strengthen immunization systems by improving planning, management of available resources, and service delivery and monitoring to sustainably and equitably increase immunization coverage rates, based on community needs. Introduced in 2002 in the African continent, RED/REC has demonstrated impact in improving immunization coverage (DPT3 coverage in Africa increased from 57% in 2000 to 80% in 2014) and the frequency of supervision visits, and increasing the number of outreach sessions conducted at the district level (World Health Organization [WHO], 2017). As immunization systems deliver vaccines at relatively high coverage rates often in primary healthcare contexts, RED has come to be recognized as a platform for delivering multiple interventions to women and children of vulnerable populations at the same time. Moving from vertical programming to integrated planning, monitoring, logistics, and resource mobilization efforts can increase efficiency and reduce costs through maximizing the same contact point with combined services, including immunization, VAS, deworming, health promotion, and nutrition screening, among others (WHO, 2017). MCSP supported the MOH to provide equitable coverage of maternal, newborn and child health (MNCH) services through training of 146 health workers in RED/REC, for adequate microplanning of outreach services in all supported health facilities in MCSP catchment areas. The Mozambique RED/REC Guide is currently under review by the MOH with support from MCSP, WHO Mozambique, and UNICEF Mozambique to reflect the latest global WHO guidelines.
It is anticipated that the monitoring of VAS coverage will improve through recently developed well‐child and sick‐child consultation registers, which have one VAS indicator disaggregated by age group (i.e., one dose VAS coverage 6–11 months and one dose VAS coverage 12–59 months). MCSP provided technical assistance to the MOH in piloting and finalizing the registers and will support the MOH in the national roll‐out from November 2018. The child health registers are aligned with the District Health Information System platform and will be used in both fixed‐ and mobile‐site vitamin A supplement distribution. Although the registers will eliminate vertical and incomplete reporting through daily and monthly VAS tally sheets, gaps still exist in guidance to calculate coverage and particularly second dose VAS coverage. Current VAS coverage indicator definition in the new child health registers uses the number of eligible children attending well‐child visits or mobile brigades as the denominator, as opposed to the estimate of the total eligible population in a given health area. MCSP supported the MOH in designing district‐specific population coefficients that allow the MOH to estimate, at all levels, who the target group is, so that needs are met equitably. It is recommended that the MOH guides sub‐national levels on the use of these coefficients to calculate the denominator for VAS coverage monitoring. Furthermore, guidance on tracking two‐dose coverage from this indicator, consistent with the latest guidance from UNICEF, has failed to be incorporated in the registers' instructions of use prior to printing for roll‐out (UNICEF, 2018). Hence, it will be of key importance to disseminate this guidance during roll‐out training events. Finally, a gap persists on the integration of CHW's VAS data in the national District Health Information System platform, which merits more attention from the MOH.
5.2. Use of micronutrient powders to address iron‐deficiency anaemia
Iron‐deficiency anaemia is purported as a primary cause of years lived with disability among children (Nyhus Dhillon et al., 2017). Given the high prevalence of anaemia in young children, the Mozambique Government adopted WHO's guidelines on the use of MNPs every 6 months to be consumed together with foods by infants and children 6–23 months of age (World Health Organization [WHO], 2011). In 2015, the MOH elaborated on WHO guidelines and developed a draft Strategy for the Implementation of Home Fortification with Multiple Micronutrient Powders in Mozambique in 2015, with a two‐pronged distribution strategy: (a) free distribution of MNPs through routine health services for children 6–23 months of age with possible extension to 24–59 months of age depending on supplies and (b) commercial distribution of MNPs to children 6–59 months of age, either subsidized or non‐subsidized.
The use of MNPs integrated in health services in Mozambique has been—and remains—fully dependent on external funding (UNICEF, World Bank, and the Dutch Government) since its introduction in the country in 2015. Commodities have only been available through pilot short‐term projects, for limited durations of time and in selected provinces and districts (Table 2). Scaling‐up MNPs requires targeting the intervention to specific segments of the population (i.e., by socio‐economic status and geographic areas), according to evidence‐based needs, alongside building public–private partnerships (i.e., subsidized vs. free distribution) to ensure programme costs are not beyond that of VAS campaigns (SPRING, 2018).
Table 2.
Anaemia prevalence in children 6–59 months and reported distribution of MNP integrated in health services, by province
| Province | Anaemia prevalence children 6–59 months (MISAU, INE, & ICFI, 2015) | Implementation partner | Delivery mechanism | Timeline | Beneficiaries reached |
|---|---|---|---|---|---|
| Niassa | 59% | Health services delivery project/community nutrition (HSDP/Nut), through ADPP Mozambique and Ariel Glaser Foundation | Free distribution through community health activists and in well‐child consultations at the health facility | 2015–2017 | 158,554/333,788 (48%)a |
| Cabo Delgado | 73% | HSDP/Nut, through Aga Khan Foundation | Free distribution through community health activists and in well‐child consultations at the health facility | 2015–2017 | 195,392/188,709 (104%)b |
| Nampula | 68% |
HSDP/Nut, through Save the Children
MCSP |
Free distribution through community health activists and in well‐child consultations at the health facility Free distribution in well‐child consultations at the health facility |
2015–2017
2016–2018 |
726,494/185,913 (391%)c
120,891 (MCSP, 2018) |
| Zambézia | 77% | UNICEF | Free distribution in well‐child consultations at the health facility | 2016–2017 | 308,989 (MISAU, 2017c) |
| Tete | 60% | UNICEF | Free distribution in well‐child consultations at the health facility | 2016–2017 | 122,453 (MISAU, 2017c) |
| Manica | 59% | UNICEF | Free distribution in well‐child consultation at the health facility | 2016 | 110,952 (MISAU, 2017c) |
| Sofala | 64% |
UNICEF, MCSP GAIN, through PSI and Save the Children |
Free distribution in well‐child consultation at the health facility Subsidized commercial distribution via vouchers distributed by health facility workers and community health workers redeemable at “Troca Aki” vendors |
2016 | 58,537 (MISAU, 2017c) |
| Gaza | 59% | HKI Mozambique | Free distribution in well‐child consultations | 2016–2017 |
54,892 (MISAU, 2017c) |
Note. HKI: Helen Keller International; MCSP: Maternal and Child Survival Program; MNP: micronutrient powder; UNICEF: United Nations Children's Fund.
Final report of the nutrition project in Niassa Province, implemented by ADDP and Ariel Glaiser.
Final report of the Health Service Delivery Project—Community‐based Nutrition Project Cabo Delgado Province.
Health Services Delivery Project—Community‐based Nutrition Project Nampula Province.
Some of the lessons learned from implementation research on MNPs are presented in Box 2 and Box 3, corresponding to free distribution (direct product provision to caregiver) and subsidized commercial distribution (provision of voucher to caregiver and redemption at designated vending agencies), respectively. Irrespective of the distribution model, designing a culture‐sensitive social behaviour change strategy on infant and young child feeding (IYCF) programming, which integrates MNPs, is key to promote acceptance of, consumption of, and adherence to the product. This should include carrying out cooking demonstrations to improve IYCF practices and correct use of MNPs (“what, why, and how”); interpersonal communication delivered by CHWs; and promotion through mass media channels to reinforce the value of messages around MNPs (“the who, what, and why”), with involvement of influential community leaders. Furthermore, strengthening the supply chain and monitoring systems is critical for the implementation of this intervention through integrated nutrition–child health programming.
Box 2 Lessons learned from the implementation of free distribution of multiple micronutrient powders integrated in child health services.
1. Carefully planned social and behaviour change communication is key to prevent distrust and associations of free micronutrient powder (MNP) distribution with negative effects.
2. Community leadership involvement in cooking demonstrations and tastings is a powerful tool to build trust and generate demand for MNP
3. MNP promotion efforts should take into account the seasonal variations in food availability so that caregivers understand that any semi‐solid food is a good vehicle for mixing the MNP
4. Delivery by community health workers versus health facility workers allows time for appropriate infant and young child feeding counselling
5. Partner support for MNP supply chain is needed to prevent frequent stock‐outs
6. Monitoring and evaluation training needs to be strengthened to allow appropriate monitoring of delivery of second and third doses of MNP
Box 3 Lessons learned from implementation of subsidized commercial distribution of multiple micronutrient powders integrated in child health servicesa,b .
• The use of micronutrient powders (MNP) saw an increase in continued breastfeeding rates from 60% to 76% and in minimum acceptable diet from 10% to 15% in one of the three implementation sites.
• Caregivers' adherence to VitaMais is highly related to knowledge, so interpersonal communication coupled with promotion through radio and television has the potential to enhance adherence.
• Cooking demonstrations constitute a powerful tool to increase acceptance and consumption of MNPs.
• Although the voucher system is deemed to be a sound mechanism to provide caregivers with VitaMais, its effectiveness relies on clear guidance on the redemption process to both caregivers and “Troca Aki” vendors. Removing the need for vouchers significantly increased coverage.
• Investments must be made in adequately training and equipping health facility personnel and community health workers with the required skills to support and guide caregivers on the use of MNPs, responsive feeding, and problem solving if the child rejects home‐fortified foods.
a MISAU. Experience with the distribution of multi‐micronutrient powders in Mozambique. Presentation for the Roundtable “Sustainability of Home Food Fortification Programs”. 10 August 2016.
b Communication with Carolyn O'Donnel, Nutrition Advisor, Save the Children US. March 2018.
The MOH and partners, including MCSP, have made strides in integrating the use of MNPs in routine child health services. This includes revising the child health card—which is provided to all caregivers—and the well‐child consultation registers to record and monitor the first three doses of MNP provided to children 6–23 months; developing and rolling out a package of SBCC materials for the promotion of MNPs to complement other IYCF counselling materials in the provinces where MNPs are being used (including Nampula and Sofala with MCSP's support); and revising guidelines and norms—including the basic nutrition package and the well‐child/at risk‐child consultation norms—to integrate MNPs.
5.3. Promotion of dietary diversity through local foods
In addition to micronutrient supplementation, investment in food‐based strategies for improving IYCF practices is critical to meet PAMRDC targets. According to the 2011 Demographic and Health Survey, only 14.5% of Mozambican children 6–23 months meet the criteria for minimum acceptable diet (MISAU et al., 2013).
Since 1994, promotion of dietary diversity for Mozambican children has been centred on “papas enriquecidas” or enriched porridges. Recognizing that porridge, a typical first food for young children made from local cereal or tuber flours prepared with water, is not sufficient to meet the nutritional needs of infants, the MOH promotes the “enrichment” of porridge by adding locally available nutritious foods, such as legumes (e.g., beans), ground nuts (e.g., peanuts or cashews), seeds (e.g., sesame), and green leafy vegetables (e.g., cassava leaves, sweet potato leaves, and amaranth greens). A teaspoon of oil is added to increase the energy density of the porridge. Cooking demonstrations is a key feature of health programming at the health facility and community level, and the use of a poster entitled “A Nossa Alimentação” (“Our diet”), depicting four food groups (cereals and tubers; meats, eggs, milk, and legumes; vegetables and fruits; and fats, nuts, and sugar/honey), was used for nutrition education until the UNICEF IYCF counselling cards and key messages were adapted to the Mozambican context in 2012 (UNICEF, 2012).
Although not fully rolled out across the country, the implementation of the Mozambique MOH IYCF community counselling package (MISAU, 2013) is of utmost importance to shift the focus beyond enriched porridges and broaden knowledge on adequate complementary feeding, in texture and consistency while also emphasizing quantity and frequency of meals.
Addressing the context‐specific determinants of behaviours, which affect complementary feeding, is also key, as guided by the SBCC Strategy to Prevent Undernutrition in Mozambique (MISAU, 2015). An MCSP‐led trials of improved practices (TIPs) assessment provided much needed formative data on cultural beliefs and perceptions, which drive complementary feeding practices in northern Mozambique (Picolo, Rácz, Kavle, & Gottwalt, 2017). These data aided to develop key counselling messages to address key challenges mothers face and recipes for cooking demonstrations as part of project implementation (Maternal and Child Survival Program [MCSP], 2017). Table 3 presents some of the challenges identified and how MCSP aimed to support the MOH in addressing those by tailoring messages and designing recipes to make small changes feasible. The messages and recipes presented are illustrative of several other applicable messages and recipes.
Table 3.
Complementary feeding problems, associated messages, and suggested recipes, example from TIPs assessment counselling guide and materialsa
| Complementary feeding problems, children 6–8 months of age | Key messages | Motivation | Recipes |
|---|---|---|---|
|
The porridges fed to the baby only have sugar or salt added to them Child is not fed with fruits |
To sweeten porridges, use fruits (banana, papaya, guava, mango, and wild fruits) rather than sugar. Give (mashed if appropriate for age) fruits (banana, papaya, guava, mango, wild fruits, orange, and pineapple) as a snack to your child, at least once per day. |
Fruits have a much higher nutritious value than sugar, which has no benefit for your child's health and growth. Your baby will like the sweetness of the fruit. Vegetables and fruits contain vitamins and minerals important to your baby and will help to prevent and protect him/her from illnesses, diseases, vitamin deficiencies, and anaemia. |
Banana and coconut compote Mashed mango |
| Child is not fed legumes, chicken, meat, fish, eggs, or a source of protein on a daily basis | If you do not have a source of chicken, meat, or fish daily, give your baby meals made from beans and grains daily (e.g., peeled mashed beans or peas, or moringa). | Legumes and grains are good for your baby's growth and can be given to the baby if you do not have chicken meat, chicken liver, fish, or red meat available. |
Mashed rice, mung beans, and coconut (“Mucapata”) Black‐eyed peas soup Mashed orange flesh sweet potato and black‐eyed peas (“xiguinha”) |
| The child's diet is simple and repetitive, with no variation | Vary the colours of the mashed vegetables you give; make sure your baby is getting green, yellow, or orange vegetables daily. |
To grow and develop well, your child needs a diverse diet, eating foods from all four food groups daily. If you vary the food you give to the child, the child will get to know different tastes and will like and eat more things. |
Pumpkin, moringa, and pureed coconut Cabbage curry with peanuts |
| Child is fed non‐nutritive liquids or foods (artificial juices in powder form diluted in water, soft drinks, sugary cakes, cookies, and biscuits) |
Give your baby a snack such as half a banana or a piece of cooked sweet potato instead of cakes or cookies. Give your baby treated, clean water and natural juices instead of soft drinks and artificial juices. |
These foods are very expensive. It is cheaper for you and better for the child to buy an egg or some fruit. These foods and liquids contain preservatives, colouring, and food additives, which can be harmful to your baby. |
Roasted pumpkin seeds Roasted orange flesh sweet potato Orange flesh sweet potato juice |
Note. TIPs: trials of improved practices.
MCSP, 2017. “A Counseling Guide for Infant and Young Child Feeding in Mozambique – Based on Results of Trials of Improved Practices (TIPs) Assessment.” Washington DC: MCSP.
In support of the MOH, MCSP trained health providers on IYCF counselling and equipped health facilities and communities in Nampula and Sofala with the Mozambique MOH IYCF community counselling package. In addition to training, MCSP worked with the MOH to strengthen the health system by providing supportive supervision, mentoring and on‐the‐job training to strengthen counselling skills. At the community level, MCSP developed songs, based on key IYCF messages, which were recorded and rolled out for entertainment education across the province.
6. RECOMMENDATIONS FOR STRENGTHENING INTEGRATED MICRONUTRIENT PROGRAMMING IN PRIMARY HEALTHCARE SERVICES IN MOZAMBIQUE
In order to make an informed choice of the intervention(s) (e.g., use of MNPs, VAS, or others) to implement in the Mozambican context, evidence should be generated on monitoring prevalence of micronutrient deficiencies in the target population, as well as on the interventions' costs, cost‐effectiveness, feasibility, and acceptability. Table 4 summarizes the challenges, recommendations, and justifications for supplementation and the use of micronutrient powders and dietary diversification strategies in Mozambique. Although this case study focuses on interventions that are integrated in healthcare services, these should be considered in the context of complementary multisectoral interventions, including biofortification and industrial food fortification.
Table 4.
Identified challenges and recommendations for strengthening integration of micronutrient interventions in primary healthcare services
| Micronutrient interventions | Challenges | Recommendations | Justification |
|---|---|---|---|
| Vitamin A supplementation |
• Low demand for VAS through routine child health services • Missed opportunities for VAS in outreach immunization services • Top‐bottom supply chain leading to localized stock‐outs • Vertical reporting of VAS that is not inclusive of all delivery platforms • Lack of up to date nationally representative vitamin A deficiency prevalence data |
• Operationalize the communication plan to strengthen routine vitamin A and deworming services to generate demand • Improve community involvement to map populations with unequal access to health facilities and adequately plan vitamin A supplements to serve that population, as part of RED/REC, to improve coverage • Improve forecasting and programme monitoring through the use of sub‐national coefficients and microplanning to better estimate the target population • Improve supply chain management to enable facility health workers and CHWs to request the amount of vitamin A capsules needed to serve the population in their catchment areas, rather than being passive receivers • Roll out the use of the new child health monitoring tools to eliminate vertical reporting of VAS and improve completeness • Pursue inclusion of CHW VAS data in the national DHIS2 platform • Assess the current prevalence of VAS to make informed decision‐making • Make opportunist use of future immunization campaigns as catch‐up/acceleration of routine supplementation of vitamin A based on the last dose received as registered on the child heath card instead of mass supplementation |
These actions will address the factors known to limit VAS coverage in integrated routine child health services, as part of the operationalization of the guide to strengthen routine vitamin A supplementation and deworming.
Since the last nationally representative vitamin A deficiency survey was conducted in 2002, the MOH should plan to conduct another prevalence study within the next decade to make an informed decision on the continuation of routine vitamin A supplementation, in the context of mandatory industrial food fortification of sugar and oil with vitamin A since 2016 (Government of the Republic of Mozambique, 2016), and the increased availability and acceptance of OFSP and other products made with OFSP.a |
| Point‐of‐use fortification with MNP |
• Low interest in continued and improved implementation of point‐of‐use fortification with MNP as a strategy to reduce iron‐deficiency anaemia in children • Lack of focus on the integration of MNP and malaria control measures • Lack of regular assessment of the formulation of MNP used |
• Finalize and approve the MNP strategy taking into account lessons learned from the implementation to date (to be inserted as a priority in the MOH nutrition socio‐economic plan for 2019) • Revitalize the MOH MNP task force to address the core issues affecting the feasibility and sustainability of MNPs in the country, particularly regarding procurement and supply chain, legal framework around marketing of MNP, SBCC strategy on MNP, and integration with malaria control strategies. • Regularly assess the formulation of MNP used to permit adjustment in relation to other interventions implemented in the country, to prevent the risk of inadequate and high intakes of specific micronutrients, for example, vitamin A, given mandatory fortification of sugar and oil with vitamin A since October 2016 |
There are unaddressed issues pertaining to MNP procurement and supply chain, the legal framework around marketing of MNP, the need for an SBCC strategy on MNP, the integration of MNP promotion, and malaria control strategies
WHO recommends regular assessment of the risk of high intakes of vitamin A considering complementary vitamin A deficiency reduction interventions implemented in the national context (WHO, 2016). |
| Dietary diversity promotion |
• Lack of coordinated and harmonized cross‐sectoral efforts. • No information sharing among governmental sectors and/or partners implementing food‐based approaches to reduce micronutrient deficiencies, for example, agriculture with biofortification,b industry and commerce with industrial food fortification,c and health with supplementation and point‐of‐use fortification |
• Develop a comprehensive national strategy on food‐based strategies to reduce malnutrition in Mozambique, for improved coordination and harmony of cross‐sectoral efforts | Food‐based approaches have the ability to produce the most sustainable improvements in micronutrient status, yet they have been implemented in silos, with no information sharing among governmental sectors and/or partners. Coordinated and harmonized cross‐sectoral efforts are required for sustainable improvements in micronutrient status |
Note. CHWs: community health workers; DHIS2: District Health Information System; MNP: micronutrient powder; MOH: Ministry of Health; OFSP: orange‐fleshed sweet potato; RED/REC: reaching every district/reaching every child; VAS: vitamin A supplementation; WHO: World Health Organization.
In 2015 alone, OFSP accounted for a third (32%) of the sweet potato production in Mozambique (Source: Ministry of Agriculture and Food Security, 2016).
OFSP is highly acceptable to Mozambicans, and trials of OFSP production and consumption have been shown to dramatically increase vitamin A intake (from 2‐ to 8.3‐fold) and reduce vitamin A deficiency among intervention children (Source: Jenkins, Byker Shanks, & Houghtaling, 2015).
Since October 2016, it is mandatory that the following foods are fortified: wheat flour fortified with iron, demerged maize fortified with iron, edible vegetable oils fortified with vitamin A, and sugar fortified with vitamin A. Fortification of salt with iodine has been mandatory since the year 2000 (Source: Government of the Republic of Mozambique, 2016).
7. CONCLUSION
In Mozambique, the success of micronutrient programing to address vitamin A and iron deficiency will be largely determined by the roll‐out of guidelines (including the planning guide for VAS and deworming and the RED/REC guide); implementation of demand generation activities (songs, theatre, cooking demonstrations, group talks, and home visits) particularly through community leaders, Agentes Polivalentes Elementares, and community activists; and adequate planning and forecasting of resources and supplies to meet needs in an equitable manner. Ongoing monitoring of the prevalence of micronutrient deficiencies and the coverage of micronutrient interventions is needed in the face of multiple interventions implemented concurrently to address vitamin A and iron deficiency for the same target groups (such as industrial food fortification, biofortification, and point‐of‐use fortification) to make evidence‐based decisions to drive health programming. To ensure coordinated, harmonized, and cost‐effective efforts, the Mozambique government should consider the development of a cohesive national strategy for the prevention and control of micronutrient malnutrition, with clearly defined monitoring and evaluation targets, and a mechanism that sustainably ensures that support for these interventions is increasingly less dependent on external funding.
CONFLICTS OF INTEREST
We declare no conflict of interests. USAID provided review of the manuscript, and authors had intellectual freedom to include feedback, as needed.
CONTRIBUTIONS
MP and JAK conceptualized and led the writing of the paper. IB, MJ, AG, and BS were involved in writing of paper. All authors were involved in the decision to submit the paper for publication.
FUNDING
This article is made possible by the generous support of the American people through the United States Agency for International Development (USAID) under the terms of the Cooperative Agreement AID‐OAA‐A‐14‐00028. The contents are the responsibility of the Maternal and Child Survival Program and do not necessarily reflect the views of USAID or the United States Government.
ACKNOWLEDGEMENT
We gratefully acknowledge Sonia Khan, UNICEF Mozambique for her review of the vitamin A supplementation data and information.
Picolo M, Barros I, Joyeux M, et al. Rethinking integrated nutrition‐health strategies to address micronutrient deficiencies in children under five in Mozambique. Matern Child Nutr. 2019;15(S1):e12721 10.1111/mcn.12721
Footnotes
Absolute poverty is defined as the “inability due to lack of capacity, or lack of opportunity of individuals, families and communities to access the minimum conditions, according to the basic norms of society.”
Fifteen micronutrients, including 10 mg of elemental iron, 5 mg of elemental zinc, and 300 μg of retinol.
Receiving 4+ food groups the day before the interview
Adapted to the Mozambique context from UNICEF's generic community‐based IYCF counselling package (available at https://www.unicef.org/nutrition/index_58362.html)
Blog post on MCSP's use of songs for breastfeeding promotion is available at https://www.mcsprogram.org/singing-for-change-in-mozambique-this-world-breastfeeding-week/.
REFERENCES
- African Development Bank Group (2018). African economic outlook 2018. Abidjan, Cote d'Ivoire: African Development Bank Group. [Google Scholar]
- Aguayo, V. M. , Khan, S. , Ismael, C. , & Meershoek, S. (2005). Vitamin A deficiency and child mortality in Mozambique. Public Health Nutrition, 8(1), 29–31. 10.1079/PHN2005664 [DOI] [PubMed] [Google Scholar]
- Carrilho, J. , Abbas, M. , Júnior, A. , Chidassicua, J. , & Mosca, J. (2016). Challenges for food security and nutrition in Mozambique. Maputo, Mozambique: Rural Observatory of Mozambique. [Google Scholar]
- Food and Agriculture Organization of the United Nations [FAO] (2011). Nutrition country profile, Republic of Mozambique: 2011. Rome, Italy: FAO. [Google Scholar]
- Government of the Republic of Mozambique (2010). Multisectorial plan for chronic malnutrition reduction in Mozambique 2011–2014 (2020). Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- Government of the Republic of Mozambique (2016). Decree no. 9/2016. Republic of Mozambique's Bulletin , 1(46). Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- Jenkins, M. , Byker Shanks, C. , & Houghtaling, B. (2015). Orange‐fleshed sweet potato: Successes and remaining challenges of the introduction of a nutritionally superior staple crop in Mozambique. Food and Nutrition Bulletin, 36(3), 327–353. 10.1177/0379572115597397 [DOI] [PubMed] [Google Scholar]
- Maternal and Child Survival Program [MCSP] (2017). A counseling guide for infant and young child feeding in Mozambique – Based on results of trials of improved practices (TIPs) assessment. Washington, DC: MCSP. [Google Scholar]
- MCSP (2018). MCSP Mozambique program reports October 2016–March 2018. Washington, DC: MCSP. [Google Scholar]
- Ministry of Agriculture and Food Security (Mozambique) (2014). National agriculture investment plan 2014–2018. Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- Ministry of Agriculture and Food Security (Mozambique) (2016). Agrarian statistics yearbook 2015. Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- Ministry of Economy and Finance (Mozambique) (2016). Poverty and wellbeing in Mozambique: Fourth national evaluation – Family budget survey 2014/15. Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- Ministry of Health [MISAU] (Mozambique) (2005). Micronutrient supplementation in Mozambique. Utilization of micronutrient supplements in health programs. Guide for health personnel. Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- MISAU (2006). National survey on vitamin A deficiency, anemia and malaria in children 6–59 months and their mothers (December 2001–February 2002). Maputo, Mozambique: MISAU Nutrition Division & INE. [Google Scholar]
- MISAU (2007). Guidance for introducing the basic nutrition package in urban and rural health facilities. Facilitator's manual and participant's manual. 3rd version. Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- MISAU (2009). Integrated plan for the achievement of millennium development goals 4 and 5.2009–2012 (2017). Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- MISAU (2011). Norms for well child and sick child consultations. Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- MISAU (2013). Community counseling package on infant feeding. Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- MISAU (2014). Integrated management of childhood illnesses (IMCI) – Booklet of maps for integrated attention to the sick child from 1 week to 2 months and from 2 months to 5 years. Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- MISAU (2015). Social and behavior change communication strategy for the prevention of undernutrition in Mozambique 2015–2019. Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- MISAU (2016). Annual report of the nutrition program 2015. National Public Health Directorate, Nutrition Department. Maputo, Mozambique: MISAU Nutrition Division. [Google Scholar]
- MISAU (2017a). Annual report of the nutrition program 2016. National Public Health Directorate, Nutrition Department. Maputo, Mozambique: MISAU Nutrition Division. [Google Scholar]
- MISAU (2017b). Planning guide of vitamin A supplementation and deworming activities in routine health services. Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- MISAU (2017c). Nutrition bulletin no. 4/2017. National Public Health Directorate, Nutrition Department. Maputo, Mozambique: MISAU Nutrition Division. [Google Scholar]
- MISAU (2018). Annual report of the nutrition program 2017. National Public Health Directorate, Nutrition Department. Maputo, Mozambique: MISAU Nutrition Division. [Google Scholar]
- MISAU , & Helen Keller International Mozambique (2018). Communication plan to operationalize the integration of health weeks in routine services. Maputo, Mozambique: Government of the Republic of Mozambique. [Google Scholar]
- MISAU , INE , & ICFI (2015). Mozambique immunization, malaria, and HIV/AIDS indicators survey 2015. Maputo, Mozambique & Rockville, MD: National Institute of Health (Mozambique), INE, & ICFI. [Google Scholar]
- MISAU , National Institute of Statistics [INE] (Mozambique) , & ICF International [ICFI] (2013). Mozambique demographic and health survey 2011. Calverton, MD: MISAU, INE, & ICFI. [Google Scholar]
- National Institute of Statistics [INE] (Mozambique) (2017). Dissemination of the preliminary results of the IV general population and housing census 2017. Maputo, Mozambique: INE. [Google Scholar]
- Nyhus Dhillon, C. , Sarkar, D. , Klemm, R. D. , Neufeld, L. M. , Rawat, R. , Tumilowicz, A. , & Namaste, S. M. (2017). Executive summary for the micronutrient powders consultation: Lessons learned for operational guidance. Maternal & Child Nutrition, 13(Suppl 1). 10.1111/mcn.12493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picolo, M. , Rácz, S. , Kavle, J. A. , & Gottwalt, A. (2017). Cultural beliefs and practices that influence infant and young child feeding in Mozambique: Results of trials of improved practices assessment. Washington DC: MCSP. [Google Scholar]
- SPRING (2018). Comprehensive costing in micronutrient supplementation: Findings from SPRING's micronutrient powder (MNP) distribution pilot program in Uganda. Washington, DC: SPRING. [Google Scholar]
- Technical Secretariat for Food Security and Nutrition [SETSAN] (Mozambique) (2013). Food and nutrition security baseline 2013 – General report. Maputo, Mozambique: SETSAN. [Google Scholar]
- UNICEF (2012). Community IYCF counselling package. New York, NY: UNICEF. [Google Scholar]
- UNICEF (2017). Mozambique 2017 budget brief: Health. Maputo, Mozambique: UNICEF. [Google Scholar]
- UNICEF (2018). Coverage at a crossroads: New directions for vitamin A supplementation programmes. New York, NY: UNICEF. [Google Scholar]
- WHO (2016). WHO guideline: Use of multiple micronutrient powders for point‐of‐use fortification of foods consumed by infants and young children aged 6–23 months and children aged 2–12 years. Geneva, Switzerland: WHO. [PubMed] [Google Scholar]
- WHO (2017). Reaching every district (RED), 2017 revision. Brazzaville, Democratic Republic of the Congo WHO. [Google Scholar]
- World Health Organization [WHO] (2011). Guideline: Use of multiple micronutrient powders for home fortification of foods consumed by infants and children 6–23 months of age. Geneva, Switzerland: WHO. [PubMed] [Google Scholar]


