ABSTRACT
Objective
To investigate whether the classification of a previous spontaneous preterm birth (sPTB) as preterm labor (PTL) with intact membranes (IM) or as preterm prelabor rupture of membranes (PPROM) impacts the efficacy of cervical pessary or vaginal progesterone for prevention of sPTB in pregnant women with short cervix on transvaginal ultrasound.
Methods
This was a retrospective cohort study of asymptomatic high‐risk singleton pregnancies with a short cervix and history of sPTB, treated using Arabin pessary or vaginal progesterone for primary PTB prevention, conducted at four European hospitals. A log‐rank test on Kaplan–Meier curves was used to assess the difference in performance of pessary and progesterone, according to history of PTL‐IM or PPROM. Linear regression analysis was used to evaluate significant predictors of gestational age at delivery.
Results
Between 2008 and 2015, 170 women were treated with a pessary and 88 with vaginal progesterone. In women treated with a pessary, rate of sPTB < 34 weeks was 16% in those with a history of PTL‐IM and 55% in those with a history of PPROM. In women treated with progesterone, rate of sPTB < 34 weeks was 13% in those with a history of PTL‐IM and 21% in those with a history of PPROM. Treatment with a pessary resulted in earlier delivery in women with previous PPROM than in any other subgroup (P < 0.0001). Linear regression analysis showed a clear effect of PPROM history (P < 0.0001), combination of PPROM history and treatment (P = 0.0003) and cervical length (P = 0.0004) on gestational age at birth.
Conclusions
Cervical pessary may be a less efficacious treatment option for women with previous PPROM; however, these results require prospective validation before change in practice is recommended. Phenotype of previous preterm birth may be an important risk predictor and treatment effect modifier; this information should be reported in future clinical trials. © 2018 The Authors. Ultrasound in Obstetrics & Gynecology published by John Wiley & Sons Ltd on behalf of the International Society of Ultrasound in Obstetrics and Gynecology.
Keywords: Arabin pessary, PPROM, preterm birth, short cervix, vaginal progesterone
INTRODUCTION
The presentation of preterm birth remains important for identifying the cause, estimating the risk of recurrence and implementing preventative strategies in subsequent pregnancies. A broad classification system of preterm birth based on presentation includes iatrogenic preterm birth, spontaneous preterm labor (PTL) with intact membranes (IM) and preterm prelabor rupture of membranes (PPROM), each accounting for approximately one‐third of all preterm births1.
More recently, preterm birth classifications have used an increasingly complex conceptual framework based on severe maternal, fetal and placental conditions causally associated with preterm birth2. At present, it is difficult to know how to apply this classification system to the management of subsequent pregnancy; many observable pregnancy characteristics fall across a minimum of two classifications, and interventions for prevention remain limited. The only presentation for which there is effective intervention in singleton pregnancy to prevent spontaneous preterm birth (sPTB) is history of sPTB and/or a short cervix3, 4.
There is increasing evidence from systems biology (the computational and mathematical modeling of complex biological systems) that sPTB with IM at labor and PPROM have distinct biological pathways5. An autoimmune/hormonal regulation axis may exist for spontaneous PTL‐IM, whilst pathways implicated in the etiology of PPROM include hematological/coagulation function disorder, collagen metabolism, matrix degradation and local inflammation. Additionally, the dissimilarity of clinical risk factors for PPROM and PTL‐IM suggests that there are different underlying pathophysiological pathways6.
It is therefore reasonable to hypothesize that treatments for short cervix may exert different biological and environmental interactions and effects resulting in different pregnancy outcomes. Although exact mechanisms of action remain to be established, the actions of vaginal progesterone and pessary are likely to have different mechanisms of therapeutic effect. A pessary is a device that provides mechanical support and increases the uterocervical angle at the cervix7, whereas vaginal progesterone has anti‐inflammatory properties and inhibits production of stimulatory prostaglandins (PG) and expression of contraction‐associated protein genes in the myometrium8.
The aim of this study was to investigate the effectiveness of vaginal progesterone and Arabin pessary for preventing sPTB in women with a short cervix on transvaginal ultrasound, according to classification of previous sPTB as PTL‐IM or PPROM.
METHODS
This was a retrospective cohort study of asymptomatic high‐risk singleton pregnancies with a short cervix and history of sPTB, conducted between 2008 and 2015 at four hospitals, one in Liverpool, UK (Liverpool Women's Hospital), two in Barcelona, Spain (Vall d'Hebron; Hospital Clinic Barcelona) and one in Turin, Italy (Università degli Studi Torino). All four hospitals used either cervical Arabin pessary (a CE‐certified pessary; CE 0482/EN ISO 13485: 2003 annex III of the council directive 93/42 EEC) or vaginal progesterone 200 mg nocte as a primary treatment for preterm birth prevention. All women were classified into one of two groups: history of PTL‐IM ≤ 34 weeks or history of PPROM ≤ 34 weeks. Classification was performed by preterm birth experts at each unit to classify cases as correctly as possible. Any woman who had a history of both PTL‐IM and PPROM was included in the PPROM group. PPROM was defined as a diagnosis of spontaneous rupture of the membranes at least 12 h prior to delivery. Excluded were all women with a history of a short cervix only (i.e. no history of preterm birth/PPROM), women treated prophylactically due to a history of PTL‐IM or PPROM but without having a short cervix, cases in which cervical‐length data were not available, multifetal pregnancies, congenital abnormalities diagnosed in the fetus and cases with cervical cerclage used as a first‐line therapy. Short cervix was defined by individual hospital protocols, but was either a single measurement of ≤ 25 mm or < 3rd centile for gestational age9. Ethical approval was obtained at each hospital for use of patient data to be analyzed retrospectively.
The primary outcome was gestational age at delivery. For the primary analysis, we excluded all women who had been additionally treated with a cervical cerclage, and who had swapped treatment or had additional treatment based on clinical perception that the primary treatment was failing. Secondary analysis included all women based on an intention‐to‐treat principle.
Statistical analysis
Demographic variables included in the analysis were age, ethnicity, body mass index (BMI), smoking, cervical surgery, number of term deliveries, number of PTL‐IM, number of PPROM, gestational age at earliest PTL‐IM/PPROM and treatment for short cervix. SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, NY, USA) was used to calculate P‐values using one‐way ANOVA, Kruskal–Wallis test, Mann–Whitney U‐test, chi‐square test or Fisher's exact test, as appropriate. Subsequently, demographics were compared between women who had previously experienced PTL‐IM and those who had previously experienced PPROM. A log‐rank test on Kaplan–Meier curves was performed to assess the difference in performance of vaginal progesterone and Arabin pessary according to history of PTL‐IM or PPROM, using the software package R (R Foundation for Statistical Computing, Vienna, Austria; https://cran.r-project.org/). In order to establish which clinical characteristics are significant predictors of gestational age at delivery and by what magnitude they contribute to this pregnancy outcome, linear regression analysis was performed, using type of treatment, cervical length and phenotype of previous sPTB as potential predictors.
RESULTS
Data on 258 women with a history of PPROM and/or PTL‐IM who had subsequent treatment for short cervix with Arabin pessary or vaginal progesterone were obtained from the four participating obstetric centers in Europe between 2008 and 2015 (Figure 1). Arabin pessary was the primary therapy in 170 women, 10 (6%) of whom required an additional therapy or change in treatment. Vaginal progesterone treatment was used in 88 women, 21 (24%) of whom received an alternative or additive treatment following further cervical shortening. The 31 women with alternative or additive therapy were excluded from the primary analysis. Demographic data for the full cohort according to center and treatment group are shown in Table S1. The demographics of the 227 women included in the primary analysis are shown according to center in Table 1 and according to treatment and classification of previous sPTB in Table 2. Significant differences in demographics between hospital populations included tobacco use, cervical surgery and gestational age at treatment, with the Turin center screening until a later gestational age than the other three hospitals (Table 1); however, there was no statistically significant difference in gestational age at delivery between the centers (P = 0.45). BMI was slightly lower in the group with history of PPROM who were treated with progesterone, although it was felt that such a small difference, while statistically significant, would not be clinically important. Cervical surgery rate was found to be higher in this group (24%), but this did not affect treatment performance as measured by gestational age at delivery. In women treated with Arabin pessary, there was a significantly greater proportion who had PPROM in the index pregnancy in those who had previously experienced PPROM compared with those with a history of PTL‐IM (32% vs 9%, P ≤ 0.001) (Table 2). Overall, women with a history of PPROM were more likely to deliver earlier than those with a history of PTL‐IM (35 weeks vs 38 weeks, P ≤ 0.001).
Figure 1.
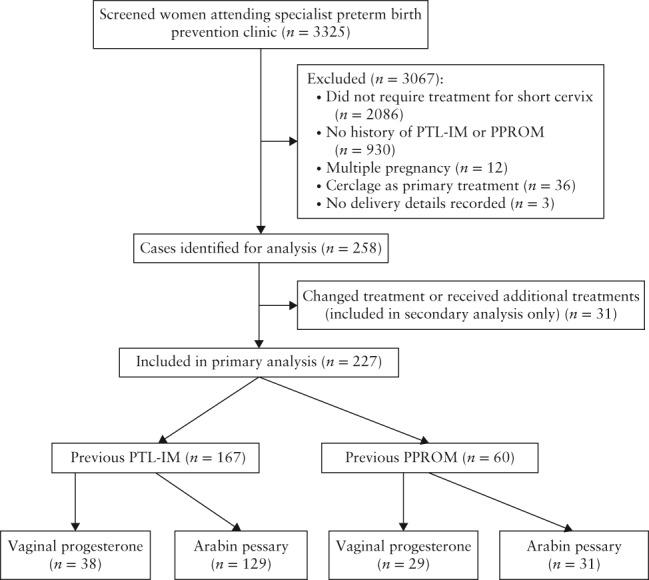
Flowchart showing inclusion of women in study. PPROM, preterm prelabor rupture of membranes; PTL‐IM, preterm labor with intact membranes.
Table 1.
Characteristics of 227 women with short cervix and previous preterm labor with intact membranes (PTL‐IM) or preterm prelabor rupture of membranes (PPROM), according to center
| Characteristic | Liverpool Women's Hospital (n = 77) | Barcelona Vall d'Hebron (n = 98) | Hospital Clinic Barcelona (n = 20) | University of Turin (n = 32) | P |
|---|---|---|---|---|---|
| Age (years) | 31 ± 5 | 31 ± 5 | 33 ± 5 | 32 ± 4 | 0.514* |
| BMI | 25 ± 5 | 26 ± 3 | 23 ± 5 | 25 ± 4 | 0.100* |
| Ethnicity | — | ||||
| Caucasian | 66 (86) | 57 (58) | 18 (90) | 28 (88) | |
| Black | 9 (12) | 8 (8) | 0 (0) | 3 (9) | |
| Asian | 1 (1) | 10 (10) | 0 (0) | 0 (0) | |
| Indian | 1 (1) | 0 (0) | 0 (0) | 0 (0) | |
| Hispanic | 0 (0) | 23 (23) | 2 (10) | 0 (0) | |
| Tobacco use | 26 (34) | 21 (21) | 4 (20) | 3 (9) | 0.039† |
| Cervical surgery | 15 (19) | 1 (1) | 2 (10) | 3 (9) | < 0.001† |
| Gestational age at treatment (weeks) | 21 (14–28) | 22 (19–24) | 23 (9–29) | 25 (15–32) | 0.001‡ |
| Cervical length at treatment (mm) | 20 (3–29) | 20 (5–25) | 21 (9–24) | 20 (0–27) | 0.401‡ |
| Arabin pessary | 38 (49) | 98 (100) | 0 (0) | 24 (75) | — |
| Vaginal progesterone | 39 (51) | 0 (0) | 20 (100) | 8 (25) | — |
Date are presented as mean ± SD, n (%) or median (range).
One‐way ANOVA.
Chi‐square test.
Kruskal–Wallis test.
BMI, body mass index.
Table 2.
Demographics and pregnancy outcome of 227 women with short cervix included in primary analysis, according to treatment and previous spontaneous preterm birth classification
| Parameter | Pessary (n = 160) | Progesterone (n = 67) | P | ||
|---|---|---|---|---|---|
| PTL‐IM (n = 129) | PPROM (n = 31) | PTL‐IM (n = 38) | PPROM (n = 29) | ||
| Demographic data | |||||
| Age (years) | 31 ± 5 | 32 ± 5 | 31 ± 6 | 32 ± 4 | 0.745* |
| BMI | 25 ± 4 | 25 ± 4 | 25 ± 4 | 23 ± 5 | 0.043* |
| Ethnicity | — | ||||
| Caucasian | 92 (71) | 17 (55) | 33 (87) | 27 (93) | |
| Black | 11 (9) | 5 (16) | 3 (8) | 1 (3) | |
| Asian | 4 (3) | 6 (19) | 0 (0) | 1 (3) | |
| Indian | 1 (1) | 0 (0) | 0 (0) | 0 (0) | |
| Hispanic | 21 (16) | 3 (10) | 2 (5) | 0 (0) | |
| Tobacco use | 31 (24) | 5 (16) | 10 (26) | 8 (28) | 0.712† |
| Cervical surgery | 9 (7) | 2 (7) | 4 (11) | 7 (24) | 0.038† |
| Gestational age at treatment (weeks) | 22 (16–32) | 22 (16–30) | 22 (14–29) | 22 (16–30) | 0.941‡ |
| Cervical length at treatment (mm) | 20 (3–29) | 17 (4–27) | 21 (6–27) | 22 (0–26) | 0.021‡ |
| Pregnancy outcome | |||||
| Gestational age at delivery (weeks) | 38 (22–41) | 29 (21–40) | 38 (27–41) | 37 (23–41) | < 0.001‡ |
| PPROM | 11 (9) | 10 (32) | 4 (11) | 9 (31) | < 0.001† |
| Preterm birth < 34 weeks | 21 (16) | 17 (55) | 5 (13) | 6 (21) | < 0.001† |
| Cesarean section | 20 (16) | 5 (16) | 5 (13) | 7 (24) | 0.650† |
Date are presented as mean ± SD, n (%) or median (range).
One‐way ANOVA.
Chi‐square test.
Kruskal–Wallis test.
BMI, body mass index; PPROM, preterm prelabor rupture of membranes; PTL‐IM, preterm labor with intact membranes.
Using a log‐rank test on Kaplan–Meier survival curves, a four‐way comparison was performed to assess if there was any difference in the duration of pregnancy between four distinct groups: (1) previous PPROM and treated with Arabin pessary; (2) previous PTL‐IM and treated with Arabin pessary; (3) previous PPROM and treated with vaginal progesterone; and (4) previous PTL‐IM and treated with vaginal progesterone. Overall, the difference between the four groups was highly significant (P < 0.0001) due to much earlier gestational age at delivery in women with previous PPROM and treated with Arabin pessary (Figure 2). When only women treated with progesterone were compared, there was no difference in the duration of pregnancy between those with previous PPROM and those with previous PTL‐IM (P = 0.365). The results remained qualitatively unchanged when the 31 women who received a combination of treatments were included (intention‐to‐treat analysis; Figure S1). The median gestational age at delivery for women on vaginal progesterone (n = 21; 10 with previous PPROM) who had additional treatment or change in treatment was 38 weeks (range, 18–41 weeks) compared with 27 weeks (range, 19–38 weeks) in the Arabin pessary group (n = 10; six with previous PPROM).
Figure 2.
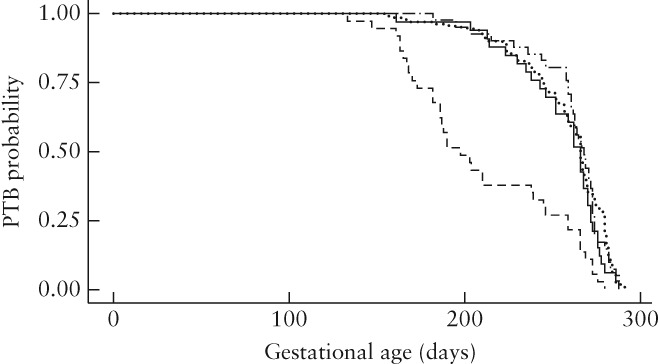
Kaplan–Meier survival curves demonstrating preterm birth (PTB) probability in 227 women with short cervix included in primary analysis, according to obstetric history and treatment: previous preterm prelabor rupture of membranes (PPROM), treated with Arabin pessary ( ); previous preterm labor with intact membranes (PTL‐IM), treated with Arabin pessary (
); previous preterm labor with intact membranes (PTL‐IM), treated with Arabin pessary ( ); previous PPROM, treated with vaginal progesterone (
); previous PPROM, treated with vaginal progesterone ( ); previous PTL‐IM, treated with vaginal progesterone (
); previous PTL‐IM, treated with vaginal progesterone ( ).
).
The shortest cervical lengths at treatment were clustered in the group with previous PPROM and treated with Arabin pessary, with the median cervical length at treatment being lower in this group by 3–5 mm (Table 2; P = 0.021). As shorter cervical length is a known risk factor for PTB, linear regression analysis was performed to determine if cervical length affected both the allocation of group and outcome. The data confirmed that cervical length seems to be an independent predictor of gestational age at birth (P = 0.0004). However, the strongest variables in predicting earlier gestational age at delivery in our dataset were history of PPROM (P < 0.0001) and a combination of history of PPROM and treatment type (P = 0.0003). Combining cervical length with treatment type or PPROM history did not improve the prediction of gestational age at delivery.
DISCUSSION
Analysis of data in this retrospective study has demonstrated that history of PPROM may be an important predictor of treatment success for short cervix in subsequent pregnancy. The Arabin pessary does not appear to have the same benefit in women who previously experienced PPROM compared with those with previous PTL‐IM. Vaginal progesterone may therefore be a more efficacious treatment option for these women.
The pathophysiological mechanism behind this effect is not clear. One possible theory is that the Arabin pessary may exacerbate a dysbiotic vaginal microbial environment. Kindinger et al. investigated the effect of suture material on the vaginal environment for a similar at‐risk population10. They demonstrated that, compared with a braided suture, a monofilament material reduced the risk of preterm birth by an additional 11% and also reduced the rate of non‐viable birth (< 24 weeks or intrauterine death). This causal effect was further supported by evidence that, despite dysbiotic microbiomes being equal in prevalence prior to suture insertion, braided cerclage led to a shift towards dysbiosis in just 4 weeks after insertion. The Arabin pessary is a cone‐shaped silicone device that, once sited around a cervix, remains in the vagina until removal prior to labor. We hypothesize that a similar effect could be involved here but found no published studies investigating the possible impact of an Arabin pessary on surrounding vaginal microbiome. One study examining ring pessaries for pelvic organ prolapse in a non‐pregnant population demonstrated that they could exacerbate growth of pre‐existing anaerobic bacteria11. The foreign body of the pessary could provide a surface for colonization or, alternatively, many Arabin pessary users report a marked increase in watery discharge, which could affect vaginal microbial flora. In contrast, vaginal progesterone does not have any adverse impact on vaginal microbiota in pregnancy12.
The effect of different outcomes in different populations may, at least in part, account for the variation that we have seen in recent years in the mixed outcomes of clinical trials of Arabin pessary for a short cervix. The landmark paper that brought Arabin pessary into more frequent use as an alternative to vaginal pessary and cervical cerclage in current clinical practice was the PECEP trial published in 2012, which reported a significant reduction in rate of spontaneous delivery before 34 weeks of gestation13. Mixed results have been reported in subsequent clinical trials of pessary for short cervix, without satisfactory explanation14, 15, 16. As most studies collect limited data on the observable characteristics of previous preterm births or any other biomarkers, further individual patient data analyses are unlikely to provide better evidence of the importance of various classifications of preterm labor as potential modifiers of treatment success.
We acknowledge that our data are retrospective and we therefore cannot be certain that all classifications were assigned correctly. However, cases of sPTB and PPROM were reviewed by preterm birth experts at each unit to classify each case as correctly as possible. We would recommend that the results of this study be validated in a separate population before advising a change in clinical practice. Our data are not randomized and therefore confounding as a cause of our results cannot be completely excluded.
Although women in each group had a comparable distribution of cervical lengths, the median measurement was lowest, at 17 mm, in the group with a history of PPROM and treated with Arabin pessary. However, a history of PPROM alone and PPROM interacting with treatment type were both independent predictors of gestational age at birth, irrespective of cervical length when treatment was initiated. Whether in fact a pessary exacerbates the risk of preterm birth in women with previous PPROM or, alternatively, progesterone modifies the risk of PPROM should be validated in future prospective studies.
We did not explore the reasons for why 10% of women given Arabin pessary and 24% of those commenced on progesterone were given additional treatment; this may reflect ongoing shortening of the cervix, lack of faith in the treatment by the clinician or patient, or physical discomfort with treatment. The concern for the analysis was that patients requiring a second treatment may be at higher risk of delivering and that excluding them would bias the results, particularly as there were a greater percentage of these cases in the progesterone group. Our intention‐to‐treat analysis (including all cases) revealed that, irrespective of women changing or receiving additional treatment, women with a history of PPROM who received an Arabin pessary as first‐line treatment remained at increased risk of delivering earlier than those receiving vaginal progesterone (Figure S1; P < 0.0001).
Regrettably, we were unable to test in our dataset whether the phenotype of previous preterm birth is also relevant for cervical cerclage. This may be potentially very important given that a significant number of UK preterm birth prevention clinics still use cervical cerclage as a first‐line treatment for short cervix17.
The data from this study have fundamental implications for ongoing clinical trials on preterm birth treatments. We argue that data collection should take into account the observable characteristics of previous preterm births to allow subclassification of results based on history. In‐depth classifications have been published2 but, as a minimum, trying to identify subgroups of sPTB and PPROM would be recommended. The authors acknowledge that the classification of PPROM can be particularly challenging given the subjectivity surrounding ‘the beginning of labor’, inability to access previous pregnancy details and poor note‐keeping. Ideally, phenotyping should also include other key features of the index pregnancy in addition to cervical length, including vaginal microbiome, quantitative fetal fibronectin and blood samples for biomarker testing (genomics, transcriptomics, proteomics, etc.). Clearly, there are important implications for the design and size of future clinical trials if we expect to test the effectiveness of ever smaller groups of patients, but better phenotyping would, as a minimum, encourage increased data sharing and much more informative and clinically useful individual patient data meta‐analyses.
Arabin pessary may not be as effective in women who have previously experienced PPROM, compared with those with a history of PTL‐IM. This differential effect is not seen with vaginal progesterone, which may therefore be a better treatment choice for women with a short cervix and history of PPROM. These data suggest that it may be possible to stratify treatments for short cervix. We recommend that data on previous pregnancy characteristics should be collected routinely as part of clinical trials on preterm birth prevention to evaluate this effect in other populations.
Disclosure
A.C. and Z.A. performed a feasibility randomized clinical trial of Arabin pessary, vaginal progesterone and cervical cerclage in 2016. The vaginal progesterone was supplied by Besins Healthcare at no cost. No funding or stock was received for this study. The remaining authors report no conflict of interest.
REFERENCES
- 1. Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet 2008; 371: 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Villar J, Papageorghiou AT, Knight HE, Gravett MG, Iams J, Waller SA, Kramer M, Culhane JF, Barros FC, Conde‐Agudelo A, Bhutta ZA, Goldenberg RL. The preterm birth syndrome: a prototype phenotypic classification. Am J Obstet Gynecol 2012; 206: 119–123. [DOI] [PubMed] [Google Scholar]
- 3. Conde‐Agudelo A, Romero R, Nicolaides K, Chaiworapongsa T, O'Brien JM, Cetingoz E, da Fonseca E, Creasy G, Soma‐Pillay P, Fusey S, Cam C, Alfirevic Z, Hassan SS. Vaginal progesterone vs . cervical cerclage for the prevention of preterm birth in women with a sonographic short cervix, previous preterm birth, and singleton gestation: a systematic review and indirect comparison metaanalysis. Am J Obstet Gynecol 2013; 208: 42.e1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Liem SM, van Pampus MG, Mol BW, Bekedam DJ. Cervical pessaries for the prevention of preterm birth: a systematic review. Obstet Gynecol Int 2013; 2013: 576723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Capece A, Vasieva O, Meher S, Alfirevic Z, Alfirevic A. Pathway analysis of genetic factors associated with spontaneous preterm birth and pre‐labor preterm rupture of membranes. PLoS One 2014; 9: e108578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Giminez LG, Krupitzki HB, Momany AM, Gili JA, Poletta FA, Campaña H Cosentino VR, Saleme C, Pawluk M, Murray JC, Castilla EE, Gadow EC, Lopez‐Camelo JS. Maternal and neonatal epidemiological features in clinical subtypes of preterm birth. J Maternal and Fetal Med 2016; 29: 3153–3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cannie MM, Dobrescu O, Gucciardo L, Strizek B, Ziane S, Sakkas E, Schoonjans F, Divano L, Jani JC. Arabin cervical pessary in women at high risk of preterm birth: a magnetic resonance imaging observational follow‐up study. Ultrasound Obstet Gynecol 2013; 42: 426–433. [DOI] [PubMed] [Google Scholar]
- 8. Sfakianaki AK, Norwitz ER. Mechanisms of progesterone action in inhibiting prematurity. J Matern Fetal Neonatal Med 2006; 19: 763–772. [DOI] [PubMed] [Google Scholar]
- 9. Salomon LJ, Diaz‐Garcia C, Bernard JP, Ville Y. Reference range for cervical length throughout pregnancy: non‐parametric LMS‐based model applied to a large sample. Ultrasound Obstet Gynecol 2009; 33: 459–464. [DOI] [PubMed] [Google Scholar]
- 10. Kindinger LM, MacIntyre DA, Lee YS, Marchesi JR, Smith A, McDonald JA, Terzidou V, Cook JR, Lees C, Israfil‐Bayli F, Faiza Y, Toozs‐Hobson P, Slack M, Cacciatore S, Holmes E, Nicholson JK, Teoh TG, Bennett PR. Relationship between vaginal microbial dysbiosis, inflammation, and pregnancy outcomes in cervical cerclage. Sci Transl Med 2016; 8: 350ra102. [DOI] [PubMed] [Google Scholar]
- 11. Yoshimura K, Morotomi N, Fukuda K, Hachisuga T, Taniguchi H. Effects of pelvic organ prolapse ring pessary therapy on intravaginal microbial flora. Int Urogynecol J 2016; 27: 219–227. [DOI] [PubMed] [Google Scholar]
- 12. Kindinger LM, Bennett PR, Lee YS, Marchesi JR, Smith A, Cacciatore S, Holmes E, Nicholson JK, Teoh TG, MacIntyre DA. The interaction between vaginal microbiota, cervical length, and vaginal progesterone treatment for preterm birth risk. Microbiome 2017; 5: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Goya M, Pratcorona L, Merced C, Rodo C, Valle L, Romero A, Juan M, Rodriguez A, Munoz B, Santacruz B, Bello‐Munoz JC, Llurba E, Higueras T, Cabero L, Carreras E, Pesario Cervical para Evitar Prematuridad Trial Group . Cervical pessary in pregnant women with a short cervix (PECEP): an open‐label randomised controlled trial. Lancet 2012; 379: 1800–186. [DOI] [PubMed] [Google Scholar]
- 14. Nicolaides KH, Syngelaki A, Poon LC, Picciarelli G, Tul N, Zamprakou A, Skyfta E, Parra‐Cordero M, Palma‐Dias R, Rodriguez Calvo J. A randomized trial of a cervical pessary to prevent preterm singleton birth. N Engl J Med 2016; 374: 1044–1052. [DOI] [PubMed] [Google Scholar]
- 15. Saccone G, Maruotti GM, Giudicepietro A, Martinelli P; Italian Preterm Birth Prevention (IPP) Working Group . Effect of cervical pessary on spontaneous preterm birth in women with singleton pregnancies and short cervical length: A randomized clinical trial. JAMA 2017; 318: 2317–2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hui SY, Chor CM, Lau TK, Lao TT, Leung TY. Cerclage pessary for preventing preterm birth in women with a singleton pregnancy and a short cervix at 20 to 24 weeks: A randomized controlled trial. Am J Perinatol 2013; 30: 283–288. [DOI] [PubMed] [Google Scholar]
- 17. Sharp AN, Alfirevic, Z . Provision and practice of specialist preterm labour clinics: a UK survey of practice. BJOG 2014; 121: 417–421. [DOI] [PubMed] [Google Scholar]
Supporting information
Figure S1 Kaplan–Meier survival curves demonstrating preterm birth probability in 258 women with short cervix included in intention‐to‐treat analysis, according to classification of previous spontaneous preterm birth (sPTB) and treatment. IM, intact membranes; PPROM, preterm prelabor rupture of membranes.
Table S1 Demographics and pregnancy outcome of 258 women with short cervix and previous preterm labor (PTL) with intact membranes or preterm prelabor rupture of membranes, according to center and treatment
ACKNOWLEDGMENTS
We thank Dr Clara Murillo, Dr Carla Julia and Dr Silvia Escura from Hospital Universitari Vall d'Hebron for their assistance in obtaining data used in this study. No funding source was used in this study for their time.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Kaplan–Meier survival curves demonstrating preterm birth probability in 258 women with short cervix included in intention‐to‐treat analysis, according to classification of previous spontaneous preterm birth (sPTB) and treatment. IM, intact membranes; PPROM, preterm prelabor rupture of membranes.
Table S1 Demographics and pregnancy outcome of 258 women with short cervix and previous preterm labor (PTL) with intact membranes or preterm prelabor rupture of membranes, according to center and treatment


