Abstract
In the Democratic Republic of Congo, 43% of children under 5 years of age suffer from stunting, and the majority (60%) of children, 6–59 months of age, are anaemic. Malaria, acute respiratory infections, and diarrheal diseases are common among children less than 5 years of age, with 31% of children 6–59 months affected by malaria. This qualitative implementation science study aimed to identify gaps and opportunities available to strengthen service delivery of nutrition within integrated community case management (iCCM) at the health facility and community level in Tshopo Province, Democratic Republic of Congo, through the following objectives: (a) examine cultural beliefs and perceptions of infant and young child feeding (IYCF) and child illness, (b) explore the perspectives and knowledge of facility‐based and community‐based health providers on nutrition and iCCM, and (c) gain an understanding of the influence of key family and community members on IYCF and care‐seeking practices. This study involved in‐depth interviews with mothers of children under 5 years of age (n = 48), grandmothers (n = 20), fathers (n = 21), facility‐based providers (n = 18), and traditional healers (n = 20) and eight focus group discussions with community health workers. Study findings reveal most mothers reported diminished quantity and quality of breastmilk linked to child/maternal illness, inadequate maternal diet, and feedings spaced too far apart. Mothers' return to work in the field led to early introduction of foods prior to 6 months of age, impeding exclusive breastfeeding. Moreover, children's diets are largely limited in frequency and diversity with small quantities of foods fed. Most families seek modern and traditional medicine to remedy child illness, dependent on type of disease, its severity, and cost. Traditional healers are the preferred source of information for families on certain child illnesses and breastmilk insufficiency. Community health workers often refer and accompany families to the health centre, yet are underutilized for nutrition counselling, which is infrequently given. Programme recommendations are to strengthen health provider capacity to counsel on IYCF and iCCM while equipping health workers with updated social and behavior change communication (SBCC) materials and continued supportive supervision. In addition, targeting key influencers to encourage optimal IYCF practices is needed through community and mother support groups. Finally, exploring innovative ways to work with traditional healers, to facilitate referrals for sick/malnourished children and provide simple nutrition advice for certain practices (i.e., breastfeeding), would aid in strengthening nutrition within iCCM.
Keywords: childhood illness, iCCM, implementation science, infant and young child nutrition, integrated community case management
Key messages.
While breastfeeding is valued, mothers', community members', and health providers' concerns on breastmilk insufficiency are linked to return to work, maternal nutrition, and maternal/child illness.
Complementary feeding practices are weak, with small amounts of food fed, limited dietary diversity and lack of information on meal frequency.
Targeting key influencers through community and mother support groups can aid in equipping caregivers with information on IYCF.
Building the capacity of facility and community level providers to counsel on preventative aspects of nutrition/IYCF is needed.
Engaging traditional healers who can provide nutrition advice and support referrals of sick and/or malnourished children is critical.
1. INTRODUCTION
The integrated community case management (iCCM) platform provides the opportunity to strengthen coverage for prevention and treatment of preventable causes of child deaths through expanding access to services and treatments and improving quality of and demand for these health services (Population Services International, 2014; Teferi, Alemu, Bulto, Ali, & Teno, 2014). ICCM guidelines have primarily focused on curative care, in terms of the identification, treatment, and referral of children who are ill with diarrhoea, pneumonia, and/or malaria. Although iCCM guidelines also incorporate nutrition components, including the identification of acute malnutrition (by measuring a child's mid‐upper arm circumference and the presence of bilateral pitting edema), immediate referral of severe acute malnutrition (SAM) cases, and guidance on the continued feeding of any sick child treated at home (Friedman & Wolfheim, 2014; WHO and UNICEF, 2012), yet the implementation of nutrition within iCCM—including preventative components—is often not delivered with the intensity, quality, and coverage needed to achieve improvements in child nutritional status (Wazny et al., 2014). A review of experiences and evidence on linkages between iCCM and nutrition revealed that iCCM's nutrition components need to be strengthened to improve the coverage and quality of services for sick children; optimize the preventive aspects of iCCM; improve implementation of the UNICEF/WHO iCCM package; and strengthen linkages between the community and health facility, while also linking health and nutrition at the institutional level (Friedman & Wolfheim, 2014). ICCM may increase reach and coverage for prevention and treatment of malnutrition among children (Friedman & Wolfheim, 2014). Strengthening nutrition services within iCCM can aid to improve infant and young child feeding (IYCF) and care practices, improve child nutritional status, and reduce rates of child morbidity and mortality.
The Democratic Republic of Congo (DRC) may substantially benefit from strengthening nutrition within the iCCM platform considering the lack of trained health care workers and difficult access to health care due to geographic constraints (as 35% of the population reside within 5 km of a health facility; MCHIP, 2012). Moreover, DRC, which has experienced political instability and war, has high rates of stunting and child mortality (104 per 1,000 live births), as approximately 43% of children under 5 years of age suffer from stunting and 8% of children are wasted and 23% are underweight (Ministry of Planning and Monitoring Implementation of the Revolution of Modernity & ICF Macro, 2014). Furthermore, the majority (60%) of children, 6–59 months of age, are anaemic (<11.0 g/dl; Ministry of Planning and Monitoring Implementation of the Revolution of Modernity & ICF Macro, 2014). Malnutrition is among the principal causes of childhood mortality in the DRC, in addition to malaria, acute respiratory infections, and diarrheal diseases (Ministry of Planning and Monitoring Implementation of the Revolution of Modernity & ICF Macro, 2014).
The national iCCM strategy in the DRC is an equity‐based approach to combat both child illness and undernutrition. In December 2005 (MCHIP, 2012), the Ministry of Health initiated iCCM for childhood illness, with a focus on treatment for malaria, acute respiratory infection, diarrhoea, and acute malnutrition, within national iCCM implementation guidelines developed in 2007, updates to policy in 2016 (revisions await finalization; Ministère de la Santé Publique 2007). In the DRC, critical gaps in iCCM include weak implementation of nutrition components, as (a) the current iCCM strategy does not sufficiently address preventive aspects as well as curative aspects of nutrition integration into iCCM (MCHIP, 2012), (b) curative support provided by health workers in the management of acute malnutrition was not always in line with WHO's protocol (WHO, 1999), (c) the nutrition component of iCCM is limited to screening for malnutrition, which includes identification, and referral, and treatment of SAM, and (d) provides brief guidance of continued feeding of sick children (Ministry of Health, 2007). The preventative aspects of nutrition, within iCCM guidelines, including strengthening IYCF practices around breastfeeding and complementary feeding and counselling skills of health providers at the community and facility level, may be neglected, because the main focus of the approach is treatment.
To date, in the DRC, there is a lack of evidence on beliefs, and perceptions related to infant and young child practices, child illness, and care‐seeking behaviours, as well as the advice on nutrition and child illness provided by health providers and key influential community members, which can inform on strengthening nutrition within iCCM in the DRC health system.
The aim of this study is to examine gaps and opportunities available to strengthen service delivery of nutrition into iCCM at the health facility and community level via the following objectives: (a) Examine cultural beliefs and perceptions that influence IYCF practices and care‐seeking behaviours for acute malnutrition and child illness among Congolese mothers; (b) explore the beliefs, perceptions, and knowledge of IYCF, in relation to child illness, of facility‐based and community‐based health providers, who provide advice and/or counselling on nutrition and iCCM; and (c) gain an understanding of the role key influential family and community members and any advice provided on nutrition practices for children less than 5 years of age, in relation to IYCF, child illness, and iCCM.
2. MATERIALS AND METHODS
2.1. Study design and site
Figure 1 presents the conceptual framework for this study, which is adapted from the WHO Framework on Child Stunting and previously published literature (J. Kavle et al., 2014; Stewart et al., 2013), which emphasizes the joint importance of exclusive breastfeeding (EBF) in the first 6 months, complementary feeding, and continued breastfeeding in children less than 2 years of age, within the context of other key factors, which are relevant to child stunting, including child illness, such as malaria, pneumonia, and diarrhoea—which are the components of iCCM. Addressing these factors are critical for strengthening nutrition programming around IYCF and iCCM (Stewart et al.). The conceptual framework illustrates how contextual factors, including cultural beliefs and norms of mothers' IYCF practices, care‐seeking behaviours given by key influential members of the community, including fathers, grandmothers, and traditional healers as well as facility and community‐based health providers should be addressed as part of iCCM. Italicized words in grey boxes reflect data presented in this paper.
Figure 1.
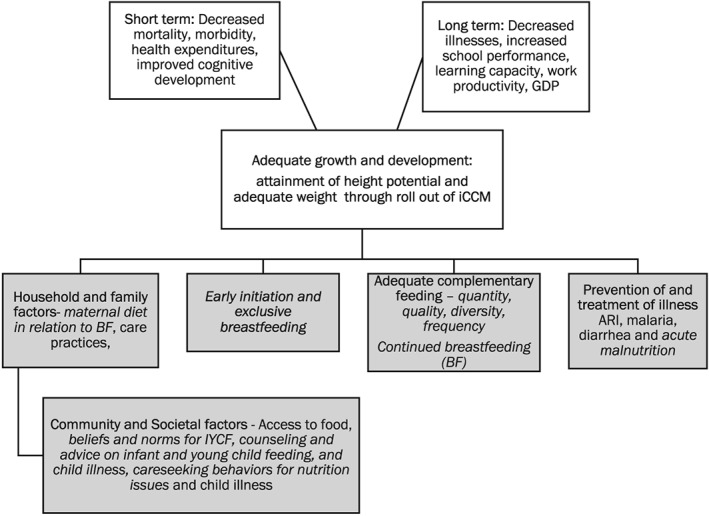
Conceptual framework of factors associated with iCCM, including IYCF practices and care seeking for child illness (Adapted from WHO Framework on Child Stunting, J. Kavle et al., 2014; Stewart, Iannotti, Dewey, Michaelsen, & Onyango, 2013). IYCF: infant and young child feeding; iCCM: integrated community case management
This study was implemented within the context of the Maternal and Child Survival Project (MCSP), the flagship project of the United States Agency for International Development on maternal, newborn, and child health. MCSP provided technical assistance to the government of the DRC to improve health service delivery of reproductive, maternal, newborn, and child health and nutrition interventions, including iCCM in 2015 (MCSP, 2017a).
The four study sites reflect MCSP implementing sites in Yaleko, Yakusu, Ubundu, and Bengamisa health zones in Tshopo District. These health zones were chosen to be regionally representative of the diversity in sociodemographic characteristics of the population, including religion, ethnicity, culture, and geography, which can influence on nutrition and child health practices. Tshopo Province is an agricultural rural region in the DRC, with three fourths of the population (6.6 million) considered (UNDP DRC, 2009; World Bank, 2008).
Fieldwork occurred between January and March 2017. These qualitative implementation science study conducted in‐depth interviews were conducted with mothers (N = 48, years of age) with children under age 5, fathers (N = 21) of children under age 5, and grandmothers (N = 20; Table 1). In‐depth interviews were also conducted with facility‐based health providers (i.e., doctors or nurses; N = 18) who provided nutrition and child health services in health centres or health posts, which were public (i.e., government) or private (i.e., mission) and traditional healers (n = 20). Focus group discussions (FGDs) were conducted with a mix of male and female relais communautaire (RECOs; community health workers [CHWs]) that provided counselling on nutrition and treatment for iCCM. Study participants were selected by purposeful sampling. Exclusion criteria for mothers, grandmothers, and fathers of children 6–59 months of age were non‐residents of study sites in Tshopo Province and study participants who are outside the following age ranges: mothers at least 15 years of age, grandmothers at least 38 years of age, and fathers at least 18 years of age. Health providers, defined as doctors or nurses, who that do not provide nutrition or child health services, who work outside of study sites, Tshopo Province, or who work in non‐MCSP supported health facilities were excluded. Non‐facility‐based service providers (CHWs) and traditional healers who work outside of Tshopo Province, or who work in nonsupported MCSP study sites were excluded. We used consolidated criteria for reporting qualitative research (Tong, Sainsbury, & Craig, 2007).
Table 1.
Descriptive characteristics of participants by site (family members)
| Index child sex | Index child age (months) | Age range (years) | Total number of children | Highest level of education obtained | Occupations | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | 0–5 | 6–23 | 24–59 | 1–2 | 3–5 | >5 | <Primary | Primary | Second+ | |||
| Mothers | |||||||||||||
| Bengamisa (N = 12) | 4 | 8 | 4 | 4 | 4 | (16–30) | 6 | 5 | 1 | 1 | 10 | 1 | Farmer |
| Ubundu (N = 12) | 8 | 4 | 4 | 4 | 4 | (19–37) | 3 | 7 | 2 | 1 | 6 | 5 | Farmer, student |
| Yakusu (N = 12) | 7 | 5 | 4 | 4 | 4 | (18–42) | 2 | 6 | 4 | 1 | 9 | 2 | Farmer, small trade |
| Yaleko (N = 12) | 6 | 6 | 4 | 4 | 4 | (16–39) | 4 | 6 | 2 | 0 | 6 | 6 | Farmer |
| Total (N = 48) | 25 | 23 | 16 | 16 | 16 | (16–42) | 15 | 24 | 9 | 3 | 31 | 14 | ‐‐ |
| Fathers | |||||||||||||
| Bengamisa (N = 5) | 2 | 3 | 0 | 4 | 1 | (22–37) | 2 | 2 | 1 | 0 | 1 | 4 | Farmer, student |
| Ubundu (N = 5) | 4 | 1 | 0 | 2 | 3 | (32–59) | 0 | 1 | 4 | 0 | 4 | 1 | Farmer, local chief |
| Yakusu (N = 5) | 2 | 3 | 1 | 2 | 2 | (25–53) | 1 | 2 | 2 | 0 | 2 | 3a | Farmer |
| Yaleko (N = 6) | 2 | 4 | 0 | 2 | 4 | (22–44) | 1 | 5 | 0 | 0 | 1 | 5 | Farmer, driver |
| Total (N = 21) | 10 | 11 | 1 | 10 | 10 | (22–59) | 4 | 10 | 7 | 0 | 8 | 13 | ‐‐ |
| Grandmothers | |||||||||||||
| Bengamisa (N = 5) | 4 | 1 | 1 | 0 | 4 | (49–58) | ‐‐ | ‐‐ | ‐‐ | 4 | 1 | 0 | Farmer |
| Ubundu (N = 5) | 4 | 1 | 0 | 2 | 3 | (49–61) | ‐‐ | ‐‐ | ‐‐ | 1 | 4 | 0 | Farmer |
| Yakusu (N = 5) | 2 | 3 | 1 | 1 | 3 | (45–53) | ‐‐ | ‐‐ | ‐‐ | 2 | 3 | 0 | Farmer |
| Yaleko (N = 5) | 4 | 1 | 1 | 3 | 1 | (49–63) | ‐‐ | ‐‐ | ‐‐ | 2 | 3 | 0 | Farmer |
| Total (N = 20) | 14 | 6 | 3 | 6 | 11 | (45–63)b | ‐‐ | ‐‐ | ‐‐ | 9 | 11 | 0 | ‐‐ |
One father had a graduate education.
Seven grandmothers did not know their age and are not included in averages.
Each mother also participated in a food frequency questionnaire that asked information on foods consumed by her child on a daily and weekly basis. Data collection occurred during the dry season (February–March 2017) of agricultural production, during which many villagers fished or found other sources of economic activity while awaiting harvest of their crops (June–September 2017). Dietary staples across all four zones included starchy foods (e.g., kwanga, lituma, and fufu) made from tubers, other starches (e.g., cassava, plantain, and maize), and beans (vigna).
Congolese study personnel were trained on research ethics, informed consent, privacy/confidentiality, key techniques related to qualitative data collection, and data storage. Verbal consent was obtained from all participants involved in interviews and FGDs, and participants were also provided with copy of the consent form (in French, Swahili, or Lingala) before audio‐recording interviews and FGDs in local languages (Swahili or Lingala). Study procedures were approved by the Institutional Review Board at John Snow Inc., the Kinshasa School of Public Health (DRC), local government authorities in Kisangani (Provincial Health Office and local representatives of the National Nutrition Program—PRONANUT), and village chiefs from study communities.
2.2. Analyses
Analysis of qualitative and quantitative data from the study were informed by the adapted WHO conceptual framework (Figure 1). This framework guided identification of dominant themes in the data. Audio‐recorded in‐depth interviews and FGDs were transcribed into French by four qualitative researchers (R. B., O. S., M. T., and J. M.).
Transcripts were analysed iteratively with the collaboration of Bukavu‐based researchers, Kisangani‐based study coordinators, Washington, DC‐based primary investigators, and remotely based qualitative research consultants (J. K., M. P., S. D., E. M., J. A., J. M., M. T., O. S., L. G., and S. S.). We conducted preliminary analyses to identify overarching themes and construct a coding structure. Following several iterations, a final codebook was formed. All interview and FGD transcripts were coded by two study team members (L. G. and S. D.), who used NVivo 11 software (QSR, 2015). During the coding process, the coders discussed and confirmed any emergent themes and resolved any areas of discrepancy with other research team members (J. K., M. P., S. D., L. G., and S. S.). Preliminary findings were shared with the national and subnational stakeholders in workshops in Kinshasa on November 30, 2017, and in Kisangani on December 5–6, 2017, respectively. Workshop attendees discussed implications of findings for strengthening nutrition within iCCM, and food frequency data were triangulated with qualitative data.
3. RESULTS
3.1. Characteristics of the participants
Mothers had similar demographic characteristics across the four health zones (Table 1). Most mothers (65%, n = 31) had a primary school education, whereas fathers had secondary education. Most mothers and fathers worked as farmers and had between three and five children. Grandmothers had either no formal education or primary education. Various cadres of health personnel participated in the study included RECOs (N = 56), traditional healers (N = 20), nurses (N = 15), doctors (N = 2), and a medical receptionist (N = 1; Table 1).
3.2. Themes
The following dominant themes emerged: Infant Feeding Behaviours; Child Feeding Behaviours; Community Perceptions About Child Health, Nutrition, and Illness; Care‐seeking Behaviours; and Roles in Provision of Services for Child Health and Nutrition. In this study sample, there was little variation among women with various educational levels. All text in quotation marks indicates direct quotes by study participants.
4. BREASTFEEDING PRACTICES
4.1. Mothers initiate breastfeeding early and give colostrum as advised by health providers yet lack understanding of the importance of the “first milk”
Most mothers reported early initiation of breastfeeding yet frequently did not remember when breastfeeding commenced. A few mothers who did not initiate breastfeeding early discussed the following reasons for delaying initiation: “The baby is sleeping, the baby was moved to a different room following childbirth and the baby didn't cry and wasn't ready to nurse,” and the “breastmilk was not coming out.”
Facility‐based and community health providers' advice strongly influenced mothers' decisions to initiate breastfeeding within 1 hr of birth and give colostrum. Nearly all mothers fed infants colostrum, yet many could not describe the importance and benefits of this practice.
As one mother from Ubundu tried to explain: “Um, it's because, well … I don't really have clear information, but I've heard that it contains vitamins.”
A minority of women said they did not give colostrum because it was “poor quality” breastmilk that “wasn't clean.” Generally, mothers, fathers, and grandmothers affirmed the importance of EBF until 6 months and stated they were specifically instructed to do so at the hospital
They taught us at the hospital to breastfeed the child for six months, and that the child shouldn't drink water and should exclusively drink mother's milk.—Mother, Bengamisa
4.2. Impediments to EBF: Breastmilk quantity and quality affected by illness, maternal nutrition, time between breastfeeding sessions, and mothers' return to work
Perceptions of the sufficiency of breastmilk to nourish infants varied among study respondents. Some community members said that mothers had no issues with the quantity of breastmilk, as evident by breastfeeding mothers' large and swollen breasts, whereas others said that mothers faced problems producing enough breastmilk to feed their infants. RECOs frequently discussed the importance of breastfeeding yet also echoed mothers' concerns of inadequate breastmilk supply.
We say this: “From zero to 6 months, the child must be exclusively breastfed with mother's milk. The mother mustn't lack milk in her breasts, and the child must breastfeed on demand, because mother's milk contains the nutrients that God prepared for the child during this period.”—RECO, Ubundu
4.3. Maternal illnesses believed to be “transmitted” through breastmilk contributed to poor quality breastmilk and were treated by traditional healers
Maternal illness, such as Kunde (a commonly cited illness that mothers can transmit to their babies through breastfeeding), was thought to cause painful breastfeeding through swollen breasts/sores on the breasts, and negatively affect the quality of the breastmilk. Kunde and other illnesses experienced by mothers such as Fota itoko (a febrile syndrome that is transmitted to children when breastfeeding mothers eat certain foods) and sanga (a condition that may occur in breastfeeding mothers who become pregnant and transmit the illness through breastmilk to her breastfeeding child), causing him or her to be malnourished or unable to walk until the mother gives birth, were believed to be transmitted to children through breastmilk.
As one RECO from Bengamisa explains
Kunde blocks the breastmilk from coming out … and sometimes make it comes out like water of a very white color. Or sometimes the milk isn't light and comes out in strings. These cases need to be treated so as to produce high‐quality milk to feed the child …. [Kunde is treated] only with traditional medicine. … all you need to do is drink our “Bakeke” tea …—A RECO from Bengamisa
4.4. Maternal nutrition influences breastmilk quality for some Congolese mothers
Whereas some mothers stated they “ate everything that was available,” others said certain foods were avoided to prevent “infecting the breastmilk” and causing diarrhoea in children. Foods considered taboo for breastfeeding mothers included game meat (e.g., snake, monkey, and crocodile), sugar cane, pineapple, mango, and sweet potato leave.
Maternal consumption of specific foods, such as sombé (a dish of cooked cassava leaves) and Cowbell (a drink made from powdered milk mixed with water), were frequently cited as beneficial to produce high amounts of good quality, “thick,” and “white” breastmilk.
Many RECOs, health workers, and family members expressed that mothers may have insufficient food to eat due to economic constraints. Economic constraints were stated to be made worse if mothers did not return to work in the fields during the first 6 months after childbirth. Mothers were pressured by community members, including RECOs, to leave the infant at home while she is/was in the fields, so the mother was less available to feed her breastfeeding child. As one RECO relayed
Life has become expensive – there's no longer the means to eat well to breastfeed the child. Because if the mother eats well, then the child eats well.—RECO, Yakusu
4.5. Time between feedings influences breastmilk quality
Mothers work primarily as farmers, spending long hours cultivating crops, alongside fathers, who also hunted or fished (Table 1). Work in the fields, as a cause of poor quality breastmilk and diarrhoea in children, was commonly mentioned by mothers, fathers, and traditional healers, due to long periods of time between breastfeeding sessions (at times greater than 12 hr, according to a traditional healer from Yaleko).
When you leave a lot of time between feedings, at that time, the [breast] milk becomes water. That's why I tell her that she needs to come back a bit earlier from the fields to feed the child while the milk is still of good quality.—A father of a 2‐year‐old daughter from Bengamisa
4.6. Early introduction of foods prior to 6 months of life addresses perceptions of insufficient breastmilk for some Congolese women
Mothers' need to return to field work and absence for long periods was the primary reason for early introduction of foods before 6 months. Other family members (i.e., older children and grandparents) often fed the child soft foods (i.e., bouille) to soothe its cries of hunger and to provide sufficient nourishment to the child (i.e., to prevent anaemia) if the mother's breastmilk is not perceived to be of good quality.
If the mother knows that her breasts are not in good health and able to furnish the child with breastmilk, she is obliged to associate liquid foods so that the child doesn't become anemic.—A traditional healer from Yaleko
Other reasons for early introduction of foods included the mother's inability to breastfeed because of tiredness or hunger from the energy expended by breastfeeding, and the child displaying signs of dissatisfaction with breastmilk (e.g., crying, sitting up, reaching towards food, and refusing to breastfeed). The most commonly introduced first food was bouillie, which is locally defined as a thin, watery term for porridge prepared with palm oil and flour of soy, plantain, cassava or corn, or occasionally biscuits (i.e., cookies), as well as variable amounts of sugar. It is introduced in small amounts bit by bit between 3 and 6 months of age.
[Bouillie] satisfied him, just as we mothers do, when he's 4 months old you start to give him food. If he starts to cry a lot it means that mother's milk isn't enough for him anymore, so you give him bouillie to drink.—A mother of three children under age 5 from Yakusu
5. CONTINUED BREASTFEEDING AND COMPLEMENTARY FEEDING PRACTICES
Most mothers said they would continue breastfeeding for 2 years or more. Breastfeeding may end earlier (before the child reaches 2 years of age) if the mother becomes pregnant again. Other reasons for stopping breastfeeding prior to 2 years of age are (a) the mother's need to go work in the fields, (b) the mother is tired of breastfeeding or hungry due to additional energy expended by breastfeeding, or (c) the child showed signs of no longer being satiated or refused the breast.
5.1. Soft foods introduced early hard foods after 7 months
Bouillie and other foods were introduced “bit by bit” in small portions until the child displayed signs, for example, frequent crying that bouille no longer satisfied his/her appetite. At this time, caregivers often introduced “soft” foods first (e.g., beans, fish, fufu, and sombé), followed by “hard” foods (e.g., meat, cassava, plantain in lituma form, kwanga, and rice) when the child reached 7–10 months of age. Soft foods were frequently introduced early because they were perceived to be easily digestible for young children. On the other hand, hard foods were perceived as difficult for young children to digest until they developed teeth and/or stomachs sufficient to do so.
5.2. Children consume primarily carbohydrates and fruits and vegetables, yet in small quantities
Daily food frequency in children 6–59 months old shown in Figure 2 indicated children's diets in Tshopo Province were predominately fruits and vegetables, which comprise 34% of foods consumed on a daily basis (inclusive of fruits and vegetables rich in vitamin A). Carbohydrates, such as tubers (i.e., cassava, and potatoes), as well as thin, watery porridge, and watery soups with small bits of meat, are main features of the Congolese diet of young children. Daily intake of red meat was 8% of all daily foods.
Figure 2.
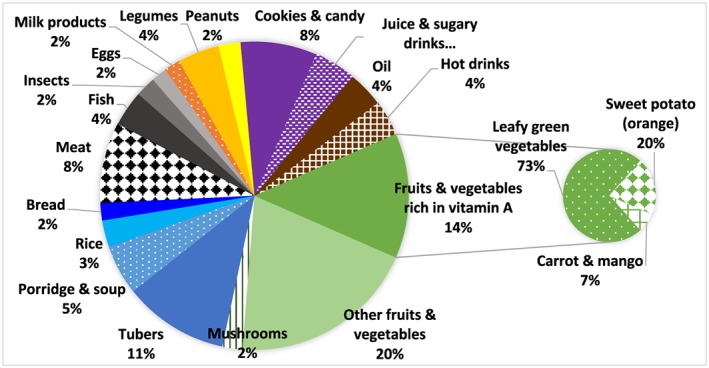
Daily food frequency children, 6–59 months of age (N = 36)
Foods are often prepared in larger quantities for families in large pots and pans—though amounts of foods, consumed on a daily basis, were small (i.e., bits of meat in watery soup). At times, the amount of food consumed by children were difficult to quantify, given that a small amount of food may be aside for the child for consumption throughout the day.
Children are like animals – if they see [food] pass them by, they will ask for it and we'll bring it to them. [Smiles]—Mother, Yakusu
While the child's mother is away in the fields, she/he feeds by his/herself or with the help of other relatives or older children in the household. However, the child's older siblings (or cousins, or other children living in the household) may eat from this plate as well, because it is often their job to feed/care younger children. Because mothers are not always the caretakers for young children, it was also difficult to estimate the number of meals children are fed each day (i.e., to compute minimum meal frequency).
Food frequency data indicate that of all foods eaten two to three times per week, animal source foods are consumed with varying frequency on a weekly basis, though in small quantities (39–74% of children consumed animal source foods, such as chicken, fish, pork, eggs, and goat, with chicken and fish most frequently consumed). Sugary biscuits, sweets/candies, and sweetened and caffeinated beverages are a notable part of young children's diets (with consumption of 12–36 g, equivalent to up to one‐fourth cup; Figure 3). Biscuits may sometimes be added to porridge or tea and can be fed at meal times, rather than just as a snack. Further, it was noted that as a child gets older, greater quantities of foods are fed to the child (closer to the upper range), yet these amounts are likely to not be sufficient for those children under 5 years of age (Table 2).
Figure 3.
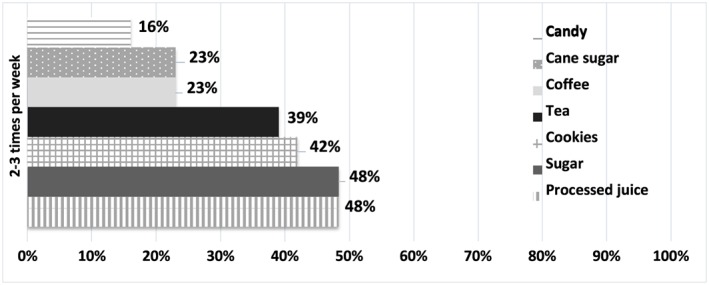
Percentage of foods consumed at least two to three times per week that are processed “junk” foods or warm/sweet beverages, by children 6–59 months
Table 2.
Estimated quantity of food consumed by food item (range in grams), children 6–59 months of age, according to 24‐hr recall, Tshopo Province, DRC
| List of foods | Typical quantities of food consumed, children 6–59 months |
|---|---|
| Papaya | 45–270 g |
| Amaranth | 20–250 g |
| Spinach | 100–200 g |
| Manioc leaves | 20–200 g |
| Banana | 25–500 g |
| Eggplant | 10–20 g |
| Soup (with a bit of meat) | 8–70 ml |
| Chicken/beef/fish | 20 g |
| Eggs | 25–50 g (0.5–1 egg) |
| Beans | 20–80 g |
| Manioc | 75–250 g |
| Sugary biscuits | 12–36 g |
Note. *1/4 cup = 37.5 g; 1/3 cup = 50 g; 1/2 cup = 75 g; 1 cup = 150 g.
5.3. Grandmothers and older siblings play a role in feeding young children, while fathers advise mothers
Family members played a range of roles with regard to infant feeding (Table 3). Fathers gave general advice and fed children when mothers were away and/or working in the fields. Grandmothers regularly provided advice on caring and feeding children and fed the children when the mother was away in the fields (Table 3). Older siblings fed young children more often than the family members. However, some community members stated that siblings may not have taken their responsibilities seriously.
You can say to the mother: “Are you going to the forest? You'll leave the children with whom?” “Oh, his older brothers, his older sisters.” Can these children take care of these other children? Well often they say they do a good job taking care of the children, but it doesn't always go so well … These [older] children, either they play, or do something else, some go to school, and sometimes they forget too.—Nurse, Yaleko
Table 3.
Roles of fathers and grandmothers in care and feeding of children less than 5 years of age, Tshopo province, DRC
| Fathers | Grandmothers |
|---|---|
| Care seeking | |
|
|
| Feeding | |
|
|
6. CARE‐SEEKING PATTERNS FOR ACUTE MALNUTRITION AND CHILD ILLNESS
6.1. Pathway of treatment for child illness dependent on whether defined as traditional illness or “white man's disease”
Among family members' roles in seeking the appropriate course of treatment (Table 3), families first decided whether their child's illness fell under the category of traditional, local illnesses, or “white man's disease.” Illnesses described by Western medicine, such as diarrhoea, malaria, fever, cough, and acute malnutrition were locally categorized as “white man's diseases,” which respondents affirmed existed in their communities (Table 4). These diseases often coexisted with “traditional” illnesses that could have spiritual or organic causes. Ideally, “white man's diseases” were perceived to be best treated by Western medicine, whereas local illnesses should be treated with traditional medicine.
Table 4.
Description of symptoms, associated diseases and care‐seeking options for common child illnesses in Tshopo Province, DRC
| Symptom | Diseases associated with | Home treatment (traditional/modern) | Treatment from traditional healer | When/why to go to the health centre/RECO |
|---|---|---|---|---|
| Lack of appetite |
(Associated with any other illness) Intestinal worms |
Enemas Medicines from the pharmacy (“Super Apeti” tablets—cyproheptadine) Prayer |
Traditional medicines or examination to determine cause |
If the enema does not work With other symptoms If there is kwashiorkor |
| “Lack of blood” |
Anaemia Poor growth |
Improved nutrition: sombé; fish; mixture of eggs, tomato and sodas (i.e., soft drinks) Plant‐based medicine made from Kopele bark (resembles blood) Burnt sugar mixed with water |
Traditional plant‐based medicines Prayer |
To do exams to understand the cause If traditional treatments fail To get an injection |
| Fever (“hot body”) | Malaria general sign of illness |
Cold bath Enema with leaves (sometimes also applied to body) or with lemon Paracetamol |
Enemas, herbal treatments (if Fota itoko) Prayer to deliver him from spirits |
To do the “test” (RDT)—many say “only the hospital can treat malaria” After 2–3 days with no improvement |
| Cough (usually with fever) |
Pneumonia Fota itoko (esp. without fever, with anal sores) Kafeke (with fast breathing) |
Herbal treatment made from reeds (Roseau), wild onion and mango tree leaves (for cough without fever) Bactrim (antibiotic) and chloramphenicol (for cough with fever) |
Scarification with powder from kobukobu plant + fish head (for pneumonia/Kafeke) Prayer to deliver him from spirits |
After 2–3 days with no improvement If the cause is modern, not spiritual With fast breathing (sometimes) With difficulty breathing |
| Diarrhoea |
Infectious causes Fota itoko (with sores on anus) Malaria Malnutrition |
Papaya or kamba leaves, tree bark, other plant‐based treatments Enemas (e.g., for worms) or with lemon for Fota itoko Medicines from pharmacy (chloramphenicol) |
Further plant‐based treatments (oral or administered by enema) Scarification around the navel (if Fota itoko) |
For severe cases After 2–3 days with no improvement To get “serum” oral rehydration salts |
| Convulsions | Lonyama | Placing the head of the child above the latrine to revive him | Liquid from leaves is placed in the child's eyes so his “gaze returns to normal” | Modern treatment may be sought after traditional treatment, however this is generally seen as an illness with spiritual causes |
Note. RECO: relais communautaire.
As one mother states
If it's a disease that has to do with traditional medicine, I go to the healer. If it's a modern disease, I go to the closest medical facility … I know [which type of disease it is] by looking at the child.—A mother of a one‐month‐old daughter from Bengamisa
6.2. Acute malnutrition is recognized, emphasized, and prioritized by families and health providers, yet there is a lack of awareness of stunting
Mothers, grandmothers, and community members, who were asked about children's “poor growth,” mentioned recognizing clinical signs of acute malnutrition.
Although recognized, acute malnutrition was rarely reported by family members as affecting their own children. Although child stunting was more prevalent, it was not discussed and potentially not recognized by families and communities. Respondents tended to refer to childhood malnutrition only as “poor diet” or “poor appetite” as a sign of some other illness or of more severe visible forms of malnutrition, such as kwashiorkor, which was generally mentioned as occurring after the onset of another illness.
Families may be less likely to seek care for less severe forms (i.e., stunting) versus more severe forms of malnutrition (i.e., kwashiorkor) but for distinct reasons. Clinical signs of SAM, often referred to as “kwashiorkor”—locally defined as a severe form of malnutrition, caused by lack of food or neglect of children or “lack of blood”/anaemia—were mentioned by many interviewees (i.e., mothers, grandmothers, and fathers). Kwashiorkor is formally defined as a type of protein energy malnutrition, characterized by clinical signs such as edema, anorexia, irritability, skin pigmentation/discoloration, and discoloured/thin hair (Waterloo, 1997; Wellcome Trust Working Party, 1970). In line with the formal definition of clinical acute malnutrition (kwashiorkor), community members relayed that kwashiorkor occurred when the child did not have enough to eat and experienced bad growth and described its symptoms (distended belly, discoloured hair, swelling, etc.).
The sign of bad growth is when a child hasn't eaten well, that's a bad sign; he'll have kwashiorkor because of this bad sign.—Father, Bengamisa
Thus, community members seem to have integrated the (medical) term kwashiorkor into local languages and do recognize it as a troubling sign of malnutrition (or “poor growth”). Acute malnutrition was most often associated with another illness. Families also sometimes spoke of their children as having a “lack of blood,” signifying anaemia.
Families may not recognize stunting because stunting is prevalent, and they tend to measure their children's growth by comparing their size to other children, often not noting a difference. On the other hand, while families recognize signs of acute malnutrition (i.e., SAM) such as changes in hair and skin colour, families may not seek care due the shameful nature of the illness. Still, despite this stigma, some families still seek care, and whereas some said kwashiorkor was a case for Western medicine, others said it could only be treated by traditional healers. Traditional healers themselves disagreed on how SAM should be treated.
If it's kwashiorkor, I say go to the medical center, because this disease goes beyond my abilities … Kwashiorkor is reserved for modern medicine.—Traditional healer, Yaleko
Modern medicine can't treat malnutrition. Only I can treat malnutrition.—Traditional healer, Bengamisa
When families recognize signs of “poor growth,” such as listlessness or lack of appetite, or clinical signs of acute malnutrition, they tend to provide improved nutrition (more food and/or more nutritious/appetizing food), take special care with hygiene, and give enemas and plants to stimulate the appetite. Families said severe cases required medical care, yet were sometimes limited in their means to go to the health centre. Yet they were also incentivized to seek care at health centres because diagnosed malnutrition cases were provided with free supplies of supplementary foods (i.e., Plumpy'Nut) to take home, along with follow‐up care. It is also possible that families sought care for acute malnutrition after interpreting malnutrition as a symptom of another illness.
At the hospital they'll examine him to see why he's not eating.—Grandmother, Yakusu
7. TRADITIONAL HEALERS, RECOS, AND HEALTH PROVIDERS HAVE A ROLE IN PROVISION OF NUTRITION ADVICE, COUNSELLING AND/OR TREATMENT
Regardless of the illness, the course of treatment for many families was defined by financial means. Although national policy is supposed to provide free care for all children under age 5, respondents affirmed that this was not true in all regions. Financial barriers were stated by community members as challenging or impossible for economically strained families to obtain treatment at health centres, which results in seeking care of traditional healers or self‐medication.
Traditional healers are often the first health providers consulted when a child falls ill and fails to improve with home treatment. Traditional healers were more appealing and accessible to families, as they provided more flexible hours and payment plans compared with modern health care providers and were located directly in the community. They also provide culturally appropriate care to families and were ranging from herbal remedies to prayers to “chase the demons” (Table 4).
With respect to nutrition, breastfeeding practices, and perceptions around transmission of certain illness through breastmilk, the traditional healer has the primary role of providing treatment of Kunde. As mentioned above, Kunde is a preoccupation of no small number of breastfeeding mothers.
I treat Kunde, I put herbs on [the child's] fingernails and on her eyes. I also put it on the mother, because the mother is the one who's contaminated with this disease. Because when the child is suckling from her mother that she becomes contaminated. The child isn't born with Kunde, she gets it from her mother.—Traditional healer, Bengamisa
Traditional healers also occasionally provide advice on appropriate foods for breastfeeding mothers to eat and for young children (i.e., avoidance of taboo foods, and/or consumption of Bakeke tea or mbochi leaves to stimulate breastmilk production).
7.1. Gap between RECOs' supposed roles and roles reported by families for nutrition
RECOs are often consulted next or at the same time as traditional healers. Two different types of RECOs are available to provide counselling and care on child illness (MCHIP, 2012). First, “RECO sites,” based at sites in villages, receive formal training to diagnose and treat basic childhood illnesses such as those included under iCCM. RECO promotionnels are meant to visit villagers' homes to provide advice on feeding and caring for young children and recognize danger signs. They are also trained to conduct health‐related communication activities and mobilization in their communities.
Yet a significant gap exists between the services that RECOs are supposed to provide (and many relayed they did provide) and those reported by community members. For example, when prompted, few family members said they recently received a home visit by a RECO, which conflicted with RECOs' recounting of their regular schedules for home visits. Home visits were only reported for vaccines (often for polio), with few, if any visits on nutrition counselling. As one mother from Yakusu relayed, “They (RECOs) didn't give any advice – they just come to give the children the vaccine, and then they leave.”
According to RECOs themselves, the advice provided to families regarding child health, illness, and nutrition was limited and included (a) to prevent disease via vaccination, use of bednets, handwashing, etc., (b) to provide a healthy, balanced, and hygienically prepared diet for children, and (c) to bring sick children to the health centre. A typical statement by a RECO on the topic of prevention was the following:
If a child suffers from malnutrition … it can be due not only to hunger, but to germs. So you advise the parent to protect the child from germs by washing his/her hands before eating. And the child shouldn't sleep in a bad place so as to protect from germs that could hurt his/her health.—RECO, Bengamisa
The nutrition advice provided to mothers and families by RECOs was general information, without specific advice tailored to IYCF practices, needs, or challenges. Whether during home visits or at the health centre, RECOs said they advised mothers and families to breastfeed exclusively for the first 6 months of life, practice good hygiene (wash hands, wash breasts before breastfeeding), give the child foods that are appropriate for his/her age, to go to health centre for difficulties with breastfeeding, and eat enough food/eat a balanced diet, to be able to breastfeed well.
However, these counselling activities do not appear to have reached families, and little is known about the content/quality of actual preventative nutrition counselling, whether in their homes (given the lack of evidence of home visits) or through other SBCC activities.
7.2. Care from facility‐based health providers as a last resort
Treatment from health providers at health centres was often a last option for families, following referral from traditional healers or RECOs. Health providers diagnosed and treated malnourished children and some cases provided influential information on nutrition and disease prevention. Yet in other cases, families reported wanting more health information from providers, which was not given to families. As one mother stated
Our service providers here don't give us advice on nutrition … the child had a lack of blood, they just injected him with a vial to bring back his blood.—Mother, 18‐month‐old child, Yaleko
8. DISCUSSION
To our knowledge, few data exist on identifying ways to strengthen nutrition services within the iCCM platform. This study explored perceptions, beliefs, and knowledge around IYCF practices, care‐seeking behaviours for acute malnutrition and child illness, and roles and advice given by health providers and traditional healers, which provide implications for nutrition–child health programming.
Our results indicate that although families and health providers viewed breastfeeding favourably, mothers and families linked the diminished quality and/or quality of breastmilk to inadequate maternal nutrition, various maternal, and child illnesses, as well as long periods of separation of mothers and infants, which impede EBF. Previous evidence corroborates these findings on insufficient breastmilk (J. A. Kavle, Lacroix, Dau, & Engmann, 2017). Observational studies have cited inadequacies in breastmilk supply as primary reasons for ceasing breastfeeding and introducing foods early to satiate infants, prior to 6 months of age (Afiyanti & Juliastuti, 2012; Mahmood, Srivastava, Shrotriya, & Mishra, 2012; Maman et al., 2012; MCSP, 2017b; Østergaard, Rosendal, & Bula, 2010; Suresh et al., 2014). In Kenya, mothers who believed they were producing sufficient breastmilk were significantly more likely to exclusively breastfeed than those who did not believe their breastmilk was sufficient (Matovu, Kirunda, Rugamba‐Kabagambe, Tumwesigye, & Nuwaha, 2008; MCSP, 2017b). Additionally, qualitative data from Eastern Uganda and Kenya have shown a link between mothers' perceptions of “eating well” and “sufficient amounts of food” with their perception of sufficient breastmilk production (Engebretsen et al., 2010; Kimani‐Murage et al., 2015; MCSP, 2017b). Congolese mothers in south Kivu, DRC, relayed that perceived reductions in breastmilk quantity were related to inability of mothers to consume enough food (Balaluka et al., 2012). In addition, most mothers faced financial challenges and stated nutrient‐rich foods such as meat, milk, fruits, and vegetables were prohibitive in cost to purchase for the family, which limited the diversity of children's diets as well.
Our data also reveal the need to strengthen capacity and skills of CHWs, who rarely conducted home visits on nutrition and/or child illness, with the exception of vaccinations. Although some facility‐ and community‐level health providers were reported to have been trained in IYCF, gaps in services remain due to lack of resources, SBCC materials, and a solid understanding of key nutrition counselling messages to provide families in the DRC (Linguissi et al., 2017; Maketa et al., 2013). At the community level, nutrition counselling on IYCF, as part of the iCCM, is critical to improving nutrition outcomes, according to recent evidence. Roll‐out of community‐based nutrition counselling through iCCM/integrated management of childhood illness (IMCI) can reduce stunting within resource‐limited settings (Reinhardt & Fanzo, 2014). In Rwanda, a “Nutrition Weeks” programme, part of the country's community‐based nutrition programme, provided information on the nutritional value of local foods and how to incorporate these foods into diets through counselling small groups of pregnant women. These messages were reinforced by CHWs during home visits and resulted in a 55% improvement in dietary diversity and meal frequency among children whose mothers took part in the intervention compared with those whose mothers did not (Friedman & Wolfheim, 2014; World Relief Innovation Child Survival Project Rwanda, 2014). Furthermore, an IMCI in Bangladesh that focused on improving EBF for the first 6 months was associated with a 7.3% decrease in child stunting (Arifeen et al., 2009).
Although our data indicate that preventative aspects of nutrition within iCCM (i.e., IYCF counselling) has largely been neglected, curative components of nutrition has been the focus of iCCM in the DRC. Our study findings showed that families and health providers primarily focused on the identification, referral, and treatment of children with acute malnutrition in the DRC. Several studies reported that correct referral and treatment for acute malnutrition within the context of strong community‐based health programmes can have an impact on cure rates. For example, community‐based management of malnutrition has been shown to improve service coverage and treatment outcomes for acute malnutrition in Sub‐Saharan Africa, with cure rates as high as 90% in Malawi (Maleta & Amadi, 2014). Community‐based management of malnutrition protocols have been adapted to treat acute malnutrition within the context of iCCM in several countries. For example, in Niger, CHWs who participated in the Rapid Access Expansion Programme increased their identification and referral of SAM cases from 94 to 392 over a 5‐month period (Concern Worldwide, 2009; Friedman & Wolfheim, 2014). Additionally, in Rwanda, trained CHWs who actively screened children for MAM and SAM using mid‐upper arm circumference and weight‐for‐age (underweight) measurement referred cases to respective health facility programmes (Concern Worldwide, 2009; Friedman & Wolfheim, 2014), which resulted in identification and treatment of over 8,000 cases of SAM and improved community awareness of and implementation of a national protocol for community‐based management of malnutrition (Concern Worldwide, 2009; Friedman & Wolfheim, 2014).
Although addressing wasting or acute malnutrition is an important feature of iCCM, both wasting and stunting generally coexist within populations yet are often overlooked by health providers. DRC has a high prevalence of stunting and wasting among children 12–23 months of age (Angood et al., 2016; Bergeron & Castleman, 2012; Khara, Mwangome, Ngari, & Dolan, 2018). Acute malnutrition is often viewed by stakeholders in government health systems as a disease, and emphasis of nutrition services has largely been placed on roll‐out of treatment (WHO, 1999; WHO/WFP/UNICEF, 2007), which has been a focus of the iCCM programme in the DRC.
Although few health programmes have been able to adequately address both acute malnutrition and stunting (Bergeron & Castleman, 2012), promoting adoption of practices for prevention, including improving the quality of local diets, IYCF practices, and reducing child illnesses (FANTA‐2, 2010; World Bank, 2006), is needed with the engagement of key influential family members who provide nutrition advice and feed young children, as well as working with trusted sources members of the community (i.e., traditional healer; Boxes 4 and 5). The emphasis on acute malnutrition, which affects few children, and lack of awareness of stunting, which affects nearly half of children, suggesting further work in the DRC is needed to focus efforts on prevention of all forms of malnutrition through the iCCM platform.
8.1. Strengths and limitations
The primary strength of this study is its role in providing robust mixed methodology data on the implementation and effectiveness of iCCM services in the DRC. We triangulated methods of data collection, as in food frequency, reinforced findings from our qualitative data, and vice versa. Moreover, the robust and in‐depth qualitative data collection included participation of a wide range of community members who played a role in child health and nutrition, rather than focusing solely on mothers or health providers. Although the study team collected data on food frequency, detailed 24‐hr recall dietary data would have provided more information on nutrient intake for young children. The consumption of meals in large pots for families to share resulted in difficulties with obtaining the information on number of meals consumed daily and quantity of foods consumed by young children. Other limitations include data collection in local languages of Swahili and Lingala but analysed in French, potentially introducing errors of interpretation, though we tried to minimize these via close collaboration with DRC‐based researchers, including in the study region.
8.2. Programme implications
We identified gaps in preventative aspects of nutrition within iCCM in this research and provided indications for how to harmonize services, protocols, and SBCC materials for nutrition and iCCM, to increase referrals, and to integrate and strengthen strategies for prevention and treatment of malnutrition experience by children under 5 years of age in the Tshopo Province of the DRC (Boxes 1 and 2). The integrated nutrition and iCCM package should build on study findings, and we present programme recommendations for the national and subnational level (i.e., provincial).
Box 1.
Recommendations for integration of findings at the national level
|
|
|
|
|
|
|
Box 2.
Recommendations for integration of findings at the provincial/health zone levels
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
9. CONCLUSION
This implementation science study provided information on the range of cultural beliefs, perceptions, and knowledge of families, health providers, and community members on IYCF practices and care‐seeking behaviours in relation to acute malnutrition and child illness in the DRC. Strengthening of preventative and curative aspects of nutrition within the iCCM platform requires addressing gaps in IYCF practices, strengthening health provider capacity and skills in nutrition counselling, and engaging key influential community members, including family members and traditional healers.
CONFLICTS OF INTEREST
We declare no conflict of interests. USAID provided review of the manuscript; authors had intellectual freedom to include feedback, as needed.
CONTRIBUTIONS
JAK conceptualized and led the writing of the paper. SD and LG carried out data analyses and contributed to writing of the paper. All authors contributed to data analyses and data interpretation. MP, EM, JA, JM, MT, OS, SS, and RB were involved in writing of paper, with MP providing significant input into drafts. All authors were involved in the decision to submit the paper for publication.
FUNDING
This publication is made possible by the generous support of the American people through the US Agency for International Development (USAID), under the terms of cooperative agreement number AID‐OAA‐A‐14‐00028. The contents are the responsibility of the MCSP and do not necessarily reflect the views of USAID or the United States Government.
Supporting information
Data S1 Supporting Information
Data S2 Supporting Information
ACKNOWLEDGEMENTS
We gratefully acknowledge the communities of Tshopo that participated in this study, as well as participation from key Ministry of Health personnel from the Provincial health offices in Tshopo, and Bas Uélé in interpretation of these findings.
Kavle JA, Pacqué M, Dalglish S, et al. Strengthening nutrition services within integrated community case management (iCCM) of childhood illnesses in the Democratic Republic of Congo: Evidence to guide implementation. Matern Child Nutr. 2019;15(S1):e12725 10.1111/mcn.12725
Footnotes
A RECO is a volunteer from a village or street, whose role is to facilitate a sustainable connection between community members and the health service. This study includes two types of RECO's: Relais promotionnels provide nutrition counselling for community members, whereas relais sites provide treatment of iCCM (MCHIP, 2012).
Breastfed children by 12 months of age require about one cup of food (150 g) per meal (with three recommended meals per day), according to global guidance from World Health Organization.
We use “Western” illnesses to refer to objectively measurable pathological conditions of the body, recognized by biomedicine. In contrast, local illness terms refer a feeling of not being normal or healthy, which can be caused by a disease or pathology, but which can also have spiritual origins. For more information on the difference between these terms, from Medical Anthropology Department at Palomar College: https://www2.palomar.edu/anthro/medical/med_1.htm
Liquid (i.e., plant solutions) introduced via the anus.
REFERENCES
- Afiyanti, Y. , & Juliastuti, D. (2012). Exclusive breastfeeding practice in Indonesia. British Journal of Midwifery, 20(7), 484–491. 10.12968/bjom.2012.20.7.484 [DOI] [Google Scholar]
- Angood, C. , Khara, T. , Dolan, C. , Berkley, J. A. , Roberfroid, D. , Seal, A. , & Kerac, M. (2016). Research priorities on the relationship between wasting and stunting. PLoS One, 11(5), 1–13. 10.1371/journal.pone.0153221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arifeen, S. E. , Hoque, D. E. , Akter, T. , Rahman, M. , Hoque, M. E. , & Begum, K. (2009). Effect of the integrated management of childhood illness strategy on childhood mortality and nutrition in a rural area in Bangladesh: A cluster randomised trial. Lancet, 374(9687), 393–403. [DOI] [PubMed] [Google Scholar]
- Balaluka, G. B. , Nabugobe, P. S. , Mitangala, P. N. , Cobohwa, N. B. , Schirvel, C. , Dramaix, M. W. , & Donnen, P. (2012). Community volunteers can improve breastfeeding among children under six months of age in the Democratic Republic of Congo crisis. International Breastfeeding Journal, 7, 1–8. 10.1186/1746-4358-7-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergeron, G. , & Castleman, T. (2012). Program responses to acute and chronic. Advances in Nutrition, 3(February), 242–249. 10.3945/an.111.001263.242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Concern Worldwide (2009). “Integrating community management of acute malnutrition into child survival programs: Concern worldwide's experience in Rwanda.”
- Engebretsen, I. M. S. , Moland, K. M. , Nankunda, J. , Karamagi, C. A. , Tylleskär, T. , & Tumwine, J. K. (2010). Gendered perceptions on infant feeding in Eastern Uganda: Continued need for exclusive breastfeeding support. International Breastfeeding Journal, 5, 13 10.1186/1746-4358-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- FANTA‐2 . (2010). “Title II technical reference materials. TRM‐01: Preventing malnutrition in children under 2 approach (PM2A): A food‐assisted approach.” Washington, D.C.
- Friedman, L. , and Wolfheim, C. 2014. “Linking nutrition and (integrated) community case management (iCCM/CCM): A review of operational experience.” London.
- Kavle, J. , Mehanna, S. , Saleh, G. , Fouad, M. A. , Ramzy, M. , Hamed, D. , … Galloway, R. (2014). Exploring why junk foods are ‘essential’ foods and how culturally tailored recommendations improved feeding in Egyptian children. Maternal & Child Nutrition, 11, 346–370. 10.1111/mcn.12165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavle, J. A. , Lacroix, E. , Dau, H. , & Engmann, C. (2017). Addressing barriers to exclusive breast‐feeding in low‐ and middle‐income countries: A systematic review and programmatic implications. Public Health Nutrition, 20(17), 3120–3134. 10.1017/S1368980017002531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khara, T. , Mwangome, M. , Ngari, M. , & Dolan, C. (2018). Children concurrently wasted and stunted: A meta‐analysis of prevalence data of children 6–59 months from 84 countries. Maternal & Child Nutrition, 14(2), 1–7. 10.1111/mcn.12516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimani‐Murage, E. W. , Wekesah, F. , Wanjohi, M. , Kyobutungi, C. , Ezeh, A. C. , Musoke, R. N. , … Griffiths, P. (2015). Factors affecting actualisation of the who breastfeeding recommendations in urban poor settings in Kenya. Maternal & Child Nutrition, 11(3), 314–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linguissi, L. S. G. , Gwom, L. C. , Nkenfou, C. N. , Bates, M. , Petersen, E. , Zumla, A. , & Ntoumi, F. (2017). Health systems in the Republic of Congo: Challenges and opportunities for implementing tuberculosis and HIV collaborative service, research, and training activities. International Journal of Infectious Diseases, 56, 62–67. 10.1016/j.ijid.2016.10.012 [DOI] [PubMed] [Google Scholar]
- Mahmood, S. E. , Srivastava, A. , Shrotriya, V. P. , & Mishra, P. (2012). Infant feeding practices in the rural population of North India. Journal of Family Community Medicine, 19(2), 130–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maketa, V. , Vuna, M. , Baloji, S. , Lubanza, S. , Hendrickx, D. , Inocêncio Da Luz, R. A. , … Lutumba, P. (2013). Perceptions of health, health care and community‐oriented health interventions in poor urban communities of Kinshasa, Democratic Republic of Congo. PLoS One, 8(12), 1–8. 10.1371/journal.pone.0084314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maleta, K. , & Amadi, B. (2014). Community‐based management of acute malnutrition (CMAM) in Sub‐Saharan Africa: Case studies from Ghana, Malawi, and Zambia. Food and Nutrition Bulletin, 35(2), S34–S38. 10.1177/15648265140352S105 [DOI] [PubMed] [Google Scholar]
- Maman, S. , Cathcart, R. , Burkhardt, G. , Omba, S. , Thompson, D. , & Behets, F. (2012). The infant feeding choices and experiences of women living with HIV in Kinshasa, Democratic Republic of Congo. AIDS Care, 24(2), 259–265. [DOI] [PubMed] [Google Scholar]
- Matovu, A. , Kirunda, B. , Rugamba‐Kabagambe, G. , Tumwesigye, N. M. , & Nuwaha, F. (2008). Factors influencing adherence to exclusive breast feeding among HIV positive mothers in Kabarole District, Uganda. East African Medical Journal, 85(4), 162–170. [DOI] [PubMed] [Google Scholar]
- MCHIP (2012). “Integrated community case management of childhood illness: Documentation of best practices and bottlenecks to program implementation in the Democratic Republic of Congo, summary report.” Washington, D.C.
- MCSP (2017a). “DRC country summary, March 2017.” 2017. https://www.mcsprogram.org/wp-content/uploads/2017/04/DRC-Country-Summary-March-2017-1.pdf.
- MCSP (2017b). “MCSP nutrition brief addressing barriers to exclusive breastfeeding: Evidence and program considerations for low‐ and middle‐income countries.” Washington, D.C.
- Ministry of Health (2007). Integrated management of childhood illness community care sites: Implementation guide. Kinshasa: Ministry of Health. [Google Scholar]
- Ministry of Planning and Monitoring Implementation of the Revolution of Modernity, ICF Macro (2014). “Demographic health survey: 2013–2014.” Rockville, MD.
- Østergaard, L. , Rosendal, L. , & Bula, A. (2010). They call our children ‘nevirapine babies?’: A qualitative study about exclusive breastfeeding among HIV positive mothers in Malawi. African Journal of Reproductive Health, 14(3), 213–222. [PubMed] [Google Scholar]
- Population Services International (2014). “PSI program brief: ICCM: Integrated community case management of pneumonia, malaria & diarrhea.” Washington, D.C.
- QSR (2015). “NVivo 11.” Cheshire. England: QSR International (UK) Limited. [Google Scholar]
- Reinhardt, K. , & Fanzo, J. (2014). Addressing chronic malnutrition through multi‐sectoral, sustainable approaches: A review of the causes and consequences. Frontiers in Nutrition, 1(August), 13 10.3389/fnut.2014.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart, C. P. , Iannotti, L. , Dewey, K. G. , Michaelsen, K. F. , & Onyango, A. W. (2013). Contextualising complementary feeding in a broader framework for stunting prevention. Maternal & Child Nutrition, 9(Suppl. 2), 27–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suresh, S. , Sharma, K. K. , Saksena, M. , Thukral, A. , Agarwal, R. , & Vatsa, M. (2014). Predictors of breastfeeding problems in the first postnatal week and its effect on exclusive breastfeeding rate at six months: Experience in a tertiary care centre in northern India. Indian Journal of Public Health, 58(4), 270–273. [DOI] [PubMed] [Google Scholar]
- Teferi, E. , Alemu, H. , Bulto, T. , Ali, I. , & Teno, D. (2014). A descriptive study of the changes in coverage of preventive and promotive interventions before and after the introduction of integrated community case management (iCCM) in Ethiopia. Ethiopian Medical Journal, 15(S3), 151–155. [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. [DOI] [PubMed] [Google Scholar]
- UNDP DRC (2009). Province orientale: Profile summary: Poverty and household conditions. Kinshasa: UNDP DRC. [Google Scholar]
- Waterloo, J. C. (1997). Protein‐energy malnutrition: The nature and extent of theproblem. Clinical Nutrition, 16, 3–9. 10.1016/S0261-5614(97)80043-X [DOI] [PubMed] [Google Scholar]
- Wazny, K. , Sadruddin, S. , Zipursky, A. , Hamer, D. H. , Jacobs, T. , Kallander, K. , & Marsh, D. R. (2014). Etting global research priorities for integrated community case management (iCCM): Results from a CHNRI (Child Health and Nutrition Research Initiative) exercise. Journal of Global Health, 4(2). 020413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellcome Trust Working Party (1970). Classification of infantile malnutrition. Lancet, 2(7667), 302–303. [PubMed] [Google Scholar]
- WHO (1999). “Management of severe malnutrition: A manual for physicians and other senior health workers.” Geneva.
- WHO/UNICEF (2012). “Joint statement: Integrated community case management (iCCM).” Geneva and New York.
- WHO/WFP/UNICEF (2007). “Community‐based management of severe acute malnutrition. A Joint Statement by the World Health Organization, the World Food Programme, the United Nations System Standing Committee on Nutrition and the United Nations Children's Fund.” Geneva.
- World Bank (2006). “Repositioning nutrition as central to development: A strategy for large‐scale action.” Washington, D.C. [Google Scholar]
- World Bank (2008). “Democratic Republic of Congo public expenditure review (PER).” Washington, D.C. http://documents.worldbank.org/curated/en/341751468026109447/pdf/421670ER0P10151osed0June025020080ZR.pdf.
- World Relief Innovation Child Survival Project Rwanda (2014). “World Relief Innovation Child Survival Project Rwanda: Third annual report.”
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1 Supporting Information
Data S2 Supporting Information


