Abstract
Objectives
Knee osteoarthritis (OA) is a prevalent disease in the elderly, causing pain and contributing to poor quality of life. Surgical intervention, such as knee arthroplasty, can be used in those with end‐stage knee OA. Total knee arthroplasty (TKA) is one of the most common surgical procedures for end‐stage knee OA, with promising clinical outcomes. However, a large proportion of patients with isolated compartment OA can be treated with unicompartmental knee arthroplasty (UKA) instead. UKA has shown better patient‐reported functional outcomes, and lower mortality and major complication rates than TKA. The percentage of UKA in knee arthroplasty varied in different orthopedic centers, and we believed that the requirement for UKA was underestimated in many centers. A retrospective study was carried out on our Chinese patient population presenting for knee arthroplasty; it aimed to identify the proportion of patients that might be suitable for UKA.
Methods
A retrospective cross‐sectional study of 155 consecutive patients (168 knees) awaiting TKA for end‐stage primary OA was performed. The pattern and grade of OA was recorded from preoperative weight‐bearing anteroposterior and non‐weight‐bearing lateral radiographs. The medial, lateral, patellofemoral compartment was given an individual Kellgren–Lawrence grade on the radiographs, and those grade ≥3 were defined as end‐stage OA. The compartments involvement was established then. The integrity of the anterior cruciate ligament (ACL) was determined by the modified Keyes classification on lateral radiographs. The applicability for total or partial knee arthroplasty was determined according to the compartments involvement.
Results
Medial compartment involvement was found in 154 (91.7%) knees, while the involvement of the lateral compartment and patellofemoral joint was found in 54 (32.1%) and 57 (33.9%) knees, respectively. Eighty‐one (48.2%) of the knees showed medial compartment OA with or without patellofemoral joint involvement, and modified Keyes classification grade 1, indicating an intact ACL, and, hence, potential suitability for medial UKA. Isolated lateral OA indicating possible suitability for lateral UKA was identified in 11 knees (6.5%). No patients showed isolated patellofemoral joint OA. The other 76 (45.2%) knees could be treated by TKA.
Conclusions
The medial compartment was the most commonly affected in our Chinese patients indicated for knee arthroplasty. More than half of the patients in this group could be treated by either medial or lateral UKA.
Keywords: Compartment involvement, Implant choice, Knee osteoarthritis, Unicompartmental knee arthroplasty
Introduction
Total knee arthroplasty (TKA) is the most successful treatment for end‐stage knee osteoarthritis (OA), offering patients’ significant symptomatic relief and functional improvement, while demonstrating a low long‐term failure rate1, 2. There has been an increase in the global burden of OA as well as the requirement for TKA. More than 620 000 TKA were carried out in the USA in 2009, with >97% of these performed for OA3, 4. It is estimated that the total volume of primary TKA procedures required will be nearly 1 million in 2015 and more than 1.3 million in 20205. In the UK, the number of TKA inserted tripled between 1991 and 20066.
In patients with unicompartmental end‐stage knee OA, partial knee replacement can be used instead of TKA. Both unicompartmental knee arthroplasty (UKA)7 and patellofemoral joint (PFJ) replacement (PFJR)8, 9 aim to replace the diseased region of the knee while preserving the intact compartments and ligaments. UKA for medial compartment OA is the most widely‐used approach for partial knee replacement. Reported advantages include a less invasive approach with less bone resection, low complication rates, easier post‐operative rehabilitation, faster recovery, greater range of motion, and good long‐term survivorship10, 11, 12. Patients who undergo UKA showed a superior functional outcome compared to TKA patients13, and were more likely to forget their artificial joint in daily life14. Good outcomes have been reported for the Oxford mobile‐bearing UKA in overweight, younger, and more active patients15, 16, as well as in the presence of co‐existent PFJ degeneration15, 17, 18, 19. In addition, isolated PFJ OA could be treated with PFJR instead of TKA8, 9.
In China, the number of joint replacements is increasing. An estimated 200 000 total hip and knee arthroplasty operations were carried out in 201220, 21, and the number increased to more than 580 000 in 2017. Although UKA has been carried out for decades in Europe and North America, it has only recently become available in China and, thus, is only carried out in a few centers, with limited short‐term outcomes reported22, 23, 24, 25, 26. It is not clear how many patients with end‐stage knee OA in China might be suitable for UKA and PFJR. A greater understanding in this area would benefit the orthopedic community and enhance patient choice. Prior to the introduction of UKA in our institution (Drum Tower Hospital, Nanjing), we treated all symptomatic end‐stage knee OA with TKA.
Despite several advantages, the usage of UKA remains relatively lower than TKA. Possible reasons might be the concern regarding the progression of OA in the other compartments, the more technical demanding nature of the procedure, and the higher revision rate for UKA than TKA. It has been shown that the progression of OA in the other compartments did not serve as the major reason for UKA revision27, 28, and the lateral progression of OA following medial UKA is mainly due to existing OA in the lateral compartment before the medial UKA27. A higher revision rate has been reported for UKA than TKA29, 30, 31; however, one of the key reasons is most surgeons do too few partial knee arthroplasties to obtain good results. It is suggested that the revision rate of UKA could be comparable to that of TKA if surgeons had at least 12 UKAs per year, and UKA was used in 20%–50% of knee arthroplasty cases32. Hence, it is critical to estimate the number and percentage of UKA in our clinical practice to evaluate the risk of failure.
We studied a consecutive series of 155 patients who presented to our outpatient clinic with symptomatic knee OA requiring TKA. Radiographs taken as part of their routine clinical work‐up were reviewed, and the severity of OA in the medial, lateral, and patellofemoral compartments was recorded. The aim of this study was to answer the following questions. First, what pattern of OA is seen in our Chinese patient population prior to knee arthroplasty? Second, what proportion of patients is suitable for partial knee replacement in the form of UKA or PFJR?
Patients and Methods
Patients
The Hospital Clinical Research Ethics Committee approved this retrospective cohort study (No. 2015‐039‐01), which included a consecutive series of 155 patients. All patients had a diagnosis of end‐stage osteoarthritis and underwent TKA between 2012 and 2013 in the first author’s center. OA in at least one compartment had to be classified as Kellgren/Lawrence (K/L) grade ≥3 for patients to be considered for arthroplasty in our institution33, 34. All patients had failed conservative treatment for at least 3 months. The patient records were reviewed, and the following exclusion criteria were applied: (i) arthritis caused by other pathogenesis, such as trauma, or rheumatoid or ankylosing spondylitis; (ii) history of surgical intervention on a lower extremity, including fracture, osteotomy, ligament reconstruction, or meniscectomy; (iii) skeletal deformity in a lower extremity that could affect the alignment in either coronal or sagittal planes (i.e. fibrous dysplasia); (iv) co‐existent pathogenesis in the spine, hip, or ankle that could significantly affect the lower extremity alignment; and (v) muscular strength less than grade IV, such as stroke, post‐poliomyelitis, or paralysis of either side.
Radiological Examination
Weight‐bearing antero‐posterior (AP) and non‐weight‐bearing lateral radiographs of the indexed knee were routinely taken before surgery. The weight‐bearing AP radiograph was taken with the knee fully extended and the tibial tuberosity and patellae facing forward. Images were taken by centering the X‐ray beam on the knee. For the lateral radiographs, the patients were positioned on their side with the knee flexed and the lateral side of knee on the film.
Radiological Assessment
On the AP and lateral radiographs, the severity of OA in medial, lateral, and PFJ compartments was graded separately using the K/L scale (grade 0, no osteophyte and joint space narrowing; grade 1, possible osteophytes only; grade 2, definite osteophytes and possible joint space narrowing; grade 3, moderate osteophytes and/or definite joint space narrowing; and grade 4, large osteophytes, severe joint space narrowing, and/or bony sclerosis)33, 34. Severe OA was defined if the K/L grade was ≥334. The presence of severe OA was used to determine the pattern of compartment involvement in each knee.
The modified Keyes classification35 was used to evaluate the integrity of the anterior cruciate ligament (ACL). On the lateral radiographs, the bone erosion was classified as grade 1 when the tibial wear was limited to the anteromedial compartment, as grade 2 once the erosion extended to the posterior margin of the plateau, and as grade 3 when there was a subluxation of the tibia on the femur. Grade 1 indicated an intact or degenerative ACL, grade 2 suggested a degenerated or torn ACL, and grade 3 demonstrated a high possibility of ACL tear.
Because high reliability in assessing the K/L grading34 and modified Keyes classification35 has been reported in previous studies, the radiographic assessment was done by the first author (W‐J. W) only. Thirty knees were randomly selected and re‐analyzed to test the intra‐observer reliability with 4‐week intervals.
Applicability of Partial Knee Arthroplasty
Medial compartment knee OA in the presence of a functioning ACL and an intact lateral compartment with or without PFJ degeneration can be treated with medial UKA (Fig. 1)15, 16, 18, 36, 37. However, patients with a knee varus of more than 15°, fixed flexion deformity over 10°, or range of motion less than 90° would be excluded. Similarly, isolated lateral compartment knee OA can be treated by lateral UKA. In addition, isolated primary PFJ OA and secondary PFJ OA are indicated for PFJR, but only if minimal OA is evident in the tibiofemoral joint (K/L grade <2)9.
Figure 1.

The knee indicated for medial unicompartmental knee arthroplasty (UKA). A 73‐year‐old woman complained of severe pain close to the medial knee joint line during walking for 2 years. The pain could not be relieved by tramadol, and so total knee arthroplasty (TKA) was carried out. (A) The antero‐posterior (AP) weight bearing X‐ray film showed K/L grade 4 in medial compartment, but only grade 1 in lateral compartment. (B) On lateral X‐ray film, the patellofemoral joint showed K/L grade 1 degeneration. Tibia plateau was classified as modified Keyes grade 1. This knee could be treated with medial UKA as an alternative to TKA.
Statistical Analysis
Intra‐observer reliability was analyzed by intraclass correlation coefficients. The modified Keyes classification was compared within different subgroups (defined by compartment involvement) using the χ2‐test. The level of significance was defined as P < 0.05.
Results
One hundred and fifty‐five patients comprising a total of 168 TKA were recruited in the present study. There were 126 women and 29 men, with a mean age of 66.4 ±7.2 years (41.8–81.5 years). The intra‐class correlations for intra‐observer reliability were 0.985 (95% confidence interval, 0.969–0.994) for the classifications of K/L Grade, and 0.965 (95% confidence interval, 0.937–0.993) for the modified Keyes classification in 30 randomly selected knees.
Compartment Involvement of Osteoarthritis
The distributions of OA with K/L grade ≥3 in different compartments are summarized in Table 1 and Fig. 2. Medial compartment involvement was found in 154 (91.7%) knees, while the involvement of lateral and PFJ OA was found in 54 (32.1%) and 57 (33.9%) knees, respectively. Isolated medial, lateral, and PFJ OA was found in 86 (51.2%), 11 (6.5%), and 2 (1.2%) knees, respectively. Isolated medial OA was the most common pattern, followed by tri‐compartment involvement (16.7%) and medial with co‐existing PFJ OA (15.5%).
Table 1.
The distributing of patterns of end‐stage knee OA (knees)
| Compartments | Modified Keyes classification | Total | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Medial | 66 | 20 | 86 | |
| Medial + PFJ | 15 | 10 | 1 | 26 |
| Lateral | 11 | 11 | ||
| Lateral + PFJ | 1 | 1 | ||
| PFJ | 1 | 1 | 2 | |
| Medial + Lateral | 5 | 8 | 1 | 14 |
| Tri‐compartments | 11 | 15 | 2 | 28 |
| Total | 109 | 55 | 4 | 168 |
OS, osteoarthritis; PFJ, patellofemoral joint; UKA, unicompartmental knee arthroplasty
Figure 2.
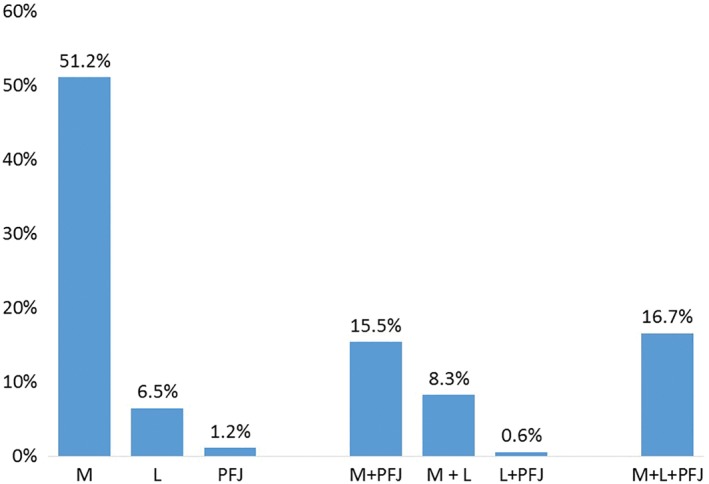
The distribution of compartment involvement in knee osteoarthritis (OA). The proportion of the involvement of isolated compartment, bi‐compartment, and tri‐compartment OA is shown. The medial compartment is more commonly affected in both isolated compartment and bi‐compartment knee OA. L, lateral; M, medial; PFJ, patellofemoral joint.
Anterior Cruciate Ligament Integrity Determined by the Modified Keyes Classification
On the lateral radiographs, 109 (64.9%) knees were considered grade 1 based on the modified Keyes classification, and 55 (32.7%) and 4 (2.4%) presented as grade 2 and 3, respectively. The incidence of grade 1 modified Keyes classification was more commonly found in knees with single compartment involvement by OA (Table 2, χ 2 = 21.1, P < 0.001).
Table 2.
Distribution of tibial cartilage erosion in end‐stage knee osteoarthritis with different numbers of compartments involved (knees)
| Modified Keyes classification | Number of compartments involved | ||
|---|---|---|---|
| Single | Double | Triple | |
| 1 | 78 | 20 | 11 |
| 2, 3 | 21 | 21 | 17 |
Comparison of the modified Keyes classifications with different numbers of compartments involved was carried out by χ2‐test (χ 2 = 21.1, P < 0.001).
Applicability of Unicompartmental Knee Arthroplasty
Grade 1 of modified Keyes classification indicates structural integrity of the ACL35. Hence, in the 109 knees, 66 with isolated medial OA as well as 15 with medial and co‐existing PFJ OA (48.2%) were eligible for Oxford medial UKA, while 11 with isolated lateral OA (6.5%) were indicated for Oxford lateral UKA. According to our criteria, both patients with isolated PFJ OA showed K/L grade 2 in medial and lateral compartments of the tibiofemoral joint, and were not indicated for PFJR9. As a result, 76 (45.2%) knees could not be treated with UKA and were indicated for treatment with TKA instead (Table 1, Fig. 3).
Figure 3.
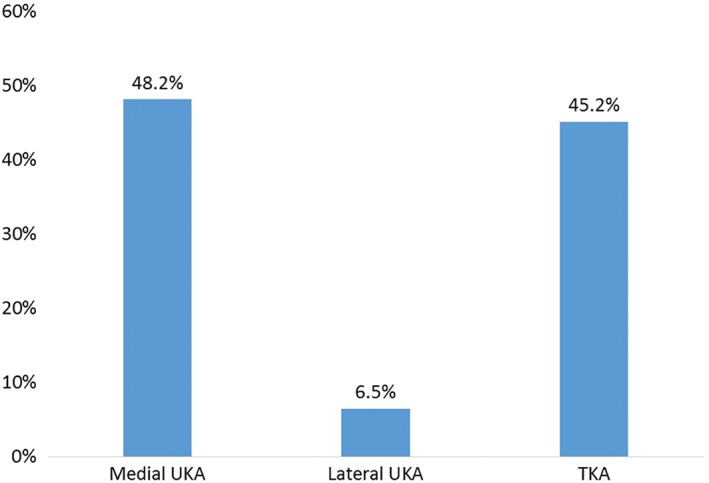
The proportion of implant selection for end‐stage knee osteoarthritis (OA). A total of 48.2% of knees indicated for medial unicompartmental knee arthroplasty (UKA) were composed of isolated medial OA (39.3%) and medial OA with co‐existing PFJ OA (8.9%), with modified Keyes classification grade 1. A total of 6.5% of knees indicated for lateral UKA were composed of isolated UKA with modified Keyes classification grade 1 only; 2 patients with K/L grade 4 PFJ OA were suggested for total knee arthroplasty (TKA) due to grade 2 OA in tibiofemoral joint, and all other knees were suggested for TKA. PFJ, patellofemoral joint; UKA, unicompartmental knee replacement.
Discussion
We have shown that over 50% of the 168 knees included in this study had isolated medial compartment OA and may be considered suitable for UKA. In total, medial compartment involvement was found in 91.7% of knees, while the lateral compartment and PFJ OA were identified in 32.1% and 33.9%, respectively. On the lateral X‐ray films, erosion of cartilage extending to the posterior tibial plateau was identified in 40.5% of knees, and the incidence increased if more compartments were affected by OA.
It is well known that the medial compartment is more frequently affected in OA of the knee; however, the prevalence in Chinese subjects is not well documented. Two studies reporting the patterns of compartment involvement in tibiofemoral OA were reviewed (Table 3)38, 39. In a population‐based study, Felson et al. identified 288 knees with OA from 1084 US subjects38, and 757 knees with OA from 1781 Chinese subjects. OA was described radiographically using K/L grade ≥2 and joint space narrowing ≥1. Isolated medial compartment OA was seen in 85.4% of US subjects and 59.7% of Chinese subjects. None of the knees showed both medial and lateral disease. In subjects participating in the Multicenter Osteoarthritis Study (MOST), Wise et al. found 305 cases of OA in 722 knees from African American subjects and 1535 cases of OA in 4480 knees from White American subjects39. Isolated medial compartment OA was seen more frequently in the White American population (63.9% and 79.3%), and the medial compartment predominance of knee OA was thought to be due to the constitutional varus leg alignment in the general population40, 41, 42, 43. In young adults, the mechanical axis of the leg is more likely to pass through the medial plateau than the lateral plateau, and the incidence of varus alignment (HKA ≤−3°) is more than 10 times that of valgus alignment (HKA ≥3°)40, 41. Varus alignment increases the risk of cartilage damage in the medial tibial plateau, while valgus alignment reduces this risk44, 45. A significant association between malalignment and progression of OA has been reported, with varus alignment promoting progression in the medial compartment while leading to the progression of OA in the lateral compartment45, 46, 47, 48. In patients with knee OA, varus alignment is caused by a more medial inclination of the tibial plateau and reduced valgus angulation of the distal femur compared to what is seen in healthy individuals49, 50. In addition, Matsumoto et al.51 found that the femur shifts from a medially bowed curvature to a laterally bowed arrangement with age. This change would reduce the condylar‐shaft angle, shift the mechanical axis medially and potentially contribute to the progression of medial OA. The high rate of medial compartment disease in our study may be due to the advanced OA seen at recruitment (K/L grade ≥3). This late stage of OA may also explain the relatively low prevalence of isolated medial OA with more compartments becoming involved as the disease progresses.
Table 3.
Summary of compartment distribution of osteoarthritis in tibiofemoral joint in different studies (knees [%])
| Gender | Compartment involved | |||
|---|---|---|---|---|
| Medial | Lateral | M + L | ||
| Felson et al.32 (K/L grade ≥2, JSN ≥1) | ||||
| Framingham, USA | Male | 93 (32.3) | 12 (4.2) | |
| Female | 153 (53.1) | 30 (10.4) | ||
| Total | 246 (85.4) | 42 (14.6) | ||
| Beijing, China | Male | 103 (13.6) | 83 (11) | |
| Female | 349 (46.1) | 222 (29.3) | ||
| Total | 452 (59.7) | 305 (40.3) | ||
| Wise et al.33 (JSN ≥1) | ||||
| African American | Male | 57 (18.7) | 20 (6.6) | 12 (3.9) |
| Female | 138 (45.2) | 46 (15.1) | 32 (10.5) | |
| Total | 195 (63.9) | 66 (21.6) | 44 (14.4) | |
| White | Male | 542 (35.3) | 59 (3.8) | 30 (2) |
| Female | 676 (44) | 183 (11.9) | 45 (2.9) | |
| Total | 1218 (79.3) | 242 (15.8) | 75 (4.9) | |
| The present study (K/L grade ≥3) | ||||
| Nanjing, China | Male | 16 (9.6) | 2 (1.2) | 14 (8.4) |
| Female | 96 (57.8) | 10 (6) | 28 (16.9) | |
| Total | 112 (67.5) | 12 (7.2) | 42 (25.3) | |
In the study of Felson et al.38, none of the knees showed osteoarthritis in both the medial and lateral compartments; two knees with isolated patellofemoral joint osteoarthritis in the present study are not included in this table
The indication for Oxford UKA has expanded. Initially, it was recommended for isolated medial or lateral compartment OA. Patients who were overweight (>82 kg), younger than 60 years, or maintained a high level of activity were thought to be contraindicated52. However, with increasing knowledge on knee kinematics and improved implant design, these conditions are no longer absolute contraindications15, 16. In addition, various studies have shown that PFJ OA does not affect functional outcome or survivorship of the Oxford UKA, suggesting that co‐existent PFJ OA should not be a contradiction for Oxford UKA15, 18, 19, 36, 37. However, a functionally intact ACL is still critical for the long‐term outcome of medial UKA, and failure of UKA would be expected in those with ACL‐deficient knees53, 54, 55. An intact ACL could maintain the stability of the knee and limit cartilage erosion of both the antero‐medial tibial plateau and femoral condyle56. One reliable method to determine the structural integrity of the ACL is to observe the bone erosion pattern of the medial plateau on the lateral radiographs57. A modified Keyes classification was established and validated by Waldstein et al.35, where grade 1 with no erosion on the tibial plateau observed on lateral X‐ray film predicted a functionally intact ACL, while grade 2 with erosion extending to the posterior margin showed more than half incidence of ACL torn. There were 109 knees classified as grade 1 in the present study. Of these knees, 66 had isolated medial OA, and 15 showed co‐existent PFJ OA, suggesting that 81 knees (48.2%) could be treated with medial UKA as an alternative to TKA. The true number of suitable candidates may be higher, because some functionally intact ACL are expected within the group of patients with a Keyes grade of 2. The applicability of UKA was also investigated in a UK population by Willis‐Owen et al.58. By analyzing the preoperative antero‐posterior weight‐bearing, lateral in 45° of flexion and “Skyline” patella views of 200 consecutive knees, the authors found that 35.1% of knees had anteromedial compartment OA with or without medial PFJ OA, and were suitable for medial UKA. In addition, 25.1% knees had medial compartment OA with or without PFJ OA, may debatable for medial UKA. The incidence of UKA found in our study and reported by Willis‐Owen et al.58 is higher than that reported by Arno et al.59, who identified 21% of 97 knees with medial OA as candidates for UKA. This discrepancy may be because Arno’s study did not include patients with patellofemoral arthritis and included patients with genu varum of less than 10° instead of 15°.
Lateral compartment knee OA can be treated by lateral UKA with predictable, good long‐term outcomes, as either fixed60, 61 or mobile bearing62. In the present study, 11 knees showed isolated lateral compartment OA with an intact ACL (Keyes grade 1). However, it is important to note that the method used to determine ACL integrity has not been validated in lateral OA. As such, it is not possible to determine if any or all of these 11 knees might have benefited from UKA without more information about the integrity of the ACL. Moreover, the effect of co‐existent PFJ OA in outcomes of lateral UKA has not been reported.
Patellofemoral OA is a common condition8, 9, confirmed by the fact that it was present in 33.9% of the knees in our study. However, isolated PFJ OA (K/L grade ≥3) is rare, and was only found in 2 knees. This isolated PJF OA could be treated by PFJR as an alternative to TKA; however, strict selection criteria are critical for its success. There should be no significant degeneration in the tibiofemoral joint and a K/L classification of no more than grade 19. Hence, neither of the 2 knees identified as isolated PFJ OA in the present study could be treated with PFJR, due to the presence of K/L grade 2 in the tibiofemoral joint.
There are limitations inherent to this retrospective study. Although all knees underwent TKA in our center, the intraoperative status of the ACL was not recorded. Because some of the patients with modified Keyes grade 2 might have had an intact ACL, the total number of patients suitable for UKA might be higher than reported. In contrast, the rate of indications for lateral UKA could be lower than what is estimated. Another limitation is that a skyline view of the knee is not routinely taken prior to TKA, and, thus, only limited views of the PFJ were available. Using a lateral radiograph to assess PFJ OA may be inadequate. However, because the severity of PFJ degeneration is not a contraindication to UKA, it may not have had a significant impact on the number of patients who fit the criteria for medial UKA.
Despite these limitations, our study has shown a high prevalence of medial compartment OA in Chinese patients undergoing TKA (91.7%). Many of these patients may be suitable for medial UKA (48.2%). A much smaller number of individuals were identified as suitable for lateral UKA (6.6%). To date, UKA is far less popular than TKA in China. This may be due to concerns regarding the learning curve associated with new surgical techniques. Zhang et al. report how well Chinese arthroplasty surgeons have adapted to handling the minimally invasive Oxford phase 3 medial UKA. They found that failure rates diminished rapidly after 16 cases, and satisfactory outcomes were achieved after approximately 25 cases63. In addition, good results can be expected when using UKA for more than 20% of overall knee arthroplasty, and the optional proportion was 40% to 60%32.
This is the first time that the pattern of OA has been determined in a group of Chinese patients with symptomatic end‐stage osteoarthritis. Many of the patients identified are suitable for partial knee arthroplasty. We encourage appropriately trained surgeons to expand the choices offered to patients by including partial knee arthroplasty as part of their treatment algorithm.
Disclosure: The authors declare that they have no conflict of interest. This work was supported by the Nanjing Medical Science and Technique Development Foundation (QRX17009), the Six Categories of Top Talents, the Jiangsu Provincial Department of Human Resources and Social Security (WSW‐002), and a Medical Research Grant supported by the Jiangsu Provincial Commission of Health and Family Planning (Q201612).
Contributor Information
Wen‐jie Weng, Email: drwilliamwang@163.com.
Andrew Price, Email: andrew.price@ndorms.ox.ac.uk.
References
- 1. Weinstein AM, Rome BN, Reichmann WM, et al Estimating the burden of total knee replacement in the United States. J Bone Joint Surg Am, 2013, 95: 385–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Paxton EW, Namba RS, Maletis GB, et al A prospective study of 80,000 total joint and 5000 anterior cruciate ligament reconstruction procedures in a community‐based registry in the United States. J Bone Joint Surg Am, 2010, 92 (Suppl. 2): 117–132. [DOI] [PubMed] [Google Scholar]
- 3. Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am, 2012, 94: 201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Maradit Kremers H, Larson DR, Crowson CS, et al Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am, 2015, 97: 1386–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am, 2014, 96: 624–630. [DOI] [PubMed] [Google Scholar]
- 6. Culliford DJ, Maskell J, Beard DJ, Murray DW, Price AJ, Arden NK. Temporal trends in hip and knee replacement in the United Kingdom: 1991 to 2006. J Bone Joint Surg Br, 2010, 92: 130–135. [DOI] [PubMed] [Google Scholar]
- 7. Murray DW. Mobile bearing unicompartmental knee replacement. Orthopedics, 2005, 28: 985–987. [DOI] [PubMed] [Google Scholar]
- 8. Walker T, Perkinson B, Mihalko WM. Patellofemoral arthroplasty: the other unicompartmental knee replacement. J Bone Joint Surg Am, 2012, 94: 1712–1720. [DOI] [PubMed] [Google Scholar]
- 9. Borus T, Brilhault J, Confalonieri N, Johnson D, Thienpont E. Patellofemoral joint replacement, an evolving concept. Knee, 2014, 21 (Suppl. 1): S47–S50. [DOI] [PubMed] [Google Scholar]
- 10. Panzram B, Bertlich I, Reiner T, Walker T, Hagmann S, Gotterbarm T. Cementless Oxford medial unicompartimental knee replacement: an independent series with a 5‐year‐follow‐up. Arch Orthop Trauma Surg, 2017, 137: 1011–1017. [DOI] [PubMed] [Google Scholar]
- 11. Price AJ, Rees JL, Beard DJ, Gill RH, Dodd CA, Murray DM. Sagittal plane kinematics of a mobile‐bearing unicompartmental knee arthroplasty at 10 years: a comparative in vivo fluoroscopic analysis. J Arthroplasty, 2004, 19: 590–597. [DOI] [PubMed] [Google Scholar]
- 12. Pandit H, Hamilton TW, Jenkins C, Mellon SJ, Dodd CA, Murray DW. The clinical outcome of minimally invasive phase 3 Oxford unicompartmental knee arthroplasty: a 15‐year follow‐up of 1000 UKAs. Bone Joint J, 2015, 97: 1493–1500. [DOI] [PubMed] [Google Scholar]
- 13. Kim MS, Koh IJ, Choi YJ, Lee JY, In Y. Differences in patient‐reported outcomes between unicompartmental and total knee arthroplasties: a propensity score‐matched analysis. J Arthroplasty, 2017, 32: 1453–1459. [DOI] [PubMed] [Google Scholar]
- 14. Zuiderbaan HA, van der List JP, Khamaisy S, et al Unicompartmental knee arthroplasty versus total knee arthroplasty: which type of artificial joint do patients forget? Knee Surg Sports Traumatol Arthrosc, 2017, 25: 681–686. [DOI] [PubMed] [Google Scholar]
- 15. Pandit H, Jenkins C, Gill HS, et al Unnecessary contraindications for mobile‐bearing unicompartmental knee replacement. J Bone Joint Surg Br, 2011, 93: 622–628. [DOI] [PubMed] [Google Scholar]
- 16. Murray DW, Pandit H, Weston‐Simons JS, et al Does body mass index affect the outcome of unicompartmental knee replacement? Knee, 2013, 20: 461–465. [DOI] [PubMed] [Google Scholar]
- 17. Beard DJ, Pandit H, Ostlere S, Jenkins C, Dodd CA, Murray DW. Pre‐operative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. J Bone Joint Surg Br, 2007, 89: 1602–1607. [DOI] [PubMed] [Google Scholar]
- 18. Kang SN, Smith TO, Sprenger De Rover WB, Walton NP. Pre‐operative patellofemoral degenerative changes do not affect the outcome after medial Oxford unicompartmental knee replacement: a report from an independent centre. J Bone Joint Surg Br, 2011, 93: 476–478. [DOI] [PubMed] [Google Scholar]
- 19. Hamilton TW, Pandit HG, Maurer DG, et al Anterior knee pain and evidence of osteoarthritis of the patellofemoral joint should not be considered contraindications to mobile‐bearing unicompartmental knee arthroplasty: a 15‐year follow‐up. Bone Joint J, 2017, 99‐B: 632–639. [DOI] [PubMed] [Google Scholar]
- 20. Pei F. The current status and future perspective of hip and knee arthroplasty in China. Chin J Bone Joint, 2012, 1: 4–8. [Google Scholar]
- 21. Huang SL, He XJ, Wang KZ. Joint replacement in China: progress and challenges. Rheumatology (Oxford), 2012, 51: 1525–1526. [DOI] [PubMed] [Google Scholar]
- 22. Sun PF, Jia YH. Mobile bearing UKA compared to fixed bearing TKA: a randomized prospective study. Knee, 2012, 19: 103–106. [DOI] [PubMed] [Google Scholar]
- 23. Zhang Z, Zhu W, Zhu L, Du Y. Superior alignment but no difference in clinical outcome after minimally invasive computer‐assisted unicompartmental knee arthroplasty (MICA‐UKA). Knee Surg Sports Traumatol Arthrosc, 2016, 24: 3419–3424. [DOI] [PubMed] [Google Scholar]
- 24. Tian S, Wang B, Wang Y, Ha C, Liu L, Sun K. Combined unicompartmental knee arthroplasty and anterior cruciate ligament reconstruction in knees with osteoarthritis and deficient anterior cruciate ligament. BMC Musculoskelet Disord, 2016, 17: 327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tu Y, Xue H, Ma T, et al Superior femoral component alignment can be achieved with Oxford microplasty instrumentation after minimally invasive unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc, 2017, 25: 729–735. [DOI] [PubMed] [Google Scholar]
- 26. Xu T, Lao Y, Wang J, Liu F, Xiao L, Tong P. Mid‐term results of Oxford phase‐3 medial unicompartmental knee arthroplasty for medial arthritis in Chinese patients. ANZ J Surg, 2017, 87: 287–290. [DOI] [PubMed] [Google Scholar]
- 27. Pandit H, Spiegelberg B, Clave A, McGrath C, Liddle AD, Murray DW. Aetiology of lateral progression of arthritis following Oxford medial unicompartmental knee replacement: a case‐control study. Musculoskelet Surg, 2016, 100: 97–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Leta TH, Lygre SH, Skredderstuen A, et al Outcomes of unicompartmental knee arthroplasty after aseptic revision to total knee arthroplasty: a comparative study of 768 TKAs and 578 UKAs revised to TKAs from the Norwegian arthroplasty register (1994 to 2011). J Bone Joint Surg Am, 2016, 98: 431–440. [DOI] [PubMed] [Google Scholar]
- 29. Liddle AD, Judge A, Pandit H, Murray DW. Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet, 2014, 384: 1437–1445. [DOI] [PubMed] [Google Scholar]
- 30. Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD. Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc, 2018, 26: 1811–1822. [DOI] [PubMed] [Google Scholar]
- 31. Goh GS, Bin Abd Razak HR, Tay DK, Chia SL, Lo NN, Yeo SJ. Unicompartmental knee arthroplasty achieves greater flexion with no difference in functional outcome, quality of life, and satisfaction vs total knee arthroplasty in patients younger than 55 years. A propensity score‐matched cohort analysis. J Arthroplasty, 2018, 33: 355–361. [DOI] [PubMed] [Google Scholar]
- 32. Liddle AD, Pandit H, Judge A, Murray DW. Optimal usage of unicompartmental knee arthroplasty: a study of 41,986 cases from the National Joint Registry for England and Wales. Bone Joint J, 2015, 97: 1506–1511. [DOI] [PubMed] [Google Scholar]
- 33. Kellgren JH, Lawrence JS. Radiological assessment of osteo‐arthrosis. Ann Rheum Dis, 1957, 16: 494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhang Y, Xu L, Nevitt MC, et al Comparison of the prevalence of knee osteoarthritis between the elderly Chinese population in Beijing and whites in the United States: the Beijing Osteoarthritis Study. Arthritis Rheum, 2001, 44: 2065–2071. [DOI] [PubMed] [Google Scholar]
- 35. Waldstein W, Merle C, Monsef JB, Boettner F. Varus knee osteoarthritis: how can we identify ACL insufficiency? Knee Surg Sports Traumatol Arthrosc, 2015, 23: 2178–2184. [DOI] [PubMed] [Google Scholar]
- 36. Kuipers BM, Kollen BJ, Bots PC, et al Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee, 2010, 17: 48–52. [DOI] [PubMed] [Google Scholar]
- 37. Beard DJ, Pandit H, Gill HS, Hollinghurst D, Dodd CA, Murray DW. The influence of the presence and severity of pre‐existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. J Bone Joint Surg Br, 2007, 89: 1597–1601. [DOI] [PubMed] [Google Scholar]
- 38. Felson DT, Nevitt MC, Zhang Y, et al High prevalence of lateral knee osteoarthritis in Beijing Chinese compared with Framingham Caucasian subjects. Arthritis Rheum, 2002, 46: 1217–1222. [DOI] [PubMed] [Google Scholar]
- 39. Wise BL, Niu J, Yang M, et al Patterns of compartment involvement in tibiofemoral osteoarthritis in men and women and in whites and African Americans. Arthritis Care Res (Hoboken), 2012, 64: 847–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res, 2012, 470: 45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shetty GM, Mullaji A, Bhayde S, Nha KW, Oh HK. Factors contributing to inherent varus alignment of lower limb in normal Asian adults: role of tibial plateau inclination. Knee, 2014, 21: 544–548. [DOI] [PubMed] [Google Scholar]
- 42. Tang WM, Zhu YH, Chiu KY. Axial alignment of the lower extremity in Chinese adults. J Bone Joint Surg Am, 2000, 82: 1603–1608. [DOI] [PubMed] [Google Scholar]
- 43. Minoda Y, Kobayashi A, Iwaki H, et al Sagittal alignment of the lower extremity while standing in Japanese male. Arch Orthop Trauma Surg, 2008, 128: 435–442. [DOI] [PubMed] [Google Scholar]
- 44. Sharma L, Chmiel JS, Almagor O, et al The role of varus and valgus alignment in the initial development of knee cartilage damage by MRI: the MOST study. Ann Rheum Dis, 2013, 72: 235–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Janakiramanan N, Teichtahl AJ, Wluka AE, et al Static knee alignment is associated with the risk of unicompartmental knee cartilage defects. J Orthop Res, 2008, 26: 225–230. [DOI] [PubMed] [Google Scholar]
- 46. Cerejo R, Dunlop DD, Cahue S, Channin D, Song J, Sharma L. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum, 2002, 46: 2632–2636. [DOI] [PubMed] [Google Scholar]
- 47. Khan FA, Koff MF, Noiseux NO, et al Effect of local alignment on compartmental patterns of knee osteoarthritis. J Bone Joint Surg Am, 2008, 90: 1961–1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cicuttini F, Wluka A, Hankin J, Wang Y. Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology (Oxford), 2004, 43: 321–324. [DOI] [PubMed] [Google Scholar]
- 49. Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P. Axial lower‐limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage, 1997, 5: 39–47. [DOI] [PubMed] [Google Scholar]
- 50. Cooke TD, Harrison L, Khan B, Scudamore A, Chaudhary MA. Analysis of limb alignment in the pathogenesis of osteoarthritis: a comparison of Saudi Arabian and Canadian cases. Rheumatol Int, 2002, 22: 160–164. [DOI] [PubMed] [Google Scholar]
- 51. Matsumoto T, Hashimura M, Takayama K, et al A radiographic analysis of alignment of the lower extremities – initiation and progression of varus‐type knee osteoarthritis. Osteoarthritis Cartilage, 2015, 23: 217–223. [DOI] [PubMed] [Google Scholar]
- 52. Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am, 1989, 71: 145–150. [PubMed] [Google Scholar]
- 53. Goodfellow JW, Kershaw CJ, Benson MK, O’Connor JJ. The Oxford knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg Br, 1988, 70: 692–701. [DOI] [PubMed] [Google Scholar]
- 54. Deschamps G, Lapeyre B. Rupture of the anterior cruciate ligament: a frequently unrecognized cause of failure of unicompartmental knee prostheses. Apropos of a series of 79 Lotus prostheses with a follow‐up of more than 5 years. Rev Chir Orthop Reparatrice Appar Mot, 1987, 73: 544–551. [PubMed] [Google Scholar]
- 55. Mancuso F, Dodd CA, Murray DW, Pandit H. Medial unicompartmental knee arthroplasty in the ACL‐deficient knee. J Orthop Traumatol, 2016, 17: 267–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Rout R, McDonnell S, Hulley P, et al The pattern of cartilage damage in antero‐medial osteoarthritis of the knee and its relationship to the anterior cruciate ligament. J Orthop Res, 2013, 31: 908–913. [DOI] [PubMed] [Google Scholar]
- 57. Keyes GW, Carr AJ, Miller RK, Goodfellow JW. The radiographic classification of medial gonarthrosis. Correlation with operation methods in 200 knees. Acta Orthop Scand, 1992, 63: 497–501. [DOI] [PubMed] [Google Scholar]
- 58. Willis‐Owen CA, Brust K, Alsop H, Miraldo M, Cobb JP. Unicondylar knee arthroplasty in the UK National Health Service: an analysis of candidacy, outcome and cost efficacy. Knee, 2009, 16: 473–478. [DOI] [PubMed] [Google Scholar]
- 59. Arno S, Maffei D, Walker PS, Schwarzkopf R, Desai P, Steiner GC. Retrospective analysis of total knee arthroplasty cases for visual, histological, and clinical eligibility of unicompartmental knee arthroplasties. J Arthroplasty, 2011, 26: 1396–1403. [DOI] [PubMed] [Google Scholar]
- 60. Pennington DW, Swienckowski JJ, Lutes WB, Drake GN. Lateral unicompartmental knee arthroplasty: survivorship and technical considerations at an average follow‐up of 12.4 years. J Arthroplasty, 2006, 21: 13–17. [DOI] [PubMed] [Google Scholar]
- 61. Lustig S, Lording T, Frank F, Debette C, Servien E, Neyret P. Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow‐up of 54 consecutive implants. Knee, 2014, 21 (Suppl. 1): S26–S32. [DOI] [PubMed] [Google Scholar]
- 62. Weston‐Simons JS, Pandit H, Kendrick BJ, et al The mid‐term outcomes of the Oxford Domed Lateral unicompartmental knee replacement. Bone Joint J, 2014, 96: 59–64. [DOI] [PubMed] [Google Scholar]
- 63. Zhang Q, Zhang Q, Guo W, et al The learning curve for minimally invasive Oxford phase 3 unicompartmental knee arthroplasty: cumulative summation test for learning curve (LC‐CUSUM). J Orthop Surg Res, 2014, 9: 81. [DOI] [PMC free article] [PubMed] [Google Scholar]


