Abstract
Objective
To evaluate the clinical outcomes of traumatic spino‐pelvic dissociation (TSD) treated with modified bilateral triangular fixation.
Methods
Eighteen consecutive patients of TSD were included in the study from March 2011 to March 2015, and the medical records of patients were reviewed retrospectively. There were 14 men and 4 women with an average age of 33.1 ± 1.4 years (range, 18–55 years). A total of 16 cases were caused by falling, and 2 cases were caused by traffic accident. All sacral fractures had associated injuries. According to the morphology of sacral fracture, U‐shaped fractures were present in 10 cases, H‐shaped fractures in 6 cases, and Y‐shaped fractures in 2 cases. According to Roy–Camille classification, there were 12 cases of type II and 6 cases of type III. All patients received surgical treatment with modified bilateral triangular fixation, and the sacral plexus decompression was performed simultaneously on 6 cases whose scores were more than 2 according to Gibbons classification and were found having traumatic canal stenosis or sacral nerve compression detected by preoperative imaging examination. Mears’ radiological evaluation criterion was applied to evaluate the reduction quality of fractures; Gibbons score was applied as the index of neurological deficiency healing, and the clinical outcome of fracture was evaluated with Majeed function assessment at last follow‐up.
Results
All patients were followed up continuously within an average of 32.4 ± 3.6 months (range, 22–48 months). All sacral fractures were healed in an average time of 11.3 ± 2.8 months (range, 8–28 months). According to the Majeed function evaluation, 12 cases were classified as excellent, 4 cases as good, and 2 cases as fair. Meanwhile, the anatomical reduction was obtained in 11 cases, satisfactory reduction in 6 cases, and unsatisfactory reduction in 1 case according to Mears’ radiological evaluation criterion. The average Gibbons score changed from 2.5 ± 0.2 preoperatively to 1.4 ± 0.5 24 months postoperatively, which had a significant difference (t = 2.15, P < 0.05).
Conclusion
Modified triangular fixation combined with internal fixations shows satisfactory clinical outcomes in the treatment of TSD, which is recommended as an effective and advanced surgical choice.
Keywords: Modified, Outcome, Spino‐pelvic Dissociation, Triangular Fixation
Introduction
Traumatic spino‐pelvic dissociation (TSD) refers to a series of complicated sacral fractures, which consists of a transverse fracture line perpendicular to the sacral canal associated with bilateral longitudinal fracture lines, resulting in complete dissociation of the upper sacrum and spine of the pelvis1. The occurrence rate of TSD is 3%–6%2, 3. Of all pelvic fractures, and the main mechanism of injury is falling. Resulting from high‐energy injuries, TSD always involves severe complications, such as cauda equina syndrome, organ injuries, or other fractures, and is challenging to treat.
Over the past 10 years, more and more surgeons have advocated for internal fixation in treating TSD; this technique can be used to reconstruct the normal weight‐bearing load axis so as to enable patients to ambulate early, to cure the injury of nerves caused by progressive fracture deformity, and to prevent the lumbo‐sacral pain resulting from instability of the lumbosacral junction1, 2, 3, 4, 5, 6, 7, 8, 9. Yi and Hak reviewed the literature and found that the prognosis of TSD was closely related to the good quality of fracture reduction, which can only be obtained by operation1. Therefore, they concluded that surgical management is the preference for TSD treatment. Other reports were of the same opinion2, 7, 8.
The current internal fixation for treating TSD includes iliosacral screws, transsacral plate, and lumbopelvic or triangular fixation. Lumbopelvic fixation and iliosacral screws are popular fixations in the treatment of TSD; however, both have limitations and deficiencies1, 2, 4. Lumbopelvic fixation fixes the sacral fracture indirectly, which makes the fracture union difficult; iliosacral screws only have the function of fixing and cannot reduce the fracture simultaneously and the quality of regular closed or open reduction is unsatisfactory for TSD. More and more surgeons are recommending triangular fixation in the treatment of TSD because of the more reasonable biomechanical model, improved fixed strength, and greater neurological deficiency improvement10, 11. This technique not only can provide reduction and fixation of the sacral fracture simultaneously, but also can formulate a tri‐dimensional interlocking structure to fix the fracture both directly and indirectly to obtain maximum stability of the sacral fracture.
However, the classic triangular fixation has some disadvantages, such as the related high occurrence of chronic lower lumbar pain because of the unbalanced loads of lumbosacral conjunctions, and the discomfort of the internal fixation prominence. To address these limitations, we made some modifications: the same lengths of rod from L5 pedicle screws to the ends of iliac screws bilaterally were applied to ensure equal forces of distraction were loaded at both sides; the bone around iliac screw ends was removed partly to deepen the implants to avoid the complications caused by the prominence of the fixation.
The purpose of this study was to evaluate the clinical outcomes of treatment on TSD with modified triangular fixation, to discuss the advantage of this technique, and to describe the key points of the operation.
Methods
Inclusion and Exclusion Criteria
Inclusion criteria: (i) TSD treated with modified bilateral triangular fixation; (ii) accurate evaluation of the prognosis of the patient, the reduction quality of the fracture, and neural healing; and (iii) continuous follow‐up more than 18 months, with the data being integral.
Exclusion criteria: (i) open sacral fracture and (ii) associated severe internal medical disease.
Patients’ Data
Eighteen consecutive cases of TSD were included in the study from March 2011 to March 2015 and the medical records of patients were reviewed retrospectively. There were 14 men and 4 women, with an average age of 33.1 ± 1.4 years (range, 18–55 years). Of these, 16 cases were caused by falling, and 2 cases were caused by traffic accidents. All sacral fractures were closed and had associated injuries, including 3 head injuries, 3 thorax injuries, 1 abdomen injury, 1 urinary system injury, 3 spine fractures, 15 other fractures, 2 Morel‐Lavallée lesions, and 14 nerve injuries, among which 6 cases had severe sacral plexus injuries and the Gibbons score was more than 2. According to the morphology of sacral fractures, U‐shaped factures were found in 10 cases, H‐shaped fractures in 6 cases, and Y‐shaped fracture in 2 cases. According to Roy–Camille classification, there were 12 cases of type II and 6 cases of type III (Supplementary Appendix S1).
Preoperative Treatment and Plan
In the acute phase, the advanced trauma life support (ATLS) protocol took precedence over definitive surgery for sacral fracture. Resuscitation and urgent surgical procedures were applied in emergency if the associated injuries threatened lives, and the fractures were managed based on damage control orthopaedics (DCO) principles. Then patients were transferred to the intensive care unit to accept further treatment. The definitive operations were performed until the physiological condition of patients was stable. The standard preoperative plan included physical examination of neurological deficiency, imaging examination to assess the lateral displacement, inclination angular and rotational deformity degree of sacral fracture, CT and MR to evaluate the area and degree of the sacral canal and foramen compression on the patients who had neural injured symptoms. 3‐D radiological simulation on normal morphology of every injured sacrum was necessary, so that we could measure the anatomic data of the sacral vestibular and judge whether the iliosacral screws were suitable to implant preoperatively. Preoperative skeletal tractions were performed on all patients to correct the deformity as far as possible and we observed the change in nerve injuries to prejudge whether decompression of sacral plexus was necessary.
Operative Techniques
The patient was placed in a prone position on the operation bed, which C‐arm fluoroscopy intraoperatively of anterior‐posterior, inlet, outlet and lateral view should be assured after general anesthesia. The median incision was from the L3 spinous process to S3; the bilateral erector spinae were dissociated, and the laminae, transverse processes, articular processes of L4,5, and laminae of sacrum were exposed. The nerve decompression should be performed before the reduction of fracture. In our study, 6 cases whose scores were more than 2 according to Gibbons classification and were found to have traumatic canal stenosis or sacral nerve compression caused by fragments of fracture detected by the preoperative imaging examination accepted the sacral laminectomy and neurolysis. The compressed fragments were removed and the sacral nerves were traced and loosened completely.
The pedicle screws were inserted through the bilateral pedicles of L5 or L4 and L5 before the neural decompression. The amount of screws depended on the degree of fracture displacement and the complexity of reduction, which was prejudged preoperatively. Then the deep fascia was dissociated and incised to expose bilateral posterior superior iliac spines (PSIS). One or two lengthened iliac screws were inserted 10‐cm deep in the direction from PSIS to the anterior inferior iliac spine and between the medial and lateral lamina of each side of the iliac wing. The bone around iliac screw ends was removed (approximately 2–3 cm) to avoid the prominence of internal fixation. The lateral modal connectors and the precontoured rods were placed and connected to the pedicle screws and iliac screws.
The reduction of vertical displacement was obtained through the distraction of the lumbopelvic device, then all connectors were screwed in and the transverse connect instruments were fixed. The rotational deformity and horizontal displacement were corrected with reduction clamps or an extra Schantz screw, which was inserted temporarily in the upper sacrum to manipulate the upper sacrum as a joystick. The intraoperative fluoroscopy of AP, inlet, outlet, and lateral views were important to evaluate the quality of the reduction. Then two 6.5‐mm full threaded cannulated screws were inserted from the lateral cortex of the iliac border to the S1 vertebral body bilaterally when the direct fixation of the sacral fracture was obtained. During this procedure, consecutive fluoroscopy of lateral, AP, inlet, and outlet views must be monitored to ensure the correct insertion of screws. The lumbosacral spondylosis was performed in 4 patients who had injuries of lumbosacral conjunction to prevent joint instability postoperatively (Fig. 1).
Figure 1.
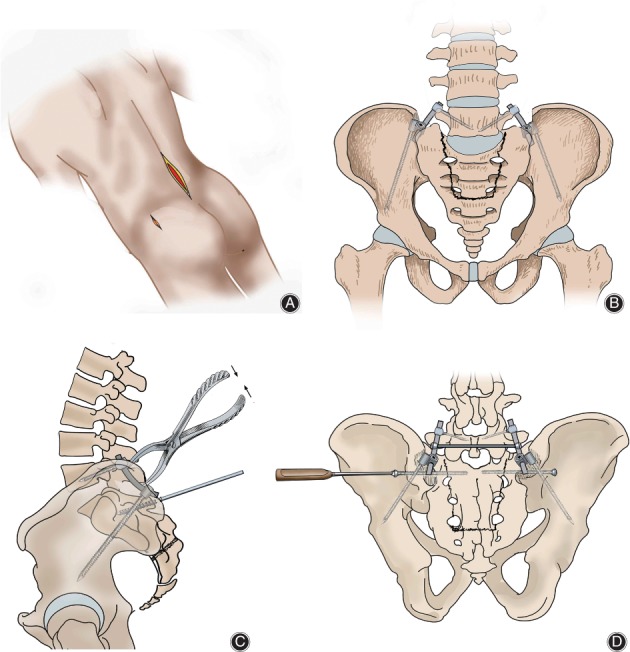
Diagram illustrating surgical process of bilateral triangular fixation. (A) The patient was placed in a prone position. (B) Pedicle screws were inserted through the bilateral pedicles of L5. A lengthened iliac screw was inserted 10‐cm deep in the direction from posterior superior iliac spines to the anterior inferior iliac spines and between the medial and lateral lamina of each side of the iliac wing. The lateral modal connectors and the precontoured rods were placed and connected the pedicle and iliac screws. (C) The reduction of vertical displacement was obtained through the distraction of the lumbopelvic device. The rotational deformity and horizontal displacement were corrected with an extra Schantz screw, which was inserted temporarily into the upper sacrum to manipulate the upper sacrum as a joystick. (D) All the connectors were screwed in and the transverse connect instruments were fixed. Then, two 6.5‐mm cannulated screws were inserted from the lateral cortex of the iliac border to the S1 vertebral body bilaterally for direct fixation of the sacral fracture.
Irrigation and vacuum drainage instruments were used and the wound was closed. The operations for anterior pelvic ring injuries were performed simultaneously or delayed based on comprehensive evaluation, taking into consideration, for instance, the amount of intraoperative bleeding and the physiological condition of patients.
Postoperative Treatment
The antibiotic was transfused 48‐h postoperatively on top of the regular application preoperatively and intraoperatively. The drainage instrument was removed 48–72‐h postoperatively according to the amount of drainage fluid. Low‐molecular heparin was applied regularly as thromboprophylaxis during the immobilization period. Rehabilitation was planned and performed by a physical therapist as soon as the physical and wound condition allowed. Full weight‐bearing was permitted 8–16 weeks postoperatively depending on the type of fracture and associated injuries.
Follow‐up and Clinical Outcome Evaluation
The schedule of follow‐up was 4 weeks, 8 weeks, and every 3 months postoperatively. Physical examinations and imaging exams were undertaken to evaluate the degree of fracture healing, neurological impairment and improvement in ability to function in daily life. The clinical outcome for fractures was evaluated with Majeed function assessment, Mears’ radiological evaluation criterion was applied to evaluate the reduction quality of fractures, and Gibbons score was applied as the index of neurological deficiency (Table 1).
Table 1.
The Gibbons classification of cauda equina impairment
| Type | Neurological deficit |
|---|---|
| 1 | None |
| 2 | Paresthesia only |
| 3 | Lower extremity motor deficit |
| 4 | Bowel/bladder dysfunction |
Statistical Analysis
The preoperative and postoperative Gibbons scores were analyzed using a t‐test (P < 0.05). The software used for statistical analysis was SPSS18.0 (SPSS, Chicago, IL, USA). Scaled data were reported as arithmetic mean ± standard deviation.
Results
Clinical Results
All operations were undertaken by the same group of surgeons between 5 and 35 days (average, 2.0 ± 3.4 days) after the primary injury. The average time of procedures for TSD was 172.0 ± 15.5 minutes (range, 130–450 minutes) and the average amount of intraoperative bleeding was 750 ± 25 mL (range, 400–3200 mL). All patients were followed up consecutively; the average follow‐up period was 32.4 ± 3.6 months (range, 22–48 months). All sacral fractures healed in an average time of 11.3 ± 2.8 months (range, 8–28 months). None of the cases had re‐displacement of fractures or fixation failure (Fig. 2).
Figure 2.
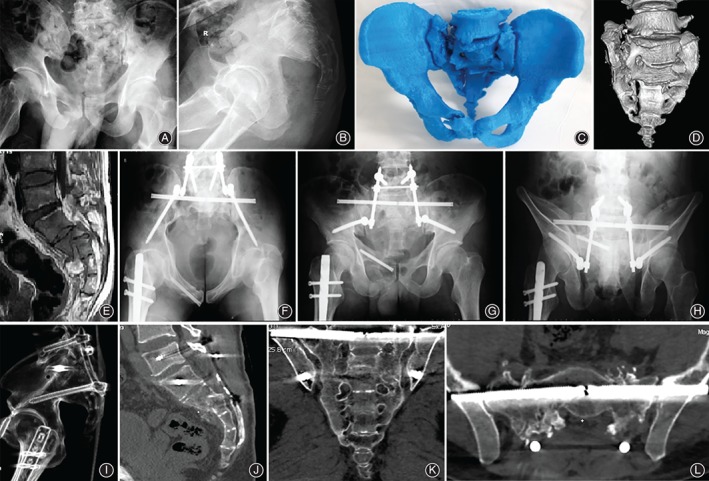
(A, B) Male, 36 years, injured by falling. The primary injury was a pelvic fracture associated with cauda equine syndrome. (C, D) The CT and 3‐D printed model showed the H‐shaped fracture of the sacrum. The displacement and angulation of the fracture is obvious. (E) MR showed the intracanal bone fragment of the sacral fracture and the compression of dura mater, which caused the cauda equine syndrome of the patient. (F–I) The operation was performed 18 days after injury and the spino‐pelvic dissociation was treated with bilateral modified triangular fixation. The radiological examination showed that the fracture was reduced and fixed satisfactorily. (J–L) CT 8 months postoperatively showed that the sacral fracture had healed well, and the neural injury was lessened to Gibbon 2 from 4.
Evaluation Results
According to the Majeed evaluation system, 12 cases were evaluated as excellent, 4 cases as good, and 2 cases as fair at last follow‐up. Meanwhile, anatomical reduction was obtained in 11 cases, satisfactory reduction in 6 cases, and unsatisfactory reduction in 1 case according to Mears’ radiological evaluation criterion.
Neurological Improvement
There were significant improvements in neurologic impairment in all postoperative patients; even 8 patients who did not undergo the nerve decompression had reduced paresthesia. In our study, only 1 patient still had partial dysfunction of the bladder, 2 did not have completely restored unilateral plantar flexion of the ankle, and 2 patients who had paresthesia of lower extremities preoperatively had no recovery postoperatively. At the follow‐up 24 months postoperatively, the average Gibbons score changed from 2.5 ± 0.2 preoperatively to 1.4 ± 0.5 postoperatively, which had a significant difference (t = 2.15, P < 0.05).
Complications
There were 5 cases that had complications. Wound dehiscence because of fat liquefaction occurred in 2 cases, and healed after debridement. One patient had severe diarrhea postoperatively and a deep infection caused by enterococcus faecalis occurred 1 week postoperatively because of fecal contamination of the wound. After the debridement and irrigation and administration of antibiotics, the patient had healed 8 weeks postoperatively. Two patients had posterior prominence of the internal fixation and complicated pain. The symptom disappeared after removing the fixation 1 year postoperatively, once the fracture had healed.
Discussion
Characteristics of Traumatic Spino‐pelvic Dissociation
Traumatic spino‐pelvic dissociation has special pathological and imaging characteristics: The correct diagnosis is often missed or delayed because of the difficulty in imaging the upper sacrum on anterior–posterior pelvic radiograph with the inclination of the sacrum and the overlying bowel gas. The physiological examination and some specific imaging signs, such as the paradoxical inlet view and the stepladder sign, are important for the index of suspicion, and multi‐planar CT is necessary for diagnosis1, 4, 10, 12. The injury energy loads through the spine–sacrum axis, and further shears the sacrum or lumbosacral region in a state of excessive flexion or extension, resulting in fractures of the weak parts of sacrum. The fractures are completely unstable; thus, 3 dimensional displacement and deformities are frequent. TSD always has associated injuries and the Injury Severity Scores (ISS) are high1, 4, 10, 13. Damage Control Orthopaedics (DCO) protocol should be undertaken through the whole treatment period if the injury is severe (ISS >17). Soft tissue injuries of the pelvis and peripheral region must receive particular attention. If Morel–Lavallée lesions exist, they must be cured before definitive surgery to avoid severe infections and skin necrosis14, 15.
Internal Fixation
The purposes of surgery on TSD include pelvic ring reconstruction, lumbopelvic stability restoration, fracture displacement prevention, and correction to improve the neurological deficiency. More and more surgeons are advocating for surgical management in the treatment of TSD, and open reduction internal fixation (ORIF) has demonstrated marked benefits over conservative treatment1, 2, 3, 4, 5, 6, 7, 8, 9, 16, 17.
Lumbopelvic fixation and iliosacral screws are popular fixations in the treatment of TSD. However, both have limitations and deficiencies1, 2, 4, 18: lumbopelvic fixation cannot fix the sacral fracture directly, which leads to the relatively high rate of non‐union because of the excessive motion of the sacrum and malunion caused by re‐displacement of the fracture; iliosacral screws cannot ensure the reduction and fixation simultaneously and the quality of regular reduction intraoperatively is worse than for lumbopelvic fixation, especially for vertical displacement, which is the most important factor affecting the prognosis. Triangular fixation is an advanced technique that combines lumbopelvic fixation with iliosacral screws. This technique was first introduced by Käch and Trentz for spino‐pelvic fixation in 1994 to treat a unilateral vertical shear lesion of the pelvis19. Schildhauer et al. developed the concept and reported positive clinical and biomechanical results10, 20. Hu et al. (2013) performed this technique bilaterally to treat TSD and had a good clinical outcome21.
Advantages of Triangular Fixation
We summarize the advantages of triangular fixation in the treatment of TSD as follows:
This technique can provide indirect reduction and fixation of sacral fractures simultaneously, to facilitate the reduction procedure and avoid excessive exposure, additional bleeding, and extra operation time that are caused by direct reduction. Compared with other methods, triangular fixation can obtain better quality of reduction, resulting in fracture healing and a satisfactory prognosis1, 22. In our study, anatomical reduction was obtained in 11 cases, and satisfactory reduction in 6 cases according to Mears’ radiological evaluation criterion. Only 1 case obtained unsatisfactory reduction. This patient underwent surgery 35 days after injury as soon as the patient’s physical condition allowed, which caused the sacral fracture was old and hard to reduce.
The triangular fixation combines indirect lumbopelvic fixation and direct screw fixation of sacral fracture, and can formulate a tri‐dimensional interlocking structure to obtain the maximum stability of fracture21, 23, 24. Furthermore, it can restore the normal load of the weight‐bearing axis. Because of these advantages, triangular fixation can avoid the shear and rotational force on the injured area of the sacrum, not only preventing progressive nerve injury and re‐displacement of fracture but also creating a stable base to improve the rate of fracture union and allow ambulation early. In our study, all sacral fractures healed and the Majeed score was better than in other studies; these outcomes prove our hypothesis2, 7, 9.
Modified Triangular Fixation
In our opinion, there are some limitations and deficiencies of traditional triangular fixation. Therefore, we made some modification to this technique and obtained better outcomes.
The occurrence of chronic lower lumbar pain was common after the triangular fixation insertion. The main reason for this complication was that forces distracting the fractures bilaterally were not equal and caused unbalanced loads of lumbosacral conjunctions18. In our study, the triangular fixations were inserted bilaterally and the same lengths of rod from L5 pedicle screws to the ends of iliac screws bilaterally were used to ensure equal forces of distraction were loaded both sides, and the same pressure was applied on the lumbar disc. In our study, the outcome that none of the patients complained of lower lumbar pain proved the success of our modification.
We used long iliac screws (100 mm), which were designed to penetrate inside the whole iliac wing, instead of the pedicle screws, which were placed inside both iliac wings using the original technique, and the length of screw insertion was much deeper, to obtain higher biomechanical stability.
We removed some area of bone around the iliac screw ends to implant lateral modal connectors more deeply to avoid associated complications resulting from prominence of the fixation, such as chronic pain and wound dehiscence, and the result was satisfactory.
Sacral Nerve Decompression
The morphology of sacral fractures in TSD easily results in neurological deficiency, ranging from incomplete monoradiculopathies to complete cauda equine syndrome25, 26, 27. Konig et al. report that the occurrence rate of nerve injury in U‐shaped fractures was 94.3%28. In our study14 patients had neurological deficiencies to different degrees. In some cases, the L5 nerve can be injured as a result of vertical shear displacement of the posterior pelvic ring and far‐out syndrome may occur. Lindahl and Hirvensalo indicate permanent neurological injury as a strongly poor prognostic factor29. Therefore, effort to recover the function of damaged nerves is vital in treatment.
Most surgeons agree that early surgery can result in better improvement of neurological impairment27, 30, but it is difficult to apply because the injures of TSD patient are always severe and the decompression operation cannot be tolerated in the acute phase.
Vaccaro et al. conclude that the chance of neurological improvement is very low when there are bilateral transections or avulsions of nerve roots31. Nevertheless, the sacral roots subjected to compression, contusion, or traction caused by displacement and angulation of sacral fracture fragments have a theoretical chance of recovery. The indications for surgical management including symptoms and signs of nerve injury are significant (Gibbons III, IV) or worsen after the traction, the free bone fragments are proved to compress nerves, and the sacral canal or sacral foremen have significant deformation and stenosis.
Decompression should be performed either indirectly with fracture reduction or directly with laminectomy or focal foraminotomy. Sacral laminectomy, complete or partial, should be performed if occlusion of the central canal is found on CT scan. The nerve roots should be traced to their anterior foraminal exit and any occupied free bone fragments must be removed. Sacral nerve root decompression should be performed before reduction even in the absence of neurological abnormality but CT scan indicates the presence of intraforaminal or intracanal bone fragments that may injure the nerve roots during fracture reduction.
Limitations
There are some limitations in our study. The size of sample is small, the follow‐up time is not long, and there is no control group, which may lead to the deviation of results and affect the validity of conclusions.
Conclusion
In conclusion, TSD comprises a series of severe injuries and is difficult to cure satisfactorily. The modified triangular fixation combined with various kinds of internal fixation shows satisfactory clinical outcomes in the treatment of TSD. Therefore, we recommend this technique for the treatment of TSD.
Supporting information
Supplementary Appendix S1 Demographic data of patients.
Disclosure: No author has any conflict of interest that relates to the content discussed in this manuscript.
References
- 1. Yi C, Hak DJ. Traumatic spinopelvic dissociation or U‐shaped sacral fracture: a review of the literature. Injury, 2012, 43: 402–408. [DOI] [PubMed] [Google Scholar]
- 2. Zhang YG, Jia J, Liu ZJ. Surgical treatment of traumatic spinopelvic dissociation with lumbopelvic fixation. Zhong hua Gu Ke Za Zhi, 2015, 35: 328–334 (in Chinese). [Google Scholar]
- 3. Lehmann W, Hoffmann M, Briem D, et al Management of traumatic spinopelvic dissociations: review of the literature. Eur J Trauma Emerg Surg, 2012, 38: 517–524. [DOI] [PubMed] [Google Scholar]
- 4. Gribnau AJ, van Hensbroek PB, Haverlag R, Ponsen KJ, Been HD, Goslings JC. U‐shaped sacral fractures: surgical treatment and quality of life. Injury, 2009, 40: 1040–1048. [DOI] [PubMed] [Google Scholar]
- 5. Formby PM, Wagner SC, Kang DG, Van Blarcum GS, Lehman RA Jr. Operative management of complex lumbosacral dissociations in combat injuries. Spine J, 2016, 16: 1200–1207. [DOI] [PubMed] [Google Scholar]
- 6. Williams SK, Quinnan SM. Percutaneous lumbopelvic fixation for reduction and stabilization of sacral fractures with spinopelvic dissociation patterns. J Orthop Trauma, 2016, 30: e318–e324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lindahl J, Mäkinen TJ, Koskinen SK, Söderlund T. Factors associated with outcome of spinopelvic dissociation treated with lumbopelvic fixation. Injury, 2014, 45: 1914–1920. [DOI] [PubMed] [Google Scholar]
- 8. Pan WB, Liang JB, Wang B, et al The invention of an iliosacral screw fixation guide and its preliminary clinical application. Orthop Surg, 2012, 4: 55–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chung HY, Suk KS, Lee HM, et al Growing rod technique for the treatment of the traumatic spinopelvic dissociation: a technical trick. Spine J, 2016, 16: e209–e214. [DOI] [PubMed] [Google Scholar]
- 10. Schildhauer TA, Josten CH, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight‐bearing. J Orthop Trauma, 2006, 20: S44–S51. [PubMed] [Google Scholar]
- 11. Holland CM, Moore MK, Valdivia Valdivia J. Traumatic spinopelvic dissociation after fall from a height with the treatment complicated by degenerative thoracic scoliosis. Spine J, 2015, 15: 1150–1151. [DOI] [PubMed] [Google Scholar]
- 12. Gupta P, Barnwell JC, Lenchik L, Wuertzer SD, Miller AN. Spinopelvic dissociation: multidetector computed tomographic evaluation of fracture patterns and associated injuries at a single level 1 trauma center. Emerg Radiol, 2016, 23: 235–240. [DOI] [PubMed] [Google Scholar]
- 13. Kane I, Ong A, Orozco FR, Post ZD, Austin LS, Radcliff KE. Thromboelastography predictive of death in trauma patients. Orthop Surg, 2015, 7: 26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dodwad SN, Niedermeier SR, Yu E, Ferguson TA, Klineberg EO, Khan SN. The Morel–Lavallée lesion revisited: management in spinopelvic dissociation. Spine J, 2015, 15: e45–e51. [DOI] [PubMed] [Google Scholar]
- 15. Scolaro JA, Chao T, Zamorano DP. The Morel‐Lavallée lesion: diagnosis and management. J Am Acad Orthop Surg, 2016, 24: 667–672. [DOI] [PubMed] [Google Scholar]
- 16. Daniels AH, DePasse JM, Eltorai AE, Palumbo MA. Perpendicular iliac screw placement for reinforcement of spinopelvic stabilization. Orthopedics, 2016, 39: e1209–e1212. [DOI] [PubMed] [Google Scholar]
- 17. Mansouri N, Graillon T, Farah K, Pesenti S, Blondel B, Fuentes S. Impact of surgical correction of a U‐shaped sacral fracture on sagittal spino‐pelvic alignment: regarding one case. Neurochirurgie, 2016, 62: 344–348. [DOI] [PubMed] [Google Scholar]
- 18. Liu ZJ, Jia J, Hu YC, et al Surgical treatment in unstable sacral fractures associated with lumbosacral junction injuries. Zhong hua Gu Ke Za Zhi, 2016, 36: 513–520 (in Chinese). [Google Scholar]
- 19. Käch K, Trentz O. Distraction spondylodesis of the sacrum in “vertical shear lesions” of the pelvis. Unfallchirurg, 1994, 97: 28–38. [PubMed] [Google Scholar]
- 20. Schildhauer TA, Ledoux WR, Chapman JR, Henley MB, Tencer AF, Routt ML Jr. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma, 2003, 17: 22–31. [DOI] [PubMed] [Google Scholar]
- 21. Hu X, Pei F, Wang G, He J, Kong Q, Tu C. Application triangular osteosynthesis for vertical unstable sacral fractures. Eur Spine J, 2013, 22: 503–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sagi HC. Technical aspects and recommended treatment algorithms in triangular osteosynthesis and spinopelvic fixation for vertical shear transforaminal sacral fractures. J Orthop Trauma, 2009, 23: 354–360. [DOI] [PubMed] [Google Scholar]
- 23. Hoffmann MF, Dudda M, Schildhauer TA. Unilateral triangular lumbopelvic stabilization: indications and techniques. Unfallchirurg, 2013, 116: 985–990. [DOI] [PubMed] [Google Scholar]
- 24. Berber O, Amis AA, Day AC. Biomechanical testing of a concept of posterior pelvic reconstruction in rotationally and vertically unstable fractures. J Bone Joint Surg Br, 2011, 93: 237–244. [DOI] [PubMed] [Google Scholar]
- 25. Khan JM, Marquez‐Lara A, Miller AN. Relationship of sacral fractures to nerve injury: is the denis classification still accurate?. J Orthop Trauma, 2017, 31: 181–184. [DOI] [PubMed] [Google Scholar]
- 26. SafaieYazdi A, Omidi‐Kashani F, Baradaran A. Intrapelvic lumbosacral fracture dislocation in a neurologically intact patient: a case report. Arch Trauma Res, 2015, 4: e25439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ayoub MA. Displaced spinopelvic dissociation with sacral cauda equina syndrome: outcome of surgical decompression with a preliminary management algorithm. Eur Spine J, 2012, 21: 1815–1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Konig MA, Jehan S, Boszczyk AA, Boszczyk BM. Surgical management of U‐shaped sacral fractures: a systematic review of current treatment strategies. Eur Spine J, 2012, 21: 829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lindahl J, Hirvensalo E. Outcome of operatively treated type‐C injuries of the pelvic ring. Acta Orthop, 2005, 76: 667–678. [DOI] [PubMed] [Google Scholar]
- 30. Chen HW, Liu GD, Zhao GS, Pan J. Isolated u‐shaped sacral fracture with cauda equina injury. Orthopedics, 2011, 34: 316–320. 10.3928/01477447-20110228-25. [DOI] [PubMed] [Google Scholar]
- 31. Vaccaro AR, Kim DH, Brodke DS, et al Diagnosis and management of sacral spine fractures. Instr Course Lect, 2004, 53: 375–385. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Appendix S1 Demographic data of patients.


