Abstract
Objective
To analyze the early complications and causes of oblique lateral interbody fusion, and put forward preventive measures.
Methods
There were 235 patients (79 males and 156 females) analyzed in our study from October 2014 to May 2017. The average age was 61.9 ± 0.21 years (from 32 to 83 years). Ninety‐one cases were treated with oblique lateral interbody fusion (OLIF) alone (OLIF alone group) and 144 with OLIF combined with posterior pedicle screw fixation through the intermuscular space approach (OLIF combined group). In addition, 137/144 cases in the combined group were primarily treated by posterior pedicle screw fixation, while the treatments were postponed in 7 cases. There were 190 cases of single fusion segments, 11 of 2 segments, 21 of 3 segments, and 13 of 4 segments. Intraoperative and postoperative complications were observed.
Results
Average follow‐up time was 15.6 ± 7.5 months (ranged from 6 to 36 months). Five cases were lost to follow‐up (2 cases from the OLIF alone group and 3 cases from the OLIF combined group). There were 7 cases of vascular injury, 22 cases of endplate damage, 2 cases of vertebral body fracture, 11 cases of nerve injury, 18 cases of cage sedimentation or cage transverse shifting, 3 cases of iliac crest pain, 1 case of right psoas major hematoma, 2 cases of incomplete ileus, 1 case of acute heart failure, 1 case of cerebral infarction, 3 case of left lower abdominal pain, 9 cases of transient psoas weakness, 3 cases of transient quadriceps weakness, and 8 cases of reoperation. The complication incidence was 32.34%. Thirty‐three cases occurred in the OLIF alone group, with a rate of 36.26%, and 43 cases in the group of OLIF combined posterior pedicle screw fixation, with a rate of 29.86%. Fifty‐seven cases occurred in single‐segment fusion, with a rate of 30.0% (57/190), 4 cases occurred in two‐segment fusion, with a rate of 36.36% (4/11), 9 cases occurred in three‐segment fusion, with a rate of 42.86% (9/21), and 6 cases occurred in four‐segment fusion, with a rate of 46.15% (6/13).
Conclusion
In summary, OLIF is a relatively safe and very effective technique for minimally invasive lumbar fusion. Nonetheless, it should be noted that OLIF carries the risk of complications, especially in the early stage of development.
Keywords: Complications, Lumbar, Oblique lateral interbody fusion, Pedicle screw
Introduction
Anterior or anterolateral interbody fusion, including anterior lumbar interbody fusion (ALIF), direct lateral interbody fusion (DLIF), extreme lateral interbody fusion (XLIF), and oblique lateral interbody fusion (OLIF) have become popular techniques for treating spinal illnesses such as degenerative disc disease, spondylolisthesis, recurrent disc herniation, and spinal deformity1, 2, 3, 4, 5, 6.
Anterior lumbar interbody fusion was introduced by Carpener in 19321. This treatment method provides direct access to the disc with potential improvement in fusion rate, but also brings the risk of injury to the iliac vessels, peritoneal content and ureteral. In 1997, Mayer found that that anterior lumbar interbody fusion might cause neurologic injuries when performing fusion through a 4‐cm skin incision, and via the standardized muscle‐splitting approach2. To overcome the above problem and to reduce approach‐related complications, OLIF was introduced in 20123. The advantages of this approach include: (i) low effect on the retroperitoneal vasculature, peritoneum, abdominal viscera, and prevertebral plexus (compared to ALIF); (ii) lower probability of damaging the psoas, lumbar plexus, lumbosacral and sacral plexus (compared to DLIF or XLIF); (iii) lower risk of damaging the sacrospinalis and not affecting the endorhachis and the nerve root (compared with traditional posterior lateral interbody fusion; i.e. PLIF or TLIF). Furthermore, OLIF has relatively broad indications, its procedure relays on small incision, it brings low risk of post‐treatment trauma or bleeding and offers good stability and quick recovery. The stand‐alone approach has shown the ability to reduce trauma, to greatly reduce the operation time, and to further promote the clinical application of OLIF6, 7, 8, 9. Anatomy and clinical research indicates that the oblique lateral interbody fusion does not damage sacrospinalis and does not affect the endorhachis and the nerve root compared with traditional posterior lateral interbody fusion (PLIF, TLIF)10, 11, 12, 13, 14. To sum up, the OLIF method is considered a relatively safe approach. Nevertheless, it has a learning curve and relative complications, especially in the early stages of the development of the technique, where complications have been reported to range from 3.7% to 66.7%2, 7, 15, 16, 17, 18, 19, 20, 21, 22, 23. To our knowledge, Mehren et al. are the first to report on intraoperative and postoperative complications of OLIF; nevertheless, their result derived from a single‐center study with small cohorts9. Few multi‐center studies have been reported. The purpose of the present study was: (i) to report the incidence and proportion of perioperative complications; and (ii) to analyze the causes of early complications based on multi‐center results.
Materials and Methods
Inclusion and Exclusion Criteria
Patients were selected based on the following inclusion criteria: (i) patients with lumbar spinal stenosis, giant lumbar intervertebral disc herniation, in situ recurrent lumbar disc herniation, degenerative slippage I–II degrees, lumbar spondylolysis with/without vertebral slippage I–II degrees, and lumbar degenerative scoliosis; (ii) segments L1–L5; and (iii) patients who experienced chronic low back pain with or without lower limb radiative pain (unilateral or bilateral), for whom conservative treatments had no effect.
Exclusion criteria were: (i) lumbar intervertebral disc herniation was not inclusive, such as with fibrous ring rupture or nucleus pulposus dissociation; (ii) severe lumbar spinal canal stenosis required direct decompression of the vertebral canal; (iii) vertebral slippage II or higher, including degenerative or spondylolysis slippage; (iv) severe osteoporosis; (v) spontaneous fusion of lumbar joint in the lesion segment; and (vi) peritoneal surgery was performed before.
General Data
There were 79 men and 156 women, with a mean age of 61.9 ± 0.21 years (from 32 to 83 years). Among 235 patients, 91 cases were treated with OLIF alone (OLIF alone group) and 144 with OLIF combined with posterior pedicle screw fixation through the intermuscular space approach (OLIF combined group). In addition, 137/144 cases in the combined group were primary treated by posterior pedicle screw fixation, while the treatments were postponed in 7 cases.
Disease types included: lumbar degenerative diseases in 44 cases, lumbar spinal stenosis in 82 cases, lumbar degenerative slippage in 49 cases, lumbar spondylolysis with or without vertebral slippage in 16 cases, lumbar degenerative scoliosis in 19 cases, discogenic lumbago in 21 cases, and primary intervertebral space inflammation in 4 cases. In addition, there were 190 cases of single fusion segment, 11 of 2 segments, 21 of 3 segments, and 13 of 4 segments.
Surgical Procedure
All patients were treated with general anesthesia, placed in a standard right side position, while their hip was kept from flexing; the axilla and hip were fixed with wide cloth glue. The incision was positioned using a C‐arm.
The single segment incision was fused to extend 2 cm along the anterior margin of the vertebral body of the vertebral space of the lesion, 1 cm backward, while the incision length was 3‐cm long. The two‐segment incision were fused into an oblique incision in the middle of the two segmental lesions, and the anterior margin of the vertebral body was still extended 2–3 cm, and 2 cm backward, and its length was approximately 4–5 cm long. The three‐segment incision was fused to the center of the three segments for a slightly longer oblique incision with a length of approximately 6 cm. The four‐segment incision consisted of two incisions, each with a length of 4–5 cm.
The obliquus externus abdominis and obliquus internus abdominis were bluntly dissected, the transversus abdominis was incised, and then the external abdominal fat and abdominal organs were gently pushed aside. A periosteal detacher was used to gently push back the psoas muscle, and then a retractor was used to pull the psoas muscle to the dorsal side and pull the abdominal organs together with the extraperitoneal fat to the ventral side. Consequently, the intervertebral space of the lesion was exposed. After the guide needle was correctly inserted at 1/3 of the intervertebral space with the help of the C‐arm, the expansion sleeve and the channel with the light source were inserted. Then the sleeve was removed and the channel was fixed (keeping the channel in an oblique direction). The rimer was vertically inserted into the intervertebral space, and the position of the intervertebral space and the endplate direction were determined by the C‐arm. If the endplate bone condition was good, the intervertebral space was expanded by rimer; otherwise, the intervertebral space was expanded by cage model. After the height and length of cage were determined by the C‐arm, the cage (Sofamor, Minnesota, USA) combined with bone block was inserted vertically into the intervertebral space. (Note: The absorbable suture was used to bind the cage and bone block to prevent the bone block from falling off.) In 43 cases iliac bone was used as autograft, while in 136 cases artificial bone was used (Wright, Tennessee, USA). In 56 cases the allogenic bone was used. Finally, the wound was sutured after bleeding ceased.
No drainage tube was used, except in 3 cases (1 case of left common iliac artery injury, 1 case of left iliac vein injury, and 1 case of left ovarian vein injury).
Postoperative Management
After surgery, anti‐infective preventive measures and low‐dose hormones were prescribed. In addition, patients were asked to perform active ankle dorsiflexion and passive straight leg raising. The drainage catheter was removed within 48 h after surgery when the amount of extracted fluid was <50 mL/24 h. Two to three days after surgery, patients were asked to do out‐of‐bed activities while wearing orthotics, and lower back and abdominal muscle exercise were progressively performed after 6 weeks.
Evaluation Method and Observation Index
Spinal dura mater tear, cauda equina injury, root nerve injury, abnormal bleeding, vertebral pedicle fracture, and endplate injury were monitored during the surgery; cerebrospinal fluid leakage, poor wound healing, wound infection, lower limb swelling, abnormal lumbar pain, lower limb nerve root injury, abnormal urination, and defecation were monitored after surgery. The visual analogue scale (VAS) scores and Oswestry disability index (ODI) were recorded before surgery and at final follow‐up.
Anteroposterior and lateral radiographs of the lumbar spine were obtained at postoperative 3–5 days and 3, 6, and 12 months. Hyperflexion and hyperextension positions radiographs of lumbar spine were obtained 12 months after surgery. CT images of the lumbar spine were obtained at postoperative 3–5 days and 12 months post‐surgery. The displacement and subsidence of interbody fusion cage, endplate, interbody fusion, and degeneration of adjacent segments were also detected.
Statistical Analysis
All data were statistically processed using SPSS 20.0 software. The measurement data were expressed with mean ± standard deviation. A t‐test was performed on the VAS and ODI index to compare the preoperative state with final follow‐up state. A P < 0.05 was considered statistically different.
Results
General Characteristics
Average follow‐up time was 15.6 ± 7.5 months (ranged from 6 to 36 months). Five cases were lost to follow‐up (two cases from OLIF alone group and three cases from OLIF combined group). The length of the incision ranged from 3 to 7 cm (4.2 ± 0.7 cm); the operation time ranged from 40 to 460 min (115 ± 66 min), while the time of OLIF ranged from 40 to 120 min (55.2 ± 14.6 min); the intraoperative blood loss ranged from 20 to 720 mL (120 ± 72.5), while every each segment of OLIF averaged 32.9 ± 15.1 mL.
Clinical Results
The VAS score (6.7 ± 2.3 points) and ODI index (36.5% ± 7.7%) were both significantly higher before surgery compared to those observed after the final follow‐up (VAS score: 1.4 ± 0.8 points; ODI: 9.4% ± 3.6%) (t = 7.21, P = 0.033; t = 8.11, P = 0.025, respectively).
Except for 9 cases (4 cases in the OLIF alone group and 5 cases in the OLIF combined group), interbody fusion was successfully performed in 221 cases. The total rate of interbody fusion was 96.09%: 95.51% in the OLIF alone group and 96.45% in the OLIF combined group.
Intraoperative Complications
Vascular Injury
Vascular injury was observed in 7 cases (Table 1), including segmental vessel injury in 4 cases (1.7%) and great vessels in 3 cases (1.29%). Among those, left arteria iliaca communis injury was repaired in 1 patient (0.43%) and left venae iliaca communis injury was locally repaired in 1 case (0.43%); while 1 case of ovarian vein injury was repaired by local pressing hemostasis (0.43%).
Table 1.
Intraoperative and postoperative complications of OLIF
| Complications | Intraoperative cases (%) | Postoperative cases (%) |
|---|---|---|
| Segmental vascular injury | 4 (1.70) | — |
| Iliac artery injury | 1 (0.43) | — |
| Ovarian venous injury | 1 (0.43) | — |
| Venae iliaca communis injury | 1 (0.43) | — |
| End plate damaged and cage embedded | 22 (9.36) | — |
| Vertebral fracture | 3 (1.28) | — |
| Iliac crest pain | — | 3 (1.28) |
| Contralateral nerve root injury | — | 1 (0.43) |
| Sympathetic chain injury | — | 3 (1.28) |
| Pain and numbness in front of left thigh | — | 7 (2.98) |
| Right psoas major hematoma | — | 1 (0.43) |
| Transient psoas weakness | — | 9 (3.83) |
| Transient quadriceps weakness | — | 3 (1.28) |
| Left lower abdominal pain | — | 3 (1.28) |
| Incomplete ileus | — | 2 (0.85) |
| Acute heart failure | — | 1 (0.43) |
| Cage sedimentation or shifting | — | 18 (7.66) |
| Cerebral infarction | — | 1 (0.43) |
OLIF, oblique lateral interbody fusion.
Damaged End Plate and Embedded Cage
Damaged end plate and embedded cage were observed in 22 cases; among these, 10 patients received first phase posterior pedicle screw fixation; 1 case was delayed for 3 weeks because of acute heart failure, 1 case was delayed for 4 weeks because of poor wound healing with the waist moxibustion, and 12 patients used a thoracic lumbar brace for protection and strengthening.
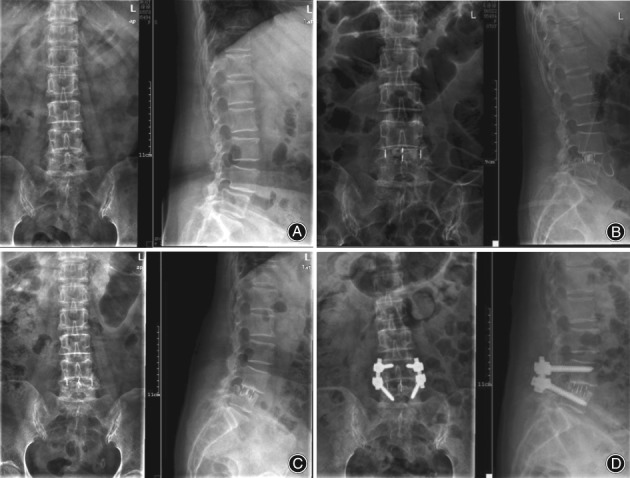
Among the 3 cases with vertebral fractures, 1 case had a fracture in the right front of the L2 vertebral body, which consequently healed well after 3 months of conservative treatment (Fig. 1). Another 2 cases received first phase posterior pedicle screw fixation.
Figure 1.

(A) Woman of 62 years old, with spinal stenosis of L2–3, L3–4, and L4–5. Preoperative lumbar X‐ray showed that the lumbar hyperostosis was obvious and the intervertebral space height decreased. (B) Postoperative lumbar X‐ray showed that the position of cages was fine and the intervertebral space height recovered. (C) Postoperative lumbar CT showed a fracture at the bottom right of L2 vertebral body. (D) After 3 months of conservative treatment, lumbar X‐ray showed that the position of the cage was fine and the intervertebral space height had been maintained.
In 14 cases the fusion graft portion came off during implantation without special treatment. In the latter case, the cages were wrapped around the absorbable suture and then implanted into the intervertebral space. So the phenomenon of bone graft off did not appeared in the later cases.
Postoperative Complications
There was no incision infection and necrosis. In addition, no pedicle screw loosening or rupture was found.
Nerve Injury
There were 3 (1.28%) cases of left sympathetic chain injury which recovered 3–5 days after surgery (1.28%). Pain and numbness in front of the left thigh was observed in 7 cases (2.98%); those patients recovered 5–7 days after surgery. There were 9 cases (3.83%) of transient psoas weakness and 3 cases (0.43%) of transient quadriceps weakness which recovered 3–5 days after surgery.
Cage‐related Complications
There were 18 cases of cage sedimentation or cage transverse shifting in the OLIF alone group (Figs 2, 3); those patients were successfully treated after conservative therapy.
Figure 2.
(A) Woman of 70 years old with lumbar spondylolisthesis of L4. Preoperative lumbar X‐ray showed that the L4 vertebral body had slipped forward. (B) Postoperative lumbar X‐ray showed that the position of the L4 vertebral body was restored and the intervertebral space height had recovered. However, the superior endplate of L5 was damaged, and the cage was inserted into the L5 vertebral body. (C) After 3 months, the lumbar X‐ray showed that the intervertebral space height had decreased obviously and the cage continued sinking. (D) The patient received posterior pedicle screw fixation. Three months later, the lumbar X‐ray showed that the intervertebral space height had stopped decreasing.
Figure 3.
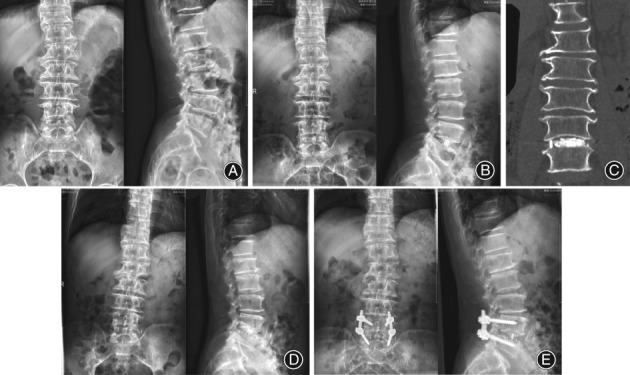
(A) Man, 63 years old, spinal stenosis of L4–5. Preoperative lumbar X‐ray showed that the lumbar hyperostosis was obvious and the intervertebral space height had decreased. (B) Postoperative lumbar X‐ray showed that the position of cages was fine and the intervertebral space height had recovered. (C) Postoperative lumbar CT showed that the position of cages was fine. (D) After 1.5 months, the lumbar X‐ray showed that the cage had slid to the left. (E) The patient received posterior pedicle screw fixation. Three months later, the lumbar X‐ray showed that the cage stopped shifting.
Pain
Iliac crest pain occurred in 3 cases (1.28%) and was relieved after 2–3 weeks. There was 1 case of contralateral nerve root injury (0.43%), because of the cage comperessed contralateral nerve root; the patient recovered from injury after adjusting the cage position and posterior pedicle screw fixation. Left lower abdominal pain occurred in 3 cases (1.28%); those patients all recovered 5–21 days later.
Others
Right psoas major hematoma occurred in 1 case (0.43%), and the hematoma had been absorbed by 3‐month follow‐up. Incomplete ileus occurred in 2 cases, with the patient recovering 2–5 days later (0.85%). Acute heart failure occurred in 1 case, with the patient recovering after treatment (0.43%). There was 1 case of cerebral infarction, with the patient still hemiplegyed on one side and unable to walk (0.43%).
Complication Incidence
There were a total 92 cases of complications in the intraoperative and postoperative stages, including 16 cases with 2 combined complications, 8 cases of cage sedimentation with endplate damage, 1 case of acute heart failure with endplate damage, 5 cases of cage sedimentation, 1 case of cage shifting that received posterior pedicle screw fixation, and 1 case of contralateral nerve root injury that received posterior cage adjustment and posterior pedicle screw fixation.
Therefore, there were actually 76 cases, and the complication incidence was 32.34%. Thirty‐three cases occurred in the OLIF alone group, with a rate of 36.26%, and 43 cases in the group of OLIF combined posterior pedicle screw fixation, with a rate of 29.86%. Fifty‐seven cases occurred in single‐segment fusion, with a rate of 30.0% (57/190), four cases occurred in two‐segment fusion, with a rate of 36.36% (4/11), nine cases occurred in three‐segment fusion, with a rate of 42.86% (9/21), and six cases occurred in four‐segment fusion, with a rate of 46.15% (6/13).
The complication incidence for the four different numbers of fusion segments varied: the single segment fusion had the lowest and the four‐segment fusion had the highest incidence of complications.
Discussion
Oblique lateral interbody fusion technology has been proven as a relatively safe approach4, 5, 6, 24, 25. Nevertheless, the occurrence of complications is inevitable, and the incidence of complications after surgery fluctuates from 3.7% to 66.7%2, 4, 5, 6, 7, 15, 16, 17, 18, 19, 20, 21, 22, 23. In the present study, the incidence was 32.3% and the following characteristics were revealed: First, the complications incidence varies between different operation groups. The incidence in the OLIF alone group (36.26%) was higher compared to the OLIF combined group (29.86%), mainly because the cage sedimentation incidence in the OLIF alone group was higher than in the OLIF combined group with posterior pedicle screw fixation. Second, the complication incidence of different fusion segments was different. In the present study, there were 57 cases with single‐segment fusion with a rate of 30.0%, 4 cases with two‐segment fusion with a rate of 36.36%, 9 cases with three‐segment fusion with a rate of 42.86%, and 6 cases with four‐segment fusion with a rate of 46.15%.
Endplate Damaged, Cage Embedded, Cage Sedimentation, and Shifting Post‐surgery
Our study showed that the incidence of these complications after surgery was 13.62%, and that these were the most common complications of OLIF. Because damaged endplate, embedded cage, cage sedimentation, and shifting were highly correlated, with the endplate lesions potentially having the main role, these complications are discussed further. In recent years, good clinical results of the OLIF without additional posterior pedicle screw fixation have been reported, but the base condition was without endplate damage6, 7, 8, 9. Therefore, the surgical method should be changed, and the posterior fixation should be applied in the operation if there is endplate injury. Since the average age of patients in this group was 61.9 years (oldest 83 years), and 156 (66.38%) cases were women, osteoporosis was the main pathological basis for endplate injury. Of course, improper practice, such as the direct use of a sharp reamer for the removal of the nucleus, or the incorrect direction applied during intervertebral treatment, were also identified as common causes of injury. In addition, obesity, high iliac crest, intervertebral space stenosis, poor stability of lesion segments, multiple segmental fusion, small or big cage (including height or length), and lack of posterior pedicle screw fixation could also explain these complications. The OLIF technique required the cage to be placed in regions two and three of the lumbar vertebra, the lumbar spine, especially the lower lumbar spine, which was behind the load conduction center. It is unknown whether the endplate thickness or mechanical strength of regions two and three were weaker compared to those of regions three or four, and the anatomy and biomechanics research still can not explain. The following aspects should be considered for the prevention of endplate damage, embedded cage, cage sedimentation, and shifting: (i) ensuring that the standard lateral position is secured; (ii) providing standard and clear anteroposterior and lateral film of lumbar spine with the C‐arm; (iii) ensuring the correct direction during the process of lumbar disc excision, endplate treatment, and intervertebral space support; (iv) using a blunt force to gently and sequentially open the intervertebral column; (v) protecting the integrity of the endplate when cleaning the endplate cartilage; (vi) the fuse should be large enough to maintain the tension of the fiber ring, but still avoid too much (the length is relevant because it should make the cage stand between the two vertebral bodies); and (vii) necessary additional posterior pedicle screw fixation, with presence of the following: body mass index more than 30 kg/m2, lumbar osteopenia or osteoporosis (t values <1.0), local instability (such as lumbar olisthe over II degrees or more), three or more‐segment fusion, or intraoperative endplate damage.
Never Injury
The nerves that might be injured during OLIF are: the iliohypogastric nerve, the ilioinguinal nerve, the genitofemoral nerve, the femoral nerve, the sympathetic chain, the lumbar plexus, the lumbosacral trunk, the caudal nerve, and the nerve root. There were 7 cases of anterolateral thigh pain or numbness, 3 cases of sympathetic chain injury, and 1 case of contralateral nerve root injury, with an incidence of 4.68%. Due to the specific anatomical path of OLIF, the possibility of nerve injury during surgery was lower9, 10, 13, 21. Possible injuries were: injury to the iliohypogastric nerve or the ilioinguinal nerve during the separation of internal oblique muscle and transverse abdominal, injury to the genitofemoral nerve and the sympathetic chain during pulling psoas major, and injury to the caudal nerve or the nerve root during incorrect direction of cage inserting. In addition, the psoas major hematoma (same side or opposite side) might compress the lumbar plexus and lumbosacral trunk. Therefore, familiar anatomy, right path, clear vision, careful performance of the operation, especially in the separation of psoas major and vascular sheath, and avoidance of electric coagulation or electric knife cut, could minimize nerve injury. Nonetheless, it has been argued that OLIF technology which refers to oblique extroversion is only the anatomic approach and channel direction, while the direction of intervertebral disc operation and cage implanting are perpendicular to the vertebral body in sagittal plane. Thus, OLIF technology prevents the operating equipment or cage from diagonally reaching into the contralateral vertebral canal or from injuring the contralateral nerve root. If unexplained ipsilateral or contralateral nerve injury does occur after surgery, imaging should be performed as soon as possible to clarify the reasons and provide timely treatment.
Psoas or Quadriceps Weakness
There were 9 cases of transient psoas weakness and 3 cases of transient quadriceps weakness. Moreover, there were 2 cases in single‐segment fusion, 4 cases in three‐segment fusion and 3 cases in four‐segment fusion. These could be explained by: (i) the superficial layer of psoas originating from the anterosuperior vertebral body being stripped and exposed in the intervertebral disc (the psoas nerve branches have been shown to be located across intervertebral discs, which could only be damaged when stripping or pulling the psoas22, 26); (ii) if the incision is not properly planned, for example the incision was after partial anterior margin of the vertebral body, the psoas stripping area and the pressure of psoas would be larger; (iii) the psoas was too much on the dorsal side, or the angle of channel was too vertical or oblique; (iv) the hematoma was formed after surgery; and (v) multi‐segment fusion was more likely to strip, stimulate, and pull the psoas. To sum up, as long as the incision is accurate, the lumbar muscle is gently dissected, the use of electric knife is reduced to a minimum, and the channel is correctly placed, the degree and possibility of lumbar muscle injury could be greatly reduced. Of course, the lumbar muscle injuries in this study were transient, and were mainly caused by lumbar plexus or lumbosacral trunk injuries when stripping and pulling the psoas, and patients recovered after undertaking rehabilitation exercises. Therefore, it is particularly necessary to operate in the nerve security zone in different lumbar fusion segments.
Vascular Injury
Vascular injury is also a common complication of the OLIF approach, which mainly includes segmental vessels and iliac vessels injury16, 21, 23. There were 7 cases of vascular injury with an incidence of 2.98%, which was lower than for nerve and psoas injuries8, 9. Vascular injury might occur either on the ipsilateral or contralateral side, and in the present study 7 cases of vascular injury occurred on the ipsilateral side (left). Although the incidence of vascular injury in our study was low, after occuring, the situation can become life threatening. There was 1 case of arteria iliaca communis injury, which did not have serious consequences due to being discovered and treated timely. There was 1 case of venae iliaca communis injury during repair treatment of and 1 case of ovarian venous injury during packing treatment. The potential of the OLIF technique for vessel injury was mainly evident during incision exposure, separation of lumbar muscle and vascular sheath, insertion of channel fixation screw, and deep clearance of the intervertebral space. In particular, there was a higher risk of vascular injury in the cases of anatomical variation, including high blood vessel bifurcation, abnormal blood vessel orientation, and the disappearance of the gap between the blood vessels and the psoas muscle. Some researchers have reported that the position of the abdominal aortic bifurcation greatly changes, while the distance between the vascular sheath and the psoas muscle varies from person to person, with especially large variation of the venae iliolumbalis and ascending lumbar vein12, 27, 28, 29, 30, 31, 32, 33.
In our study, there was 1 case of left common iliac artery injury, which was caused by the left common iliac artery being pushed backwards and oppressed by sleeve, and subsequently damaged when implanting screws. The following suggestions could be useful in preventing vascular injuries: (i) familiarity with the anatomy of the lumbar spine, especially using CT and MRI examination to master the bifurcation of the iliac vessels and the relationship between psoas and psoas vessels (the iliac angiography and 3‐D reconstruction of lumbosacral vertebra should be examined if necessary); (ii) using gauze or Cobb to push the psoas aside when operating in the gap between the psoas and vagina vasorum, making sure not to exceed the lateral vertebral body margin and not to use sharp instruments to grab or nibble in the deep part of the vertebral space; (iii) according to the anatomy of lumbar segment vessels, the channel fixation screws should be inserted in the inferior endplate of the upper vertebral body12; (iv) checking again and confirming that there is no active bleeding in the incision after removal of the channel; and (v) after surgery, once the patient's blood pressure fluctuates or falls rapidly, the possibility of vascular injury should be taken into consideration and should be checked and treated timely.
Vertebral Fractures
Vertebral fractures have been reported as a rare complication of OLIF techniques8, 34, 35, and in the present study, there were only 3 cases with an incidence of 1.28%. Once the vertebral fracture occurs, patients should remain in bed, because it can affect the stability of the cage and the ultimate osseous fusion, and even increase the risk of renovation. Vertebral fracture had the cause of osteoporosis, but the main factor might be surgery. For example, the direction was not accurate when inserting the test mode in the operation and selected too large test mode and cage. The treatment of vertebral fractures was based on the location, morphology, size, and separation of fractures. Most vertebral fractures did not need special treatment.
Lower Abdominal Pain
There were 3 cases of lower abdominal pain in our study, with no identified abnormalities detected during CT, MRI, and ultrasound examination. All of the 3 cases recovered within 5–21 days without special treatment. The reason might be the iliac subventral nerve injury, psoas injury, or left lower abdominal hematoma. If lower abdominal pain occurs, examination and observation are necessary.
Other complications, such as ureteral injury, peritoneal injury, abdominal visceral injury, and deep hematoma (ipsilateral or contralateral) had very low incidence. Incision infection and cauda equina injury did not occur in the present study5, 9, 18, 22, 23, 36, 37. The causes of ureteral injury, peritoneal injury, and abdominal visceral injury might be related to the incorrect surgical approach.
Limitations
Because this was a multicenter study, the surgical experience of doctors for each group, surgical technology, case selection, and postoperative treatment was not the same. Therefore, complication incidences varied across groups, revealing different characteristics, and, thus, affecting the postoperative results and data comparability.
The follow‐up time was 6–36 months (15.6 ± 7.5 months). With the extension of follow‐up time, complications would increase, such as internal fixation loosening or fracture, cage loosening or shifting, and intervertebral height reduction.
The complication characteristics and incidence of different diseases have not been summarized or statistically analyzed in the present study.
Conclusion
In summary, OLIF is a relatively safe and very effective technique for minimally invasive lumbar fusion. Nonetheless, it should be noted that OLIF has the risk of complications, especially in the early stages of development. Although most of the complications are transient and bring no lasting and substantial damage to the patients, there are some serious and potentially life‐threatening complications. The OLIF technique is not a simple operation but a very demanding technique during which a special emphasis should be placed on the following. First, surgeons should have a rich experience in lumbar anatomy and lumbar anterior or lateral surgery, and they should be able to judge, discover, and treat effectively serious complications, such as vascular injury, if they should occur. Second, surgeons should undergo systematic and comprehensive training, including theoretical study, corpse surgery, and participating in operation demonstrations. Surgeons should also gain greater understanding of the surgical indications, operation characteristics, complications and preventive measures. Third, all operations should be performed under direct vision. Good familiarization with anatomy, good planning, and enough lighting are necessary for making the small incision. The incision length should be 3–7 cm (4.2 ± 0.7 cm). Fourth, although the indications of OLIF are relatively broad, it is recommended to choose cases from simple to complex and from single segment to multiple segments. Fifth, treating by stand‐alone should be prudent and increasing the follow‐up time (monthly outpatient follow‐up during the first 3 months after surgery) and for patinets to wear a thoracolumbar vertebra brace. Once cage sedimentation or shifting, accompanied with clinical symptoms and signs are identified, posterior pedicle screw fixation should be performed. Finally, a right oblique lateral approach is not recommended because of the anatomical characteristics of the lumbar, the difference in the arteriovenous structure and elasticity, the high incidence of lumbar lateral anterior vein injury, and the difficulty of repair after large vein injury30, 31, 38, 39, 40.
Acknowledgement
I would like to express my appreciate to all those who helped me during the writing of this thesis. My deepest gratitude goes first and foremost to Professor Shun‐wu Fan, my supervisor, for his constant encouragement and guidance. He has walked me through all the stages of the writing of this thesis. Without his consistent and illuminating instruction, this thesis could not have reached its present form. Second, I would like to express my heartfelt gratitude to my colleagues, who helped me a lot in this research. Last my thanks would go to my beloved family for their loving considerations and great confidence in me all through these years.
Disclosure: This study was supported by the National Natural Science Foundation of China (81271971, 81472064), the Zhejiang Provincal Natural Science Foundation (LQ13H060002, LQ15H090002), the Zhejiang Provincal Medical and Health General Project (2015KYA133), the Zhejiang Provincal Medical and Health Research Fund Project (2017KY091), and the Zhejiang Provincal Education Department Project (Y201017108).
References
- 1. Carpener N. Spondylolisthesis. Br J Surg, 1932, 19: 374–386. [Google Scholar]
- 2. Mayer HM. A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine (Phila Pa 1976), 1997, 22: 691–699. [DOI] [PubMed] [Google Scholar]
- 3. Silvestre C, Mac‐Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini‐open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J, 2012, 6: 89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ohtori S, Orita S, Yamauchi K, et al Mini‐open retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J, 2015, 56: 1051–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Molloy S, Butler JS, Benton A, Malhotra K, Selvadurai S, Agu O. A new extensile anterolateral retroperitoneal approach for lumbar interbody fusion from L1 to S1: a prospective series with clinical outcomes. Spine J, 2016, 16: 786–791. [DOI] [PubMed] [Google Scholar]
- 6. Zhang JF, Fan SW, Fang XQ, et al Clinical value of one‐level oblique lateral interbody fusion in the treatment of degenerative lumbar disc diseases. Zhonghua Gu Ke Za Zhi, 2017, 37: 80–88 (in Chinese). [Google Scholar]
- 7. Pimenta L, Marchi L, Oliveira L, Coutinho E, Amaral R. A prospective, randomized, controlled trial comparing radiographic and clinical outcomes between stand‐alone lateral interbody lumbar fusion with either silicate calcium phosphate or rh‐BMP2. J Neurol Surg A Cent Eur Neurosurg, 2013, 74: 343–350. [DOI] [PubMed] [Google Scholar]
- 8. Kwon YK, Jang JH, Lee CD, Lee SH. Fracture of the L‐4 vertebral body after use of a stand‐alone interbody fusion device in degenerative spondylolisthesis for anterior L3‐4 fixation. J Neurosurg Spine, 2014, 20: 653–656. [DOI] [PubMed] [Google Scholar]
- 9. Mehren C, Mayer HM, Zandanell C, Siepe CJ, Korge A. The oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications. Clin Orthop Relat Res, 2016, 474: 2020–2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moro T, Kikuchi S, Konno S, Yaginuma H. An anatomic study of the lumbar plexus with respect to retroperitoneal endoscopic surgery. Spine (Phila Pa 1976), 2003, 28: 423–428. [DOI] [PubMed] [Google Scholar]
- 11. Hu WK, He SS, Zhang SC , et al An MRI study of psoas major and abdominal large vessels with respect to the X/DLIF approach. Eur Spine J, 2011, 20: 557–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Orita S, Inage K, Sainoh T, et al Lower lumbar segmental arteries can intersect over the intervertebral disc in the oblique lateral interbody fusion approach with a risk for arterial injury: radiological analysis of lumbar segmental arteries by using magnetic resonance imaging. Spine (Phila Pa 1976), 2017, 42: 135–142. [DOI] [PubMed] [Google Scholar]
- 13. Oikawa Y, Eguchi Y, Watanabe A, et al Anatomical evaluation of lumbar nerves using diffusion tensor imaging and implications of lateral decubitus for lateral transpsoas approach. Eur Spine J, 2017, 26: 2804–2810. [DOI] [PubMed] [Google Scholar]
- 14. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI‐TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg, 2015, 1: 2–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wolfla CE, Maiman D, Coufal FJ, Wallace JR. Retroperitoneal lateral lumbar interbody fusion with titanium threaded fusion cages. J Neurosurg, 2002, 96: 50–55. [DOI] [PubMed] [Google Scholar]
- 16. Kaiser MG, Haid RW Jr, Subach BR, Miller JS, Smith CD, Rodts GE Jr. Comparison of the mini‐open versus laparoscopic approach for anterior lumbar inerbody fusion: a retrospective review. Neurosurgery, 2002, 51: 97–103. [DOI] [PubMed] [Google Scholar]
- 17. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976), 2015, 40: E175–E182. [DOI] [PubMed] [Google Scholar]
- 18. Sato J, Ohtori S, Orita S, et al Radiographic evaluation of indirect decompression of mini‐open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J, 2017, 26: 671–678. [DOI] [PubMed] [Google Scholar]
- 19. Graqnaniello C, Seex K. Anterior to psoas (ATP) fusion of the lumbar spine: evolution of a techniques facilitated by changes in equipment. J Spine Surg, 2016, 2: 256–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jin J, Ryu KS, Hur JW, Seong JH, Kim JS, Cho HJ. Comparative study of the difference of perioperative complication and radiological results: MIS‐DLIF (minimally invasive direct lateral lumbar interbody fusion) versus MIS‐OLIF (minimally invasive oblique lateral lumbar interbody fusion). Clin Spine Surg, 2018, 31: 31–36. [DOI] [PubMed] [Google Scholar]
- 21. Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1‐L5 (OLIF25) and at L5‐S1 (OLIF51) and evaluation of complication and fusion rates. Spine J, 2017, 17: 545–553. [DOI] [PubMed] [Google Scholar]
- 22. Abe K, Orita S, Mannoji C, et al Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: perspectives and indications from a retrospective, multicenter survey. Spine (Phila Pa 1976), 2017, 42: 55–62. [DOI] [PubMed] [Google Scholar]
- 23. Wang JY, Zhou ZJ, Fan SW, et al Early complications associated with oblique lateral interbody fusion in the treatment of degenerative lumbar diseases. Zhonghua Gu Ke Za Zhi, 2017, 37: 1006–1013 (in Chinese). [Google Scholar]
- 24. Zhang YH, White I, Potts E, Mobasser JP, Chou D. Comparison perioperative factors during minimally invasive pre‐psoas lateral interbody fusion of the lumbar spine using either navigation or conventional fluoroscopy. Global Spine J, 2017, 7: 657–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kim KT, Jo DJ, Lee SH, Seo EM. Oblique retroperitoneal approach for lumbar interbody fusion from L1 to S1 in adult spinal deformity. Neurosurg Rev, 2018, 41: 355–363. [DOI] [PubMed] [Google Scholar]
- 26. Mahan MA, Sanders LE, Guan J, Dailey AT, Taylor W, Morton DA. Anatomy of psoas muscle innervation: cadaveric study. Clin Anat, 2017, 30: 479–486. [DOI] [PubMed] [Google Scholar]
- 27. Chithriki M, Jaibaji M, Steele RD. The anatomical relationship of the aortic bifurcation to the lumbar vertebrae: a MRI study. Surg Radiol Anat, 2002, 24: 308–312. [DOI] [PubMed] [Google Scholar]
- 28. Moussallem CD, Abou Hamad I, EI‐Yahchouchi CA, et al Relationship of the lumbar lordosis angle to the abdominal aortic bifurcation and inferior vena cava confluence levels. Clin Anat, 2012, 25: 866–871. [DOI] [PubMed] [Google Scholar]
- 29. Molinares DM, Davis TT, Fung DA. Retroperationeal oblique corridor to the L2‐S1 intervertebral discs:an MRI study. J Neurosurg Spine, 2015, 9: 1–8. [DOI] [PubMed] [Google Scholar]
- 30. Davis TT, Hynes RA, Fung DA, et al Retroperitoneal oblique corridor to the L2‐S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine, 2014, 21: 785–793. [DOI] [PubMed] [Google Scholar]
- 31. Julian Li JX, Mobbs R, Phan K. Morphometric MRI imaging study of the corridor for the Oblique Lumbar Interbody Fusion (OLIF) technique at L1‐L5. World Neurosurg, 2018, 111: e678–e685. [DOI] [PubMed] [Google Scholar]
- 32. Jasani V, Jaffray D. The anatomy of the iliolumbar vein. A cadaver study. J Bone Joint Surg Br, 2002, 84: 1046–1049. [DOI] [PubMed] [Google Scholar]
- 33. Kiray A, Akcali O, Guvencer M, Tetik S, Alici E. Iliolumbar veins have a high frequency of variations. Clin Orthop Relat Res, 2004, 425: 252–257. [DOI] [PubMed] [Google Scholar]
- 34. Brier‐Jones JE, Palmer DK, ĭnceolu S, Cheng WK. Vertebral body fractures after transpsoas interbody fusion procedures. Spine J, 2011, 11: 1068–1072. [DOI] [PubMed] [Google Scholar]
- 35. Tender GC. Caudal vertebral body fractures following lateral interbody fusion in nonosteoporotic patients. Ochsner J, 2014, 14: 123–130. [PMC free article] [PubMed] [Google Scholar]
- 36. Kubota G, Orita S, Umimura T, Takahashi K, Ohtori S. Insidious intraoperative ureteral injury as a complication in oblique lumbar interbody fusion surgery: a case report. BMC Res Notes, 2017, 10: 193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chang J, Kim JS, Jo H. Ventral dural injury after oblique lumbar interbody fusion. World Neurosurg, 2017, 98: 881.e1–881.e4. [DOI] [PubMed] [Google Scholar]
- 38. Baker JK, Reardon PR, Reardon MJ, Heggeness MH. Vascular injury in anterior lumbar surgery. Spine (Phila Pa 1976), 1993, 18: 2227–2230. [DOI] [PubMed] [Google Scholar]
- 39. Zdeblick TA, David SM. A prospective comparison of surgical approach for anterior L4‐L5 fusion: laparoscopic versus mini anterior lumbar interbody fusion. Spine (Phila Pa 1976), 2000, 25: 2682–2687. [DOI] [PubMed] [Google Scholar]
- 40. Tribus CB, Belanger T. The vascular anatomy anterior to the L5‐S1 disk space. Spine (Phila Pa 1976), 2001, 26: 1205–1208. [DOI] [PubMed] [Google Scholar]


