Abstract
Schools are a recommended place for childhood obesity prevention. Local Wellness Policies (LWPs) establish guidelines for schools to provide opportunities for students to access nutritious foods and be physically active. Little is known about the impact of LWPs, when implemented, on students’ behavior and body mass index (BMI). The Wellness Champions for Change trial assesses the student-level impact of providing theory-based training and technical assistance to help schools implement LWPs. This 3-arm, cluster randomized controlled trial will take place in 30 low- or middle-income schools (15 elementary and 15 middle) in five Maryland school districts. Ten schools will receive both Wellness Champions for Change (WCC), which involves training teacher-led wellness teams, and Wellness Champions for Change-Student (WCC-S), which engages students as wellness team members. Ten schools will receive WCC only, and ten control schools will receive a delayed intervention. The RE-AIM framework will guide evaluation. Student Effectiveness measures will include BMI z-scores, self-reported diet patterns, and objectively-measured physical activity. The sample size (1080 students across 30 schools, followed for 2.5 years) will enable power (>0.8) to detect BMI z-score differences. A three-level linear mixed model that accounts for clustering will be used to assess Effectiveness. A mixed methods approach will assess school- and district-level Reach, Adoption, and Implementation. If effective, this approach will represent a sustainable, multi-level, school-based strategy to prevent childhood obesity. The evaluation framework will allow for the description of factors necessary to broadly disseminate this approach for obesity prevention on a large scale.
Keywords: Child/adolescent, Childhood obesity prevention, School-based obesity intervention, Local Wellness Policies, Physical activity, Healthy eating
BACKGROUND
Childhood obesity continues to prevail as a leading public health problem [1]. Obesity is a complex issue, as multiple factors (i.e., interpersonal, intrapersonal, environmental, policy) across multiple settings (i.e., home, school, neighborhood) influence obesity-related behaviors [2,3]. This process, reflected in the Social Ecological model (SEM), illustrates the need for strategies for obesity prevention to take a multi-level approach.
Schools are a strategic site for multi-level interventions because students spend much of their day in school, where their behaviors are influenced by interpersonal interactions with peers, teachers, and staff, and the physical environment and policies. It is critical that these exposures support healthy eating and physical activity (PA) [2–5]. In 2006, all school districts (i.e., Local Education Agencies) participating in federal meal programs were mandated to have a written Local Wellness Policy (LWP) that addresses goals for nutrition education, foods sold, physical education, and PA[6]. As the impact of LWPs depends on implementation, this mandate was expanded in 2016 to focus on school-level implementation [7,8].
Schools need support mechanisms to meet this mandate, including the formation and maintenance of wellness teams with key stakeholders (e.g., teachers, nurses, administrators, parents/students) that implement LWPs. Growing evidence supports this approach, particularly when teams meet best practices [9–11], are maintained over time, and receive theory-based training and support [12–14].
Although evidence is growing that providing training for wellness teams can augment LWP implementation, less research has focused on the process of this approach or its impact on students’ health behaviors and weight status. Additionally, despite the hypothesis that involving students on wellness teams will increase the likelihood that implementation will be sustainable and impact students, this practice is infrequently reported [9, 15–19].
In line with the SEM, a child’s risk for obesity is influenced not only by his/her school’s health-promoting environment, but also the home and neighborhood environments. Based on the Yerkes-Dodson Law, students with a moderate (not high or low) degree of support across these environments optimally benefit from multi-level interventions. For example, a school-based intervention may not be as effective for students whose homes display a high degree (e.g., consistent access to healthy foods) or low degree (e.g., access to only unhealthy foods) of support at baseline, compared to students with moderate support [20–21].
Wellness Champions for Change is a cluster randomized trial that builds on existing LWP implementation evidence. The trial evaluates the impact of a theory-based program designed to improve LWP implementation in schools on student-level behavior and weight outcomes, including the moderating effect of the home and neighborhood environment. The program includes (1) Wellness Champions for Change (WCC), a training and technical assistance curriculum to support teacher wellness teams and (2) Wellness Champions for Change-Student (WCC-S), a yearlong curriculum to support Student Leaders on wellness teams. The trial prioritizes collection of key implementation data and explores feasible dissemination methods that meet the unique needs of schools and districts [22,23]. This paper describes the trial protocol, including aims, design, framework, and evaluation plan.
METHODS
Trial Aims
WCC is a 3-arm cluster randomized controlled trial guided by RE-AIM, a pragmatic evaluation framework [15, 16] that includes Reach, Effectiveness, Adoption, Implementation, and Maintenance. This design compares outcomes among schools receiving (A) WCC + WCC-S (B) WCC only and (C) delayed control. The student-level effectiveness aims are:
-
(1)
to determine the impact of WCC on student-level health behaviors (diet and PA) and weight status (BMI z-score), as well as determine the added impact of WCC-S, compared to delayed control;
-
(2)
to examine factors (i.e., student perceptions, parent perceptions and behaviors, neighborhood characteristics) in the home environment that moderate the impact of WCC and WCC+WCC-S, hypothesizing that the interventions will have the most impact on students from moderately-health promoting homes/neighborhoods, compared to students from high- or low- health-promoting homes/neighborhood;
-
(3)
to assess the impact of participating on a wellness team (component of WCC-S) on Student Leaders’ advocacy and public health literacy skills and diet/PA behaviors, compared to Student Leaders in control schools, receiving a general Adolescent Health Curriculum (AHC)
In addition to these student-level effectiveness aims, the study aims to:
-
(4)
describe reach, organizational effectiveness, adoption, implementation, and maintenance of the curricula and LWPs during the study period;
-
(5)
describe dissemination of both interventions in eXtension, an online forum, as continuing education for teachers and administrators after study completion.
The study is a collaborative effort of the Maryland School Wellness Partnership, which includes members from University of Maryland Baltimore, University of Maryland College Park, Maryland State Departments of Education and Health, and University of Maryland Extension. It was approved by the Institutional Review Board (IRB) of the University of Maryland Baltimore on October 20, 2016. The transdisciplinary research team consists of epidemiologists, nutritionists, health literacy experts, psychologists, statisticians, and Extension educators.
Study Design
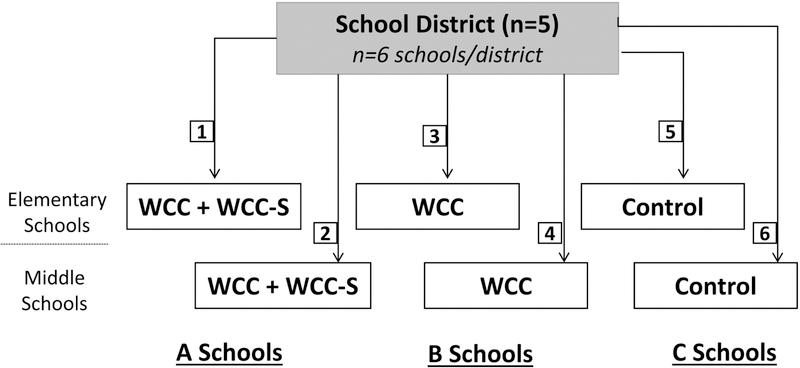
The WCC trial will take place in 15 elementary and 15 middle schools across five school districts in Maryland using a phased (i.e., 2–3 school districts per school year) timeline. Within each selected district, six schools (three elementary and three middle) will be recruited and randomized to receive both WCC and WCC-S (“A” schools), WCC only (“B” schools), or serve as a delayed contact control (“C” schools) (Figure 1). Within each selected school, teachers, students (3rd or 6th graders) and their caregivers, and Student Leaders (4th or 7th graders) will be recruited. The teachers will participate in the WCC curriculum, the students (Evaluation Cohort) and their caregivers will be evaluated over 2½ years (five data collection points) to assess Aims 1 and 2, and the Student Leaders will participate in the WCC-S curriculum and be evaluated over one year to assess Aim 3. The WCC and WCC-S curricula will be administered over one full school year by a trained health educator, referred to as a Wellness Specialist, followed by a second full school year with no intervention activities (to assess maintenance of effects). Throughout both the intervention and maintenance years, school-, student- and process-level data will be collected. Table 1 describes the study timeline.
Fig. 1.
Wellness Champions for Change planned randomization design.
Table 1:
Timeline of Wellness Champions for Change study within a school district
| School Year 0 | School Year 1: Intervention | School Year 2: Maintenance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Jan-Mar | Apr-Jun | Jul-Sept | Oct-Dec | Jan-Mar | Apr-Jun | Jul-Sept | Oct-Dec | Jan-Mar | Apr-Jun | July-Sept | |
| District and School Recruitment | X | ||||||||||
| Student Recruitment | X | ||||||||||
| Spring Baseline data collection (T0) | X | ||||||||||
| Randomization | X | ||||||||||
| WCC Training (A and B Schools) | X | ||||||||||
| Fall check-in data collection (T1) | X | ||||||||||
| WCC-S (A schools) or AHC (B, C schools) implementation | X | X | X | ||||||||
| WCC TA (A, B schools) implementation | X | X | X | ||||||||
| Process data collection | X | X | X | ||||||||
| Spring follow-up data collection (T2) | X | ||||||||||
| WCC-S Delayed (B, C schools) | X | ||||||||||
| Fall check-in data collection (T3) | X | ||||||||||
| Spring follow-up data collection (T4) | X | ||||||||||
| WCC Delayed (C schools) | X | ||||||||||
Recruitment and Randomization Procedures
Figure 2 describes the planned recruitment, enrollment, and randomization of districts, schools, and students in the study.
Fig. 2.
Study design and flow of participants through Wellness Champions for Change trial.
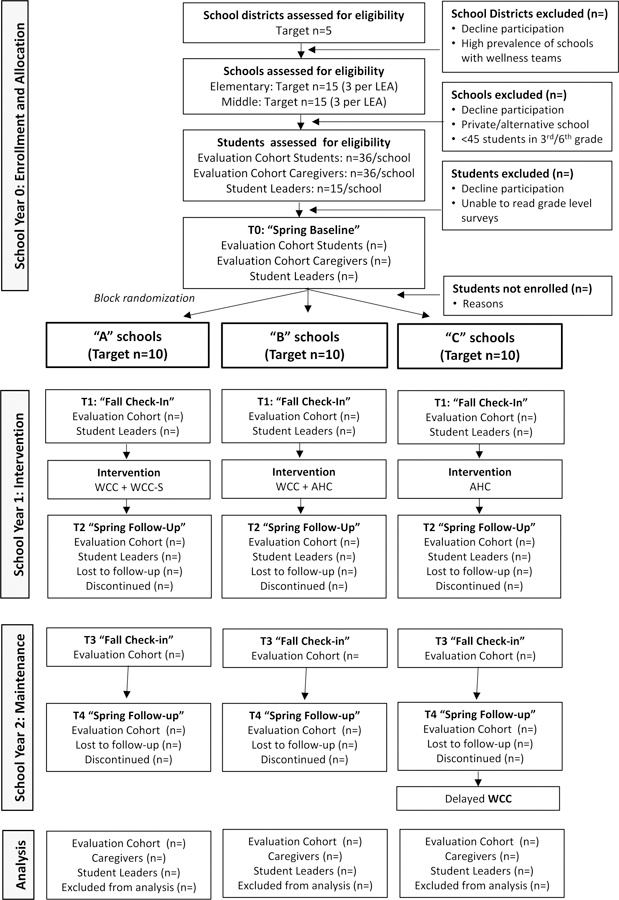
WCC=Wellness Champions for Change
WCC-S=Wellness Champions for Change-Student
AHC=Adolescent Health Curriculum
District recruitment.
In Maryland, each of the 24 counties represents a school district which are typically large and demographically diverse. Both urban and rural districts will be recruited. Eligible districts have a low prevalence of schools with existing wellness teams based on recent data gathered from an ongoing biennial survey[12]. District recruitment will be initiated by contacting partners on district-level school health councils and completing each district’s IRB applications.
School Recruitment.
Once the IRB application is approved, partners will help identify demographically similar “clusters” of 4 elementary and 4 middle schools (3 preferred, 1 alternate) for recruitment. Schools with higher Free-and-Reduced Price Meals (FARMS) rates will be given preference. To be eligible, schools must: (1) be standard elementary/middle schools (inclusive of grades K-5 or 6–8; not an alternative/special school) and (2) have a minimum of 45 students enrolled in 3rd or 6th grade. Study staff will contact selected schools and set up in-person meetings with school principals to introduce the study and obtain memoranda of understanding, which indicates that schools agree to participate, be randomized, and provide time and space for data collection. Principals will be asked to recommend a “Wellness Champion” prior to randomization. At all schools, the Wellness Champion will serve as the study liaison, and in A and B schools, the Wellness Champion will be the wellness team lead.
Student Recruitment.
In the spring prior to the intervention year, an “Evaluation Cohort” of students (3rd or 6th graders; target n=36) will be recruited in each school to assess study Aims 1 and 2. These grades were selected because students can be followed over two school years before advancing to middle or high school. Also in the spring prior to the intervention year, “Student Leaders” (4th or 7th graders, target n=15 per school) will be recruited. Student Leaders in “A” schools will receive WCC-S, and Student Leaders in B and C schools will receive a control curriculum (Adolescent Health Curriculum [AHC]). Student Leaders will be followed over one year to assess Aim 3. Student recruitment methods will be determined by school preference, but may include school announcements, posters and flyers, in-school distribution of informational pamphlets, attendance at PTA meetings, and presentations to students during class. Student Leaders can be nominated by teachers and/or asked to submit a brief paragraph on the importance of school wellness. Study staff will contact caregivers of Evaluation Cohort students to obtain consent, confirm eligibility, and enroll the caregivers to assess Aim 2 (home/neighborhood environment). Study staff will also contact caregivers of Student Leaders to confirm eligibility and obtain consent. Evaluation Cohort students and Student Leaders will sign assent forms.
Randomization.
Once the target number of Evaluation Cohort students (n=36/school) are recruited in each school, baseline data (T0) will be collected and randomization will be carried out at the school level (Table 1) using a random number generator. Schools will be block randomized (elementary and middle) within each school district to group A, B, or C (Figure 1). Data collectors will be unaware of school assignment for both student-level and school-level assessments across all data collection points.
Power Calculation and Sample Size
The trial will provide enough power (>0.8) to detect a small-medium effect (Cohen’s d≥0.3) for student-level outcomes for the primary outcome variable, BMI z-score, as well as physical activity. This is a plausible effect size based on the literature[24, 25]. For this outcome, 1080 Evaluation Cohort students and their caregivers (n=36/school) will be recruited, accounting for an estimated 20% attrition rate, and an average intraclass correlation coefficient (ICC) of 0.03, which are common in school-based studies. Data from previous school-based studies targeting a similar population (Black, under review) also estimates a correlation between repeated measures of 0.87 and 0.35 for BMI and physical activity, respectively. Based on G*Power, this is also a plausible sample size to detect a small to medium effect size (Cohen’s f≥0.18) with >80% power for effect modifications (Aim 2).
For Aim 3, 450 Student Leaders (15/school) will be recruited. Using the same attrition and ICC estimates described for the Evaluation Cohort and data from a study with similar outcome measures[27], the study will provide enough power (>0.8) to detect group differences in youth advocacy and public health literacy outcomes.
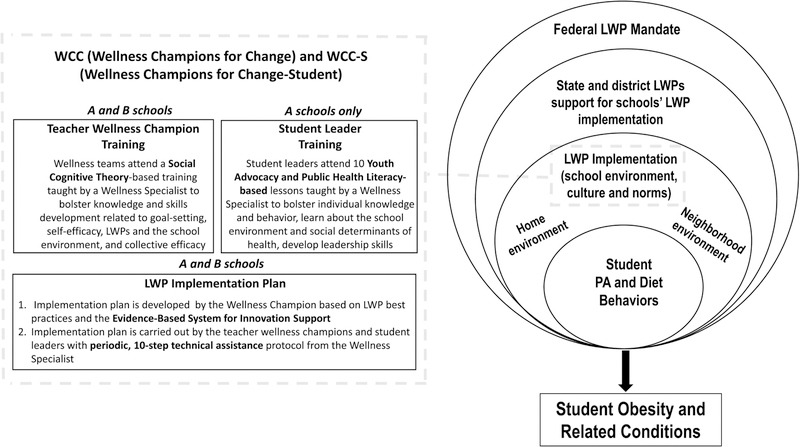
Theoretical Framework
This study was developed according to the SEM [2, 3] (Figure 3). The federal mandates for LWPs fall into the outermost system of influence on child PA and diet behaviors and obesity risk, followed by state-level support for LWPs, school districts’ written LWPs and support for LWP implementation, and school-level LWP implementation. This study tests two theory-based curricula (WCC and WCC-S) designed to enhance school-level LWP implementation and create a culture and environment that are conducive to positive health behaviors. The study also assesses the moderating role of factors across the SEM beyond the school culture and environment, including parent role modeling and health-related behaviors, home environment, and neighborhood environment.
Fig. 3.
Wellness Champions for Change (WCC) and Wellness Champions for Change-Student (WCC-S) theoretical framework and intervention description.
Both WCC and WCC-S curricula are grounded in behavioral and organizational theories, to ensure that they build skills among participants and can be feasibly implemented within schools. WCC is grounded in Social Cognitive Theory [13, 28, 29]. The content of the training and technical assistance (TA) emphasizes goal-setting, self-efficacy to build wellness teams, and collective efficacy to facilitate changes within their school that align with LWPs. The plan for the wellness teams to actually implement LWP-related changes is guided by the Evidence-Based System for Innovation Support (EBSIS). This system is designed to both build schools’ capacity and improve implementation of these changes through the provision of training, TA, tools, and quality improvement. EBSIS presents 10 general steps to follow to ensure accountability [30, 31].
WCC-S is grounded in a theoretical framework that combines health literacy, public health literacy and youth advocacy [21, 32]. Health literacy, or the ability to read, understand, and act on health information, is a dynamic construct that, while generally understudied among children and adolescents, is significantly associated with health knowledge, attitudes and behaviors; thus, introducing health literacy concepts and teaching related skills is important for preventing obesity-related behaviors [33, 34]. While health literacy is an important precursor to individualized behavior change, addressing obesity-related factors across social ecological levels requires an expanded definition. Public health literacy is defined as the ability to obtain, understand, and act on information to make public health decisions that benefit a larger school or community, and bolsters knowledge of social and ecological forces at play [31, 35]. Youth advocacy strategies can be used in tandem with health and public health literacy concepts to build skills related to persuading others and taking action to make policy and environmental change [21, 26]. Thus, WCC-S curricula was developed to first target Student Leaders’ own nutrition and PA knowledge and skills, then bolster their self-efficacy, advocacy, and communication skills while providing them with resources and guidance to be “agents of change” to take action toward a healthier school environment and work with the Wellness Champion and wellness team to make sustainable changes (Figure 2).
Intervention Development
Both WCC and WCC-S were developed through an iterative process and pilot tested prior to the initiation of the study. WCC was pilot tested in 63 schools in five school districts[13]. Following the pilot, modifications were made based on the study findings, in addition to necessary changes following LWP implementation mandates related to the 2016 Final Rule [7, 13]. Specifically, a more structured, yet tailorable strategy for implementing technical assistance for the Wellness Champions throughout the year was developed[13, 30]. A “TA protocol” was developed to ensure that the general TA strategy was consistent across schools (i.e., receiving support, tools/resources, and quality assurance), yet tailored to meet the needs, readiness and resources within individual schools [30, 31]. Using the EBSIS model, a menu of LWP best practices [10] (e.g., eliminating school food fundraising) options are presented for schools to choose to work toward, and 10 iterative, actionable steps are provided to ensure accountability, guide the technical assistance toward best practices, and plan for sustainability beyond the study period [7, 10, 30, 31].
To develop WCC-S, 8 focus groups (4–8 students per group) were conducted with 5th and 7th grade students, and in-depth interviews (n=2) were held with two school researchers who had developed similar programs. WCC-S was then pilot tested on two separate occasions with 27 students ranging from 5th to 10th grade to both ensure that lessons could be feasibly delivered during a short time frame, as well as optimize acceptability. Pilot testing led to re-structuring some lessons to emphasize key “take home messages” in the event of shortened delivery periods, and refining some activities and content to be more age appropriate. The final curriculum guide was designed to be delivered weekly for 30 weeks, and consisted of a teaching manual with learning objectives and lesson guides and a student workbook with activity sheets. The first 10 weeks include structured lesson plans and theory-based learning objectives to build foundational knowledge and skills. The next ~20 weeks follow a similar step-by-step strategy to help Student Leaders work with teacher wellness teams to accomplish their goals related to LWP implementation.[31]
Intervention Delivery
WCC and WCC-S will both be delivered by a Wellness Specialist. The Wellness Specialist is a health educator with specific expertise in behavioral theory, nutrition/physical activity, and knowledge of LWPs. WCC will begin with a 4-hour training prior to the start of the intervention school year. All teacher Wellness Champions from A and B schools within each district will attend the same training to facilitate discussion and exchange ideas. During the training, all Wellness Champions will set their first goal: to form a wellness team that meets at least four times a year [7, 10]. The Wellness Specialist will then meet with each individual Wellness Champion for tailored technical assistance at least two times per month throughout the school year to set goals and review progress. These TA sessions can take place via phone or in-person, with the recommendation being at least once a month in-person. The content and pacing of the TA will vary depending on the selected actions of the wellness team, but generally follows the ten implementation steps outlined in EBSIS [31]:
Conduct a needs assessment using an “LWP scorecard” to identify needs and resources [36]
Form wellness team and establish 2–3 goals/desired outcomes related to LWP implementation based on scorecard
Use “TA protocol” to review best practices for achieving goals
Ensure best practice aligns with school and team interests
Investigate and address any issues with alignment
Develop an implementation plan to meet goals and work toward best practices
Implement plan, and track implementation using robust process evaluation plan
Conduct outcome evaluation to assess whether goals are met and effective
Engage in constant monitoring/feedback to improve implementation
Develop sustainability plan for maintenance year, set new goals, maintain team
For WCC-S, Student Leaders will meet with the Wellness Specialist approximately once weekly throughout the school year. The first lesson will be co-delivered by the Wellness Specialist and Wellness Champion for an hour after school to establish rapport and build trust. Subsequent lessons will be administered by the Wellness Specialist during weekly lunch meetings. Following 10 structured lessons, students will use a similar implementation strategy to set goals and take action, with fewer and simpler steps, including:
Conduct a needs assessment using Photo Voice to identify needs and resources
Set 2–3 goals for social/environmental change related to LWP implementation based on Photo Voice
Ensure that goals are feasible and align with LWP best practices and goals of teacher wellness team
Work with teacher wellness team to help develop an implementation plan to meet goals
Implement plan and track implementation using a process evaluation plan
Work with teacher wellness team to help develop a sustainability plan for maintenance year
Control Intervention
Wellness Champions in C schools will receive the WCC training and access to the technical assistance toolkit after the final data collection time point (T4) at the end of Year 2. Student Leaders in B and C schools will receive a general Adolescent Health Curriculum (AHC) throughout the intervention school year. They meet with the Wellness Specialist monthly during lunch for interactive lessons on various health topics (e.g., hygiene, bullying, mental health).
Data Collection Procedures
To assess individual effectiveness, Evaluation Cohort students will be evaluated across five time points over 2.5 school years (T0 to T4). Student Leaders will be evaluated across the first three time points (T0 to T2) before advancing to middle or high school (See timeline, Table 1). All assessments will be conducted during or after school, depending on the school’s preference. The complete protocol, including anthropometrics, surveys completed electronically using Questionnaire Development Systems: QDS Version 4.0 (NOVA Research Company, Silver Spring, MD) on touch screen laptops, and semi-structured interviews, is estimated to take between 45 minutes and 1.5 hours to complete, and can be divided over two days. Evaluation Cohort caregivers complete assessments using Qualtrics (Qualtrics, Provo, UT ) via either a personalized email link or by paper survey at baseline only (T0). Caregiver surveys take approximately one hour to complete. The full battery of outcome and process measures for each participant group and the time points at which they are administered are presented in Tables 2 and 3.
Table 2:
Individual (Student-level) and Organizational (School-level) Effectiveness measures
| Data Collectiona | |||||
|---|---|---|---|---|---|
| T0 | T1 | T2 | T3 | T4 | |
| Evaluation Cohort (3rd or 6th graders; n per school=36) | |||||
| Anthropometric | |||||
| BMI z-scores (height and weight) | X | X | X | X | X |
| Waist Circumference | X | X | X | X | X |
| Body Composition (BIA) | X | X | X | X | X |
| Diet/PA Behaviors | |||||
| Patterns of Diet at School (PODS) survey [40] | X | X | X | X | X |
| Physical Activity checklist[38] (22 items) | X | X | X | X | X |
| Physical Activity Questionnaire for Older Children (PAQ-C)[39] (6 items) | |||||
| 7-day Accelerometry [37] | X | X | X | X | X |
| School and Home Environment | |||||
| Perceptions of Environment at School (PEA)[40](39 items) | X | X | X | ||
| Parent Support for Healthy Eating and PA[41] (32 items) | X | X | X | ||
| Ecological Momentary Assessment | X | ||||
| Health Literacy | |||||
| Newest Vital Sign[50](6 items) | X | X | X | ||
| Demographics | X | ||||
| Evaluation Cohort Caregivers (n per school=36) | |||||
| School, Home, and Neighborhood Environment | |||||
| Perceptions of Environment at School (PEA)[40] (39 items) | X | ||||
| Parent Support and Rules for Healthy Eating and PA [41] (32 items) | X | ||||
| Food Insecurity [54] (2 items) | X | ||||
| Food and Drink Availability [41](23 items) | X | ||||
| Physical Activity Barriers and Availability [41](23 items) | X | ||||
| Screen Time[41](10 items) | X | ||||
| Community/Neighborhood Access to Healthy Eating[47](13 items) | X | ||||
| Community/Neighborhood Access to Physical Activity[48](11 items) | X | ||||
| Demographics | X | ||||
| Student Leaders (4th or 5th graders; n per school=15) | |||||
| Health and Public Health Literacy | |||||
| Newest Vital Sign[50] (6 items) | X | X | |||
| Public Health Literacy Survey [35, 52] (5 items) | X | X | |||
| Focus groups | |||||
| Advocacy | |||||
| Youth Advocacy for Obesity Prevention Survey [27] (19 items) | X | X | |||
| Self-Efficacy for Healthy Eating and Physical Activity [53] (16 items) | X | ||||
| Semi-structured interview (3 items) | X | X | |||
| Focus groups | X | X | |||
| Anthropometric | |||||
| Height and Weight | X | X | X | ||
| Waist Circumference | X | X | X | ||
| Diet/PA Behaviors | |||||
| Patterns of Diet at School (PODS) survey [40] | X | X | X | ||
| Physical Activity checklist[38] (22 items) | X | X | X | ||
| The Physical Activity Questionnaire for Older Children (PAQ-C)[39] (6 items) | X | X | X | ||
| School Environment | |||||
| Perceptions of Environment at School (PEA)[40] (39 items) | X | X | |||
| Demographics | |||||
| Organizational Effectiveness | |||||
| Administrator Survey (Maryland Wellness Policies and Practices Project)[12] | X | ||||
| Observational School Environment Checklist | X | X | X | X | X |
| Exit interviews with WCC and WCC-S participants | |||||
T0 = Spring Baseline data collection; T1 = Fall check-in data collection; T2 = Spring follow-up data collection; T4 = Fall check-in data collection
Table 3:
RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance) measures
| Construct | Measures |
|---|---|
| Reach. Number, proportion, representativeness of participants in an intervention |
Reach and representativeness of participants • Demographics, school records (% FARMS, race/ethnicity, etc) to compare participating students to non-participators (Evaluation Cohort and Student Leaders) |
|
Reach of intervention components • Semi-structured interviews (Wellness Specialist, Teacher Wellness Champions) | |
| Effectiveness. Impact on primary study outcomes, quality of life, and unintended consequences |
Individual Effectiveness • Evaluation Cohort measures • Caregiver measures • Student Leader measures |
|
Organizational Effectiveness • School Observational Environmental Checklist • School Survey (MWPPP) | |
| Adoption. Number, proportion representativeness of settings and staff who implement intervention | • State records to describe participating districts compared to non-participators • District records to describe participating schools and compare to non-participators • Description of reasons for declining participation |
| Implementation. Degree to which intervention was delivered as intended; costs associated with continued delivery | • Independent observer fidelity checks using Wellness Specialist training manual • Wellness Specialist self-assessments and contact logs • Record attendance (sign-in sheet) and cost (total and per participant) • Semi-structured post-interviews (Wellness Specialist) and focus groups (SWC) |
| Maintenance. Long-term individual change in primary outcomes; extent to which intervention delivery/implementation is sustained over time |
Individual Maintenance • Long-term cost analysis (total, per participant) • Semi-structured post-interviews (Wellness Specialist, Teacher Wellness Champions) |
|
Organizational Maintenance • Proportion of schools who formally institutionalize SWCC (i.e., build in budget) • Observational School Environment Checklist • Describe dissemination via eXtension (or other forum) |
Measures
Individual Effectiveness Measures (Student-level)
Weight Status, Waist Circumference, and Body Composition.
Evaluation Cohort students and Student Leaders will have their weight status determined by measuring height (cm) and weight (kg) in triplicate using a portable stadiometer (Shorr Productions, Olney MD) and standard scale (300 GS, Tanita Corp, Tokyo Japan). BMI-for-age z-scores and percentiles will be calculated and weight status thresholds applied (CDC-2000). Waist circumference will be measured in duplicate at the umbilicus. Body composition (fat mass, fat free mass, percent body fat) will be assessed via Bioelectrical Impedance Analysis (BIA) in conjunction with body weight.
Evaluation Cohort caregiver weight status will be assessed by calculating BMI from self-reported height and weight.
Physical Activity.
Students in the Evaluation Cohort will wear an Actical accelerometer (Philips Respironics, Bend, OR) for up to 7 consecutive days to objectively measure physical activity. Researchers will place accelerometers on the students’ non-dominant ankle with a non-removable, reinforced hospital band worn next to the skin, under the sock (Hager, 2015). Accelerometers will be attached on the first day of data collection and removed one week later. Data will be time-stamped to differentiate between in-school and out-of-school time. Data will include average and total activity counts and minutes of sedentary, light, and moderate-to-vigorous intensity physical activity using validated thresholds [37].
Both Evaluation Cohort students and Student Leaders will complete validated survey measures including Physical Activity Questionnaire for Older Children (PAQ-C) and a Physical Activity Checklist, which asks students how often (5-option Likert-type responses ranging from “never” to “a lot”) they perform 22 different activities (i.e., basketball, dance, homework)[38, 39].
Diet.
Evaluation Cohort students and Student Leaders will both complete PODS (Patterns of Diet at School), a survey developed to assess in-school eating patterns. PODS evaluates “usual” diet patterns during the school week by inquiring about the frequency (5-option Likert response set “never” to “always”) they usually eat lunch from various locations (home, school cafeteria, restaurant, before-school program), and what types of foods they usually consume within MyPlate categories (i.e., Fruits, Vegetables, Protein, Grains, Dairy, Beverages). PODS had acceptable test-retest reliability and validity compared to a five-day food record among 58 students in grades 3, 6, and 9[40].
Health-Promoting Environment at School.
Perceptions of how school policies, practices, and environments are conducive to healthy eating and PA will be assessed in all three groups (Evaluation Cohort, Student Leaders, caregivers) using the Perceptions of Environment at School (PEAS) survey, developed and assessed for reliability for this study[39]. PEAS consists of 40 items (5-item Likert-type responses ranging from “never” to “always”) in 4 subscales: (1) perceptions of school PA and nutrition policies/practices; (2) perceptions of teacher and classroom policies/practices; (3) perceptions of cafeteria policies/practices; and (4) perceptions of recess policies/practices (Cronbach’s α≥0.78). Example items include “I can easily get water at my school when I am thirsty” and “Teachers at my school tell us it is important to move and be active.” Caregiver surveys use the same response sets with slightly re-worded questions (e.g., “My child can easily get water at school when he or she is thirsty”).
Health-Promoting Environment at Home and Neighborhood.
Information about Evaluation Cohort students’ home environment will be assessed in several ways. Students will complete an adapted version of the Comprehensive Home Environment Survey (CHES), which consists of 32 items with 5-item Likert response sets in 4 subscales: (1) perceptions of parental support for PA (2) perceptions of parental support for healthy eating; (3) perceptions of parent rules for healthy eating; and (4) perceptions of parent healthy role modeling[41].
Evaluation Cohort students will participate in Ecological Momentary Assessment (EMA), a reporting method that captures real-time information on contextual factors in the home environment that may influence diet/PA behaviors[42–44]. Students will be loaned an inexpensive Android smart phone loaded with the MovisensXS App Version 1.1. (Karlsruhe, Germany). During the same period (~7 days) of accelerometry wear, the phone will beep randomly during out of school, non-sleep periods up to 29 times (7 times between 9 AM and 8 PM on weekend days, 3 times between 3 PM and 8 PM per afternoon/evening on school days), which is an acceptable number for children [43, 44]. Upon hearing the beep, students will be instructed to complete a brief (~2–3 minutes) survey on the app. Students can delay the beep up to nine minutes, and will be re-prompted one time per beep. The questions will ask for categorical responses about their current diet or PA behaviors and current context[43, 44]. Targeted constructs include: Consumption/Activity (what are you eating/doing), Context (where are you, who are you with, what is happening around you), Access (i.e., is there food/PA options where you are right now), Accessibility (i.e., if you wanted to eat food/get PA, could you), and Autonomy (i.e., did you choose to eat/do this?).
Caregivers will also provide information on the home environment using scales adapted from the CHES[41], including the 32-item Parent Support and Rules for Healthy Eating/PA scale administered to the Evaluation Cohort students, a 23-item home Food and Drink Availability inventory, a 23-item Physical Activity Barriers and Availability inventory, and a 10-item screen time survey. The inventories will ask caregivers to report the frequency (5-item response set from “Never” to “Always”) that various foods and beverages (i.e., whole fruit, dark-green vegetables, candy/chocolate, regular soda) and types of space and PA equipment (i.e., yard, running shoes) are available and accessible to their child. The screen time items were adapted to account for new delivery modes for television and media (i.e., smartphones, tablets, computers), and ask caregivers to report the number of screens the child accesses and the frequency of time spent in front of a screen per day or week.
Caregivers will also complete a survey to assess health-promoting neighborhood environments, which consists of 24-items adapted from several existing surveys. Thirteen items ask about the availability and accessibility of healthy, good quality food options (i.e., grocery store) and 11-items inquire about physical activity (i.e., safely walkable sidewalks) [45–48].
To assess the environment around the homes, home addresses will be geo-coded in ArcGIS, and publicly available neighborhood data (e.g., corner/convenience stores, fast food restaurants, parks, recreation centers) will be spatially linked to examine the neighborhood environments [49].
Health Literacy.
The Newest Vital Sign (NVS), a commonly used tool to assess health literacy (i.e., reading, numeracy, prose), will be administered among Evaluation Cohort students and Student Leaders. The NVS consists of six questions related to a nutrition label and takes about three minutes to complete [50, 51]. Students will be given a paper copy of the nutrition label from the back of an ice cream container, then asked to answer questions about the label on the electronic survey. They can use a pen or pencil to make calculations on the paper copy, but cannot use a calculator.
Student Leaders will also complete a 5-item survey to assess public health literacy. The survey has been used in two previous studies, and was adapted to be obesity-specific and school-centered[35, 52]. The survey assesses knowledge of and desire to change social determinants of obesity (i.e., Obesity affects my community unfairly) using a 5-item Likert response set (“Never” to “Always”).
Youth Advocacy for Obesity Prevention.
Youth advocacy will be assessed among Student Leaders through a convergent mixed methods approach, with simultaneous collection of qualitative/quantitative data sources at all time points. A 19-item survey adapted from the Youth Advocacy for Obesity Prevention Survey will be administered, as well as a 16-item Self-Efficacy for Healthy Eating and Physical Activity survey (5-item Likert response sets “Strongly Agree” to “Strongly Disagree”)[27, 53]. Example questions include: “I can talk with others about howto make our school healthier” and “I am sure I can tell my friends to eat healthy.” Half of the Student Leaders will be randomly selected to also participate in brief (<10 minute) semi-structured interviews that inquire about their general health literacy and skills for advocacy. Prior to their first meeting and following their last meeting with the Wellness Specialist, all Student Leaders will participate in brief focus groups to further explore public health literacy and advocacy constructs (e.g., “Tell me some ways your school makes it easier/harder for kids to be healthy”).
Demographics.
All students will report their age, gender, race/ethnicity, primary caretaker, and the mode of transportation they generally use to get to and from school. Caregiver demographic data will include gender, race/ethnicity, marital status, highest level of education, employment status, income status, and food insecurity[54].
Organizational Effectiveness Measures(School level)
The effectiveness of WCC and WCC-S at improving LWP implementation and changing the school’s health-promoting environment will be assessed using data collected from an administrator survey, an observational environmental audit, and exit interviews with WCC and WCC-S participants.
The administrator survey, the 17-item Maryland Wellness Policies and Practices Project Survey (MWPPP), is part of a statewide project that examines strength and comprehensiveness of LWPs, and tracks school-level implementation longitudinally. School administrators will complete the MWPPP survey at T0, T2, and T4 to track school-level changes[12].
Observational audits will be conducted at all five time points. A comprehensive audit tool, the Observational School Environment Checklist (OSEC), was developed using several existing instruments to assess the physical and structural environment of schools [55–57]. The tool assesses the physical environment in four main locations (cafeteria, lobby/hallway, gym, outdoor areas). It was refined through pilot testing in two schools and input from school wellness experts. Auditors will be trained and practice achieving agreement prior to data collection. Two auditors will conduct the audit in each school and take photographs, which takes about two hours. Inter-rater reliability will be calculated, and raters will meet to arrive at consensus.
Student and caregiver responses to the PEAS (Perceptions of the Environment at School) survey and exit interviews with WCC and WCC-S participants will also be used to inform organizational effectiveness.
Reach, Adoption, Implementation, Maintenance
To assess additional RE-AIM indicators, all study phases will be documented, including what is done, who does it, how long it takes, and what resources are required [15, 16]. School level data will be collected, as well as quantitative and qualitative data from teacher and student intervention participants, as described below.
Adoption.
The study team will monitor the school districts invited to participate, and track schools that accept or decline the invitation. District and school-level data will include demographics and LWP implementation data from MWPPP surveys, in order to describe the proportion and representativeness of participating districts related to non-participants as well as the state as a whole, and participating schools compared to all schools in the district.
Reach.
Participation rates and representativeness of student participants will be assessed using school-level demographic information (e.g., race/ethnicity, free and reduced meal participation) and comparing participating students in the Evaluation Cohort and Student Leader groups with the student body as a whole. Semi-structured exit interviews with teachers on the wellness team and focus groups with Student Leaders, as well as additional survey questions at the last time point (T4) for the Evaluation Cohort, will inform the perceived reach of LWP changes to the rest of the school.
Implementation.
While WCC and WCC-S will vary in implementation process depending on school-specific needs and resources, both have structured implementation guides and learning objectives; thus, fidelity checklists will be completed to ensure that they are delivered as intended. These checklists were adapted from existing instruments (i.e., adherence, duration/exposure, quality of delivery, program specificity)[58–60]. Trained observers will complete fidelity checklists at the WCC training and 40% of WCC-S lessons. Implementation fidelity will be further assessed through self-assessment completed by the Wellness Specialist after each WCC-S meeting and tracking sheets compiled throughout technical assistance. Attendance will be recorded at each WCC-S meeting. Costs related to implementation (i.e., supplies, prizes, time) will also be tracked. Exit interviews with teachers and focus groups with Student Leaders will inform satisfaction and provide feedback on implementation.
Maintenance.
Maintenance will be assessed at both the individual and organizational level. Participants’ improvements in anthropometric and behavioral outcomes following the maintenance year will inform individual maintenance. For organizational maintenance, WCC and WCC-S participants will be asked about the potential sustainability of WCC and WCC-S during exit interviews, and will describe potential barriers and challenges. Wellness Specialists will work with schools to facilitate use of the online eXtension forum as a method to disseminate WCC as a continuing education opportunity for teachers, and to create a toolkit to disseminate WCC-S for Student Leaders. The proportion of schools that formally institutionalize WCC or WCC-S by allocating or securing funding for these or other dissemination methods will be tracked.
Planned Analytical Approach
For all aims, socio-demographic information will be compared by loss-to-follow up. Data will be checked for normality and missingness. Intent-to-treat analyses with missing data imputed will be used to evaluate intervention effects[61].
For Aim 1 on student-level outcomes, three-level linear mixed modeling (LMM) for continuous variables and Generalized Linear Mixed Modeling (GLMM) for categorical variables (e.g. overweight or obesity) with random effects will be performed to account for clustering of repeated measures (level-1) within each student (level-2) and clustering of students within each school (level-3)[59]. For school-level outcomes, two-level LMM for continuous variables and GLMM for categorical variables will be conducted, accounting for clustering of repeated measures (level 1) within each school (level 2) and including district as a covariate. Interactions between time and intervention status will be included in the mixed model to assess the intervention effect. District and student-level demographic variables that differ between groups or by loss to follow-up will be included as covariates.
For Aim 2, the differential impact of the interventions by home and school-neighborhood factors, which are hypothesized to follow the Yerkes-Dodson inverted-U pattern, will be assessed by first categorizing environment variables into low, medium, and high scores based on tertiles, then comparing intervention effects among students with medium and high scores to those with low scores[22, 23]. For the LMM or GLMM models, two three-way interactions will be included among environment score, intervention group, time, and all lower-order two-way interactions. If regression coefficients are significant, indicating that the environment moderates the intervention effect, stratified analyses will assess intervention effect at each environment score.
For Aim 3, quantitative data will be analyzed using LMM or GLMM, as described for Aim 1. Qualitative data from brief, semi-structured interviews and focus groups will be transcribed verbatim. Interviews and focus groups will be deductively coded based on the theoretical framework using a rapid evaluation and assessment method [62, 63], which is appropriate for quick analysis of data to inform future research and/or to analyze in concordance with quantitative data. In this method, coders will create brief transcription summaries based on a priori domains in order to complete a Respondent*Domain matrix such that all interviews can be analyzed simultaneously along each domain. Summaries and matrices will be entered into MAXQDA (VERBI Software, 2016, Germany), then two coders will separately code the matrices each domain using the constant comparative method, which involves independent identification of emerging themes, then meeting to reach consensus, sort data, and compile a thematic codebook[64, 65]. Validity and trustworthiness will be maintained through double checking 50% of transcript summaries, meeting weekly as a team, and double coding matrices[66].
Study Timeline and Study Status
A sample study timeline is presented for a single school district. School district recruitment was initiated in Fall 2016 for the first school district in Cohort 1, student recruitment was initiated in Spring 2017, and intervention delivery began in Fall 2017. Final follow-up measurements are estimated to be completed in Spring 2021.
DISCUSSION
This paper provides an overview of the Wellness Champions for Change study, including theoretical framework, aims, target population, recruitment strategies, study design, intervention development and delivery, and planned evaluation timeline. Wellness Champions for Change is a cluster randomized controlled trial that aims to improve LWP implementation in order to enhance health-promoting school environments and improve student-level outcomes across a mid-Atlantic state. While other studies have addressed LWP implementation [9, 12, 14], this study is unique in linking LWP implementation to student-level BMI percentile and z-scores, physical activity, and diet patterns.
The study has significant strengths. First, the WCC and WCC-S interventions are theory-based, systematically developed, and pilot tested. Both curricula engage school stakeholders (i.e., teachers, staff, and students), and thus have greater potential to be acceptable and sustainable [9, 15, 19]. The formal incorporation of the important concepts of health literacy, public health literacy and youth advocacy is an additional strength of WCC-S, as this is not often found in the literature. The study includes an extensive battery of both quantitative and qualitative measures administered by data collectors who are unaware of the intervention status of students, caregivers, and schools, which enables broad analysis of the social ecological factors that influence student outcomes. This battery includes multiple measures for many variables (i.e., self-report and accelerometry for PA), employs mixed methods measures to investigate complex processes and outcomes, and uses EMA, a novel method to collect data in real time. The collection of reach, adoption, implementation, and organizational maintenance data informs both the implementation process for the intervention as well as the capacity for broader dissemination and sustainability. Finally, the involvement of state-level partners including Extension and the Departments of Education and Health increases the likelihood that this intervention, if effective, can be scaled up and broadly implemented to enhance LWP implementation and reduce pediatric obesity prevalence.
Limitations
This study has several limitations to consider. First, WCC will not directly address key social ecological factors both inside (e.g., teacher behaviors and modeling in the classroom) and outside the school environment (e.g., parent behaviors and modeling at home and home and neighborhood environments), that influence obesogenic behaviors and weight outcomes[2, 3, 67]. The study will, however, include myriad subjective and objective measures to describe these factors, and evaluate their moderating effective on the school-level intervention. These data can inform future research studies to address these factors. Second, while recruitment strategies will aim to recruit a sample that is geographically diverse, this study takes place in a single state, which may limit generalizability.
Conclusion
This study is timely, given the recent LWP implementation final rule stemming from the HHFKA[7, 8]. A growing body of evidence supports the role of wellness teams, led by wellness champions, in enhancing school-level LWP implementation, yet few studies have examined the role of students in leading/participating in wellness teams. Little is known about student-level outcomes associated with school-level LWP implementation. This study will provide clear evidence for the impact of LWP implementation on student health.
ACKNOWLEDGEMENTS
We would like to acknowledgement additional members of the Wellness Champions for Change team, including partners at the Maryland Department of Education (Stew Eidel and Megan Lopes, Lea Jaspers) and Department of Health (Erin Penniston and Caroline Green), Maryland Extension (Patsy Ezell) staff and research assistants (Amy Zemanick, Katherine Campbell, Katherine Ordonio, Salma Sharaf, Fatmata Timbo) and Wellness Specialists (Perri Carroll). We would also like to acknowledge the many members of the Maryland School Wellness Partnership for their contribution and input. Finally, we would like to thank the school district, schools, teachers and students across the state who generously help with recruitment and/or serve as participants in this study
FUNDING
This study is funded primarily by a United States Department of Agriculture AFRI Childhood Obesity grant (ID: 2016-68001-24927), with additional funding from a National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health post-doctoral training grant (ID: F32DK115146), and Seed grant research funding from the Program in Health Disparities and Population Health, University of Maryland School of Medicine Department of Epidemiology and Public Health and from the Mid-Atlantic Nutrition Obesity Research Center (NIH NIDDK ID: 30DK072488).
LIST OF ABBREVIATIONS
- PA
Physical Activity
- LWP
Local Wellness Policy
- WCC
Wellness Champions for Change
- WCC-S
Wellness Champions for Change-Student
- RE-AIM
Reach, Effectiveness, Adoption, Implementation, Maintenance
- IRB
Institutional Review Board
- FARMS
Free-and-Reduced Price Meals
- AHC
Adolescent Health Curriculum
- ICC
Intra-class Correlation Coefficient
- SEM
Social Ecological M odel
- TA
Technical Assistance
- EBSIS
Evidence-Based System for Innovation Support
- PODS
Patterns of Diet in School survey
- PEAS
Perceptions of the Environment at School survey
- CHES
Comprehensive Home Environment Survey
- EMA
Ecological M omentary Assessment
- NVS
Newest Vital Sign
- MWPPP
Maryland Wellness Policies and Practices Project survey
- OSEC
Observational School Environment Checklist
- LMM
Linear Mixed M odeling
- GLMM
General Linear Mixed M odeling
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Hannah G. Lane, University of Maryland School of Medicine, Department of Pediatrics, Growth and Nutrition Division, 737 West Lombard Street, Baltimore, MD, USA 21201, hlane@som.umaryland.edu.
Rachel Deitch, University of Maryland School of Medicine, Department of Pediatrics, Growth and Nutrition Division, 737 West Lombard Street, Baltimore, MD, USA 21201, rdeitch@som.umaryland.edu.
Yan Wang, University of Maryland School of Medicine, Department of Pediatrics, Growth and Nutrition Division, Department of Epidemiology and Public Health, 737 West Lombard Street, Baltimore, MD, USA 21201, yan.wang@som.umaryland.edu.
Maureen M. Black, University of Maryland School of Medicine, Department of Pediatrics, Growth and Nutrition Division, Department of Epidemiology and Public Health, 737 West Lombard Street, Baltimore, MD 21201, RTI International, Research Triangle Park, NC, USA 27709, mblack@som.umaryland.edu.
Genevieve F. Dunton, Departments of Preventive Medicine and Psychology, University of Southern California, 2001 N. Soto St., Los Angeles, CA, USA 90032, 323-442-8224, dunton@usc.edu.
Linda Aldoory, Department of Communication, College of Arts and Humanities, University of Maryland College Park, College Park, MD, USA 20742, laldoory@umd.edu.
Lindsey Turner, Boise State University, College of Education, 1910 University Drive, #1740, Boise, ID, USA 83725, lindseyturner1@boisestate.edu.
Elizabeth A. Parker, University of Maryland School of Medicine, Department of Family and Community Medicine, Center for Integrative Medicine, 520 W. Lombard Street, East Hall, Baltimore, MD, USA 21201 Elizabeth.parker@som.umaryland.edu.
Shauna C. Henley, University of Maryland Extension, Department of Agriculture and Natural Resources, 1114 Shawan Road, Cockeysville, MD, USA 21030, shenley@umd.edu.
Brit Saksvig, Department of Epidemiology and Biostatistics, School of Public Health, University of Maryland College Park, College Park, MD, USA 20742, bsaksvig@umd.edu.
Hee-Jung Song, Department of Nutrition and Food Science, College of Agriculture and Natural Resources, University of Maryland College Park, College Park, MD, USA 20742, hjsong@umd.edu.
Erin R. Hager, University of Maryland School of Medicine, Department of Pediatrics, Growth and Nutrition Division Department of Epidemiology and Public Health, 737 West Lombard Street, Baltimore, MD, USA 21201, ehager@som.umaryland.edu.
REFERENCES
- 1.Skinner AC, Perrin EM, Skelton JA. Prevalence of obesity and severe obesity in US children, 1999–2014. Obesity 2016;24(5):1116–1123. [DOI] [PubMed] [Google Scholar]
- 2.Brofenbrenner U Ecological Models of Human Development 2nd ed. Oxford: Elsevier; 1994. [Google Scholar]
- 3.Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. British Medical Journal 1997;315(7106):477–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. The Cochrane Database of Systematic Reviews 2005(3):Cd001871. [DOI] [PubMed] [Google Scholar]
- 5.Wechsler H, Devereaux RS, Davis M, Collins J. Using the school environment to promote physical activity and healthy eating. Preventive Medicine 2000;31(2):S121–S137. [Google Scholar]
- 6.Child Nutrition and Women, Infants, and Children Reauthorization Act of 2004 Public Law No. 108–265, 118 Sta 729 (June 2004). Available at: https://www.gpo.gov/fdsys/pkg/PLAW-108publ265/pdf/PLAW-108publ265.pdf. [Accessed 9/30/16].
- 7.United States Department of Agriculture. Local School Wellness Policy Implementation Under the Healthy, Hunger-Free Kids Act of 2010: Summary of the Final Rule (July 2016). Available at: http://www.fns.usda.gov/sites/default/files/tn/LWPsummary_finalrule.pdf [Accessed 8/16/16]. [PubMed]
- 8.Healthy Hunger-Free Kids Act of 2010 Pub L No 111–296, 124 Stat 3183. 3183. https://www.gpo.gov/fdsys/pkg/PLAW-111publ296/pdf/PLAW-111publ296.pdf [Accessed 8/16/16].
- 9.Profili E, Rubio DS, Lane HG, Jaspers LH, Lopes MS, Black MM, Hager ER. School wellness team best practices to promote wellness policy implementation. Prev Med 2017;101:34–37. [DOI] [PubMed] [Google Scholar]
- 10.Alliance for a Healthier Generation (2016). Healthy Schools Program framework of best practices Available at: https://www.healthiergeneration.org/_asset/l062yk/07-278_HSPFramework.pdf [Accessed 9/30/16].
- 11.United States Department of Agriculture. Local School Wellness Policy Outreach Toolkit (November 2016). Available at: https://www.fns.usda.gov/tn/local-school-wellness-policy-outreach-toolkit [Accessed 6/26/18]
- 12.Hager ER, Rubio DS, Eidel GS, Penniston ES, Lopes M, Saksvig BI, et al. Implementation of local wellness policies in schools: role of school systems, school health councils, and health disparities. Journal of School Health 2016;86(10):742–750. [DOI] [PubMed] [Google Scholar]
- 13.Hager E, Song HJ, Lane HG, Guo H, Jaspers L, Lopes MA. Pilot-testing an intervention to enhance wellness policy implementation in schools: Wellness Champions for Change. Journal of Nutrition Education and Behavior 2018;50(8):765–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McIlree C, Lane HG, Wang Y, Greene C, Hager ER. Wellness team stability and Local Wellness Policy implementation: A longitudinal study. Annals of Behavioral Medicine 2018;52(Suppl 1):S95. [Google Scholar]
- 15.Jones S, Spence M, Hardin S, Clemente N, Schoch A. Youth Can! results of a pilot trial to improve the school food environment. Journal of Nutrition Education and Behavior 2011;43(4):284–287. [DOI] [PubMed] [Google Scholar]
- 16.Mitra DL. Adults advising youth: Leading while getting out of the way. Educational Administration Quarterly 2005;41(3):520–553. [Google Scholar]
- 17.Jomaa LH, McDonnell E, Weirich E, Hartman T, Jensen L, Probart C. Student involvement in wellness policies: a study of Pennsylvania local education agencies. Journal of Nutrition Education and Behavior 2010;42(6):372–379. [DOI] [PubMed] [Google Scholar]
- 18.Hoelscher DM, Moag-Stahlberg A, Ellis K, Vandewater EA, Malkani R. Evaluation of a student participatory, low-intensity program to improve school wellness environment and students’ eating and activity behaviors. The International Journal of Behavioral Nutrition and Physical Activity 2016;13:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Millstein RA, Sallis JF. Youth advocacy for obesity prevention: the next wave of social change for health. Translational Behavioral Medicine 2011;1(3):497–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnston CA, Moreno JP, Regas K, Tyler C, Foreyt JP. The application of the Yerkes-Dodson law in a childhood weight management program: Examining weight dissatisfaction. J Pediatr Psychol 2012;37(6):674–9. [DOI] [PubMed] [Google Scholar]
- 21.Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-formation. J Comp Neurol Psychol 1908;18:459–82. [Google Scholar]
- 22.Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Annals of Behavioral Medicine 2004;27(1):3–12. [DOI] [PubMed] [Google Scholar]
- 23.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. American Journal of Public Health 1999;89(9):1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coleman KJ, Shordon M, Caparosa SL, Pomichowski ME, Dzewaltowski DA. The healthy options for nutrition environments in schools (Healthy ONES) group randomized trial: using implementation models to change nutrition policy and environments in low income schools. International Journal of Behavioral Nutrition and Physical Activity 2012;9(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foster GD, Sherman S, Borradaile KE, Grundy KM, Vander Veur SS, Nachmani J, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics 2008. 121(4):e794–e802. [DOI] [PubMed] [Google Scholar]
- 26.Black MM, Hager ER, Le K, et al. Challenge! Health promotion/obesity prevention mentorship model among urban, black adolescents. Pediatrics 2010;August;126(2):280–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Millstein RA, Woodruff SI, Linton LS, Edwards CC, Sallis JF. Development of measures to evaluate youth advocacy for obesity prevention. International Journal of Behavioral Nutrition and Physical Activity 2016;13(1):84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bandura A Social foundations of thought and action: a social cognitive theory Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 29.Bandura A Health promotion by social cognitive means. Health Education & Behavior 2004; 31(2):143–164. [DOI] [PubMed] [Google Scholar]
- 30.Wandersman A, Chien VH, Katz J. Toward an Evidence‐Based System for Innovation Support for implementing innovations with quality: tools, training, technical assistance, and quality assurance/quality improvement. American Journal of Community Psychology 2012;50(3–4):445–459. [DOI] [PubMed] [Google Scholar]
- 31.Wandersman A, Imm P, Chinman M, Kaftarian S. Getting to outcomes: A results-based approach to accountability. Evaluation and Program Planning 2000;23(3):389–395. [Google Scholar]
- 32.Freedman DA, Bess KD, Tucker HA, Boyd DL, Tuchman AM, Wallston KA. Public health literacy defined. American Journal of Preventive Medicine 2009;36(5):446–451. [DOI] [PubMed] [Google Scholar]
- 33.Sanders LM, Shaw JS, Guez G, Baur C, Rudd R. Health literacy and child health promotion: implications for research, clinical care, and public policy. Pediatrics 2009;124 Suppl 3:S306–314. [DOI] [PubMed] [Google Scholar]
- 34.Manganello JA. Health literacy and adolescents: a framework and agenda for future research. Health Education Research 2008;23(5):840–847. [DOI] [PubMed] [Google Scholar]
- 35.Lane H, Porter KJ, Hecht E, Harris P, Kraak V, Zoellner J. Kids SIPsmartER: A feasibility study to reduce sugar-sweetened beverage consumption among middle school youth in Central Appalachia. American Journal of Health Promotion 2017; doi: 0890117117715052. [DOI] [PMC free article] [PubMed]
- 36.Maryland State Department of Education Office of School and Community Nutrition Programs. “School Wellness Policy” 2018. Accessed June 26, 2081 from: http://www.marylandpublicschools.org/programs/Pages/SchoolWellnessPolicy/index.aspx.
- 37.Hager ER, Treuth MS, Gormely C, Epps L, Snitker S, Black MM. Ankle accelerometry for assessing physical activity among adolescent girls: Threshold determination, validity, reliability, and feasibility. Research Quarterly for Exercise and Sport 2015;86(4):397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Treuth MS, Sherwood NE, Baranowski T, Butte NF, Jacobs DR Jr, McClanahan B, et al. Physical activity self-report and accelerometry measures from the Girls health Enrichment Multi-site Studies. Preventive Medicine 2004;38:43–49. [DOI] [PubMed] [Google Scholar]
- 39.C Kowalski K, Crocker P, M Donen R, Honours B. The Physical Activity Questionnaire for Older Children (PAQ-C) and Adolescents (PAQ-A) Manual; 2004.
- 40.Lane HG, Driessen R, Campbell K, Deitch R, Turner L, Parker E, Hager ER. Development and of the PEA-PODS (Perceptions of the Environment and Patterns of Diet at School) survey for students. Preventing Chronic Disease 2018;15:E88: 10.5888/pcd15.170561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pinard CA, Yaroch AL, Hart MH, Serrano EL, McFerren MM, Estabrooks PA. The validity and reliability of the Comprehensive Home Environment Survey (CHES). Health Promotion Practice 2014; 15(1):109–117. [DOI] [PubMed] [Google Scholar]
- 42.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology 2008;4:1–32. [DOI] [PubMed] [Google Scholar]
- 43.Dunton GF, Liao Y, Intille SS, Spruijt‐Metz D, Pentz M. Investigating children’s physical activity and sedentary behavior using ecological momentary assessment with mobile phones. Obesity 2011; 19(6):1205–1212. [DOI] [PubMed] [Google Scholar]
- 44.Dunton GF, Liao Y, Intille S, Wolch J, Pentz MA. Physical and social contextual influences on children’s leisure-time physical activity: an ecological momentary assessment study. Journal of Physical Activity and Health 2011;8(s1):S103–S108. [DOI] [PubMed] [Google Scholar]
- 45.Ma X, Barnes TL, Freedman DA, Bell BA, Colabianchi N, Liese AD. Test-retest reliability of a questionnaire measuring perceptions of neighborhood food environment. Health & Place 2013;21:65–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. American Journal of Epidemiology 2007; 165(8):858–867. [DOI] [PubMed] [Google Scholar]
- 47.Green SH, Glanz K. Development of the Perceived Nutrition Environment Measures Survey. American Journal of Preventive Medicine 2015;49(1):50–61. [DOI] [PubMed] [Google Scholar]
- 48.Hager ER, Cockerham A, O’Reilly N, Harrington D, Harding J, Hurley KM, Black MM. Food swamps and food deserts in Baltimore City, MD, USA: associations with dietary behaviours among urban adolescent girls. Public Health Nutrition 2017;20(14):2598–2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: The Newest Vital Sign. Annals of Family Medicine 2005; 3(6):514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Warsh J, Chari R, Badaczewski A, Hossain J, Sharif I. Can the Newest Vital Sign be used to assess health literacy in children and adolescents? Clinical Pediatrics 2014;53(2):141–144. [DOI] [PubMed] [Google Scholar]
- 51.Rogers EA, Fine S, Handley MA, Davis H, Kass J, Schillinger D. Development and early implementation of The Bigger Picture, a youth-targeted public health literacy campaign to prevent type 2 diabetes. Journal of Health Communication 2014;19(sup2):144–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Steele MM, Burns LG, Whitaker BN. Reliability and validity of the SE-HEPA: Examining physical activity–and healthy eating–specific self-efficacy among a sample of preadolescents. Health Education & Behavior 2013;40(3):355–361. [DOI] [PubMed] [Google Scholar]
- 53.Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010;126(1):e26–32. [DOI] [PubMed] [Google Scholar]
- 54.Jones NR, Jones A, van Sluijs EM, Panter J, Harrison F, Griffin SJ. School environments and physical activity: the development and testing of an audit tool. Health & Place 2010;16(5):776–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kenney EL, Gortmaker SL, Cohen JF, Rimm EB, Cradock AL. Limited school drinking water access for youth. Journal of Adolescent Health 2016;59(1):24–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thomas LN, Hill TF, Gaines A, Dollahite JS. Implementing Smarter Lunchrooms makeovers in New York state middle schools: an initial process evaluation. Archives of Public Health 2016;74(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mellard D Fidelity of implementation within a response to intervention (RtI) framework: Tools for schools (2010). Available at: http://ped.state.nm.us/ped/RtIdocs/Fidelity%20of%20Implementation%20guidev5.pdf. [Accessed: 7/08/17]
- 58.Intervention Fidelity checklist (nd) Available at: https://rtips.cancer.gov/rtips/viewProduct.do?viewMode=product&productId=27133361 [Accessed 7/08/17]
- 59.Breitenstein SM, Fogg L, Garvey C, Hill C, Resnick B, Gross D. Measuring implementation fidelity in a community-based parenting intervention. Nursing Research 2010;59(3):158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rubin DB, Little RJA. Statistical analysis with missing data New York: Wiley; 2002. [Google Scholar]
- 61.McNall M, Foster-Fishman PG. Methods of Rapid Evaluation, Assessment, and Appraisal. American Journal of Evaluation 2007;28(2):151–168. [Google Scholar]
- 62.Watkins DC. Rapid and Rigorous Qualitative Data Analysis: The “RADaR” Technique for applied research. International Journal of Qualitative Methods 2017;16(1):1609406917712131. [Google Scholar]
- 63.Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qualitative Health Research 2002;12(6):855–866. [DOI] [PubMed] [Google Scholar]
- 64.Creswell JW, Clark VLP. Designing and conducting mixed methods research, 2nd edn: SAGE Publications; 2010. [Google Scholar]
- 65.Brod M, Tesler LE, Christensen TL. Qualitative research and content validity: developing best practices based on science and experience. Quality of Life Research 2009;18(9):1263–1278. [DOI] [PubMed] [Google Scholar]
- 66.Ickes MJ, McMullen J, Haider T, Sharma M. Global school-based childhood obesity interventions: a review. International Journal of Environmental Research and Public Health 2014;11(9):8940–8961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Treuth MS, Sherwood NE, Butte NF, Mcclanahan B, Obarzanek E, Zhou A, et al. Validity and reliability of activity measures in African-American girls for GEMS. Medicine and Science in Sports and Exercise 2003;35(3):532–539. [DOI] [PubMed] [Google Scholar]
- 68.Sallis JF, Taylor WC, Dowda M, Freedson PS, Pate RR. Correlates of vigorous physical activity for children in grades 1 through 12: comparing parent-reported and objectively-measured physical activity. Pediatric Exercise Science 2002;14(1):30–44. [Google Scholar]
- 69.Ma X, Barnes TL, Freedman DA, Bell BA, Colabianchi N, Liese AD. Test–retest reliability of a questionnaire measuring perceptions of neighborhood food environment. Health & Place 2013;21:65–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.SIP 4–99 Research Group (October 2002). Environmental Supports for Physical Activity Questionnaire Prevention Research Center, Norman J. School of Public Health, University of South Carolina. Available at: http://prevention.sph.sc.edu/tools/Env_Supports_for_PA.pdf. [Accessed 09/30/2016].