Abstract
Objective
According to the guidelines, rescuers should provide chest compressions (CC) ~1.5 inches (40 mm) for infants. Feedback devices could help rescuers perform CC with adequate rates (CCR) and depths (CCD). However, there is no CC feedback device for infant cardiopulmonary resuscitation (CPR). We suggest a smartwatch-based CC feedback application for infant CPR.
Participants and methods
We created a smartwatch-based CC feedback application. This application provides feedback on CCD and CCR by colour and text for infant CPR. To evaluate the application, 30 participants were divided randomly into two groups on the basis of whether CC was performed with or without the assistance of the smartwatch application. Both groups performed continuous CC-only CPR for 2 min on an infant mannequin placed on a firm table. We collected CC parameters from the mannequin, including the proportion of correct depth, CCR, CCD and the proportion of correct decompression depth.
Results
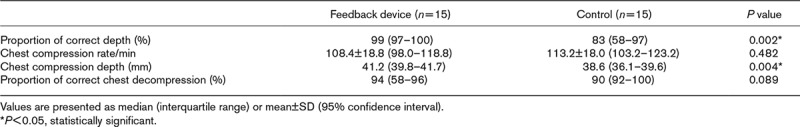
Demographics between the two groups were not significantly different. The median (interquartile range) proportion of correct depth was 99 (97–100) with feedback compared with 83 (58–97) without feedback (P = 0.002). The CCR and proportion of correct decompression depth were not significantly different between the two groups (P = 0.482 and 0.089). The CCD of the feedback group was significantly deeper than that of the control group [feedback vs. control: 41.2 (39.8–41.7) mm vs. 38.6 (36.1–39.6) mm; P=0.004].
Conclusion
Rescuers who receive feedback of CC parameters from a smartwatch could perform adequate CC during infant CPR.
Keywords: application, cardiopulmonary resuscitation, paediatric basic life support, smartwatch
Introduction
Paediatric cardiac arrest has a lower reported survival rate than adult cardiac arrest [1,2]. In addition, the cerebral performance category level of paediatric postcardiac arrest patients with the return of spontaneous circulation has been reported to be poorer than that for adults [3]. Among paediatric cardiac arrest cases, the survival rate for infants is lower than that for children or adolescents [3].
The American Heart Association (AHA) and the European Resuscitation Council guidelines have emphasized that survival rates and good neurologic outcomes are closely related to the quality of cardiopulmonary resuscitation (CPR) [4,5]. According to the 2015 AHA guidelines, in case of cardiac arrest in infants, rescuers should provide chest compressions (CC) with a depth (CCD) that is at least one-third the anterior–posterior diameter of the chest. This equates to ~1.5 inches (4 cm) in infants [4]. The chest compression rate (CCR) recommendation is 100–120 counts/min. However, several studies have reported that rescuers are unable to perform high-quality CC in accordance with the guidelines [6].
For effective CC, visual and audible feedback devices have been developed and are used frequently; these devices are recommended in the guidelines. Furthermore, many studies have reported the effectiveness of feedback devices. These visual and audible devices provide the real-time depths and rates on the compressed chest wall by using an accelerometer and/or a pressure sensor [7–15]. However, almost all commercial feedback devices are for adult CPR. To the best of our knowledge, there is no CC feedback device for infant CPR. According to the 2015 AHA guidelines, although the effectiveness of paediatric CPR feedback devices was not reviewed, the consensus of the group is that the use of feedback devices will likely help rescuers perform adequate CCR and CCD, and that they should be used when available [4].
The current CC feedback devices are difficult to apply to infants. Most feedback devices for adults are meant to be attached to the adult patient’s chest wall; therefore, they are too large for infants. In addition, the target depths for adults and infants are different. Furthermore, the performance of adult CC requires the use of both hands, whereas that for infants requires the use of two fingers.
Recently, the effectiveness of a feedback device on the basis of a smartwatch for CC has been reported [16]. A smartwatch is beneficial for infant CC because it is not in direct contact with the patient’s body; therefore, it is appropriate for the small bodies of infants. This study evaluated the effectiveness of a feedback device on the basis of a smartwatch for infant cardiac arrest treated by the two-finger method of CPR by a single rescuer.
Participants and methods
Study design
We designed a prospective, randomized, controlled parallel study. The study was carried out at Hanyang University’s Simulation Centre (Seoul, Republic of Korea) in April 2016. The study was approved by the Institutional Review Board of the Hanyang University Hospital (HYUH2016-06-030-003). The study protocol was registered at the Clinical Research Information Service (cris.nih.go.kr: KCT0002016).
Participants
We recruited a total of 30 volunteers from Hanyang University; all of them were students of the medical college. The inclusion criteria were age older than 18 years and good health status. Volunteers were excluded if they had wrist, spine or pulmonary/heart diseases. All participants were taught a 4 h course of paediatric basic life support training over 2 weeks. The participants received information on this study before the experiment and they provided written consent.
We evaluated the preliminary results of six participants from the pilot study. The six volunteers were divided randomly evenly into two groups, the smartwatch feedback group and the control group, by drawing lots. All six participants compressed below the intermammary line of the infant mannequin for 2 min without performing rescue breathing; we evaluated the proportions of correct depth (%CD) (mean ± SD). The %CD is defined as the ratio of the number of CCD between 3.5 and 4.5 cm to the total number of CC during 2 min. The %CD values were 99 ± 1.7% for the feedback group and 72 ± 25.5% for the control group. The sample size was calculated using the G-power 3.1.9 program (Heine Heinrich University, Düsseldorf, Germany), an α error of 0.05, a power of 0.95 and the results of the previous pilot study; the estimated sample size was 26 participants (effect size, 1.49; intervention group, 13; control group, 13). However, 30 participants were enroled to account for a 10% dropout rate (Fig. 1).
Fig. 1.
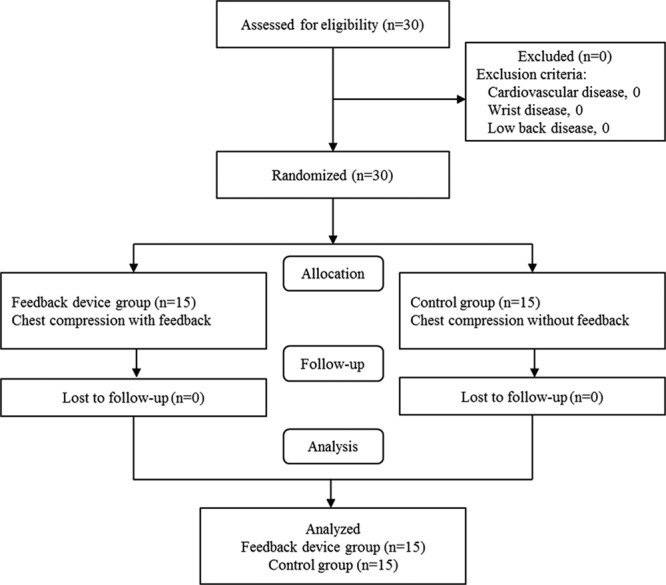
Flowchart of participant enrolment.
Equipment and material
A CPR training infant mannequin (Resusci Baby QCPR; Laerdal, Stavanger, Norway) and recording program (Simpad Skillreporter; Laerdal) were used for this study. The mannequin was able to measure several parameters, including CCD, CCR and decompression depth, by a sensor when participants compressed below the intermammary line. The maximum compressed depth for this mannequin was 47 mm. A smartwatch (Galaxy Gear Live; Samsung Electronics, Seoul, Republic of Korea) was used as a feedback device to implement the android application. The development of the CCD feedback application has been reported previously [16]. To estimate real-time CCD, we developed an algorithm for smartwatches by double integration of the three-axis acceleration signals from a built-in accelerometer with additional signal processing [16,17]. The experiment was conducted on a table and firm surface to avoid the influence of the mattress effect (the absorption of some of the force of the CC) [18].
Participants performed CC on a mannequin while wearing a smartwatch. During this time, the display of the device showed three different colours as visual feedback. A flowchart of CC feedback algorithm is shown in Fig. 2. A blue colour was shown on the display when the CCD was more than 4.5 cm. A red colour was shown when the CCD was less than 3.5 cm. A green colour was shown when the range of the CCD was between 3.5 and 4.5 cm (Fig. 2). In addition, regular vibrations generated by the smartwatch at a rate of 110/min were used to guide the CCR. The numbers of compressions with certain depths and rates were shown on the display of the smartwatch.
Fig. 2.
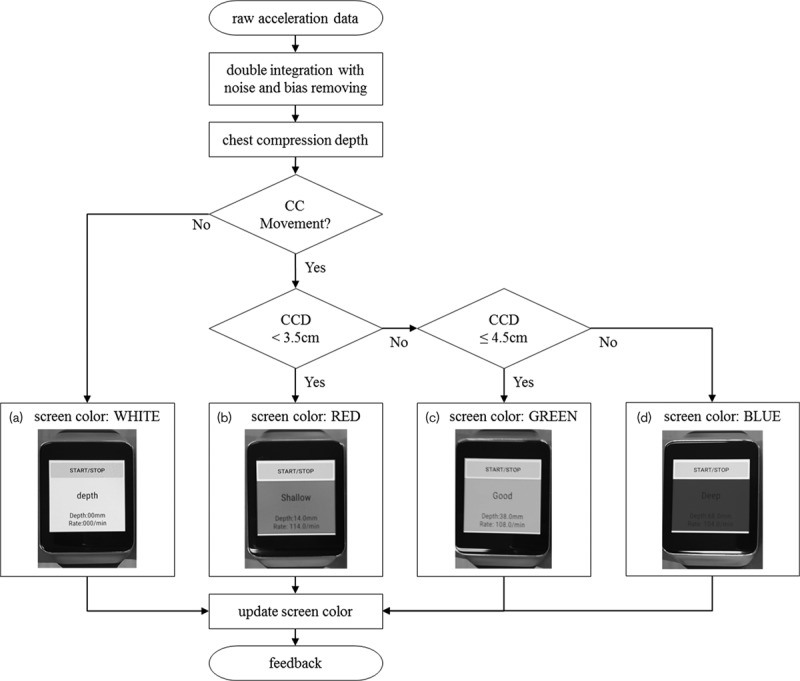
Flowchart of chest compression (CC) feedback. (a) White was shown when the smartwatch was not moved. (b) Red was shown on the display of smartwatch when the depth was less than 3.5 cm, (c) green was shown when the depth was between 3.5 and 4.5 cm and (d) blue was shown when the depth was more than 4.5 cm.
Intervention
All participants were allocated randomly in a 1: 1 ratio to the intervention group (n = 15) and the control group (n = 15). Randomization was performed using a sequence generator (http://www.random.org/). All participants performed CC continuously without artificial breathing in the standing position adjacent to the mannequin on a table for 2 min and compressed below the intermammary line using the two-finger method. During the experiment, investigators and participants could not see each other because of a partition that separated them. In addition, investigators were not aware of the participant groups. In the intervention group, individuals with no connection to this study wore a smartwatch on their wrist and used the feedback program; participants performed CC with the aid of feedback. Conversely, the participants of the control group performed CC without the aid of a feedback device. Participant characteristics such as age, weight, CPR education and experience with real-life CPR were recorded. Data were downloaded and collected directly from the mannequin’s recording system by one author who was blinded to the group allocations.
Primary and secondary outcomes
In this study, the primary outcome was the estimation of the %CD, which was defined as the ratio of the number of CCD between 3.5 and 4.5 cm to the total number of CC during 2 min. In addition, CCD, CCR and %DD were investigated as secondary outcomes. The %DD was defined as the ratio of the number of decompressions with a recoil depth less than 0.5 cm to the total number of decompressions during 2 min.
Statistical analysis
The data were compiled using a standard spread sheet application (Excel 2016; Microsoft, Redmond, Washington, USA) and were analysed using SPSS, version 21.0 KO for Windows (SPSS Inc., Chicago, Illinois, USA). Kolmogorov–Smirnov tests were performed for normal distribution for all datasets. Descriptive statistics were used to describe the baseline characteristics of the study and to present categorical variables as frequencies and percentages. Normally distributed data are presented as the mean ± SD with 95% confidence intervals, whereas non-normally distributed data are presented as medians with interquartile ranges (IQRs) with 95% confidence interval. Student’s t-test or Mann–Whitney U-test was used for comparisons of continuous variables; the χ2-test or Fisher’s exact test was used for categorical variables.
Results
A total of 30 participants were recruited in this study; there were no exclusions (Fig. 1). The baseline characteristics of the participants are summarized in Table 1. There were no significant differences in the demographic characteristics between the two groups. The results for the CC performance are shown in Table 2. The median (IQR) values of the %CD for the intervention and control groups were 99% (97–100) and 83% (58–97), respectively (P = 0.002). The median (IQR) values of CCD for the intervention and control groups were 41.2 mm (39.8–41.7) and 38.6 mm (36.1–39.6), respectively (P = 0.004). There were no significant differences between the two groups for CCR and %DD (P = 0.482 and 0.089, respectively).
Table 1.
Baseline characteristics
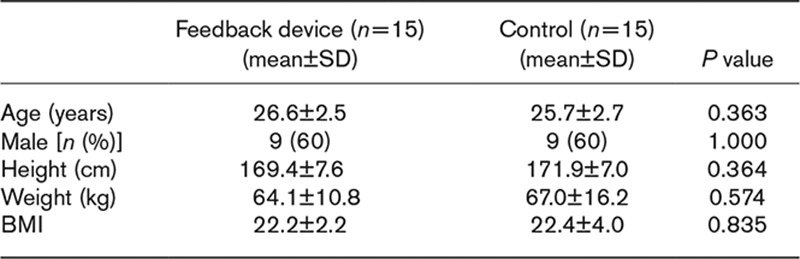
Table 2.
Quality of chest compressions compared between the two groups using the feedback device and not using the feedback device
Discussion
Many feedback devices have been developed and used for high-quality CC [7–15]. Several recent studies have reported the use of smartphones as feedback devices [17,19,20]. In the event of sudden cardiac arrest, the probability that there will be no commercial feedback device available is high. However, smartphones will solve this problem. For infant CC (two-finger method), a smartphone should be fixed to the wrist, forearm or upper arm using an armband. However, the farther the smartphone is from the sternum, the less accurate the feedback [21]. Smartwatch-based feedback devices would be adequate for infant CPR because they are easy to wear, lightweight and able to provide feedback near the patient’s chest wall (but not directly touching it).
The feedback of the smartwatch helped in the performance of CC with accurate depths [%CD, 99% (97–100) vs. 83% (58–97); P = 0.002]. A smartwatch-based feedback device would increase %CD by allowing for adequate compression depth ranges (3.5–4.5 cm) and avoiding shallow or excessively deep compressions. In the case of shallow CC, the cardiac output is not appropriate [22–24]. Excessive CCD cause complications, including fractures of the ribs, pneumothorax and haemothorax [25–28].
Participants of the two groups achieved adequate CCR. This might be because participants were taught paediatric basic life support only 2 weeks before the experiment. However, we expect that feedback from a smartwatch would be effective after the effectiveness of the education had declined [29]. There was a large SD of CCR in the smartwatch feedback device group. It seems that, although the CCR was guided by vibration, the participants could not feel the vibration well during CC. They also could not see the text of CCR feedback on the screen well during CC. There were no significant differences in %DD because the smartwatch-based feedback device could not provide feedback on decompression.
Haque et al. [30] reported that when performing CC using the two-finger method, rescuer fatigue increased and the quality of CC decreased. According to the report by Martin et al. [31], CC feedback helped maintain high-quality CC despite increased fatigue. Therefore, smartwatch-based feedback may also reduce fatigue-related quality degradation.
Martin et al. [31] reported that real-time feedback was helpful during infant CC. In that study, it was reported that the participants performed high-quality CPR when feedback was provided by the mannequin. Although this is expected to be effective during education involving feedback sensors inside the infant mannequin, it cannot be applied to real patients. However, the smartwatch-based feedback device proposed in our study can be applied to real patients.
For infants experiencing cardiac arrest, rescuers should compress the chest at least one-third the anterior–posterior diameter of the chest [4]. This equates to ~1.5 inches (4 cm) in infants; however, depending on the infant’s age and weight, the anterior–posterior diameter could be different. Therefore, the quantified 1.5 inches (4 cm) might not be appropriate for all infants. However, if the anterior–posterior diameter is measured and the target depth is obtained by inputting the information into the smartwatch, then CC can be performed with a more accurate depth.
There were several limitations to this study. First, although there was a significant difference in %CD and CCD in this study, these results do not necessarily translate into improved clinical outcome. Because this was a simulation study using a mannequin rather than a clinical study, the features of a clinical situation were not entirely reflected. To address this, clinical studies of the CC feedback effects are required. Second, only one type of smartwatch (Android) was used for this study. Third, rescuers performed the two-finger method, not the two-thumb method [32]. In this smartwatch-based feedback system, as the CCD is estimated through the movement of the acceleration sensor, it is difficult to apply to the two-thumb method. Fourth, this feedback system with an accelerometer does not compensate for mattress compression and could be inappropriate for cardiac arrest patients on a bed. Fifth, a real cardiac arrest situation is often urgent and the rescuer is typically in a panicked state; therefore, it is important that feedback devices are used quickly. However, this study did not assess the time that it took participants to operate the smartwatch feedback program. Further studies are required that include factors associated with the operating time because there are many variables involved with the operating program, despite the actual operating time taking only seconds.
Conclusion
A smartwatch CPR feedback system could provide assistance in achieving the ideal CCD range in accordance with CPR guidelines from the AHA for infants experiencing cardiac arrest.
Acknowledgements
J. Lee, Y. Song and J. Oh conceived the study, designed the trial and obtained the research funding; Y. Chee and Y. Song developed the algorithm; H. Kang, TH. Lim and J. Oh supervised the trial conduct and data collection; C. Ahn and H. Shin analysed the data statistically; Y. Song and J. Lee drafted the manuscript, and all authors contributed substantially to its revision; J. Oh takes responsibility for the paper as a whole.
This work was supported by the research fund of Hanyang University (HY-2017).
This study was supported by the National Research Foundation of Korea (NRF-2017R1C1B5017116).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Juncheol Lee and Yeongtak Song contributed equally to the writing of this article.
References
- 1.Donoghue AJ, Nadkarni V, Berg RA, Osmond MH, Wells G, Nesbitt L, et al. Out-of-hospital pediatric cardiac arrest: an epidemiologic review and assessment of current knowledge. Ann Emerg Med. 2005; 46:512–522. [DOI] [PubMed] [Google Scholar]
- 2.Young KD, Gausche-Hill M, McClung CD, Lewis RJ. A prospective, population-based study of the epidemiology and outcome of out-of-hospital pediatric cardiopulmonary arrest. Pediatrics. 2004; 114:157–164. [DOI] [PubMed] [Google Scholar]
- 3.Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children the resuscitation outcomes consortium epistry–cardiac arrest. Circulation. 2009; 119:1484–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atkins DL, Berger S, Duff JP, Gonzales JC, Hunt EA, Joyner BL, et al. Part 11: Pediatric Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015; 132:S519–S525. [DOI] [PubMed] [Google Scholar]
- 5.Maconochie IK, Bingham R, Eich C, López-Herce J, Rodríguez-Núnez A, Rajka T, et al. European Resuscitation Council guidelines for resuscitation 2015: section 6. Paediatric life support. Resuscitation. 2015; 95:223–248. [DOI] [PubMed] [Google Scholar]
- 6.Martin PS, Kemp AM, Theobald PS, Maguire SA, Jones MD. Do chest compressions during simulated infant CPR comply with international recommendations?. Arch Dis Child. 2012; 98:576–581. [DOI] [PubMed] [Google Scholar]
- 7.Abella BS, Edelson DP, Kim S, Retzer E, Myklebust H, Barry AM, et al. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation. 2007; 73:54–61. [DOI] [PubMed] [Google Scholar]
- 8.Hostler D, Everson-Stewart S, Rea TD, Stiell IG, Callaway CW, Kudenchuk PJ, et al. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. BMJ. 2011; 342:d512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeung J, Meeks R, Edelson D, Gao F, Soar J, Perkins GD. The use of CPR feedback/prompt devices during training and CPR performance: a systematic review. Resuscitation. 2009; 80:743–751. [DOI] [PubMed] [Google Scholar]
- 10.Kirkbright S, Finn J, Tohira H, Bremner A, Jacobs I, Celenza A. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation. 2014; 85:460–471. [DOI] [PubMed] [Google Scholar]
- 11.Kramer-Johansen J, Myklebust H, Wik L, Fellows B, Svensson L, Sørebø H, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006; 71:283–292. [DOI] [PubMed] [Google Scholar]
- 12.Buléon C, Parienti JJ, Halbout L, Arrot X, Régent HDF, Chelarescu D, et al. Improvement in chest compression quality using a feedback device (CPRmeter): a simulation randomized crossover study. Am J Emerg Med. 2013; 31:1457–1461. [DOI] [PubMed] [Google Scholar]
- 13.Krasteva V, Jekova I, Didon JP. An audiovisual feedback device for compression depth, rate and complete chest recoil can improve the CPR performance of lay persons during self-training on a manikin. Physiol Meas. 2011; 32:687–699. [DOI] [PubMed] [Google Scholar]
- 14.Skorning M, Beckers SK, Brokmann JC, Rörtgen D, Bergrath S, Veiser T, et al. New visual feedback device improves performance of chest compressions by professionals in simulated cardiac arrest. Resuscitation. 2010; 81:53–58. [DOI] [PubMed] [Google Scholar]
- 15.Bohn A, Weber TP, Wecker S, Harding U, Osada N, van Aken H, et al. The addition of voice prompts to audiovisual feedback and debriefing does not modify CPR quality or outcomes in out of hospital cardiac arrest – a prospective, randomized trial. Resuscitation. 2011; 82:257–262. [DOI] [PubMed] [Google Scholar]
- 16.Song Y, Chee Y, Oh J, Ahn C, Lim TH. Smartwatches as chest compression feedback devices: A feasibility study. Resuscitation. 2016; 103:20–23. [DOI] [PubMed] [Google Scholar]
- 17.Song Y, Oh J, Chee Y. A new chest compression depth feedback algorithm for high-quality CPR based on smartphone. Telemed J E Health. 2015; 21:36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perkins GD, Benny R, Giles S, Gao F, Tweed MJ. Do different mattresses affect the quality of cardiopulmonary resuscitation?. Intensive Care Med. 2003; 29:2330–2335. [DOI] [PubMed] [Google Scholar]
- 19.Park C, Kang I, Heo S, Chae Y, Kim H, Park S, et al. A randomised, cross over study using a mannequin model to evaluate the effects on CPR quality of real-time audio-visual feedback provided by a smartphone application. Hong Kong J Emerg Med. 2014; 21:153–160. [Google Scholar]
- 20.Sakai T, Kitamura T, Nishiyama C, Murakami Y, Ando M, Kawamura T, et al. Cardiopulmonary resuscitation support application on a smartphone. Circ J. 2015; 79:1052–1057. [DOI] [PubMed] [Google Scholar]
- 21.Park J, Lim T, Lee Y, Kim W, Cho Y, Kang H. Assessment of chest compression depth obtained using the PocketCPR as an educational tool according to smartphone attachment site. Am J Emerg Med. 2016; 34:2243–2246. [DOI] [PubMed] [Google Scholar]
- 22.Vadeboncoeur T, Stolz U, Panchal A, Silver A, Venuti M, Tobin J, et al. Chest compression depth and survival in out-of-hospital cardiac arrest. Resuscitation. 2014; 85:182–188. [DOI] [PubMed] [Google Scholar]
- 23.Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G, Powell J, et al. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation?. Crit Care Med. 2012; 40:1192–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stiell IG, Brown SP, Nichol G, Cheskes S, Vaillancourt C, Callaway CW, et al. What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients?. Circulation. 2014; 130:1962–1970. [DOI] [PubMed] [Google Scholar]
- 25.Kim MJ, Park YS, Kim SW, Yoon YS, Lee KR, Lim TH, et al. Chest injury following cardiopulmonary resuscitation: a prospective computed tomography evaluation. Resuscitation. 2013; 84:361–364. [DOI] [PubMed] [Google Scholar]
- 26.Hellevuo H, Sainio M, Nevalainen R, Huhtala H, Olkkola KT, Tenhunen J, et al. Deeper chest compression–more complications for cardiac arrest patients?. Resuscitation. 2013; 84:760–765. [DOI] [PubMed] [Google Scholar]
- 27.Hoke RS, Chamberlain D. Skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation. 2004; 63:327–338. [DOI] [PubMed] [Google Scholar]
- 28.Reyes J, Somers G, Taylor G, Chiasson D. Increased incidence of CPR-related rib fractures in infants – is it related to changes in CPR technique?. Resuscitation. 2011; 82:545–548. [DOI] [PubMed] [Google Scholar]
- 29.Berden H, Willems FF, Hendrick J, Pijls N, Knape J. How frequently should basic cardiopulmonary resuscitation training be repeated to maintain adequate skills?. BMJ. 1993; 306:1576–1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haque IU, Udassi JP, Udassi S, Theriaque DW, Shuster JJ, Zaritsky AL. Chest compression quality and rescuer fatigue with increased compression to ventilation ratio during single rescuer pediatric CPR. Resuscitation. 2008; 79:82–89. [DOI] [PubMed] [Google Scholar]
- 31.Martin P, Theobald P, Kemp A, Maguire S, Maconochie I, Jones M. Real-time feedback can improve infant manikin cardiopulmonary resuscitation by up to 79% – a randomised controlled trial. Resuscitation. 2013; 84:1125–1130. [DOI] [PubMed] [Google Scholar]
- 32.Huynh TK, Hemway RJ, Perlman JM. The two-thumb technique using an elevated surface is preferable for teaching infant cardiopulmonary resuscitation. J pediatr. 2012; 161:658–661. [DOI] [PubMed] [Google Scholar]


